Introduction
Refractive errors are one of the most common ophthalmologic problems. Implantable contact lens (ICL) implantation has received attention for its excellent and rapid visual and refractive results in eyes with high myopia. There are still concerns about complications such as anterior capsule opacity, cataracts,1,2 pupillary block glaucoma,3,4 chronic inflammation,5 pigmentary dispersion syndrome,6,7 and pigmentary glaucoma.8 We report an interesting case of a patient who had undergone ICL implantation presenting as a case of pupillary block glaucoma and how the patient was effectively managed.
Case report
A 23 years old male patient came to the eye opd with a chief complaint of sudden onset Diminution of Vision (DOV) in the left eye since 2 days. The DOV was associated with redness, pain & watering of left eye. Patient gave history of undergoing ICL implantation in both eyes 2 months back. Previous documents showed that the patient was a high myope and − 17 D STAAR ICL (overall diameter 12.5 mm, optic diameter 4.6–5.5 mm) was implanted in both eyes on the same day 2 months back in a private hospital. The vision recorded post ICl implantation was 6/6 in both eyes. Post operative period was uneventful.
There were no history of flashes, floaters, trauma or similar episodes in the past.
On examination – Distant visual acuity right eye – 6/6 unaided.
Distant visual acuity left eye − 6/36 unaided, no improvement with pinhole.
Right eye – examination of ant segment – lid and adnexa, conjunctiva were within normal limits, cornea-lustrous, anterior chamber – shallow grade II by Van Herrics, iris showed a LASER peripheral iridotomy at 10 o'clock which was patent, pupil was brisk. ICL in situ, lens was clear, gonioscopy – angle of anterior chamber grade II by Shaffer's grading.
Fundus examination showed presence of myopic changes.
IOP recorded by Goldmanns Applanaion Tonometer was 16 mm of Hg.
Left eye-Examination of anterior segment-lid and adnexa were within normal limits, conjunctiva showed circumciliary congestion. Cornea had microcystic edema along with corneal haze. The anterior chamber was shallow grade II (Van Herricks) cells ++, flare+ [Fig. 1], iris details hazily seen, pupil mid dilated non-reacting to light. Pigment was present on the anterior surface of the ICL [Fig. 2]. Lens appeared clear.
Fig. 1.
Shallow anterior chamber with cells and flare.
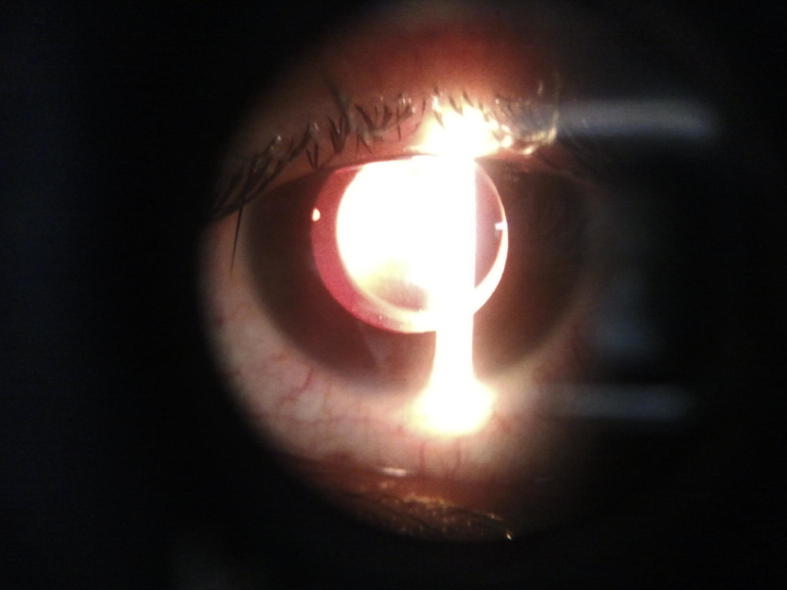
Fig. 2.
ICL seen on retroillumination, also note the mid dilated pupil not reacting to light.
