Abstract
We report our experience in B-mode ocular ultrasonography, focusing on its contribution when the clinical examination proves to be difficult, mainly due to the existence of intraocular opacities of the ocular fundus or diagnostic doubts. We revise the ocular ultrasound technique, its indications and contraindications, comparing to the other imaging techniques. In our experience ultrasonography revealed pathological findings which confirmed the clinical suspicion in most of cases or provide additional information. With understanding of the indications for ultrasonography and proper examination technique, one can gather a vast amount of information not possible with clinical examination alone.
Keywords: Ophthalmic ultrasonography, Cataract, Hyphema, Hypopyon, Hemovitreous, Vogt–Koyanagi–Harada
Sommario
Riportiamo la nostra esperienza di ecografia oculare in B-mode, concentrandoci sul suo contributo quando l’esame clinico si riveli difficile, principalmente per l’esistenza di opacità intraoculari del fondo o in presenza di dubbi diagnostici. Rivediamo la tecnica ecografica, le sue indicazioni e controindicazioni, anche a confronto con le altre tecniche di imaging. Nella nostra esperienza l’ecografia ha rilevato reperti patologici che, nella maggior parte dei casi, hanno confermato il sospetto clinico, o fornito informazioni aggiuntive. Limitando le indicazioni ed eseguendo l’esame con tecnica corretta, si possono raccogliere una grande quantità d’informazioni che non è possibile avere con il solo esame clinico.
Introduction
The present study reports our experience in ophthalmic ultrasonography, highlighting the additional value of B-mode ultrasound with respect to clinical examination and A-mode (pen-probe) techniques usually performed by ophthalmologists in order to evaluate patients with ophthalmic diseases.
The study focuses on the contribution of ocular ultrasonography when clinical examination proves to be difficult, mainly due to the existence of intraocular opacities or diagnostic doubts. In these cases, the implementation of a B-mode ultrasound examination can streamline or modify the management of patient condition.
Materials and methods
We used linear high-frequency (7.5–13.0 MHz) transducers, HD11XE Philips and GE Logiq 500. The examinations were performed in B-mode and in color Doppler imaging by dedicated radiologists with more than 10 years of experience in this field. Also, a dedicated ophthalmic scanner (Aviso Ultrasound Platform UBM, High-frequency, A/B scan) was used in some examinations.
Patients were in supine decubitus with eyes closed. Contact lenses were removed before performing ultrasound (US). Axial images were obtained from the upper to lower poles of the entire globe (Fig. 1a–c). Sagittal images were obtained from the temporal to the nasal side. Oblique views and dynamic images were also performed with eye movements from right to left and up to down. Dynamic imaging was unavoidable; it improves visualization of the entire eye and depicts movement of vitreous echoes or lines [1].
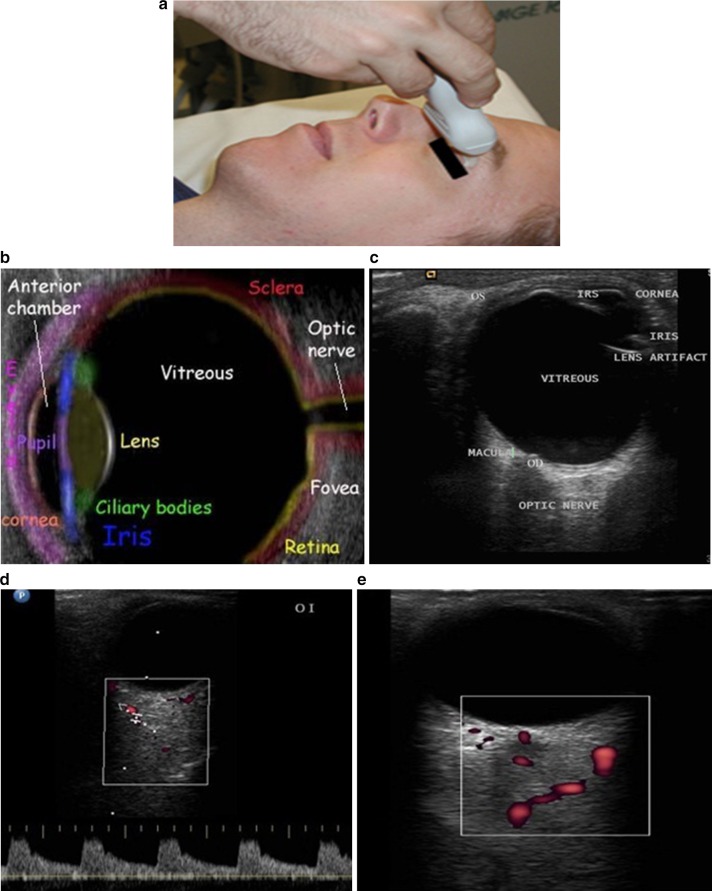
Fig. 1.
a Contact technique for eye ultrasound echography. b, c Eyeball anatomy seen by B-mode ultrasonography. d, e Doppler ecography showing the central retinal artery
Color Doppler US easily visualizes the central retinal artery and the short posterior ciliary arteries, and can also depict the retinal layer and the central retinal vein [2, 3]. B-mode ultrasonography (or B-scan) of the eye is performed by interposing an ultrasound gel and then leaning the probe directly on the eyelid of the patient with the patient’s eye closed (Fig. 1a). B-mode ecography visualizes the anterior chamber and lens, and the anechoic vitreous with the posterior wall in the deep. More deeply, the hypoechoic band of the optic nerve is observed (Fig. 1b, c).
In some cases it’s possible to perform Doppler ultrasonography in order to visualize the blood flow thorough the central retinal artery (Fig. 1d, e).
Results
We assessed several groups of diseases: complete cataracts; lesions of the anterior chamber—bleeding (hyphema) and due to pus deposit (hypopyon); hemovitreous; neoplastic lesions—choroidal melanomas (including one amelanotic melanoma), one nevus and one melanocytoma; macular degenerations (drusen); congenital diseases (juxtapapillary colobomas); inflammatory pathologies, including one Vogt–Koyanagi–Harada syndrome; lesions in the posterior parietal layers of the eyeball—retinal detachment, choroidal detachment, mixed retinal and choroidal detachment, vitreous detachment.
