Highlights
-
•
Preoperative imaging is essential for minimal invasive parathyroidectomy.
-
•
Conventional imaging is often negative or inconclusive.
-
•
18F-Fluorocholine PET–CT might be a solution.
-
•
We describe a patient with negative SPECT–CT and ultrasound.
-
•
Patient underwent successful surgery after positive PET–CT.
Abbreviations: pHPT, primary hyperparathyroidism; MIP, minimal invasive parathyroidectomy; BNE, bilateral neck exploration; Ca, calcium; PTH, parathormone; SPECT, single photon emission computed tomography; CT, computed tomography; PET, positron emission tomography; FCH, 18F-fluorocholine; US, ultrasound
Keywords: Primary hyperparathyroidism, Minimal invasive parathyroidectomy, Parathyroid adenoma, 18F-Fluorocholine PET–CT
Abstract
Introduction
Primary hyperparathyroidism is a common endocrine disorder for which the primary treatment is surgery. For minimal invasive parathyroidectomy adequate pre-operative imaging is essential. Conventional imaging is often inconclusive. There are reports that 18F-fluorocholine PET–CT might be a superior imaging modality, however evidence is still very scarce. This is the first report of a case with negative ultrasound and sestamibi SPECT–CT imaging that underwent successful minimal invasive surgery because of 18F-fluorocholine PET–CT.
Presentation of case
A 57 year-old man presented to us with complaints of fatigue. Laboratory results showed a biochemical primary hyperparathyroidism and an additional DEXA-scan revealed osteopenia of the lumbar spine. Conventional imaging consisting of neck ultrasound and Tc-99m-sestamibi SPECT–CT was however unable to localize the pathological gland. Subsequent 18F-fluorocholine PET–CT did clearly localize an adenoma dorsally of the left thyroid lobe which was removed at that exact location using minimal invasive parathyroidectomy. Histological examination confirmed the diagnosis adenoma and calcium levels remained normal at follow-up.
Discussion
There is clinical need for a superior imaging modality to detect pathological parathyroid glands to enable minimal invasive surgery. 18F-Fluorocholine is widely available.
Conclusion
18F-Fluorocholine PET–CT is a promising new imaging modality for localizing parathyroid adenomas and enabling minimal invasive parathyroidectomy when conventional imaging fails to do. Clinicians should consider its use as a second line modality for optimal patient care.
1. Introduction
Primary hyperparathyroidism (pHPT) is characterized by autonomous hypersecretion of parathyroid hormone (PTH) by one or more parathyroid glands, leading to an elevated serum calcium concentration. Hypercalcemia can cause a wide variety of well-described symptoms ranging from constipation and nausea to kidney stones and osteoporosis [1]. Diagnosis is established biochemically, with the finding of a relatively elevated serum calcium (Ca) level with a concomitant inappropriately elevated PTH level. In over 80% of cases, pHPT is caused by a single parathyroid adenoma [2]. Although both medical and surgical options for treatment are available, surgery is currently the only method of definitive cure as well as the most effective treatment modality overall [3].
The method of surgical intervention has shifted over the past two decades from extensive bilateral neck exploration (BNE) to minimal invasive parathyroidectomy (MIP). Minimal invasive surgery has its attendant benefits to shorter operative time, lower complication rate, and smaller incision length [4–6]. For surgery to be successful, adequate pre-operative imaging is essential to localize the abnormal gland(s). Conventional imaging consists of ultrasound (US) and Tc-99-sestamibi scanning. However even the most sensitive sestamibi scan, single photon emission computed tomography (SPECT)—computed tomography (CT), fails to identify abnormal parathyroid glands in up to 30% of cases [7]. These cases mandate traditional BNE or treatment with calcimimetics. Recently, a case report was published describing a potential new imaging modality for patients with pHPT. Quak et al. reported the incidental finding of a parathyroid adenoma using 18F-fluorocholine (FCH) positron emission tomography (PET)–CT in a patient suspected of recurrence of prostate cancer [8]. Choline is part of the phospholipid layer in the cell membrane and it is hypothesized that hyperfunctioning parathyroid cells have an increased activity of the phospholipid/Ca2+-dependent protein kinase which would lead to increased choline uptake [9]. Since then two studies with preliminary results have been published showing a superior detecting rate of FCH PET–CT over different types of conventional imaging [10,11]. We present, to our knowledge, the first case with negative US and SPECT–CT who underwent a successful MIP based on FCH PET–CT.
