Abstract
Objectives. We evaluated sex-related differences in HIV and criminal justice (CJ) outcomes.
Methods. We quantified sex-related differences in criminal offenses, incarcerations, and HIV outcomes among all HIV-infected inmates on antiretroviral therapy (ART) in Connecticut (2005–2012). Computed criminogenic risk scores estimated future CJ involvement. Stacked logistic regression models with random effects identified significant correlates of HIV viral suppression on CJ entry, reflecting preceding community-based treatment.
Results. Compared with 866 HIV-infected men on ART (1619 incarcerations), 223 women (461 incarcerations) were more likely to be younger, White, and medically insured, with shorter incarceration periods (mean = 196.8 vs 368.1 days), mostly for public disorder offenses. One third of both women and men had viral suppression on CJ entry, correlating positively with older age and having treated comorbidities. Entry viral suppression inversely correlated with incarceration duration for women and with criminogenic risk score for men.
Conclusions. In the largest contemporary cohort of HIV-infected inmates on ART, women’s higher prevalence of nonviolent offenses and treatable comorbidities supports alternatives to incarceration strategies. Sex-specific interventions for CJ populations with HIV effectively align public health and safety goals.
Compared with any other country worldwide, the United States incarcerates the highest proportion of its citizens,1,2 especially those with underlying medical and psychiatric disorders.3 The central purpose of correctional systems is to administer punishment for crimes and protect the public by rehabilitating offenders. Treatment of inmates’ perceived nonurgent medical issues is thus often deprioritized, frequently at the expense of individual and public health.4,5 Incarceration is most disruptive to treatment continuity for people living with HIV/AIDS (PLWHA),6 who are often isolated from systems of care by poverty, racial or ethnic group, and substance use. One-sixth of the nearly 1 200 000 PLWHA in the United States cycle through criminal justice (CJ) settings annually,7 further constraining state budgets.8 It is thus critical to identify PLWHA who could benefit from alternatives to incarceration that reduce medical and custodial costs.
Women with HIV are vulnerable to incarceration because of associated drug use behaviors, commercial sex work, and having high-risk male partners.9,10 CJ-involved women are twice as likely as CJ-involved men and 15 times as likely as community-based women to have HIV and meet AIDS-defining criteria,6,11 reinforcing the need to keep HIV-infected women in the community and engaged in care. Women initiating antiretroviral therapy (ART) in community settings experience higher longitudinal survival rates than men.12 Incarceration is destabilizing, with high associated fiscal, ethical, and social costs, and it should remain the last resort to identify and treat HIV, though women are twice as likely as men to achieve viral suppression when treated in prison.13,14
After prison release, ART benefits wane for both women and men.13,15,16 During this chaotic transition period, suboptimal engagement in care, paired with reduced ART adherence and persistence, increases risk of genotypic resistance and continued HIV transmission, with negative consequences for individual and public health.13,15,17,18 Just 26% of men and 25% of women have viral suppression on jail entry, which reflects a lack of treatment engagement in the community.19 Women are significantly less likely than men to (1) report taking any prescribed ART immediately before jail entry,20 (2) fill an ART prescription in the 60 days after prison release,21 or (3) be retained in longitudinal HIV care with sustained viral suppression after release from jail.19,22 For CJ-involved women, HIV treatment persistence may be preferentially disrupted by untreated substance use and psychiatric disorders and by partner violence.23–26 We have previously reported that compared with men, women are significantly more likely to experience homelessness, ongoing cocaine use, and depression immediately before jail entry and 6 months after jail release—factors that contribute to loss of viral suppression after release.19
Aside from HIV, considerable sex disparities prevail in terms of frequency and type of criminal offending27 and sentencing standards. Women receive shorter federal sentences than men when matched on charged offense and criminal history,28,29 particularly with regard to property and drug-related offenses.30 In some states, women have longer sentences than men.31 Some have argued that women’s pathways to crime make incarceration less persuasive,32 requiring alternatives that more holistically address substance use and psychiatric treatment needs. Although previous studies have suggested a direct correlation between frequency of offending and medical comorbidity severity,33 to our knowledge this association has never been explored in terms of HIV.
New strategies are urgently needed to sustain community treatment and align public safety with public health goals. To support the development of gender-informed HIV interventions among CJ populations and to evaluate the specific effect of sex on HIV treatment and CJ outcomes, we analyzed data from a retrospective cohort of HIV-infected prisoners and jail detainees using longitudinally linked demographic, CJ, pharmacy, and laboratory data. The generated cohort is, to our knowledge, the largest of its kind in an integrated health system, and the only cohort to combine demographic and health data with specific data on criminal offense charges.