Each group revealed specific B-scan sonographic features:
Cataracts are a degenerative disease of the lens that is usually seen in older age-groups. They can sometimes be secondary to trauma, when the lens becomes opaque due to deposition of reflective material beneath the lens capsule [4]. In ophthalmoscopy, a white reflection with an opaque lens is seen, a finding known as leukocoria [5] (Fig. 2a). An immature cataract shows scattered opacities separated by clear zones. In a complete cataract, the lens has a completely opaque cortex and is seen as a hyperechoic structure (Fig. 2b, c).
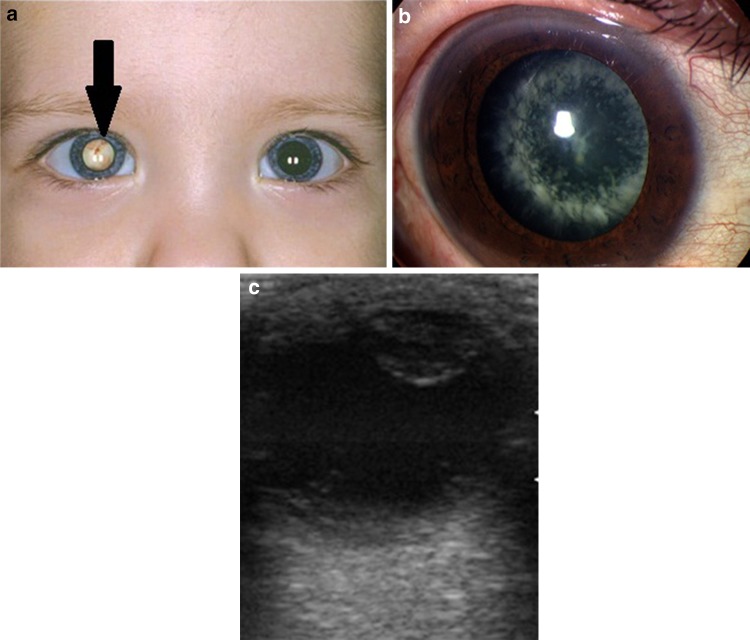
Fig. 2.
a Color image of leukokoria in the right eye. b Ophthalmoscopic image of a complete cataract. c Corresponding B-mode US
Hyphema is represented by the presence of blood in the anterior chamber caused by disruption of vessels in the iris and ciliary body [6]. Ultrasound performed with higher-frequency (35–50 MHz) scanners may improve the visualization of the anterior chamber; however, conventional US also provides diagnostic information [7]. The ultrasound image shows small echogenic areas due to bleeding (Fig. 3a, b).
Fig. 3.
a Ophthalmoscopic image of a post-traumatic hyphema. b Corresponding B-mode US: in the circle is the blood effusion in the anterior chamber of the eye
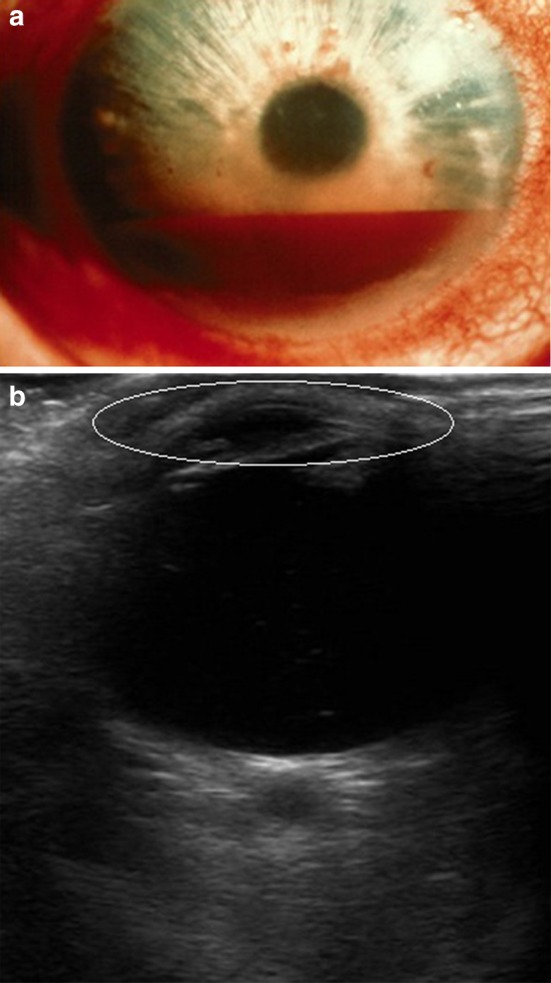
Hypopyon is a leukocytic exudate (pus), seen in the anterior chamber, usually associated with redness of the conjunctiva and the underlying episclera. It is a sign of inflammation of the anterior uvea and iris, i.e., iritis, which is a form of anterior uveitis. The exudate settles at the bottom due to gravity. It is represented as an echogenic band in the anterior chamber due to the collection of purulent debris (Fig. 4a, b).
Fig. 4.
