Introduction
Iris cysts are not uncommonly seen entities in clinical practice. They could be primary or secondary to some other cause.1–5 Generally primary iris cysts do not require any treatment if small and without complications. However, stromal variety of iris cysts, which are further rare, demand intervention as they tend to enlarge. A thorough slit lamp microscope examination with Ultrasonic Bio-Microscopy was done to clinch the diagnosis. The case was managed successfully without recurrence and complications with Nd YAG laser cystostomy under steroid and anti-glaucoma coverage. This report aims to document and familiarise ophthalmologists with a rare ocular pathology and its management.
Case report
A 49 years old female patient reported to our OPD with insidious onset painless diminution of vision in left eye of six months duration. There was no history of redness, flashes, floaters or diplopia. She did not give any history of ocular injury, topical medication or any history suggestive of neurological illness. There was no history of previous ocular surgery.
Ocular examination revealed a visual acuity of 6/6 in right eye and perception of Hand Movements Close to Face with accurate Projection of Rays in left eye. There was no bony deformity in the orbital margins. Lids and adnexa were also normal. She was orthophoric with ocular movements full and free in all cardinal directions of gaze. Detailed ocular examination with Slit Lamp Bio-microscope revealed a normal right eye. A large smooth surfaced, semi-transparent opalescent cystic mass with clear fluid, obscuring the visual axis was seen in the temporal part of the Anterior Chamber (AC) of the left eye. Pigmentary markings were also noted on the surface. There was no change with decubitus suggesting that the cyst was fixed. The pupil was pushed posteriorly by large iris cyst. There were no features suggestive of previous ocular injury or surgery. Fundus examination could not be done (Figs. 1 and 2).
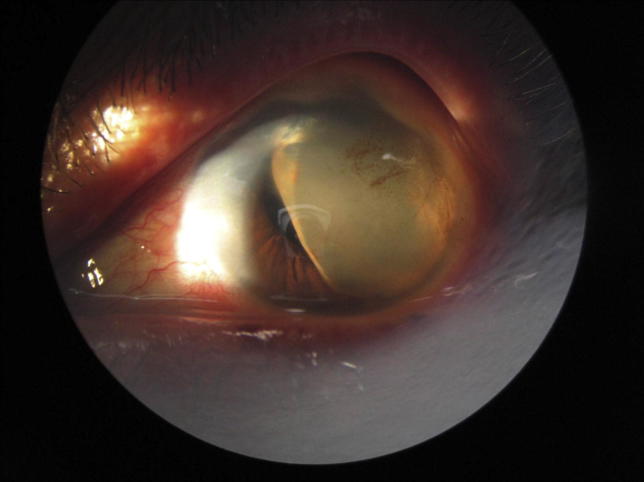
Fig. 1.
A smooth surfaced large stromal iris cyst occupying anterior chamber.
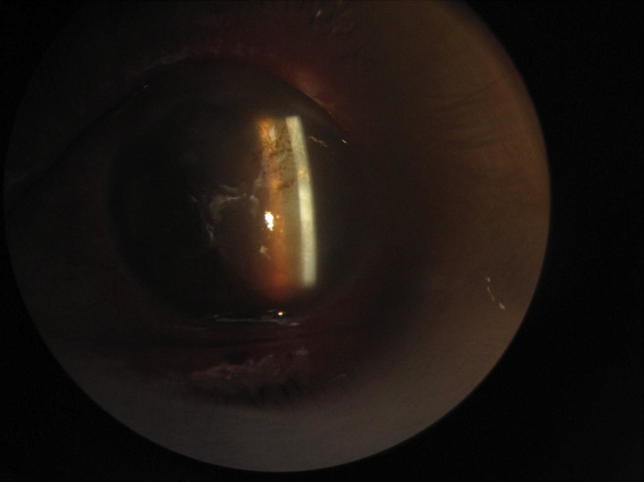
Fig. 2.
Iris cysts in anterior camber with pigment markings on the anterior surface.