On gonioscopy the details of the angle of anterior chamber of the left eye were not visualized due to the corneal edema.
Fundus Examination – Fundus glow was seen, optic disc details not clearly visualized due to media haze.
IOP was 70 mm of Hg by Goldmanns Applanation Tonometer.
Treatment
Patient was diagnosed as case of pupillary block glaucoma secondary to ICL implantation. The patient was admitted and started on intravenous mannitol 300 ml, oral acetazolamide 250 mg QID along with topical anti glaucoma medication (timolol 0.5%, brimonidine0.2%, dorzolamide 2% and pilocarpine 4%).
After 48 h, in spite of these medications the IOP in the LE was 52 mm of Hg and the pupil was mid dilated, not reacting to light. Patient was planned explantation of the ICL on the second day after effective IOP control was not achieved. Pre operatively mannitol 300 ml was given, and it was decided on the operation table to go in for a surgical peripheral iridectomy under topical anesthesia and monitor the IOP. Peripheral surgical iridectomy at 11'oclock was performed by entering into the same site of the main port incision which was used to implant the ICL (Fig. 3).
Fig. 3.
Intraoperative picture showing the conjunctival and circumciliary congestion.
First post operative day the IOP dropped to 21 mm of Hg. Patient was then taken off the parenteral and oral anti glaucoma medications but no rise in IOP was recorded. All the topical anti glaucoma medications were stopped from the 4th post operative day, patients IOP was 16 mm of Hg. Patient was discharged after 1 week with vision of 6/6 and an IOP of 14 mm of Hg in the left eye. Patient was called for weekly follow up for the next 2 months and IOP was closely monitored during this period. There was no record of raised IOP during the patients follow up (Fig. 4).
Fig. 4.
Patient on discharge from hospital the eye is quiet.
During the follow up period slit lamp biomicroscopy of left eye showed the absence of krukenberg spindle or iris transillumination defects. Gonioscopy revealed grade II angles by Shaffer's grading and absence of heavily pigmented trabecular meshwork. Fundus examination showed an optic disc which was normal with a healthy neuroretinal rim, CDR 0.4 and myopic changes similar to the right eye.
Discussion
Phakic Intraocular Lens (PIOL) for the correction of high myopia, and also for high hyperopia, have several potential advantages, including excellent refractive results, excellent stability of refraction, good quality of vision, preservation of accommodation, and reversibility.9–11
Currently, PIOLs are mainly useful in treating high myopia from −10.00 to −23.0 D and high hyperopia from +5.00 to +11.00 D in young patients.
General patient selection criteria for implanting PIOLs for myopia correction include: age between 22 and 45 years; stable high myopia between −10.00 and −23.00 D; unsuccessful attempt to wear contact lenses, and refusal to wear spectacles; normal anterior segment (no uveitis, cataract or glaucoma); anterior chamber depth (ACD) > 3.2 mm (measured from corneal epithelium); endothelial cell density >2300 cells/mm2; mesopic pupil diameter <6 mm; and normal peripheral retina.11–15
Contraindications for implanting myopic PIOLs include – ocular conditions such as corneal disease, especially endothelial cell counts below 2000 cells/mm2, glaucoma, cataract, atrophic iris disease, past history of retinal detachment.
The anterior segment anatomy should be adequate with an ACD of at least 2.8 mm from the endothelium (3.2 mm from corneal surface) to the lens capsule, and normal iris root configuration. Potential hazards of this procedure should be explained to the patient, and an informed consent is obtained before surgery.
Complications
ICL implantation has shown a low and non-progressive endothelial cell loss over time (5.5% at 2 years). Induced cataract has been reported between 1% and 7%, although some authors found lens opacities in 14.5%.16,17 Pigmentary dispersion syndrome has been reported in 2.2% of eyes at 12 months after ICL implantation, although a true pigmentary glaucoma is rare. Other sporadic complications include pupillary block and malignant glaucoma.