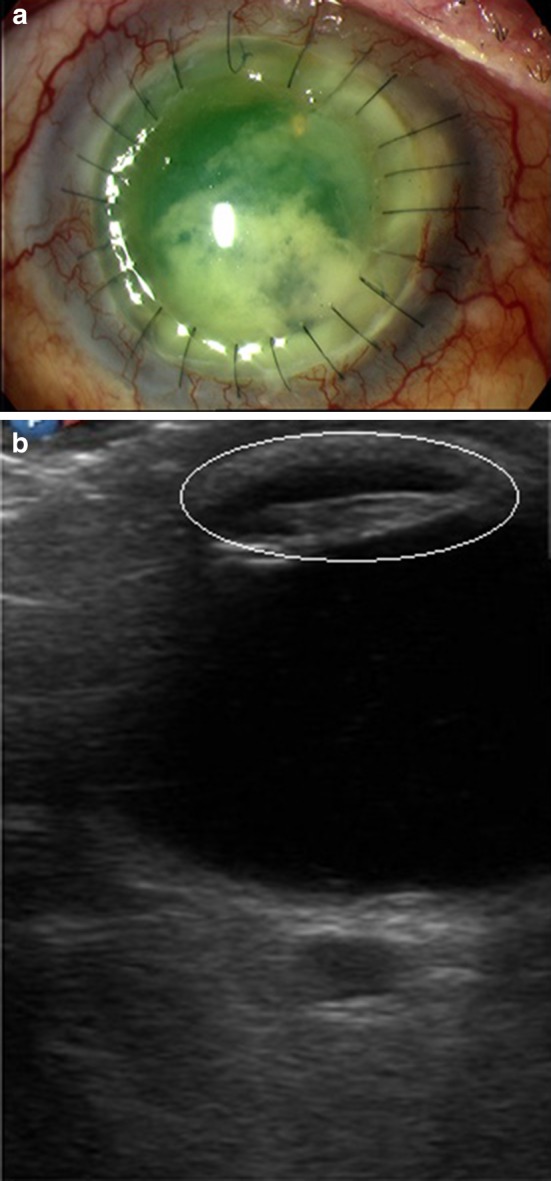
a Hypopyon after penetrating keratoplasty, ophthalmoscopic image. b Pus and fibrin in the anterior chamber
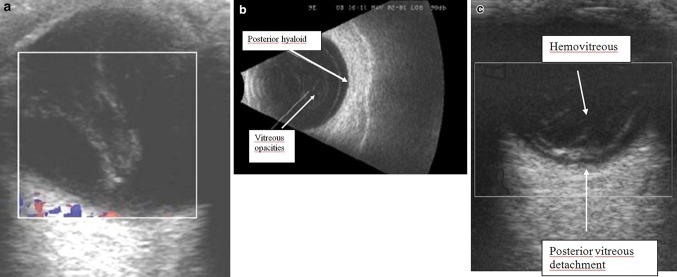
Vitreous hemorrhage can result from tearing due to vitreoretinal traction, diabetic retinopathy, vasculitis, subarachnoid hemorrhage, and blunt trauma to the eye. B-scan of vitreous hemorrhage reveals widespread low-intensity echoes in the vitreous chamber, which shows marked after-movement on dynamic scanning (Fig. 5). Small hemorrhages may be difficult to demonstrate and usually resolve after an interval. Larger bleeds are seen more easily as low density echoes, which may persist with development of fibrinous membranes [8].
Fig. 5.
Hemovitreous associated with retinal detachment
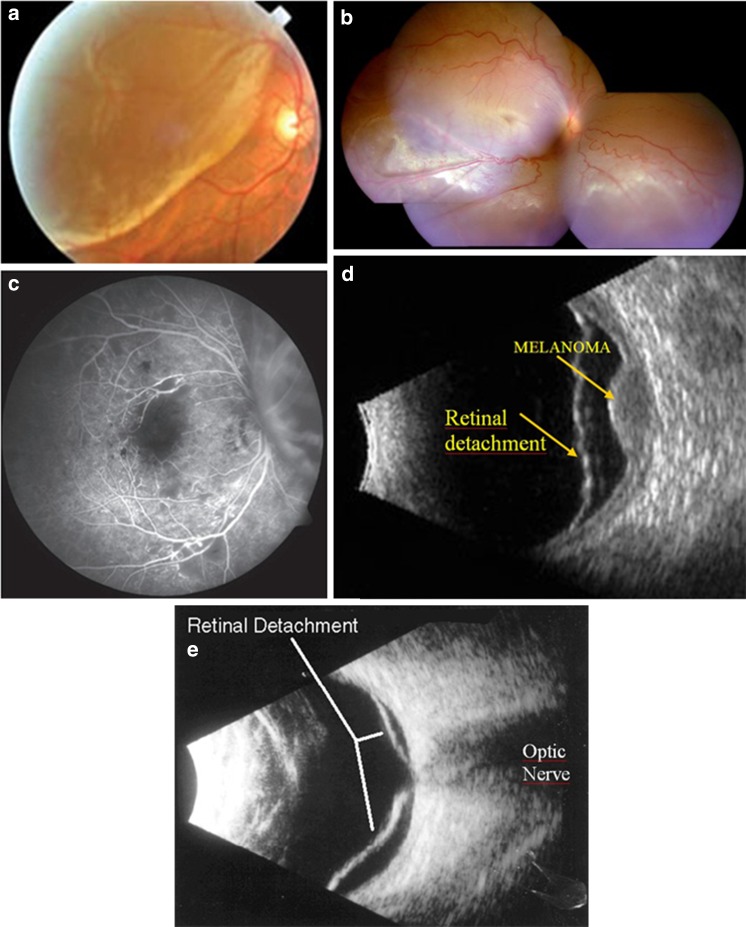
Choroidal melanoma, the commonest primary intraocular tumor in adults, arises from the choroid and ciliary bodies. Most of these lesions arise posterior to the equator of the eyeball. On B-scan, it is seen as a lenticular-shaped mass arising from the choroid. Ultrasonography is used to assess scleral erosions and extraocular extension into orbital fat. Some tumors have a collar-button or mushroom shape. Blood flow within the tumor is seen on color Doppler as pulsating channels or lakes of color. Choroidal melanoma may be associated with retinal detachment. The tumor has a bilobed or ‘cottage-loaf’ appearance, which is caused by wasting as it breaks through Bruch’s membrane (Fig. 6a–d).
