Highlights
-
•
Spontaneous epidural hematoma of the spine (SEHS) is an extremely rare entity.
-
•
Early diagnosis and treatment showed to have the best outcome.
-
•
SESH should be suspected in every acute medullary syndrome with spinal pain, motor and/or sensory deficit.
Keywords: Spontaneous epidural hematoma of the spine, Oral anticoagulants, Acenocoumarol
Abstract
Introduction
Spontaneous epidural hematoma of the spine (SEHS) is an extremely rare entity. Patients known to have thrombophilia or on anticoagulant drugs are the most affected. It is generally caused by a rupture of the postero-internal vertebral venous plexus secondary to minor barotrauma such as cough, peridural catheter insertion...
Early diagnosis and treatment showed to have the best outcome.
Cases report
We report 3 cases of spontaneous epidural hematoma in patients treated by acenocoumarol, which occurred without any provocative factor. All 3 patients were treated with decompressive laminectomy.
Discussion
We described the MRI findings and discussed the spontaneity of the entity. Our present case studies and the review of the literature showed that early diagnosis and management of SEHS can lead to improvement of the neurological state and avoid definitive motor and sensitive deficit.
Conclusion
This rare entity should be suspected in every acute medullary syndrome with spinal pain, motor and/or sensory deficit. In order to decrease the sequelae, neurologically unstable patients should benefit from early diagnosis and urgent surgical decompression.
1. Introduction
Spontaneous epidural hematoma of the spine (SEHS) is an extremely rare entity. In 1869, Jackson described the first case that occurred in a 14 year-old girl [1]. Since then, about 600 cases were described in the literature [1,2].
The hematoma is defined as a blood collection in the extradural space compressing the anterior part of the medulla. Such rare event should figure in the differential diagnosis of patients presenting for any of the following: acute spinal syndrome, acute cervical pain or dorsal pain associated with sensory and/or motor and/or sphincter disturbances.
In our review of the literature, most of the investigators favored venous origin coming from the non-valvular postero-internal spinal venous plexus [1–2] [3–4] which makes it vulnerable to intra-thoracic and intra-abdominal pressures.
It occurs most commonly in the dorsal or the cervico-dorsal spine [5]. The description of the hematoma as a spontaneous accident is not always true. In fact, the epidural hematoma can be secondary to an arterio-venous malformation, a cavernoma, a vertebral hemangioma, and frequently associated with provocative factors such as: anticoagulant or anti-aggregating drugs, minor trauma, peridural catheter insertion, severe cough or extreme effort such as delivery, etc… [6]. All these facts question the spontaneity of the hematoma.
Anticoagulant drugs are linked to 17% of the patients [7], yet other factors seemed to contribute to the pathology in the majority of the cases. In this article, we report 3 patients on acenocoumarol, an anticoagulant drug that belongs to the anti-vitamin K drugs family, diagnosed to have spontaneous epidural hematoma that occurred without any provocative factors. All three patients had progressive neurologic deterioration and were treated surgically within the first 24 h.
2. Cases report
2.1. Case 1
A 68 year-old man, left handed, known to have a benign prostatic hypertrophy and a pulmonary embolus 1 year ago, treated with acenocoumarol 4 mg with controlled INR (International normalized ratio) at therapeutic range presented for acute tetraplegia.
The history goes back to the morning of the same day, the patient was awaked at 5:00 AM from a severe lower cervicalgia radiating bilaterally to his shoulders. He was addressed to the cardiovascular surgery unit for suspicion of an aortic dissection. An angio-CT was performed and showed a normal aorta. Four hours later, he started to complain from tetraparesis that progressed to complete tetraplegia after 6 h.
On physical examination, the patient was conscious and well oriented. His 4 extremities were paralytic both proximally and distally and he had a sensitive level at C4–C5. Babinski sign was positive at the right side and all his osteotendinous reflexes were abolished. The blood workup was normal except for an INR of 2.54. A cervical MRI was done and revealed a cervical epidural hematoma from C2 to T1 (Fig. 1). After INR correction with vitamin K and fresh frozen plasma, the patient underwent total laminectomy of C3–C4 and hemi-laminectomy from C5 to T1.
