Abstract
Calcifying tendinitis of the shoulder is a common condition characterized by the deposition of calcium, predominantly hydroxyapatite crystals, in the rotator cuff. A rare complication of this condition is the migration of calcium deposits from tendons, usually the supraspinatus, into the subacromial–subdeltoid bursa or into the humeral greater tuberosity. These complications are responsible for intense acute shoulder pain and functional disability. Patient anamnesis and clinical symptoms must be considered to make the diagnosis, but imaging, particularly sonography, is often necessary, showing a typical presentation related to the locations of calcium deposits. We present sonographic and other imaging features of subacromial–subdeltoid bursitis and humeral osteitis related to the migration of calcium.
Keywords: Shoulder pain, Sonography, Subacromial–subdeltoid bursitis, Humeral osteitis, Calcifying tendinitis
Riassunto
La tendinite calcifica della spalla è una patologia di comune riscontro caratterizzata dal deposito di calcio, prevalentemente cristalli di idrossiapatite, nella cuffia dei rotatori. Una rara complicanza di tale patologia è la migrazione di depositi calcifici dal tendine, solitamente il sovraspinato, nella borsa subacromion-deltoidea o a livello del trochite omerale. Queste complicanze determinano intensa sintomatologia algica ed impotenza funzionale. L’anamnesi e la sintomatologia clinica possono indirizzare la diagnosi ma il ricorso alla diagnostica per immagini, in particolare alla valutazione ecografica, spesso è necessario per giungere alla diagnosi, mostrando caratteristiche patognomoniche in relazione alla sede dei depositi calcifici. In questo lavoro vengono presentati i quadri imaging esemplificativi della borsite subacromion-deltoidea e dell’osteite omerale derivanti dalla migrazione dei depositi di calcio.
Introduction
Calcifying tendinitis of the shoulder is a condition characterized by the deposition of calcium, predominantly hydroxyapatite crystals in the rotator cuff tendons. Rotator cuff calcifications are common findings which occur in up to 7.5 % of adults. Women are more frequently affected than men, with a prevalence in their fourth to sixth decades of life [1].
The most commonly affected tendon of the rotator cuff is the supraspinatus (80 %), followed by the infraspinatus (15 %) and the subscapularis (5 %); more specifically, the critical zone of the supraspinatus tendon (about 1 cm from the tendinous insertion of the supraspinatus on the greater humeral tuberosity), the lower third of the infraspinatus tendon and the pre-insertional fibers of the subscapularis tendon are the most commonly involved sites [2].
The pathogenesis of this disorder is not completely understood but it seems to be related to areas of hypoxia in tendons that lead to a fibrocartilaginous metaplasia and cellular necrosis followed by calcium deposit formation, which typically occurs in an intact tendon. Although considered a self-healing condition it can cause acute/chronic pain and functional disability depending on the stage of the disease.
In the literature, four stages of disease have been described: pre-calcific (Stage 1) in which fibrocartilaginous transformation occurs within tendon fibers, usually asymptomatic; formative (Stage 2) in which calcifications are formed, usually poorly symptomatic, including sub-acute low-grade shoulder pain increasing at night; resorptive (Stage 3), in which the tendon develops increased vasculature and the calcium deposits are usually removed by phagocytes but calcifications may migrate into the adjacent structures in some cases; and post-calcific (Stage 4), in which self-healing and repair of the tendon fibers occur, lasting for several months and which may be associated with shoulder pain and restricted function [2].
Treatment strategies depend on the patient’s symptoms: asymptomatic rotator cuff calcifications do not require any treatment, while cases of symptomatic calcifying tendinitis are treated with non-steroidal anti-inflammatory drugs (NSAIDs) and require an evacuation of calcific material which can be obtained by means of arthroscopy or US-guided puncture, steroid injection, lavage and aspiration [3, 4].
Imaging description
The diagnosis of calcifying tendinitis is mainly based on standard radiographs and ultrasound (US) examination of the shoulder. Plain films (antero-posterior views in neutral and external arm rotation) can accurately assess the presence, size and location of the calcifications.
At US, rotator cuff calcifications appear as intratendinous hyperechoic foci. Bianchi and Martinoli described three main types of calcifications, depending on their percentage of calcium: in type I, calcifications appear as hyperechoic foci with a well-defined acoustic shadowing because it is rich in calcium, corresponds to the formative phase and is presented in up to 80 % of cases; in type II, calcification appears as hyperechoic foci with a faint acoustic shadow, based on the reduced amount of calcium; and in type III, calcification is mildly hyperechoic, nearly isoechoic with the tendon, without an acoustic shadow and thus sometimes difficult to diagnose [2]. Type II and III calcifications (defined “slurry calcifications”) correspond to the resorptive phase in which deposits are almost liquid and can migrate to adjacent structures.