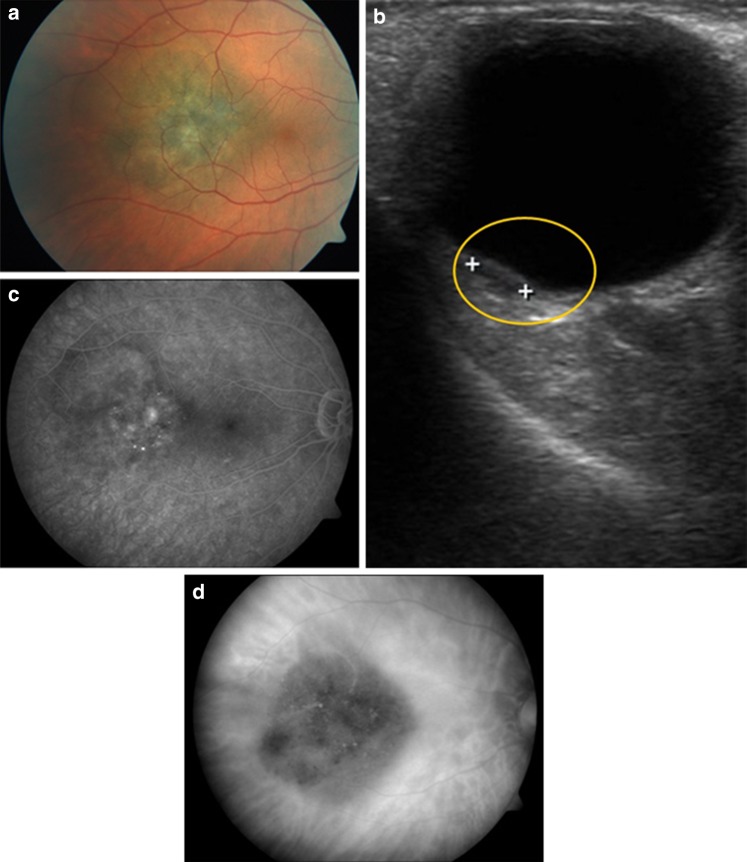
Fig. 6.
a Ophthalmoscopic image of choroidal melanoma involving the posterior pole of the eye. b Corresponding ultrasonography image of choroidal melanoma. c Corresponding angiography with fluorescein. d Corresponding angiography with indocyanine-green
The pigmentation can range from deep brown (melanotic) to no pigmentation (amelanotic) (Fig. 7a–d). An area of excavation under a small posterior wall mass is indicative of melanoma, although this feature is not always present [1].
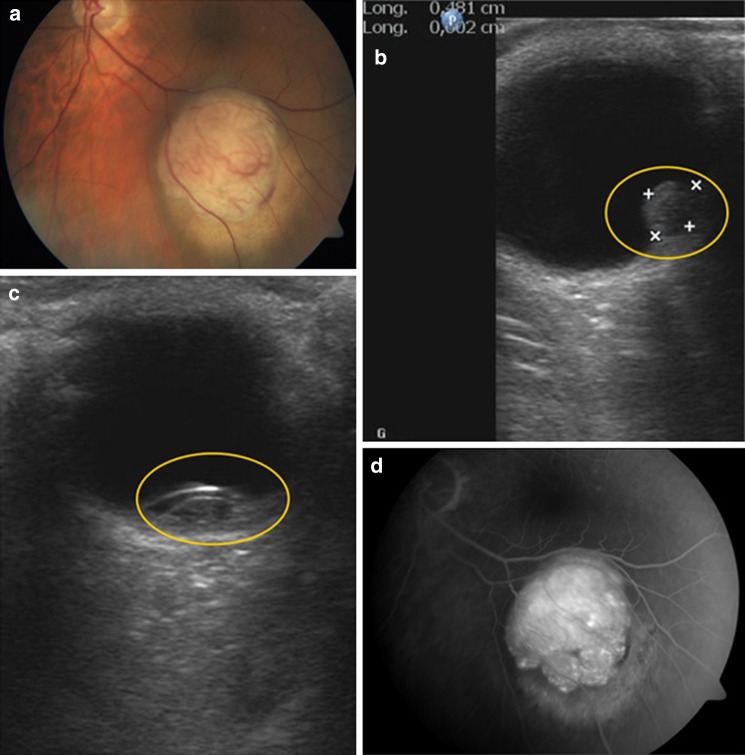
Fig. 7.
a Ophthalmoscopic image of choroidal amelanotic melanoma involving the lower temporal quadrant of the eye. b Corresponding ultrasonography image of choroidal amelanotic melanoma. c Corresponding ultrasonography image of choroidal amelanotic melanoma (different projection). d Corresponding angiography with fluorescein
Benign melanocytic tumors include nevi and melanocytomas. Like a melanoma, the pigmentation of a nevus can range from no pigmentation (amelanotic) to deep brown pigmentation (melanotic). A melanocytoma typically is heavily pigmented. They, too, have a dome-shaped configuration but, in contrast to melanoma, are highly reflective and do not have internal vascularity (Fig. 8a, b). Unfortunately, small melanomas may show an absence of low internal reflectivity, and, consequently, it may be difficult to differentiate a small benign lesion from a similarly sized malignant one.
Fig. 8.
a Ophthalmoscopic image of a benign melanocytic lesion overlying to the optic nerve. b Corresponding ultrasonography image of benign melanocytic lesion
Drusen are calcified plaques within the optic disc. They are usually bilateral and asymptomatic, but they may cause atrophy of the optic nerve. Hyperechoic lesions at the papilla with acoustic shadowing are seen at US. The presence of calcifications and their location are the clues to the diagnosis [1] (Fig. 9a, b). Although the presence of drusen is common in older people, in our experience we detected this disease primarily in young people (75 %).
