Introduction
The commonly encountered osteochondroma is a benign tumour that usually arises from the metaphyseal region of long bones, demonstrates mature bone with a cartilaginous cap, a continuation of the medullary cavity with that of the long bone and grows away from the joint till achievement of skeletal maturity. Extraskeletal para-articular osteochondroma, also known as intracapsular chondroma, arises from the capsule and/or connective tissue adjacent to the capsule due to osteocartilaginous metaplasia and occurs most frequently around the knee, particularly the infrapatellar fat pad of Hoffa.1 Extraskeletal para-articular osteochondroma is a rare entity with only 23 cases reported till 19972 and about 40 cases by 2006.3 This article reports another giant intra-articular extrasynovial osteochondroma of the knee which was surgically excised and discusses the clinical and imaging features, the histology and purported pathogenesis, and the differential diagnosis.
Case report
A 43-year-old male soldier presented with the complaints of pain and bony swelling in his left knee for a duration of about 6 months. The pain was moderate in intensity and usually followed strenuous physical activity. The first episode occurred 6 months back following long-distance running. There was no history of acute direct trauma. Since then, the pain was recurrent with intervening asymptomatic periods. The pain was relieved by rest and anti-inflammatory medication. The patient also noticed clicking sounds during movements at the knee joint. No other comorbid conditions were present.
Physical examination of the patient revealed a non-tender, Bony-hard mass, measuring approximately 3.0 cm–4.0 cm, in the left knee just inferior to the patella. There were no signs of superficial bruise or injury marks about the knee. Terminal knee flexion was restricted and also elicited pain. Clinical tests for meniscal and cruciate ligament integrity did not reveal any abnormality.
Plain radiographs of the knee revealed a sharply marginated, corticated, ovoid bony mass inferior to the left patella in the Hoffa's fat pad, asymmetrically off-midline laterally. The mass exhibited internal bony trabeculae (Fig. 1). There was no osseous continuity with the patella, femur, tibia or fibula. Subsequently, a non-contrast enhanced Magnetic Resonance Imaging (MRI) was performed which revealed a 26.0 mm × 43.0 mm × 37.0 mm (AP × TR × CC) ovoid lesion located inferolateral to the patella within the Hoffa's fat pad. The lesion revealed a thin uniform cortical rim (hypointense on all sequences). The internal matrix was hyperintense to muscle on T1-weighted images (similar to the marrow signal intensity in the adjoining bones) and hyperintense on T2-weighted and PD fat saturated images (hyperintense to the marrow in the adjoining bones). A smooth well-delineated rim of soft tissue (hyperintense on T2-weighted and PD fat saturated images) measuring 4.0 mm in thickness, suggestive of cartilage (Fig. 2a–c) was present. The menisci and cruciate ligaments were normal. There was no evidence of synovial thickening or haemorrhage. On the basis of these imaging findings, an impression of intra-articular extrasynovial osteochondroma was made.
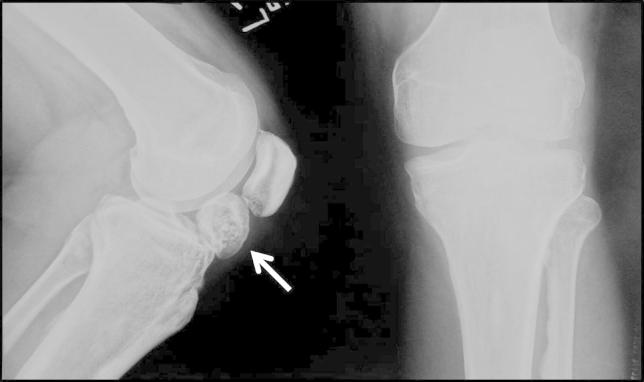
Fig. 1.
Radiograph of the left knee (lateral and AP views) reveal a well-corticated bony mass (arrow) located in the infrapatellar fat pad. Bone trabeculae are noted within the mass. There is no continuity with the adjoining bones.
Fig. 2.
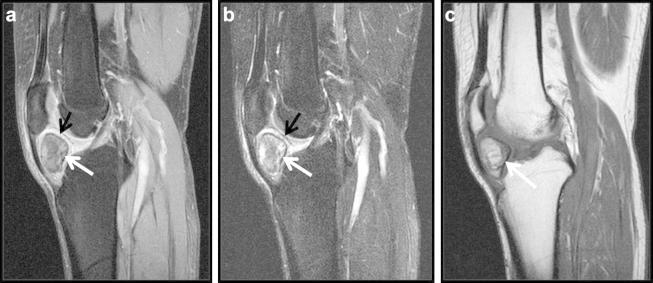
(a–c). The panel shows (a) sagittal T2-weighted (TR/TE = 4150/87), (b) PD (TR/TE = 4150/14) fat saturated and (c) sagittal T1-weighted (TR/TE = 495/12) MRI images. A sharply marginated mass is noted in the infrapatellar fat which follows similar marrow signal intensity as the adjoining bones. A smooth thin hypointense rim (white arrows) of cortex is noted on all sequences. A peripheral rim of cartilage (black arrows) is noted outside the cortex in the T2- and PD-weighted images.