2. Case report
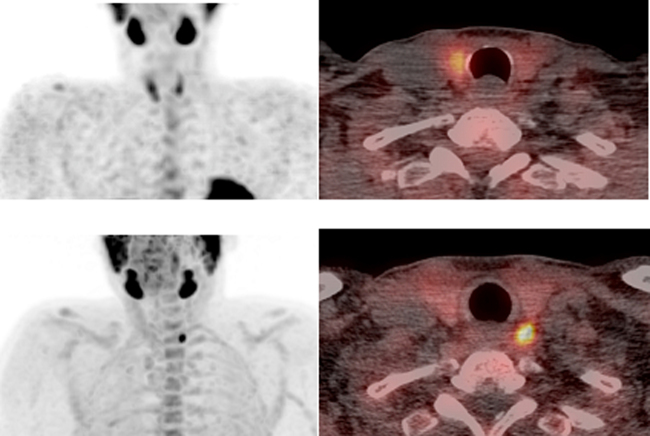
A 57-year-old man was referred to the Department of Surgery in February 2013 with complaints of fatigue. Biochemical laboratory investigation revealed pHPT. Laboratory results showed slightly elevated levels of Ca 2.78 mmol/L (normal: 2.20–2.60 mmol/L) and PTH of 10 pmol/L (normal: 1–7 pmol/L). Albumin level was 47.4 g/L (normal: 35–50 g/L) and 25-OH-vitamin-D was 67 nmol/L (normal: 50–100 nmol/L). Additional DEXA scanning showed osteopenia of the lumbar spine and it was decided that surgery was indicated. Conventional pre-operative imaging studies (US and 99mTc-sestamibi SPECT–CT (Fig. 1a)) did not reveal a parathyroid adenoma. Calcimimetics were prescribed, but serum Ca levels remained elevated. Subsequently a FCH PET–CT of the neck and mediastinum was performed 30 min after injection of 171MBq FCH. PET–CT showed intense focal FCH accumulation in a hypodense lesion posterior to the left upper thyroid lobe (Fig. 1b). Subsequently targeted US was performed and the parathyroid adenoma was visualized and marked for a MIP.
Fig. 1.
Coronal maximum intensity projection (MIP) of negative 99mTc-sestamibi SPECT and axial SPECT–CT (1a). Coronal MIP and axial PET–CT (1b) performed with 18F-fluorocholine clearly show a hotspot located posterior to the left upper thyroid lobe.
During surgery an abnormal gland was removed at the exact location indicated by FCH PET–CT. Histological examination showed a gland of 0.59 g and the diagnosis parathyroid adenoma was confirmed. Post-operatively Ca levels normalized and the patient remains normocalcemic at follow-up.
3. Discussion
Our patient had pHPT with an indication for surgery, however conventional imaging studies were unable to localize the pathological gland. This can be the case in up to 30% of patients and does not even take into account cases in which one study is discordant with another. Clinicians face a dilemma in all of these cases; they can either choose to perform a traditional BNE with greater morbidity or repeat the imaging after 6 months. In the meantime, the patient can be placed on medical therapy such as calcimimetics. Treatment with calcimimetics however, is not curative and often causes significant side effects including nausea and vomiting [12]. Both waiting and performing a BNE may, therefore, prove to be suboptimal for the patient. We propose that FCH PET–CT might be a solution whenever conventional imaging is unrevealing or discordant. So far two studies have published preliminary results. Michaud et al. investigated 12 patients with both primary and secondary HPT and negative or equivocal conventional imaging studies [10]. Their conventional imaging consisted of US and 123I/99mTc-sestamibi subtraction scintigraphy. They found an excellent parathyroid detection rate of 92% for FCH PET–CT. Lezaic et al. included 24 patients with HPT and performed three types of sestamibi scanning next to the FCH PET–CT [11]. They found a sensitivity of 92% for FCH PET–CT, which was significantly higher compared to the sestamibi scans. The advantage of FCH PET–CT over SPECT–CT is the higher spatial resolution and the signifcantly shorter scanning time with a single acquisition of only 8 min. The disadvantage of this modality is the high cost compared to conventional modalities and therefore an option would be to preserve it for the cases with negative/discordant imaging. At this moment, the combination of US and SPECT–CT is considered to be most accurate in the case of pHPT and is commonly used worldwide [13,14]. Our case is, to our knowledge, the first in which both US and SPECT–CT were negative but that could be operated on successfully by minimally invasive approach thanks to FCH PET–CT.
4. Conclusions
In conclusion, pHPT is a common disorder for which the primary treatment of choice is MIP. For MIP adequate pre-operative imaging is needed. FCH PET–CT is a promising new second line imaging modality that can guide succesfull MIP in the case of negative SPECT–CT and US.
Contributor Information
Wouter P. Kluijfhout, Email: Wpkluijfhout@gmail.com.
Menno R. Vriens, Email: M.R.Vriens@umcutrecht.nl.
Gerlof D. Valk, Email: G.D.Valk@umcutrecht.nl.