We experienced ICL induced pupillary block glaucoma in this case, a LASER Peripheral Iridotomy could not be performed as the beam of the Nd YAG LASER was not getting focused on the iris due to the corneal edema and the anterior chamber reaction. Also on reviewing literature there are reports of recurrent obstruction of LASER iridotomy sites which are induced by ICL implantation.18 During the patients follow up a partially patent LASER iridotomy was found at 10 o'clock in the left eye, which would have been the inciting factor for the pupillary block glaucoma to develop. Pigment Dispersion Syndrome (PDS) did come to our mind as a possible differential diagnosis or contributory factor but the absence of krukenberg spindle, iris transillumination defects and heavily pigmented trabecular meshwork went against it. The only point in favor of PDS was presence of pigment on the ICL. UBM would have definitely aided in the diagnosis and helped in ruling out inciting factors like enlarged ciliary process. But since this investigatory facility was not available, we could not perform the same. Also on reviewing literature pupillary block caused by enlarged ciliary processes is not effectively relieved by peripheral iridectomy as compared to our case in which the IOP was controlled.19 After an extensive search of literature which was limited we found that explantation of the lens was the procedure undertaken in majority of these cases.20,21 However if problem was uniocular it left the patient with severe anisometropia after explantation.
Hence bearing in mind the pros and cons a surgical Iridectomy was the best intervention in this case scenario. We therefore advocate that surgical iridectomy can be a viable option in patients presenting with a similar clinical picture rather than explantation of the ICL.
Conflicts of interest
All authors have none to declare.
References
- 1.Gonvers M., Bornet C., Othenin-Girard P. Implantable contact lens for moderate to high myopia-relationship of vaulting to cataract formation. J Cataract Refract Surg. 2003;29:918–924. doi: 10.1016/s0886-3350(03)00065-8. [DOI] [PubMed] [Google Scholar]
- 2.Sanchez-Galeana C.A., Smith R.J., Sanders D.R. Lens opacities after posterior chamber phakic intraocular lens implantation. Ophthalmology. 2003;110:781–785. doi: 10.1016/s0161-6420(02)01973-5. [DOI] [PubMed] [Google Scholar]
- 3.Bylsma S.S., Zalta A.H., Foley E. Phakic posterior chamber intraocular lens pupillary block. J Cataract Refract Surg. 2002;28:2222–2228. doi: 10.1016/s0886-3350(02)01303-2. [DOI] [PubMed] [Google Scholar]
- 4.Smallman D.S., Probst L., Rafuse P.E. Pupillary block glaucoma secondary to posterior chamber phakic intraocular lens implantation for high myopia. J Cataract Refract Surg. 2004;30:905–907. doi: 10.1016/j.jcrs.2003.09.019. [DOI] [PubMed] [Google Scholar]
- 5.Jimenez-Alfaro I., Benitez del Castillo J.M., Garcia-Feijoo J. Safety of posterior chamber phakic intraocular lenses for the correction of high myopia: anterior segment changes after posterior chamber phakic intraocular lens implantation. Ophthalmology. 2001;108:90–99. doi: 10.1016/s0161-6420(00)00403-6. [DOI] [PubMed] [Google Scholar]
- 6.Brandt J.D., Mockovak M.E., Chayet A. Pigmentary dispersion syndrome induced by a posterior chamber phakic refractive lens. Am J Ophthalmol. 2001;131:260–263. doi: 10.1016/s0002-9394(00)00606-1. [DOI] [PubMed] [Google Scholar]
- 7.Abela-Formanek C., Kruger A.J., Dejaco-Ruhswurm I. Gonioscopic changes after implantation of a posterior chamber lens in phakic myopic eyes. J Cataract Refract Surg. 2001;27:1919–1925. doi: 10.1016/s0886-3350(01)01229-9. [DOI] [PubMed] [Google Scholar]
