Introduction
Hypertrophic osteoarthropathy (HOA) is a clinical syndrome that causes clubbing of the fingers and toes, enlargement of the extremities and pain and swelling of the joints. Patients may have one or more of these manifestations. The syndrome can be primary or secondary. The primary idiopathic form of HOA is called as pachydermoperiostosis (PDP).1 It is characterized by clubbing of the digits of both hands and feet, pachydermia (thickening of the facial skin and/or scalp), and periostosis (swelling of periarticular tissue and subperiosteal new bone formation).2 It is a rare genetic disorder with autosomal dominant transmission; however, autosomal recessive forms have been reported.3 It occurs predominantly in men and has been reported in many races. Here, we report a young male patient diagnosed to have PDP with delayed puberty at our tertiary care center.
Case report
An 18-years-old male patient, born of second degree consanguineous marriage, with no known comorbidities had been symptomatic for two years with insidious onset progressive enlargement of bilateral hands and feet (Fig. 1A, D). He developed symmetrical and gradually progressive increase in shoe size. This was also associated with gradually progressive swelling of bilateral ankle and knee joints which were initially painless but gradually became painful (Fig. 1C, D). Patient also developed gradually increasing swelling of bilateral wrists. Patient also complained of profuse sweating over palms and soles on minimal heat exposure. This was not associated with any restriction in movements. There is no history of headache, vomiting, visual disturbances, back pain or neck pain, skin rash, oral ulcers, or redness of eyes. There are no similar cases in his family. He was referred to our center with a provisional diagnosis of acromegaly.
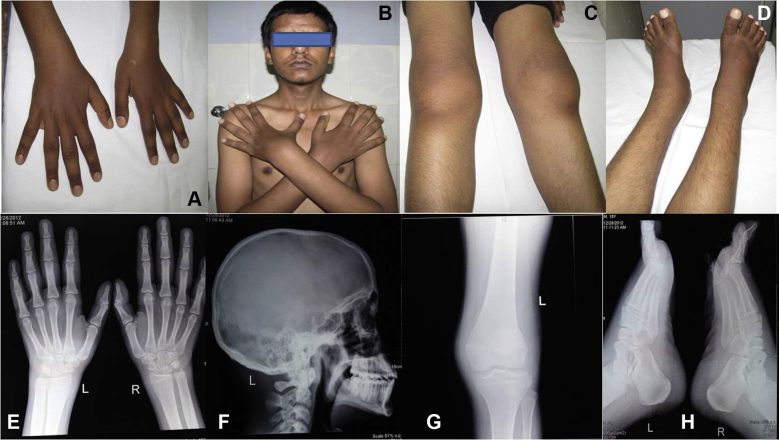
Fig. 1.
Photograph depicting: clubbing (A), cutis verticis gyrata on forehead (B), swelling involving bilateral knee (C) and ankle joint (D). Radiograph depicting: Increased ossification of the ulnar aspect of interosseous membrane (E), Normal sella turcica (F), soft tissue swelling involving bilateral knee (G) and ankle joint (H).
Physical examination revealed severe clubbing of bilateral hand and feet (Fig. 1A). Musculoskeletal system examination revealed swelling involving bilateral knee, ankle and wrist joint (Fig. 1C, D). Dermatologic examination revealed coarse facies, furrowing of the face, with cutis verticis gyrata mainly on his forehead (Fig. 1B), although the scalp was not affected. There was associated seborrhea, facial acne and hyperhydrosis involving both hand and feet. There was no acanthosis nigricans, skin tags, macroglossia, occipital prominence, cafe au lait spots or neurofibromas. There was lack of facial hair. His testicular volume was 10 ml and was in sexual maturity score of stage-3. The systemic examination was unremarkable.
Laboratory analyses showed normal hematological and biochemical parameters. Hormonal profile including growth hormone (GH) suppression test (basal GH – 1.31 ng/ml, 30 min-0.16 ng/ml, 60 min-0.15 ng/ml, 90 min-0.17 ng/ml) did not reveal any abnormality. The radiology revealed soft tissue swelling involving bilateral wrist, knees and ankles (Fig. 1G, H) along with increased ossification of the ulnar aspect of interosseous membrane (Fig. 1E). Radiograph of skull showed normal sella turcica (Fig. 1F). Bone scintigraphy showed clear visualization of his entire axial and peripheral skeleton. A chest radiograph, CECT chest, echocardiograph and upper GI endoscopy were all normal. He was managed with NSAIDS and supportive care. He is presently on follow up with improvement in his rheumatologic symptoms.