Calcium deposit migration from tendons to the adjacent structures [5] is an uncommon complication of calcifying tendonitis in which intratendinous calcifications are extruded from the tendon into the sub-bursal space and intra-subacromial–subdeltoid bursa (more frequently) (Figs. 1, 2, 3) (movie 1) or into the humeral head (less frequently) (Figs. 4, 5, 6) (movie 2, 3). This complication is accompanied by a severe exacerbation of pain, local tenderness, restricted shoulder mobility and systemic symptoms (fever, raised white cell counts).
Fig. 1.
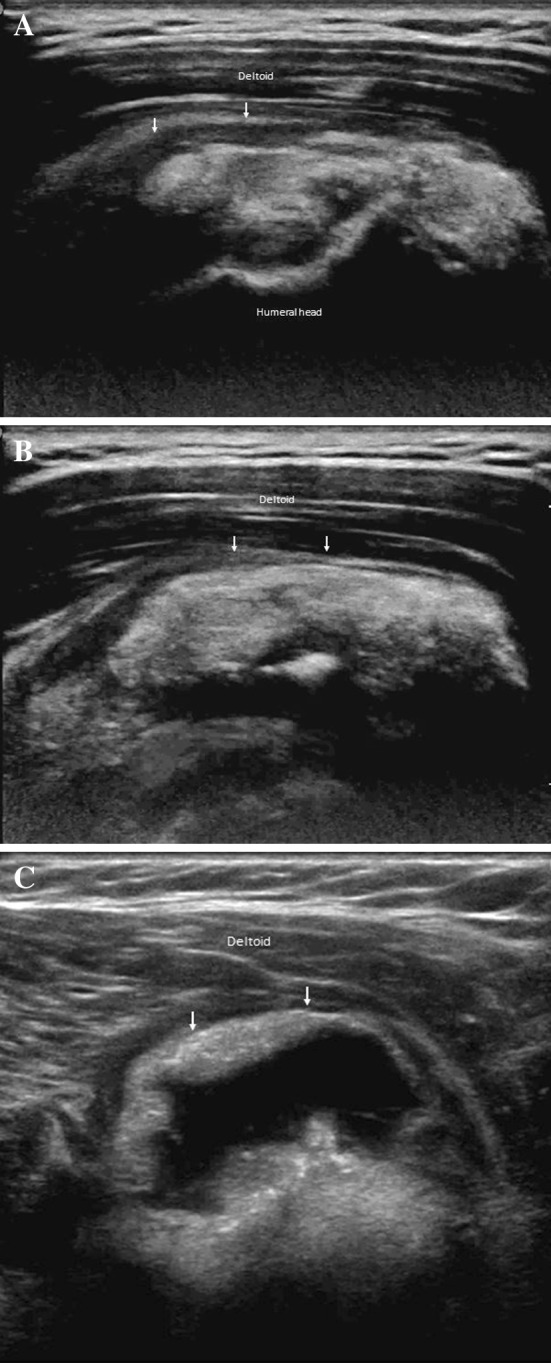
Calcium-related bursitis. From proximal to distal part (a, b, c) ultrasonography shows hyperechoic material (calcium) within the effusion in the subacromial–subdeltoid bursa. The bursa presents thickened walls
Fig. 2.

Calcium-related bursitis. Standard frontal radiography of the shoulder detects multiple ill-defined calcifications between deltoid and supraspinatus
Fig. 3.