Fig. 9.
a Drusen of the optic nerve. b Bilateral drusen of the optic nerve in a young patient
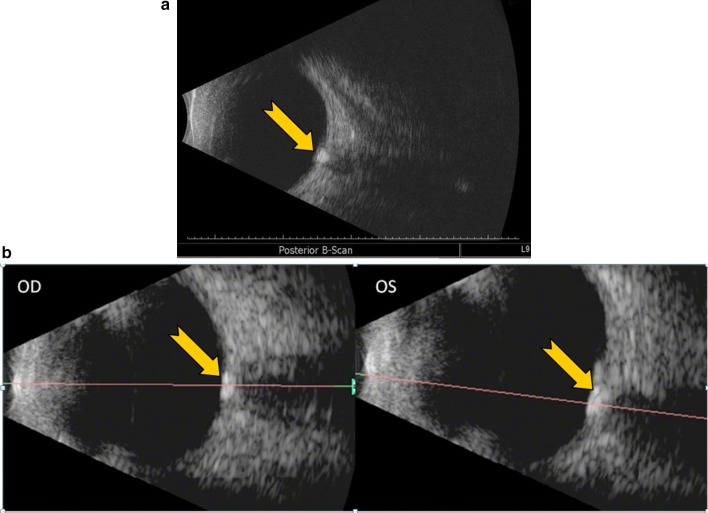
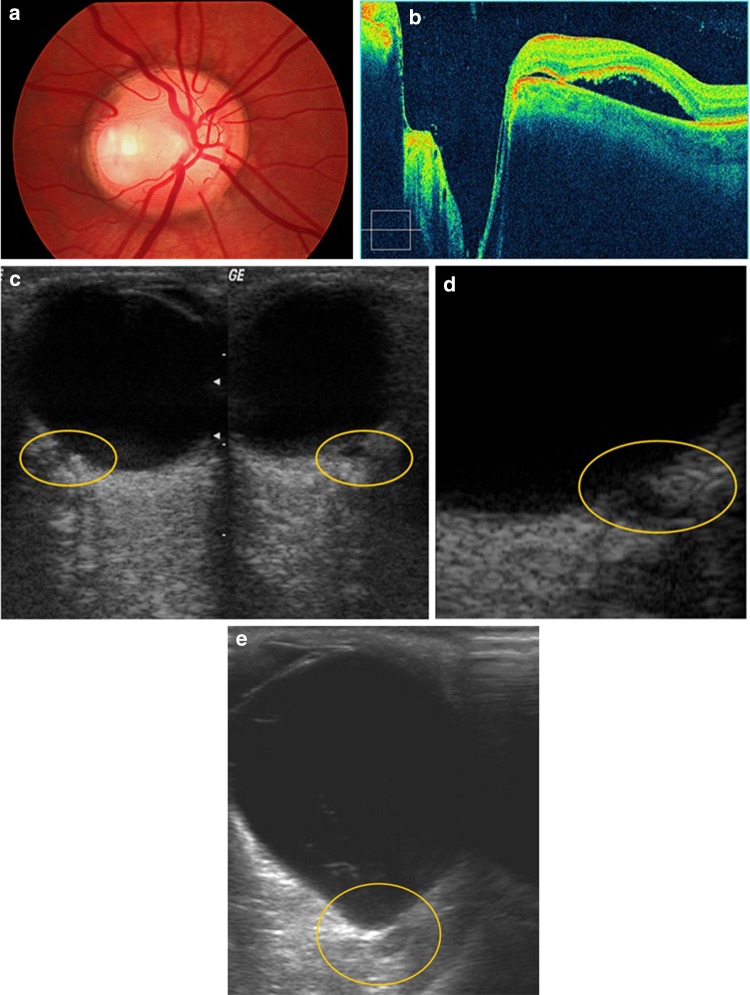
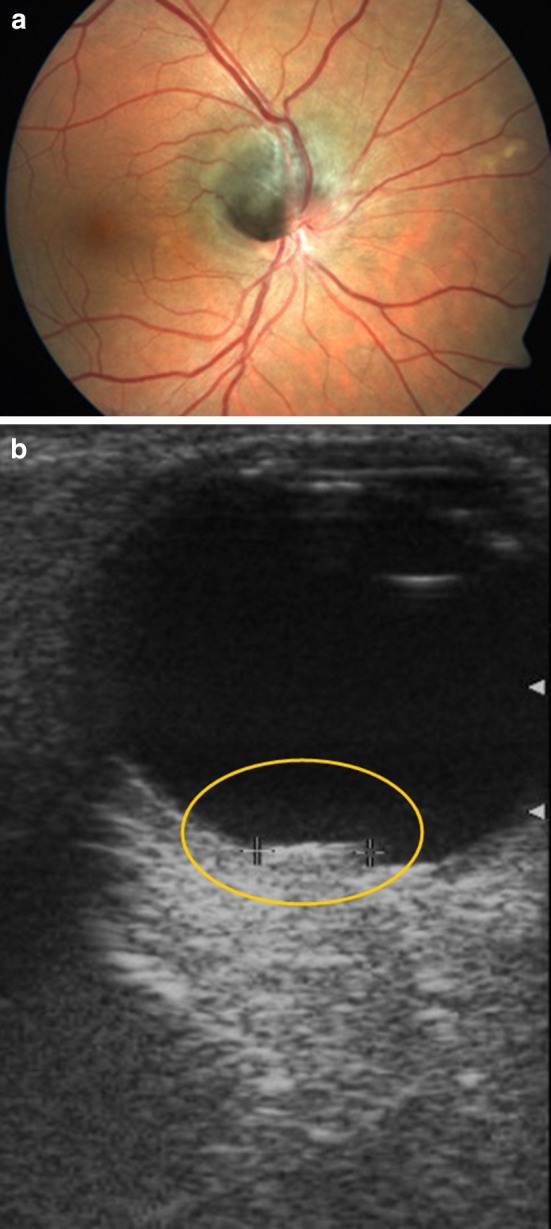
A coloboma of the optic nerve head involves a congenital defect in its structure occurring as a result of malclosure of the ocular fissure (Fig. 10a). At US, a defect in the optic disc and a papillary excavation are seen (Fig. 10b–e). It may be mild, in which case there is a defect in the optic nerve substance, usually inferiorly. This defect may be more extensive and involve the juxtapapillary choroid and retina. It may be associated with a pit deformity and with a juxtapapillary staphyloma. This latter term refers to an outpouching of the ocular wall around the optic nerve head. In our study, four juxtapapillary colobomas were demonstrated with one of them not known. In the other three cases, US helped to quantify the level of excavation.