METHODS
The study sample was derived from the Connecticut Department of Correction (CTDOC), with approximately 16 347 inmates in 16 facilities.34 Women are confined to a single facility for pretrial detainees and sentenced inmates. With the exception of 5 other states (Rhode Island, Vermont, Delaware, Alaska, Hawaii),35 Connecticut has one of the few fully integrated correctional health systems that includes jails and prisons; all HIV care is provided onsite by infectious disease specialists and dedicated nurse case managers, and all Food and Drug Administration–approved ARTs are available. Although care for women is delivered in a single facility, health care across the CTDOC is standardized by the integrated health system.
The cohort has previously been described in terms of HIV treatment outcomes and recidivism.14,16 Individuals were included in this analysis if they (1) were incarcerated in any CTDOC facility (prison or jail) for any duration between March 2005 and June 2012, (2) had documented HIV and received ART during any incarceration, and (3) had at least 1 measurement of HIV viral load during incarceration.
Data Sources
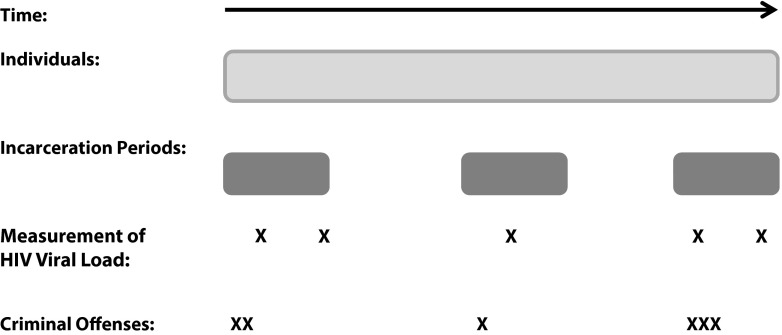
Data were derived from 4 existing statewide sources (Figure 1): (1) a custodial database with individual demographic information and dates and types of movements into, out of, and between facilities; (2) a pharmacy database with dates and types of prescribed medications, including ART; (3) a laboratory database with CD4 and viral load measurements during incarceration; and (4) CJ information, including dates and types of all state-level criminal offense charges. After merging databases using inmate number, we removed all unique personal identifiers to protect participant anonymity; data were stored and analyzed on triple-password-protected computers.
FIGURE 1—
Data sources for a sample participant and levels of analysis: Connecticut Department of Corrections, 2005–2012.
Measures
The primary outcome was viral suppression on entry, defined as having an HIV viral load of less than 400 copies per milliliter on intake into a CTDOC facility, to reflect HIV treatment delivered in community settings immediately preceding incarceration. Sociodemographic characteristics, derived from intake evaluations, included those listed in Table 1. We used custody information to define an incarceration period as the time from entry into a CTDOC facility to first date of release (completion of time served), conditional release to probation or parole, or death. We included incarceration period in the analysis only if HIV viral load was measured at any time. Interfacility transfers were defined as mandated movements between correctional facilities, including jails, prisons, hospitals, and halfway houses. We calculated reincarceration rate as the number of incarceration periods per time under observation, defined as the time from first release to data censor.