Roos E. Barth, Email: R.E.Barth@umcutrecht.nl.
Inne H.M. Borel Rinkes, Email: I.H.M.BorelRinkes@umcutrecht.nl.
Bart de Keizer, Email: B.deKeizer@umcutrecht.nl.
References
- 1.Alex G., Morris L., Pasieka J., Perrier N. Nonclassical symptoms of primary hyperparathyroidism and their response to parathyroidectomy. Am. Surg. 2013;79:337–343. [PubMed] [Google Scholar]
- 2.2Ruda J.M., Hollenbeak C.S., Stack B.C., Jr. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolarayngol. Head Neck Surg. 2005;132:359–372. doi: 10.1016/j.otohns.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Bilezikian J.P., Khan A.A., Potts J.T., Jr. Third international workshop on the management of asymptomatic primary hyperthyroidism. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J. Clin. Endocrinol. Metab. 2009;94:335. doi: 10.1210/jc.2008-1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sackett W.R., Barraclough B., Reeve T.S., Delbridge L.W. Worldwide trends in the surgical treatment of primary hyperparathyroidism in the era of minimally invasive parathyroidectomy. Arch. Surg. 2002;137:1055–1059. doi: 10.1001/archsurg.137.9.1055. [DOI] [PubMed] [Google Scholar]
- 5.Irvin G.L., Carneiro D.M., Solorzano C.C. Progress in the operative management of sporadic primary hyperparathyroidism over 34 years. Ann. Surg. 2004;239:704–708. doi: 10.1097/01.sla.0000124448.49794.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Norman J., Chheda H., Farrell C. Minimally invasive parathyroidectomy for primary hyperparathyroidism: decreasing operative time and potential complications while improving cosmetic results. Am. Surg. 1998;64:391–395. discussion 395-396. [PubMed] [Google Scholar]
- Ciappuccini R., Morera J., Pascal P., Rame J.P., Heutte N., Aide N. Dual-phase 99mTc sestamibi scintigraphy with neck and thorax SPECT/CT in primary hyperparathyroidism: a single-institution experience. Clin. Nucl. Med. 2012;37:223–228. doi: 10.1097/RLU.0b013e31823362e5. [DOI] [PubMed] [Google Scholar]
- 8.Quak E., Lheureux S., Reznik Y., Bardet S., Aide N. F18-Choline, a novel PET tracer for parathyroid adenoma? J. Clin. Endocrinol. Metab. 2013;98:3111–3112. doi: 10.1210/jc.2013-2084. [DOI] [PubMed] [Google Scholar]
- 9.Ishizuka T., Kajita K., Kamikubo K., Komaki T., Miura K., Nagao S. Phospholipid/Ca2+-dependent protein kinase activity in human parathyroid adenoma. Endocrinol. Jpn. 1987;34:965–968. doi: 10.1507/endocrj1954.34.965. [DOI] [PubMed] [Google Scholar]
- 10.Michaud L., Burgess A., Huchet V., Lefevre M., Tassart M., Ohnona J. Is 18F-fluorocholine-PET/CT a new imaging tool for detecting hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism? J. Clin. Endocrinol. Metab. 2014;12:jc20142821. doi: 10.1210/jc.2014-2821. [DOI] [PubMed] [Google Scholar]
- 11.11Lezaic L., Rep S., Sever M.J., Kocjan T., Hocevar M., Fettich J. 18F-Fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: a pilot study. Eur. J. Nucl. Med. Mol. Imaging. 2014;41:2083–2089. doi: 10.1007/s00259-014-2837-0. [DOI] [PubMed] [Google Scholar]
- 12.Marcocci C., Chanson P., Shoback D., Bilezikian J., Fernandez-Cruz L., Orgiazzi J. Cinacalcet reduces serum calcium concentrations in patients with intractable primary hyperparathyroidism. J. Clin. Endocrinol. Met. 2009;94:2766–2772. doi: 10.1210/jc.2008-2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neumann D.R., Obuchowski N.A., Difilippo F.P. Preoperative 123I/99mTc-sestamibi subtraction SPECT and SPECT/CT in primary hyperparathyroidism. J. Nucl. Med. 2008;49:2012–2017. doi: 10.2967/jnumed.108.054858. [DOI] [PubMed] [Google Scholar]
- 14.14Lavely W.C., Goetze S., Friedman K.P., Leal J.P., Zhang Z., Garret-Mayer E. Comparison of SPECT/CT, SPECT, and planar imaging with single- and dual-phase (99m) Tc-sestamibi parathyroid scintigraphy. J. Nucl. Med. 2007;48:1084–1089. doi: 10.2967/jnumed.107.040428. [DOI] [PubMed] [Google Scholar]