Fig. 10.
a Ophthalmoscopic image of a coloboma of the optic nerve. b Optical coherence tomography (OCT) image of a coloboma of the optic nerve. c Ultrasonography image of a bilateral coloboma of the optic nerve. d Detail of the previous image. e Optic nerve coloboma associated with myopic staphyloma
Vogt–Koyanagi–Harada (VKH) disease is a rare multisystem disorder that affects the eye, inner ear, skin and meninges, with granulomatous appearance. The typical ocular manifestations are severe bilateral panuveitis with iridocyclitis, serous retinal detachment, diffuse choroidal swelling and optic disc hyperemia (Fig. 11a). These findings are usually bilateral, but the severe forms may be asymmetric [9]. Ultrasonographic imagery displays the lobular nodular thickening of the posterior ocular wall and the mixed detachments of the ocular membranes due to the inflammatory granulomatous lesions (Fig. 11b). Angiography shows the typical a retinal nodular enhancement (Fig. 11c).
Fig. 11.
a Ophthalmoscopic image of serous retinal detachment in Vogt–Koyanagi–Harada disease. b Ultrasonographic image in Vogt–Koyanagi–Harada syndrome. c Fluorescein angiography in Vogt–Koyanagi–Harada disease
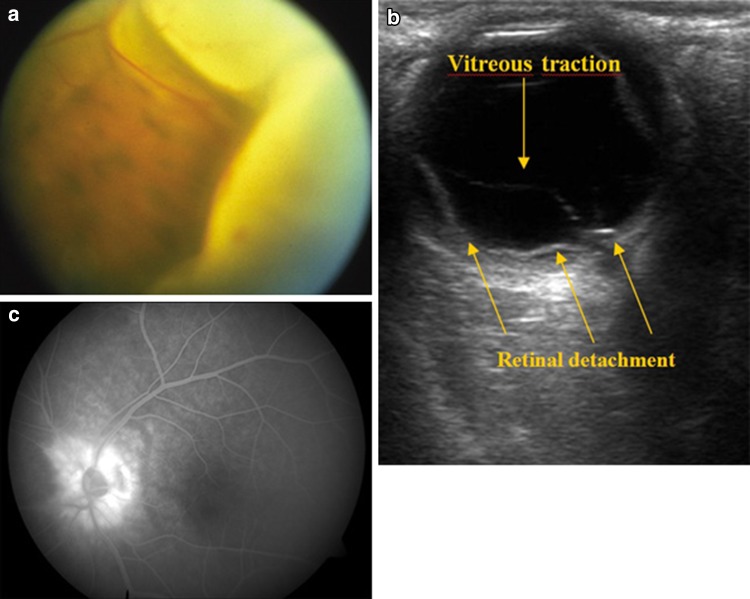
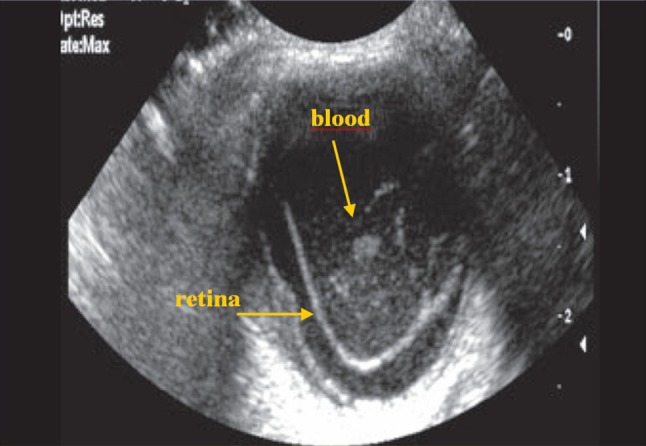
Retinal detachment (RD) is usually due to a break or tear in the retina; it may also be caused by vitreoretinal traction due to contracting membranes or because of subretinal exudates. The detached retina is usually attached to the firm anchoring points of the ora serrata anteriorly and the optic nerve head posteriorly and, consequently, a total RD shows a funnel shape [4] (Fig. 12).
Fig. 12.
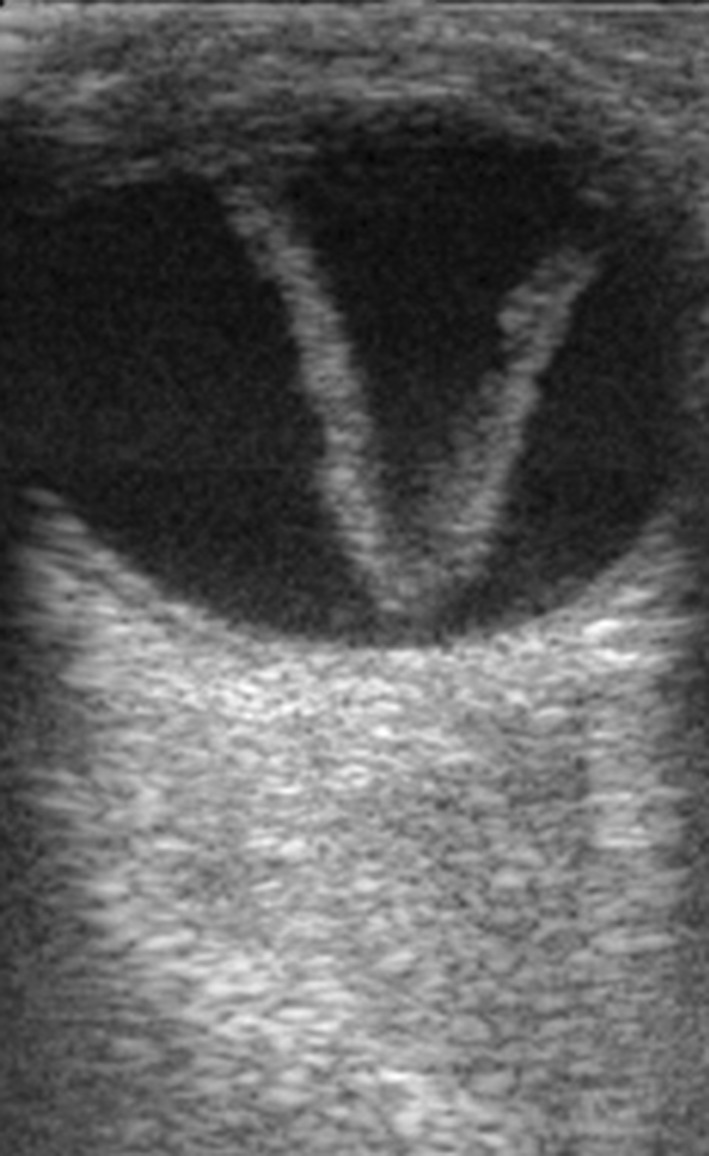
Total retinal detachment showing the typical “funnel shape”
Dynamic scan may reveal an undulating motion of the retinal membrane, particularly in a recent RD. RD can be acute or chronic, total or partial (Fig. 13a, b).