The mass was excised by an anterior approach. Macroscopic examination revealed a bony hard extrasynovial mass (Fig. 3). Histopathology showed an outer layer of hyaline cartilage without significant chondrocyte atypia and an inner region of bone trabeculae formed by endochondral ossification (Fig. 4). These features were consistent with extraskeletal para-articular osteochondroma.
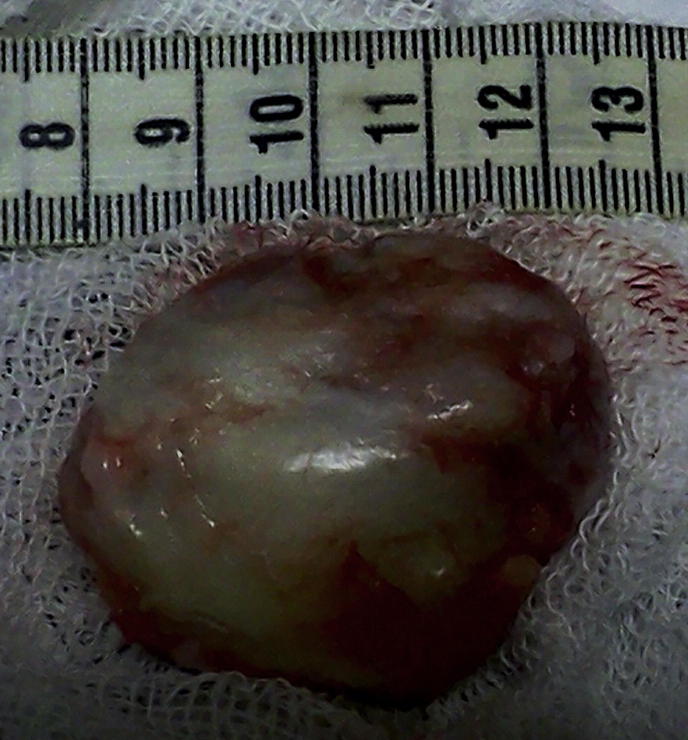
Fig. 3.
Gross specimen reveals a large bony mass covered by fat.
Fig. 4.
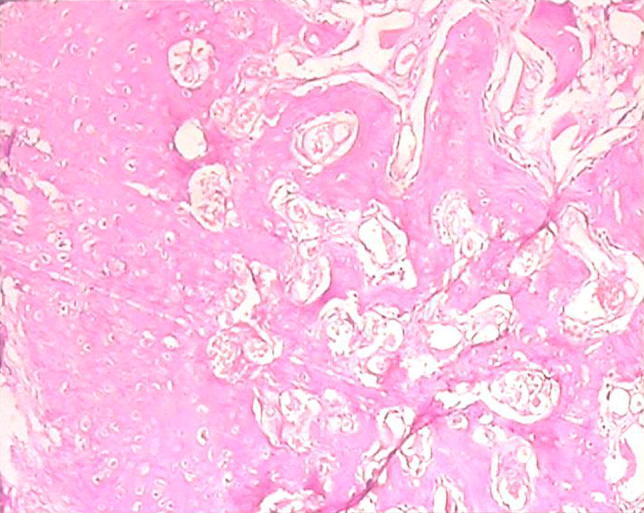
Histopathology appearance (Haematoxylin-Eosin): a cap of mature hyaline cartilaginous tissue was noted. The centre of the lesion, beneath the cartilaginous cap is composed of mature bone trabeculae containing fatty bone marrow. Original magnification: ×40.