Calcium-related bursitis. Axial (a) and sagittal (b) T1-weighted fat saturated sequences after gadolinium injection (Dotarem) show the presence of calcium within the effusion in the subacromial–subdeltoid bursa. Note the contrast enhancement of the thickened bursal walls
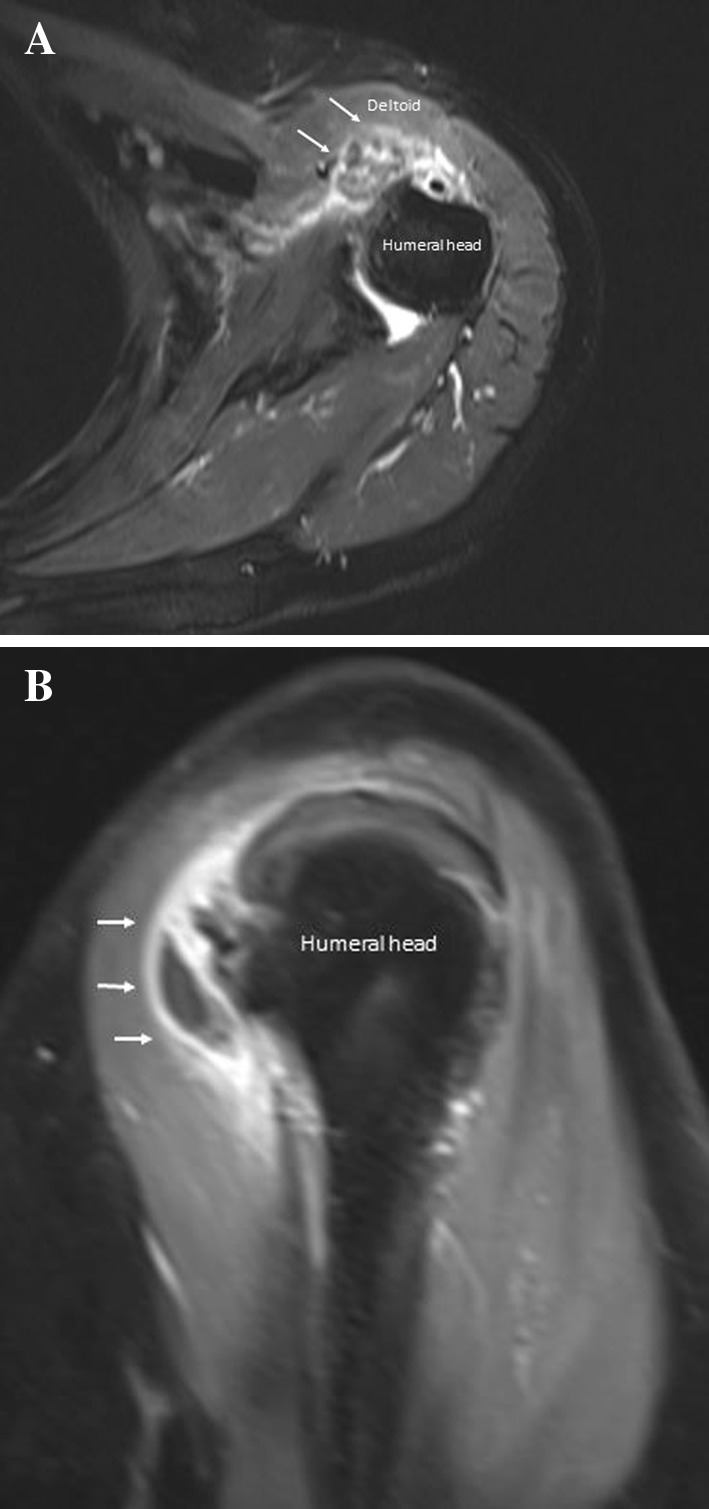
Fig. 4.

Calcium-related osteitis. Ultrasonography shows hyperchoic spots (calcium) (arrows) within humeral head erosion (a, b)
Fig. 5.