TABLE 1—
Descriptive Characteristics of HIV-Infected Individuals and Incarceration Periods, Stratified by Sex: Connecticut Department of Corrections, 2005–2012
| Characteristics | Total Sample (n = 1089, No. Incarceration Periods = 2080) | Men (n = 866, No. Incarceration Periods = 1619) | Women (n = 223, No. Incarceration Periods = 461) | Pa |
| Age, y, mean ±SD | 42.6 ±8.4 | 43.3 ±8.5 | 40.2 ±7.1 | < .001 |
| Race/ethnicity, no. (%) | < .001 | |||
| Non-Hispanic White | 218 (20.0) | 149 (17.1) | 69 (31.0) | |
| Non-Hispanic Black | 515 (47.3) | 411 (47.5) | 104 (46.6) | |
| Hispanic | 351 (32.2) | 303 (35.0) | 48 (21.5) | |
| Other | 5 (0.5) | 3 (0.4) | 2 (0.9) | |
| Married, no. (%) | 179 (16.4) | 149 (17.2) | 30 (13.5) | .18 |
| Dependent children, no. (%) | .21 | |||
| None | 400 (36.7) | 310 (35.8) | 90 (40.4) | |
| ≥ 1 | 689 (63.3) | 556 (64.2) | 133 (59.6) | |
| Education, no. (%) | .28 | |||
| ≤ high school | 502 (46.1) | 392 (45.3) | 110 (49.3) | |
| > high school | 587 (53.9) | 474 (54.7) | 113 (50.7) | |
| Ever had medical insurance on entry, no. (%) | 194 (17.8) | 79 (9.1) | 115 (51.6) | < .001 |
| No. of incarceration periods/person, mean ±SD | 1.9 ±1.4 | 1.9 ±1.4 | 2.1 ±1.4 | .06 |
| Incarceration duration, d | < .001 | |||
| Mean ±SD | 330.1 ±473.4 | 368.1 ±510.6 | 196.8 ±269.7 | |
| Median (IQR) | 166.5 (304) | 182 (383) | 96 (222) | |
| Interfacility transfers, no. (%) | .05 | |||
| 0 | 1954 (93.9) | 1512 (93.4) | 442 (95.9) | |
| ≥ 1 | 126 (6.1) | 107 (6.6) | 19 (4.1) | |
| Time spent in community between incarceration periods, db | ||||
| Mean ±SD | 325.9 ±357.7 | 323.1 ±353.3 | 334.6 ±317.9 | .3 |
| Median (min, max) | 194.5 (1, 2069) | 190.5 (1, 2069) | 208 (5, 2064) | .68 |
| Intake year, no. (%) | < .001 | |||
| 2005–2007 | 1025 (49.3) | 759 (46.9) | 266 (57.7) | |
| 2008–2010 | 803 (38.6) | 655 (40.5) | 148 (32.1) | |
| 2011–2012 | 252 (12.1) | 205 (12.7) | 47 (10.2) | |
| Discharge status, no. (%) | .22 | |||
| Probation or parole | 679 (32.6) | 533 (32.9) | 146 (31.7) | |
| Release | 1384 (66.6) | 1070 (66.1) | 314 (68.1) | |
| Death | 17 (0.8) | 16 (1.0) | 1 (0.2) | |
| Reincarceration ratec | .006 | |||
| Mean ±SD | 0.63 ±0.92 | 0.67 ±1.0 | 0.47 ±0.38 | |
| Median (IQR) | 0.41 (0.50) | 0.42 (0.52) | 0.38 (0.40) |
Note. IQR = interquartile range. The sample size was n = 1089 individuals and n = 2080 incarceration periods.
Calculated using Student t test for continuous variables and χ2 test for categorical variables unless otherwise noted.
For individuals with ≥ 1 incarceration during the observation period.
By Wilcoxon rank sum.
We characterized criminal offense charges by mutually exclusive classifications and types and subtypes. Because of the organization of the CJ data, criminal offense charges were attributable to an individual, but not to a specific incarceration period. As is customary in criminology literature, offenses were aggregated by arrest date, from which we extracted the most severe charge (on an ordinal scale, with public disorder offenses being the least severe; followed by violation of probation or parole or failure to appear; and drug- or alcohol-related, property, and person or violent offenses being the most severe). We approximated an “offending specification” as the mean number of arrests per individual by offense classification. We also generated an offending rate, defined as the number of arrests per time under observation less the time spent incarcerated in a facility.
CJ risk scores are often used to estimate actuarial criminogenic risk and predict future related CJ involvement on the basis of a number of individual demographic and support factors and history of offending.36–38 Standard of practice is for courts to use these scores in sentencing decisions. We adapted a salient factor estimate of CJ risk based on the Level of Services Inventory—Revised scale38 score during the observation period. We calculated scores by assigning 1 point to each of the following mutually exclusive factors:
having 2 or more arrests,
having a violation of conditional terms (i.e., violation of probation or parole or failure to appear),
having 2 incarcerations (2 points if ≥ 3),
having an escape charge,
ever having had a drug- or alcohol-related offense,
ever having had 3 or more charges on a single arrest, and
having the total days incarcerated within the sample’s middle tertile (2 points if highest tertile).
For individuals without any available offense information (26% of sampled men and 27% of sampled women), we assigned 0 points for each offense-related factor because we assumed that minor offenses would be more likely to be missing from a correctional database designed to manage the custodial population. Points were summed, and a sample distribution histogram defined the lowest score range as 0 to 1, the middle as 2 to 3, and the highest as more than 3. When individuals with missing offense data were alternately removed from the analysis, the sample distribution of the CJ risk score and modeling results remained relatively unchanged.