Fig. 1.

Sagittal T2 weighted MRI with spinal cord compression from C2 to D2.
On Day 1 after the decompression, patient’s condition showed clear motor improvement with 2/5 proximal force in his 4 limbs. At 2 weeks, his right hemi-body totally recovered whereas his left hemiparesis persisted with a motor deficit of the upper limb (3/5 proximally, 0/5 distally) and the lower limb (2/5 all over). After 1 year of rehabilitation, the patient totally recovered except for only a slight spasticity and episodes of urinary urgencies.
2.2. Case 2
A 49 year old male, right handed, presented for progressive tetraparesis over hours associated with interscapular pain. He is known to have a heterozygote mutation of factor V Leiden and a hyperhomocysteinemia complicated by many episodes of deep vein thrombosis (DVT) and one episode of pulmonary embolism after which the patient was treated by acenocoumarol.
At the Emergency Room, the patient was conscious, cooperative and well oriented. Neurological examination revealed a motor deficit of 3/5 both proximally and distally in the 4 limbs, a positive Babinski sign bilaterally, diffused hypereflexia and an atonic anal sphincter on digital rectal exam.
Blood tests were normal except for an INR of 2.31. A cervicothoracic MRI was done and was interpreted as normal and the patient was sent to the intensive care unit for surveillance. After 3 h, he had total paralysis and another cervicothoracolumbar MRI revealed a compressive spinal epidural hematoma from C3 to T12 (Figs. 2 and 3) and a subdural hematoma extending from L1 to L 4. After INR correction, the patient underwent decompressive laminectomy from C4- to T2 and from T8 to T12 in order to evacuate the epidural hematoma. Laminectomy was also performed from L1 to L4 in order to evacuate a subdural hematoma.
Fig. 2.

Sagittal T2 weighted MRI showing a subdural hematoma compressing the spinal cord and cauda equina from L1 to L4.
Fig. 3.
Sagittal T2 weighted MRI showing the extradural hematoma compressing the spinal cord from D8 to D12.
Three days later, a marked improvement was noted with motility reaching 4/5 in the upper limbs. In the lower limbs, lesser improvement was noted, especially in the right lower limb with a motor deficit of 2/5. The patient maintained fecal and urinary incontinence. He was transferred to a rehabilitation center. After 1 year, he was capable of walking using an English cane but his sphincteric incontinence persisted.
2.3. Case 3
A 74 years old male, right handed, under acenocoumarol for 3 years following an ischemic cerebral vascular accident recovering without any sequelae, presented to the ER one hour after an acute inter-scapular pain associated with left upper limb paresis.
On physical examination, the patient was in a good general condition. Neurological exam showed a motor deficit of 3/5 to the left brachial biceps and triceps. Osteotendinous reflexes were abolished in the left upper limb.
A brain MRI ruled out another ischemic cerebral vascular accident. Heparin was started on an electric syringe pump. Twenty four hours later, his cervical pain aggravated and he developed spinal symptoms. A cervical MRI showed a compressive epidural hematoma spreading from C3 to C6 (Figs. 4 and 5). The patient underwent a decompressive laminectomy from C3 to C6 about 24 h after his admission to the ER. He was discharged 3 days later without any neurological sequelae.
Fig. 4.
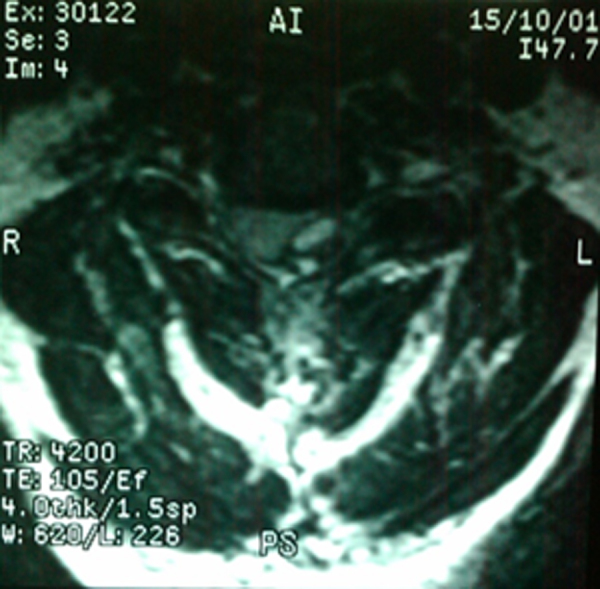
Axial T2 weighted MRI showing an extradural hematoma compressing the left hemicord.