Fig. 13.
a Ophthalmoscopy image of a recent partial retinal detachment. b Color retinography of a total retinal detachment. c Angiography of the patient with retinal detachment with some enhancing areas suspecting a neoplastic lesion below causing detachment. d Ultrasonography showing choroidal melanoma associated with retinal detachment. e Ultrasonography in retinal detachment with no underlying cause
In acute RD the membrane is thin and mobile. Over time the membranes become thicker and echogenic, and with eye movements become rigid. Arterial and venous flows can be seen inside. There are three types of RD, depending on the underlying mechanism: rhegmatogenous, or retinal tearing; tractional, or separation of the retinal layer due to tugging by vitreous membranes; and exudative, in which blood, fluid, or a lesion is present in the subretinal space. In the presence of RD, the sub-retinal space and vitreous should always be examined because they may contain blood, exudative fluid, or tumor, thus providing the cause of the detachment, a determination that is usually not possible with ophthalmoscopy (Fig 13c) [1].
In some patients with partial RD, the request for US was to rule out a neoplasm causing detachment (Fig. 13d, e).
Choroidal detachment is caused by accumulation of fluid in the potential suprachoroidal space, which is located between the choroid and sclera and extends from the ora serrata to the optic disc, but the choroid is fixed to the sclera by vortex veins. At US, the bands visible in the choroidal detachment are typically thick and rigid, convex (in obtuse angle), and not “anchored” on the optic disc but at the level of vortex veins. Arterial flow can be seen in the thickness of these membranes (Fig. 14a, b).
Fig. 14.
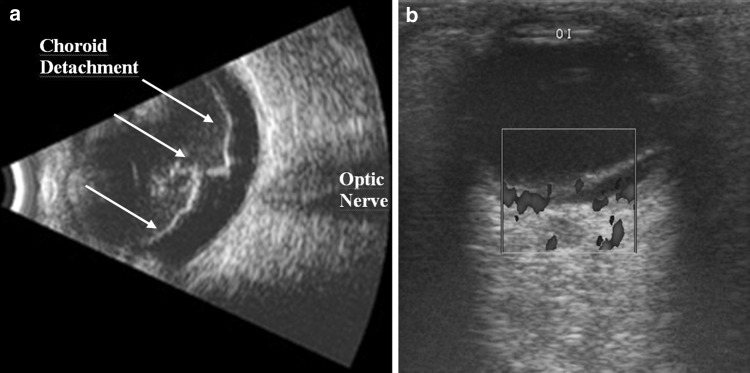
a Choroidal detachment, then area of the detachment is not “anchored” to the optic nerve. b Doppler study revealed arterial flow in the membrane
In our experience, most cases (75 %) of choroidal detachment were observed to be associated with retinal detachment (Fig. 15).
Vitreous detachment is usually seen in elderly individuals. It results from gel liquefaction and collection of fluid in the subvitreal space, which in turn results in vitreous detachment. It is seen frequently in cataractous eyes on B-scan. The posterior vitreous detachment or hyaloid detachment appears as avascular membranes and reduced volume of vitreous gel [4] (Fig. 16a, b).
With very low echogenicity that also exhibits a typical fluid movement when the patient performs eye movement (Fig. 16c). Vitreous detachment can be observed either associated or not with hemovitreous.
Fig. 15.
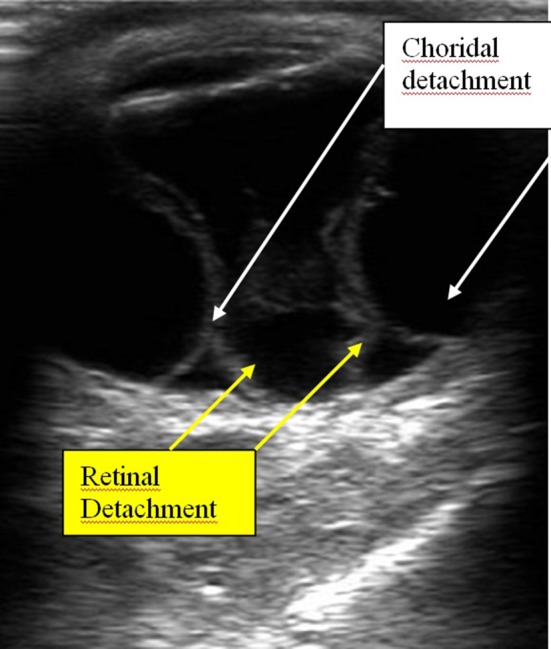
Mixed retinal and choroidal detachment. Multiple membranes suggesting mixed detachment: retinal and choroidal
Fig. 16.
a Posterior vitreous detachment: no blood flow into the membrane. b Posterior vitreous detachment with vitreous opacities. c Posterior vitreous detachment with similar curve as the posterior ocular wall. It is associated with hemovitreous
Discussion
Although clinical examination and ophthalmoscopy are the basis of diagnosis in most patients with eye disease, in many cases, especially when clinical examination of the ocular fundus is difficult, ultrasound is an important tool. In addition to its specific role in selected cases, ultrasound is a safe technique, cheaper and more affordable compared to other techniques that would also provide good data (such as optical coherence tomography, CT, or MRI) [4]. Ultrasonography does not involve the contraindications that may make other techniques more expensive and less accessible, such as MRI (presence of metallic items, claustrophobia, etc.) or optical coherence tomography (although it has some specific indications, especially in optic nerve diseases, due to its high spatial resolution, the technique is less more affordable than ultrasound). Contraindications for ocular US are rare; the main contraindication is suspected ocular globe rupture in patients with trauma or patients who recently underwent surgery, because it may cause extrusion of ocular contents [1].