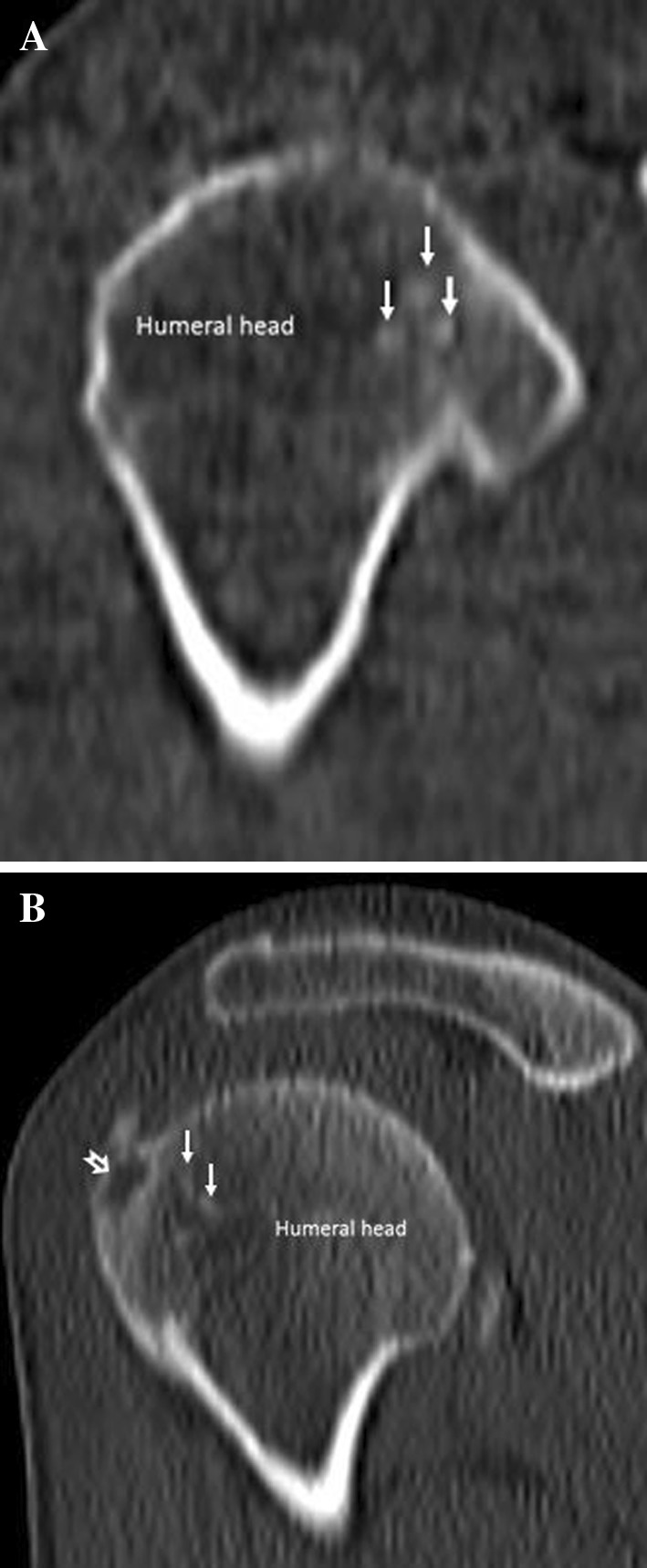
Calcium-related osteitis. Coronal (a) and sagittal (b) computed tomography images detect a well-defined rounded lytic lesion of the humeral greater tuberosity (empty arrow in b) and multiple calcifications within the humeral erosion (arrows)
Fig. 6.
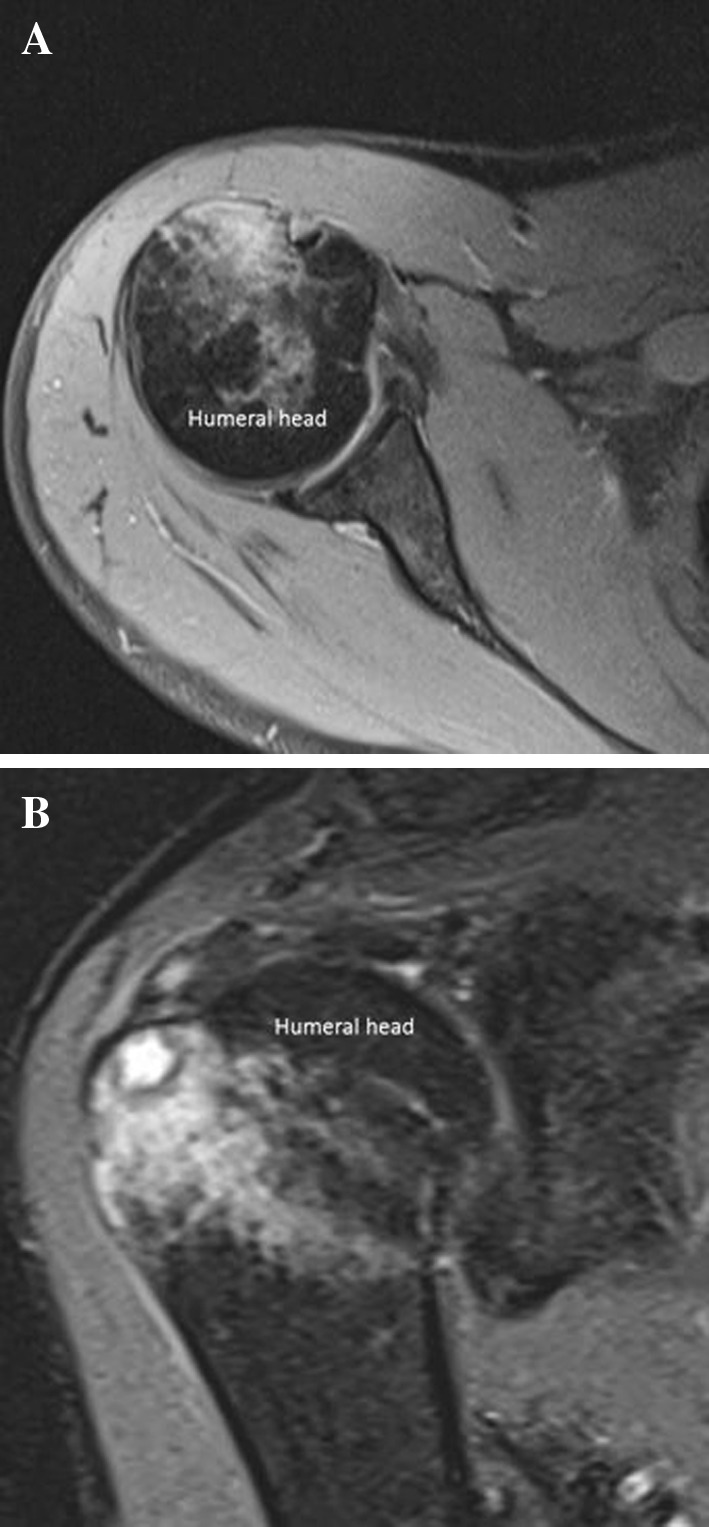
Calcium-related osteitis. Axial (a) and sagittal (b) DP-weighted fat suppression sequences show bone marrow edema of the humeral head
In the sub-bursal extrusion, the calcific deposit relocates between the subacromial–subdeltoid bursa and the tendon from which it derives. Standard radiographs of the shoulder can detect multiple ill-defined calcifications in the subacromial space, but it is often not possible to assess their exact location, whether intratendinous, sub-bursal, or intrabursal. US examination can precisely locate calcium deposits in the subacromial (extra-bursal) space; calcifications usually appear slightly hyperechoic with the tendon displacing a collapsed bursa and are associated with edematous changes in the surrounding fatty space.
In cases of intrabursal penetration of the calcification, at US (Fig. 1) (movie 1) and magnetic resonance (MR) examinations (Fig. 3), the subacromial–subdeltoid bursa presents thickened walls and appears filled with dishomogeneous fluid containing calcium and debris. Bursal-side partial-thickness tendon tears may occur during extrusion of the calcifications into the subacromial bursa. Standard radiographs of the shoulder can detect multiple ill-defined calcifications between the deltoid and supraspinatus (Fig. 2).