Ocular ultrasound AB scan did not reveal any abnormality in posterior segment in both the eyes. Ultra Bio-Microscopic scan (UBM) done revealed a smooth, thick walled cystic swelling arising from the iris and occupying the temporal part of the anterior chamber. The lumen of the cyst was anechoic. (Fig. 3). MR scan of the brain and orbit to rule out any similar lesion was non-contributory. There was no rise in intraocular tension. Routine blood examination and blood sugar level were normal. Microscopic examination of the stool on three consecutive days was also normal. The patient was then labelled as a case of Primary Iris Cyst of the left eye. Nd YAG cystostomy was performed under one week peri-procedural coverage of systemic and topical steroids and anti-glaucoma medication (Fig. 4). Immediate regression in the size of cyst was noted with full recovery of visual acuity to 6/6 with clearing of pupil was noted. No post-procedural reaction in the AC or rise in IOP was noted for one week. Patient was so happy with the treatment that she refused any surgical intervention. Follow up of the case after a month and thereafter six monthly for two years has shown no recurrence.
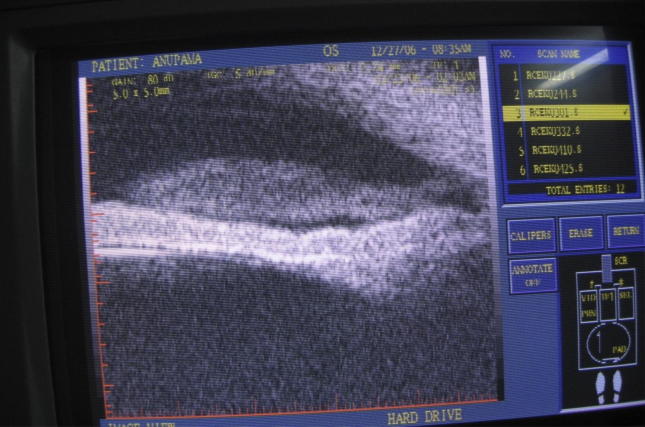
Fig. 3.
UBM scan showing a thick walled cyst arising from the anterior surface of the iris.
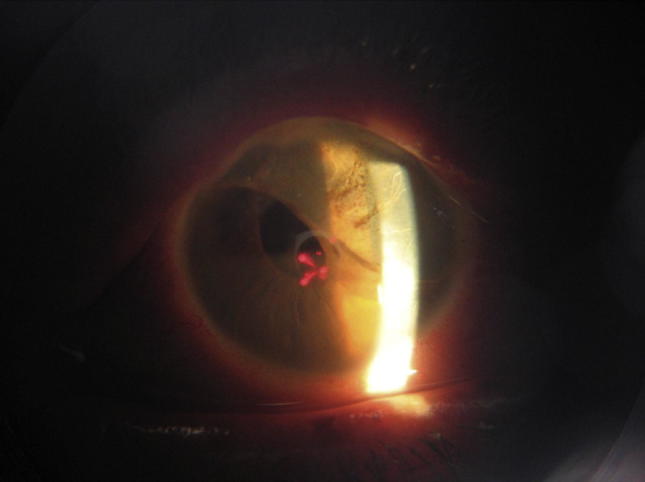
Fig. 4.
Laser cystostomy leading to immediate regression in the size of the cyst with clearing of pupillary axis.
Discussion
Iris cysts have been classified into primary and secondary types (Table 1). Primary iris cysts which commonly arise from the posterior pigment epithelium of the iris are more common in children as compared to secondary iris cysts. In a large series of 251 cases of iris cysts in children less than 20 years of age, primary and secondary iris cyst have been reported in 53 and 4 cases respectively. Of the 53 primary iris cysts, 44 were pigment epithelial and nine were stromal. The peripheral pigment epithelial cyst accounted for 34 cases or 59% of all childhood iris cysts. They are more common in girls and most commonly diagnosed in the teenage years. The primary iris cysts are benign, usually stationary or even regress in some cases and do not require any intervention.1However very rarely they enlarge, occupy anterior chamber and have a thick walled clear lumen. When they obscure pupillary axis or cause pressure symptoms, surgery or by Laser cystostomy as done in our case is required.1,6,7 An adequate steroid cover and anti-glaucoma measure should be considered to prevent any Anterior Chamber reaction.