Fig. 5.

Sagittal cervical T2 weighted MRI revealing an extradural hematoma from C3 to C5.
3. Discussion
Spinal epidural hematoma is rare. Only 1:100,000 patient per year is affected [8,9]. Evolution of acute spinal epidural hematoma is severe, leading sometimes to a spinal shock [10] or even death if the hemorrhage is at a high cervical level [11].
Chronic epidural hematoma is even rarer, and is most frequently located at the lumbar area. With mild symptoms and slight pain for months or years, the diagnosis is even more difficult with a differential going from abcess to neoplastic lesions. In such chronic forms, the delayed operative treatment does not have a negative influence on the outcome [12].
Many factors predispose to hematoma formation but the direct underlying cause is unknown in most cases [13]. Anti-coagulant treatment is mainly indicated in the treatment of thrombophilia and cardiovascular diseases and it seemed to contribute to nearly 17% of the cases. Other predisposing factors such as minor trauma or coughing were often associated. In our reported cases, the hematoma was spontaneous without any provocative factors. The second case was associated with blood dyscrasia.
Acute severe spinal pain followed by a neurologic deficit is the major symptom of spinal epidural hematoma [5,7] and should alert the treating physician to the possible diagnosis of SEHS. In our three cases, the clinical presentation was typical but the diagnosis was not made until after the aggravation of their neurological deficit, which could potentially impact the long-term outcome.
MRI is the diagnostic tool of choice. A CT scan should be obtained if MRI is not available but it is less sensitive. Intra-spinal hematomas are classified as subdural or epidural depending on their location and the suppression of epidural fat. Epidural hematoma displaces the dural space towards the spinal cord whereas, subdural hematoma maintains the dura and displaces it externally. Fat suppression sequences differentiate epidural hematoma and epidural fat. Sometimes peripheral enhancement is observed after contrast injection. This is probably due to dural hyperemia and/or adjacent meningeal thickening. Nodular enhancement is sometimes observed. Central enhancements of epidural hematomas seem to result from active extravasation.
Surgical treatment by decompression laminectomy and drainage is the treatment of choice [7]. Groen et al. found a significant relation between surgical delay and neurological sequelae with a maximum interval of 48 h [8]. It is a surgical emergency; early diagnosis and treatment are essential to decrease neurological sequelae. The main prognostic factors are the importance of preoperative neurological deficit [8], the time from clinical presentation to surgical decompression [5,8,9,11] and the time from clinical presentation to maximal deficit.
Conservative treatment was established with success in some cases [8,14], especially for patients with neurological stability and in case of surgical contraindication [15]. Conservative treatment consisted of complete bed rest with neurological surveillance.
All of our patients were operated after INR correction due to neurological aggravation. Only one patient completely recovered whereas the two others had a partial recovery with persistence of some neurological symptoms.
Specimens were sent to pathology and the results were negative for vascular malformations. Preoperative arteriography was considered unnecessary in our cases because of the delay that it could have caused for the operative management without offering, any additional information for the diagnosis.
4. Conclusion
Non-traumatic hematomas of the spine are rare and severe and can lead to serious neurological sequelae. Severe acute spinal pain followed by progressive neurological deficit is the major symptom that should alert the treating physician on the possible diagnosis of SEHS. MRI is the gold standard to confirm the presence and the extent of the hematoma. Early diagnosis and urgent surgical decompression are essential to decrease the neurological sequelae.