Intraosseous migration of tendon calcifications is another rare painful complication of calcifying tendinitis that has been described in the literature, not only in the shoulder [6–8], but also in other tendon insertions such as the pectoralis major, glutei maximus and medius, adductor magnus and deltoid insertions [9]. The pathomechanism is still unknown, but seems to be mediated by acute inflammation and local vasculature changes at the tendon insertion and by mechanical effects of the muscle traction causing bone destruction. In the shoulder, calcium deposits located at the pre-insertional level (calcific enthesopathy) of supraspinatus and infraspinatus, more easily suffer from intrahumeral head migration, into the greater tuberosity [7]. Intraosseous calcification is mobile and may initially appear in the greater tuberosity, where it causes a lytic lesion and then migrates outside the bone.
Sonographic diagnosis of intraosseous loculation from calcifying tendinitis is difficult since US has intrinsic limitations in the assessment of bone. However, with US, it is possible to depict irregularities of cortical outlines, focal bone erosions of the greater tuberosity and multiple small calcifications inside the cortical erosions along with the rotator cuff tendon (Fig. 4) (movies 2, 3); these findings should make the lesion suspected if the patient complains of intense pain without previous injury, but require confirmation with other imaging modalities, including radiography, computed tomography (CT) (Fig. 5) and magnetic resonance (MR) imaging (Fig. 6).