Table 1.
Classification of iris cysts.
|
Secondary iris cysts develop due to trauma, malignancies such as melanoma or medulloepithelioma and long-term topical instillation of pilocarpine and/or prostaglandin analogues in the management of glaucoma. Parasitic infestation such as echinococcosis and cysticercosis may also sometimes present as cysts in anterior chamber of eye.8 In addition to complete removal of iris cyst, iridocyclectomy, lensectomy, vitrectomy, penetrating keratoplasty and intraocular (IOL) removal has been documented and may be needed.9 Care is needed to prevent any spillage of the contents of the cysts to avoid toxic reactions.8,10,11
Conflicts of interest
All authors have none to declare.
References
- 1.Shields Jerry A., Shields Carol L., Lois Noemi, Mercado Gary. Iris cysts in children: classification, incidence and management. Br J Ophthalmol. 1999;83:334–338. doi: 10.1136/bjo.83.3.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lois N., Shields C.L., Shields J.A. Primary cysts of the iris pigment epithelium: clinical features and natural course in234 patients. Ophthalmology. 1998;105:1879–1885. doi: 10.1016/S0161-6420(98)91034-X. [DOI] [PubMed] [Google Scholar]
- 3.Lois N., Shields C.L., Shields J.A. Primary iris stromal cysts: a report of 17 cases. Ophthalmology. 1998;105:1317–1322. doi: 10.1016/S0161-6420(98)97041-5. [DOI] [PubMed] [Google Scholar]
- 4.Shields J.A., Eagle R.C., Jr., Shields C.L. Natural course and histopathologic findings of lacrimal gland choristoma of the iris and ciliary body. Am J Ophthalmol. 1995;119:219–224. doi: 10.1016/s0002-9394(14)73876-0. [DOI] [PubMed] [Google Scholar]
- 5.Shields J.A., Shields C.L. Melanocytic tumors of the iris. In: Shields J.A., Shields C.L., editors. Intraocular Tumors. A Text and Atlas. WB Saunders; Philadelphia: 1993. p. 65. [Google Scholar]
- 6.Bron A.J., Wilson C.B., Hill A.R. Laser treatment of primary ring-shaped epithelial iris cyst. Br J Ophthalmol. 1984 December;68(12):859–865. doi: 10.1136/bjo.68.12.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duan Xiaoming, Zhang Yanxia, Wang Ningli. Laser treatment to large iris cyst secondary to trabeculectomy. Can J Ophthalmol. 2007;42:316–317. [PubMed] [Google Scholar]
- 8.Shields J.A., Shields C.L., De Potter P. Free-floating cyst in the anterior chamber of the eye. J Pediatr Ophthalmol Strabismus. 1996;33:330–331. doi: 10.3928/0191-3913-19961101-12. [DOI] [PubMed] [Google Scholar]
- 9.Rishi Pukhraj, Rishi Ekta, Biswas Jyotirmay, Nandi Krishnendu. Clinical and histopathological features of posttraumatic iris cyst. Indian J Ophthalmol. 2008 Nov–Dec;56(6):518–521. doi: 10.4103/0301-4738.43383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naumann G.O.H., Rummelt V. Congenital nonpigmented epithelial iris cyst removed by block-excision. Graefes Arch Clin Exp Ophthalmol. 1990;228:392–397. doi: 10.1007/BF00927248. [DOI] [PubMed] [Google Scholar]
- 11.Naumann G.O.H., Rummelt V. Block excision of cystic and diffuse epithelial ingrowth of the anterior chamber. Arch Ophthalmol. 1992;110:223–227. doi: 10.1001/archopht.1992.01080140079031. [DOI] [PubMed] [Google Scholar]