In our hospital, thanks to close cooperation between the Ophthalmology and Radiology Units, many patients benefit from ultrasound examinations performed by trained radiologists. In our experience disorders of the posterior layers of the eyeball were the diseases detected with greater frequency (20 cases). However, sonography was revealed to be an important adjuvant in detecting other groups of ocular diseases, such as cataracts, lesions of the anterior chamber, hemovitreous, neoplastic lesions, macular degenerations, congenital diseases and inflammatory pathologies.
Therefore, we consider scan ophthalmic ultrasonography to be an important adjuvant for the clinical assessment of various ocular and orbital diseases. With understanding of the indications for ultrasonography and proper examination technique, one can gather a vast amount of information not possible with clinical examination alone. In addition to the usual A-mode technique (pen-probe US) performed by ophthalmologists, the B-mode technique can provide a good anatomical background and the Doppler tools are essential in confirming several diseases like choroidal detachment, melanoma vs. melanocytoma, and arterial occlusion. The A-mode technique can be used for IOL (intraocular lens) calculation in cataract surgery and for differential diagnosis in suspected melanoma, owing to its own typical ecographic pattern.
However, B-mode is the most used technique because it provides a good sensitivity and specificity, even if it’s operator-dependent. B-mode ecography is required every time the vitreous chamber and the retina are not visible; for example, in cases of very mature cataracts, hemovitreous, corneal opacities, blood or pus in the anterior chamber (traumas, herpes keratitis, endophthalmitis) and lesions of uncertain nature for a differential diagnosis. Sometimes B-mode ecography can be useful for better characterization of a lesion of the posterior segment of the eye, such as retinal detachment, partial hemovitreous, diabetic retinopathy, suspected melanomas, and foreign bodies (especially for metallic bodies where the MRI can’t be used).
In cases of facial or cranial trauma (especially of the frontal or parietal region), B-mode ecography and CT can be used together to detect lesions of the eye and orbit. Patients with retinal/choroidal detachment and/or associated masses, in whom findings on conventional grayscale and Doppler modes are equivocal, can be submitted to contrast-enhanced ultrasound (CEUS). CEUS can be used as a problem-solving technique when conventional ultrasound modes are not diagnostic for retinal/choroidal detachment and when intraocular lumps cannot be characterized as tumor or non-tumor masses on conventional modes [11].
Conflict of interest
Gerardo Dessi, Eduardo Ferrer Lahuerta, Fabrizio Giorgio Puce, Luis Humberto Ros Mendoza, Teseo Stefanini, Ilan Rosenberg, Alberto Del Prato, Michela Perinetti, Alessandro Villa declare that they have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). All patients provided written informed consent to enrolment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Human and animal studies
The study conducted in accordance with all institutional and national guidelines for the care and use of laboratory animals.
References
- 1.Lorente-Ramos RM, Armán JA, Muñoz-Hernández A, Gómez JM, de la Torre SB. US of the eye made easy: a comprehensive how-to review with ophthalmoscopic correlation. Radiographics. 2012;32(5):E175–E200. doi: 10.1148/rg.325115105. [DOI] [PubMed] [Google Scholar]
- 2.Dimitrova G, Kato S. Color doppler imaging of retinal diseases. Surv Ophthalmol. 2010;55(3):193–214. doi: 10.1016/j.survophthal.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 3.Cejas C, Benavidez S, Sanguinetti. MM, et al. (2004) Ecografía y doppler ocular. Ediciones J pp 35–62
- 4.Aironi VD, Gandage SG. Pictorial essay: B-scan ultrasonography in ocular abnormalities. Ind J Radiol Imag. 2009;19:109–115. doi: 10.4103/0971-3026.50827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smirniotopoulos JG, Bargallo N, Mafee MF. Differential diagnosis of leukokoria: radiologic-pathologic correlation. Radiographics. 1994;14(5):1059–1079. doi: 10.1148/radiographics.14.5.7991814. [DOI] [PubMed] [Google Scholar]
- 6.Bord SP, Linden J. Trauma to the globe and orbit. Emerg Med Clin North Am. 2008;26(1):97–123. doi: 10.1016/j.emc.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Silverman RH. High-resolution ultrasound imaging of the eye: a review. Clin Experiment Ophthalmol. 2009;37(1):54–67. doi: 10.1111/j.1442-9071.2008.01892.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fielding JA. Pictorial review ocular ultrasound. Clinic Radiol. 1996;51:533–544. doi: 10.1016/S0009-9260(96)80131-0. [DOI] [PubMed] [Google Scholar]
- 9.Agrawal A, Biswas J. Unilateral Vogt-Koyanagi-Harada disease: report of two cases. Middle East Afr J Ophthalmol. 2011;18(1):82–84. doi: 10.4103/0974-9233.75898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bedi GB, Gombos DS, Ng CS, Singh S. Sonography of the eye. AJR. 2006;187:1061–1072. doi: 10.2214/AJR.04.1842. [DOI] [PubMed] [Google Scholar]
- 11.Bertolotto M, Serafini G, et al. The use of CEUS in the diagnosis of retinal/choroidal detachment and associated intraocular masses -preliminary investigation in patients with equivocal findings at conventional ultrasound. Ultraschall Med. 2014;35(2):173–180. doi: 10.1055/s-0032-1330321. [DOI] [PubMed] [Google Scholar]