Standard radiographs show focal erosions of the humeral head and a rounded sclerotic intraosseous lesion in the greater tuberosity surrounded by a radiolucent halo; if the calcific deposit has migrated outside the humeral head, plain film shows a rounded well-defined lytic lesion in the greater tuberosity, along with a tendon calcification. CT is the gold standard imaging modality to depict bone lesions (Fig. 5); CTI demonstrates cortical erosion of the humeral head and a rounded well-defined lytic area located in the greater tuberosity; it can also detect calcium deposit in its intraosseous location or in the adjacent tendinous insertion. MRI shows a cystic lesion in the greater tuberosity and the intraosseous/intratendinous calcification; MR is superior in evaluating bone medullary involvement, in fact the bone marrow (Fig. 6) surrounding the cystic lesion of the greater tuberosity presents a typical reactive edema pattern extending from the greater to the lesser tuberosity with a characteristic spare of the cranial part of the proximal humeral epiphysis. Both CT and MR can easily depict a possible tendon-associated tear.
When the calcification presents an intraosseous location, the differential diagnoses for a single sclerotic lesion of humeral head include bone island, osteoblastic metastases and osteoid/osteoblastoma osteoma. When the calcification has migrated outside the humeral head, the differential diagnoses for single lytic lesion include osteonecrosis, chondroma, erosion from synovial processes, soft tissue sarcoma with secondary bone invasion and metastatic lesions. Patient anamnesis, symptoms and imaging information can avoid performing unnecessary tests such as skeletal scintigraphy in the search for a tumor or inadequate aggressive surgery.
Conclusions
Calcifying tendinitis of the shoulder is a common condition characterized by the deposition of calcium, predominantly hydroxyapatite crystals, in the rotator cuff (1, 2). A rare complication of this condition is the migration of calcium deposits from tendon fibers, usually of the supraspinatus, to the subacromial space, into the subacromial–subdeltoid bursa (2) or into the humeral greater tuberosity (6, 7, 8, 9), which is responsible for the intense acute shoulder pain and functional disability. This complication shows a typical US, radiographic, CT and MR imaging presentation, described in this article, which is important to know to make the correct diagnosis and avoid unnecessary invasive tests or aggressive surgery.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. All patients provided written informed consent to the inclusion in this article of information that could potentially lead to their identification.
Conflict of interest
The Authors, Valeria Della Valle, Emilio Maria Bassi and Fabrizio Calliada have no conflict of interests to disclose.
References
- 1.Serafini G, Sconfienza LM, Lacelli F, et al. Rotator cuff calcific tendonitis: short-term and 10-year outcomes after two-needle US-guided percutaneous treatment—nonrandomized controlled trial. Radiology. 2009;252(1):157–164. doi: 10.1148/radiol.2521081816. [DOI] [PubMed] [Google Scholar]
- 2.Bianchi S, Martinoli C (2007) Ultrasound of the musculoskeletal system. Springer. Berlin 198–332
- 3.Tagliafico A, Russo G, Boccalini S et al. (2014) Ultrasound-guided interventional procedures around the shoulder. Radiol Med 119(5):318–26. doi:10.1007/s11547-013-0351-2 [Epub 2013 Dec 3] (Review) [DOI] [PubMed]
- 4.Draghi F, Robotti G, Jacob D, Bianchi S. Interventional musculoskeletal ultrasonography: precautions and contraindications. J Ultrasound. 2010;13(3):126–133. doi: 10.1016/j.jus.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Precerutti M, Garioni E, Madonia L, Draghi F. US anatomy of the shoulder: pictorial essay. J Ultrasound. 2010;13(4):179–187. doi: 10.1016/j.jus.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan R, Kim DH, Millett PJ, Weissman BN (2004). Calcifying tendinitis of the rotator cuff with cortical bone erosion. Skeletal Radiol 33(10):596–9. [Epub 2004 May 25. Erratum in: Skeletal Radiol (2005) 34(1):61] [DOI] [PubMed]
- 7.Martin S, Rapariz M (2010) Intraosseous calcium migration in calcifying tendinitis: a rare cause of single sclerotic injury in the humeral head (2010: 2b) Eur Radiol 20(5):1284–6. doi:10.1007/s00330-009-1500-9 [Epub 2010 Apr 7] [DOI] [PubMed]
- 8.Chagnaud C, Gaubert JY, Champsaur P, et al. Vanishing osteosclerotic lesion of the humeral head. Skeletal Radiol. 1998;27(1):50–52. doi: 10.1007/s002560050337. [DOI] [PubMed] [Google Scholar]
- 9.Flemming DJ, Murphey MD, Shekitka KM, et al. Osseous involvement in calcific tendinitis: a retrospective review of 50 cases. AJR Am J Roentgenol. 2003;181(4):965–972. doi: 10.2214/ajr.181.4.1810965. [DOI] [PubMed] [Google Scholar]