Discussion
Osteochondromas are common bone tumours and are hyperplastic–dysplastic developmental anomalies of the growth plate rather than true neoplasms. They constitute 20%–50% of all benign bone tumours and 10%–15% of all bone tumours.4 There are three variants of extraskeletal chondromas – soft tissue chondromas, synovial chondromatosis and para-articular chondromas.1 Most of the soft tissue chondromas arise in the hands and feet,5 however soft tissue chondromas have also been reported in the buttock6 and nape of the neck.7 Extraskeletal chondromas or osteochondromas may occur in patients at any age, although they are most commonly encountered between the ages of 30 and 60 years.5 Para-articular chondromas, also known as intracapsular chondromas, arise from the capsule and/or connective tissue adjacent to the capsule due to cartilaginous metaplasia.8 If the metaplasia progresses to ossification, the term para-articular osteochondroma may be used. Most of these entities arise around the knee though they have been noted in the vicinity of the elbow, hip, and ankle.1,9 Within the knee, the most common site is the infrapatellar fat pad of Hoffa. Reith et al proposed the following criteria for a lesion to be diagnosed as para-articular osteochondroma: (a) the lesion presents as a single, dominant mass, both radiographically and grossly; (b) the mass consists histopathologically of both bone and cartilage, organized in a manner similar to conventional osteochondromas; and (c) the lesion is not intra-articular, that is, it does not arise within the synovial lining of a joint.2 The term ‘giant intra-articular extrasynovial osteochondroma’ was first used by Maio et al.9 There may be dense fibrous attachment of these lesions to the tissues around the tibial plateau or the coronary ligament of the meniscus.8
On lateral radiographs and computerized tomography (CT), foci of calcification to rounded ossifying masses are seen in the Hoffa's fat pad. Remodelling of the anterosuperior cortex of the tibia may be present. MRI reveals obliteration of the normal fat signal intensity in the infrapatellar fat pad by a central or eccentric rounded or lobulated mass. These masses are predominantly isointense with muscle on T1-weighted images with areas of marrow signal intensity in those cases where ossification is present. Administration of contrast reveals peripheral enhancement of the cartilage. On T2-weighted and STIR (short tau inversion recovery) images the masses appear heterogeneously hyperintense, the degree of heterogeneity depending on the extent of calcification.1,8
The pathogenesis of this lesion is controversial. It is generally considered to originate from a cartilaginous metaplasia of the articular and para-articular connective tissue. Apart from primary metaplasia, the proposed triggers for metaplasia include trauma and chronic impingement of the infrapatellar fat pad.9 Grossly, these tumours are characterized by a solitary mass composed of multiple osteochondral nodules. Histologically, these entities consist of peripheral cartilaginous areas with central lamellar, trabecular bone. Endochondral ossification is usually present at the interface between the cartilage and bone. The overall configuration of these lesions is similar to a conventional osteochondroma; however, the quality of the cartilaginous matrix seems to vary more than in conventional osteochondroma, which has a pure hyaline cartilage cap.8 These lesions are not known to recur after complete excision.2
Radiologically, para-articular osteochondromas must be considered in the differential diagnosis of radiological calcified/ossified soft tissue lesions about the Hoffa's fat pad, such as old haematomas, calcifying bursitis, tumoral calcinosis, myositis ossificans, crystal deposition disease, calcified synovial sarcomas, primary synovial chondromatosis, and synovial chondrosarcoma.
Conclusion
Giant intra-articular extrasynovial osteochondroma is a very rare entity which arises most commonly around the knee joint, particularly the infrapatellar fat pad of Hoffa by osteocartilaginous metaplasia. The imaging appearances of this entity are often diagnostic, however an integrated radio-pathologic diagnosis may help to distinguish this entity from other lesions arising in the area. Surgical excision is adequate management and these masses are not known to recur.
Conflicts of interest
All authors have none to declare.
References
- 1.Helpert C., Davies A.M., Evans M., Grimer R.J. Differential diagnosis of tumours and tumour-like lesions of the infrapatellar (Hoffa's) fat pad: pictorial review with an emphasis on MR imaging. Eur Radiol. 2004;14:2337–2346. doi: 10.1007/s00330-004-2491-1. [DOI] [PubMed] [Google Scholar]
- 2.Reith J.D., Bauer T.W., Joyce M.J. Paraarticular osteochondroma of the knee. Report of two cases and review of literature. Clin Orthop. 1997;334:225–232. [PubMed] [Google Scholar]
- 3.Oliva F., Marconi A., Fratoni S., Maffulli N. Extra-osseous osteochondroma-like soft tissue mass of the patello-femoral space. BMC Musculoskelet Disord. 2006;7:57. doi: 10.1186/1471-2474-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH. From the archives of the AFIP. Imaging of osteochondroma: variants and complications with radiologic-pathologic correlation. Radiographics. 2000;20:1407–1434. doi: 10.1148/radiographics.20.5.g00se171407. [DOI] [PubMed] [Google Scholar]
- 5.Kransdorf M.J., Meis J.M. From the archives of the AFIP. Extraskeletal osseous and cartilagineous tumors of the extremities. Radiographics. 1993;13:853–884. doi: 10.1148/radiographics.13.4.8356273. [DOI] [PubMed] [Google Scholar]
- 6.Lim S.C., Kim Yun S., Kim Young S., Moon Y.R. Extraskeletal osteochondroma of the buttock. J Korean Med Sci. 2003;18:127–130. doi: 10.3346/jkms.2003.18.1.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh R., Sharma A.K., Magu N.K. Extraskeletal osteochondroma in the nape of the neck: a case report. J Orthop Surg. 2006;14(2):192–195. doi: 10.1177/230949900601400217. [DOI] [PubMed] [Google Scholar]
- 8.Mulcahy H., Hoch B. An extraskeletal para-articular osteochondroma of Hoffa's fat pad. Radiol Case Rep. 2010;5:420. doi: 10.2484/rcr.v5i4.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maio F.D., Bisicchia S., Potenza V., Caterini R., Farsetti P. Giant intra-articular extrasynovial osteochondroma of the knee: a report of two cases. Open Orthop J. 2011;5:368–371. doi: 10.2174/1874325001105010368. [DOI] [PMC free article] [PubMed] [Google Scholar]