Discussion
Pachydermoperiostosis was first described in 1868 by Friedrich in two young brothers. PDP is the primary form of HOA and accounts for 3%–5% of all cases of HOA. Three forms of PDP have been described. First, a complete form with pachydermia, clubbing and periostosis. Second, an incomplete form with evidence of bone abnormalities but lacking pachydermia, and lastly, a forme fruste with prominent pachydermia and minimal-to-absent skeletal changes. PDP is diagnosed on the basis of presence of at least two of the four criteria: a history of familial transmission, pachydermia, digital clubbing and skeletal manifestations, such as pain or signs of radiographic periostosis.4
Our patient had the complete form of PDP, since he had severe finger clubbing, pachydermia and periostosis. The periostosis in our patient was not very prominent as the disease has been diagnosed within couple of years of onset. Most patients with PDP have normal development until adolescence, when skin thickening and joint deformities begin to occur. The changes progress for many years and usually stabilize thereafter. The disease occurs predominantly in men (sex ratio: nine to one) and is considered to be familial [25%–40% of cases].5 It is caused by mutations in 15-hydroxyprostaglandin dehydrogenase gene (HPGD), encoding 15-hydroxyprostaglandin dehydrogenase, the key enzyme of prostaglandin-D degradation.1 Our patient's parents are cousins, but there are no other affected family members, suggesting de novo mutation. The genetic studies were not carried out due to financial constraints.
The most prominent finding of PDP is digital clubbing which is seen in 89% of cases.5 Pachydermia meaning thickening and wrinkling of facial features including the forehead and the nasolabial folds is seen in 30%–40% of cases. The furrowing may involve the scalp or forehead, where it is known as cutis verticis gyrata which is seen in 24% of cases.5 The combination of thickened skin and bony enlargement can result in great thickening of the extremities, which is the most striking physical finding of PDP. Seborrhea is noted in more than 90% of cases, and hyperhydrosis particularly in the hands and feet is seen in 44% cases.5 Our patient had all of these findings.
Rheumatological manifestations of the disease include polyarthralgia which usually involve the knees and ankles. Synovial effusion affecting the knees may be seen in 41% of cases.4 Our patient had arthralgia involving knee and ankle joint; however there was no evidence of effusion. Radiology reveals diffuse periostosis along the length of long bones.2 The radiologic findings in our case were limited possibly due to early course of the disease.
Most patients tolerate the disease well. The chief complaints are related to polyarthralgias, their appearance and to hyperhydrosis. Our patient was chiefly troubled by polyarthralgias involving the knees and hyperhydrosis.
There is no specific treatment for PDP due to the lack of controlled data and current modalities are largely based on case reports. The therapeutic options for the control of symptoms consist of salicylates, non-steroidal anti-inflammatory drugs, systemic corticosteroids and colchicines. Rheumatologic symptoms can also be improved by treatment with bisphosphonates. Bisphosphonates inhibit osteoclastic bone resorption and therefore reduce bone remodeling and alleviate painful polyarthralgias.
Conclusion
PDP is a rare disease and can be diagnosed by the presence of digital clubbing, periostosis and pachydermia in the absence of any cardiovascular, pulmonary, liver, intestinal or mediastinal diseases, and can be a mimic to acromegaly.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Conflicts of interest
The authors have none to declare.
References
- 1.Castori M., Sinibaldi L., Mingarelli R., Lachman R.S., Rimoin D.L., Dallapiccola B. Pachydermoperiostosis: an update. Clin Genet. 2005;68:477–486. doi: 10.1111/j.1399-0004.2005.00533.x. [DOI] [PubMed] [Google Scholar]
- 2.Martinez-Lavin M. Miscellaneous non-inflammatory musculoskeletal conditions. Pachydermoperiostosis. Best Pract Res Clin Rheumatol. 2011;25:727–734. doi: 10.1016/j.berh.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 3.Harbison J.B., Nice C.M., Jr. Familial pachydermoperiostosis presenting as an acromegaly like syndrome. Am J Roentgenol Radium Ther Nucl Med. 1971;112:532–536. doi: 10.2214/ajr.112.3.532. [DOI] [PubMed] [Google Scholar]
- 4.Akrout R., Bendjema S., Fourati H., Ezzeddi M., Hachicha I., Baklouti S. Hypertrophy of the feet and ankles presenting in primary hypertrophic osteoarthropathy or pachydermoperiostosis: a case report. J Med Case Rep. 2012;6:31–34. doi: 10.1186/1752-1947-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kabi F., Mkinsi O., Janani S., Raissouni N. Pachydermoperiostosis. A case report. J Intern Med. 2006;27:710–712. doi: 10.1016/j.revmed.2006.04.019. [DOI] [PubMed] [Google Scholar]