References
- 1.Jackson R. Case of spinal apoplexy. Lancet. 1869;2:5. [Google Scholar]
- 2.Kreppel D., Antoniadis G., Seeling W. Spinal hematoma: a literature survey with a meta-analysis of 613 patients. Neurosurg. Rev. 2003;26:1–49. doi: 10.1007/s10143-002-0224-y. [DOI] [PubMed] [Google Scholar]
- 3.Beatty R.M., Winston K.R. Spontaneous cervical epidural hematoma. A consideration of etiology. J. Neurosurg. 1984;61:143–148. doi: 10.3171/jns.1984.61.1.0143. [DOI] [PubMed] [Google Scholar]
- 4.Groen R.J.M., Ponssen H. The spontaneousspinal epidural hematoma. A study of the etiology. J. Neurol. Sci. 1990;98:121–138. doi: 10.1016/0022-510x(90)90253-j. [DOI] [PubMed] [Google Scholar]
- 5.Nuti C., Fotso M.J., Duhel R., Hatem B., Dumas B., Brunon J. Hématomes épiduraux non traumatiques du rachis. Présentation de 20 cas. Revue de la littérature et étude des aspects évolutifs. Neurochirurgie. 2003;49:563–570. [PubMed] [Google Scholar]
- 6.Moises Heleno V.B., Raphael B. Conservative treatment of large spontaneous spinal extradural hematoma. Arq. Neuropsiquiatr. 2010;68:130–131. doi: 10.1590/s0004-282x2010000100027. [DOI] [PubMed] [Google Scholar]
- 7.Matsumura A., Namikawa T., Hashimoto R., Okamoto T., Yanagida I., Hoshi M. Clinical management for spontaneous epidural hematoma: diagnosis and treatment. Spine J. 2007;8:534–537. doi: 10.1016/j.spinee.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 8.Groen R.J.M., Van Alphen H.A.M. Operative treatment of spontaneous spinal epidural hematomas, a study of the factors determining postoperative outcome. Neurosurgery. 1996;39:494–508. doi: 10.1097/00006123-199609000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Holtas S., Heiling M., Lonntoft M. Spontaneous spinal epidural hematoma: findings at MR imaging and clinical correlation. Radiology. 1996;199:409–413. doi: 10.1148/radiology.199.2.8668786. [DOI] [PubMed] [Google Scholar]
- 10.Chan D.T., Boet R., Poon W.S., Yap F., Chan Y.L. Spinal shock in spontaneous cervical spinal epidural haematoma. Acta Neurochir. (Wien) 2004;146:161–162. doi: 10.1007/s00701-004-0347-8. [DOI] [PubMed] [Google Scholar]
- 11.Adamson Bulsars D.C.K., Bronec P.R. Spontaneous cervical epidural hematoma: case report and literature review. Surg. Neurol. 2004;62:156–160. doi: 10.1016/j.surneu.2003.10.040. [DOI] [PubMed] [Google Scholar]
- 12.Belinchón J.M., Campos J., Merino J., Gallego J.M., Barcia Y.C. Chronic spontaneous lumbar epidural hematoma. Neurocirugia (Astur) 2005;16(6):533–536. [PubMed] [Google Scholar]
- 13.Oh J.Y.L., Lingaraj K., Rahmat R. Spontaneous spinal epidural haematoma associated with aspirin intake. Singapore Med. J. 2008;49:353–355. [PubMed] [Google Scholar]
- 14.Duffill J., Sparrow O.C., Millar J. Can spontaneous spinal epidural heamatoma be managed safely without operation? A report of four cases. J. Neurol. Neurosurg. Psychiatry. 2000;69:816–819. doi: 10.1136/jnnp.69.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tailor J., Dunn I.F., Smith E. Conservative treatment of spontaneous spinal epidural hematoma associated with oral anticoagulant therapy in a child. Childs Nerv. Syst. 2006;22:1643–1645. doi: 10.1007/s00381-006-0220-6. [DOI] [PubMed] [Google Scholar]