- 8.Sanchez-Galeana C.A., Zadok D., Montes M. Refractory intraocular pressure increase after phakic posterior chamber intraocular lens implantation. Am J Ophthalmol. 2002;134:121–123. doi: 10.1016/s0002-9394(02)01414-9. [DOI] [PubMed] [Google Scholar]
- 9.Colin J., Mimouni F., Robinet A. The surgical treatment of high myopia: comparison of epikeratoplasty, keratomileusis and minus power AC lenses. Refract Corneal Surg. 1990;6:245–251. [PubMed] [Google Scholar]
- 10.Fechner P.U., van der Heijde G.L., Worst J.G.F. The correction of myopia by lens implantation into phakic eyes. Am J Ophthalmol. 1989;107:659–663. doi: 10.1016/0002-9394(89)90264-x. [DOI] [PubMed] [Google Scholar]
- 11.Fechner P.U., Strobel J., Wichmann W. Correction of myopia by implantation of a concave Worst-iris claw lens into phakic eyes. Refract Corneal Surg. 1991;7:286–298. [PubMed] [Google Scholar]
- 12.Perez-Santonja J.J., Antico L., Ali J.L. Refractive Surgery and Phakic IOLs. In: Ali J.L., Perez-Santonja J.J., editors. Refractive Surgery with Phakic IOLs. Fundamentals and Clinical Practice. Highlights of Ophthalmology International; Panama: 2004. pp. 25–35. [Google Scholar]
- 13.Baikoff G., Arne J.L., Bokobza Y. Angle-fixated anterior chamber phakic intraocular lens for myopia of –7 to –19 diopters. J Refract Surg. 1998;14:282–293. doi: 10.3928/1081-597X-19980501-12. [DOI] [PubMed] [Google Scholar]
- 14.Perez-Santonja J.J., Ali J.L., Jimnez-Alfaro I., Zato M.A. Surgical correction of severe myopia with an angle-supported phakic intraocular lens. J Cataract Refract Surg. 2000;26:1288–1302. doi: 10.1016/s0886-3350(00)00543-5. [DOI] [PubMed] [Google Scholar]
- 15.Budo C., Hessloehl J.C., Izak M. Multicenter study of the Artisan phakic intraocular lens. J Cataract Refract Surg. 2000;26:1163–1171. doi: 10.1016/s0886-3350(00)00545-9. [DOI] [PubMed] [Google Scholar]
- 16.Sanders D.R., Vukich J.A. ICL in Treatment of Myopia Study Group: incidence of lens opacities and clinically significant cataracts with the implantable contact lens: comparison of two lens designs. J Refract Surg. 2002;18:673–682. doi: 10.3928/1081-597X-20021101-03. [DOI] [PubMed] [Google Scholar]
- 17.Lackner B., Pieh S., Schimidinger G. Long-term results of implantation of phakic posterior chamber intraocular lenses. J Cataract Refract Surg. 2004;30:2269–2276. doi: 10.1016/j.jcrs.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 18.Park In Ki, Lee Je Myung, Chun Yeoun Sook. Recurrent occlusion of laser iridotomy sites after posterior chamber phakic IOL implantation. Korean J Ophthalmol. 2008;22(2):130–132. doi: 10.3341/kjo.2008.22.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan Kenneth C.Y., Birchall Wayne, Gray Trevor B., Wells Anthony P. Acute angle closure after implantable contact lens insertion unresponsive to surgical peripheral iridectomy. J Cataract Refract Surg. 2008;34:696–699. doi: 10.1016/j.jcrs.2007.10.048. [DOI] [PubMed] [Google Scholar]
- 20.Khalifa Y.M., Goldsmith J., Moshirfar M. Bilateral explantation Visian Implantable Collamer Lenses secondary bilateral acute angle closure resulting from a non-pupillary block mechanism. J Refract Surg. 2010 Dec;26(12):991–994. doi: 10.3928/1081597X-20100521-01. [DOI] [PubMed] [Google Scholar]
- 21.Vetter J.M., Tehrani M., Dick H.B. Surgical management acute angle-closure glaucoma after toric implantable contact lens implantation. J Cataract Refract Surg. 2006 Jun;32(6):1065–1067. doi: 10.1016/j.jcrs.2006.02.028. [DOI] [PubMed] [Google Scholar]