We determined HIV treatment outcomes and characteristics from laboratory and pharmacy data. CD4 and viral load variables were analyzed continuously on intake and release; viral suppression was analyzed as a dichotomous variable. ART regimen was examined at the times of entry and release and was defined by its components in terms of mutually exclusive categories, as previously described.14,16 We further characterized ART regimen in terms of calculated daily pill burden (based on included components and dosing strategy) and mode of medication administration, as previously described.14 We also examined whether individuals were ever prescribed ART as directly observed therapy during the observation period.
Medical and psychiatric severity scores are generated on intake by nursing staff as part of standard custodial procedure and classified on a scale ranging from 1, indicating no issues, to 5, indicating 24-hour nursing needs in a specialized unit. We grouped documented prescription of psychiatric and other medications by indicated condition and coded each category dichotomously. Diagnoses or diagnostic codes were not available in the electronic records, limiting available comorbidity data to conditions that were identified and treated, based on pharmacy records. A comorbidity score was generated for each individual participant, representing the sum total number of comorbidities (other than HIV) for which each participant was ever prescribed medication during any observed incarceration period, as shown in Table 2. Categories were mutually exclusive, and we analyzed the comorbidity score as a continuous variable.
TABLE 2—
Characteristics of Criminal Offense Charges, Stratified by Sex: Connecticut Department of Corrections, 2005–2012
| Criminal Offense Charges | Total Sample (n = 3242) | Men (n = 2631) | Women (n = 611) | Pa |
| Classification, no. (%) | < .001 | |||
| Misdemeanors | 1322 (40.8) | 1014 (38.5) | 308 (50.4) | |
| Felonies | 1235 (38.1) | 1045 (39.7) | 190 (31.1) | |
| Not classified | 685 (21.1) | 572 (21.7) | 113 (18.5) | |
| Crime against persons, no (%) | 463 (14.3) | 401 (15.2) | 62 (10.1) | < .001 |
| Crime against property, no (%) | 981 (30.3) | 794 (30.2) | 187 (30.6) | |
| Drug- or alcohol-related crime, no. (%) | 624 (19.3) | 530 (20.1) | 94 (15.4) | .04 |
| Possession or purchasing | 318 (51.0) | 261 (49.3) | 57 (60.6) | |
| Manufacturing or sale | 176 (28.2) | 150 (28.3) | 26 (27.7) | |
| Driving while Intoxicated | 130 (20.8) | 119 (22.5) | 11 (11.7) | |
| Public disorder, no. (%) | 1032 (31.8) | 777 (29.5) | 255 (41.7) | < .001 |
| Violation of probation or parole | 327 (31.7) | 261 (33.6) | 66 (25.9) | |
| Prostitution | 70 (6.8) | 14 (1.8) | 56 (22.0) | |
| Failure to appear | 259 (25.1) | 172 (22.1) | 87 (34.1) | |
| Other or escape | 376 (36.4) | 330 (42.4) | 46 (18.0) | |
| Other types, no (%) | 142 (4.4) | 129 (4.9) | 13 (2.1) | |
| Most severe arrest | < .001 | |||
| No. | 2111 | 1717 | 394 | |
| Persons, no. (%) | 368 (17.4) | 319 (18.6) | 49 (12.4) | |
| Property, no. (%) | 761 (36.0) | 618 (36.0) | 143 (36.3) | |
| Drug or alcohol-related, no. (%) | 511 (24.2) | 435 (25.3) | 76 (19.3) | |
| Violation of conditional terms,b no. (%) | 118 (5.6) | 82 (4.8) | 36 (9.1) | |
| Other public disorder, no. (%) | 353 (16.7) | 263 (15.3) | 90 (22.8) | |
| No. of arrests per individual, by class, mean ±SD | ||||
| Total | 4.06 ±3.3 | 4.13 ±3.3 | 3.77 ±3.1 | .21 |
| Persons | 0.58 ±1.0 | 0.63 ±1.1 | 0.38 ±0.8 | .001 |
| Property | 1.23 ±1.95 | 1.25 ±2.0 | 1.15 ±1.9 | .59 |
| Drug or alcohol-related | 0.78 ±1.2 | 0.83 ±1.2 | 0.58 ±0.9 | .003 |
| Public disorder | 1.47 ±1.7 | 1.42 ±1.7 | 1.65 ±1.6 | .12 |
| Arrest frequency per year | .006 | |||
| Mean ±SD | 0.45 ±0.4 | 0.47 ±0.4 | 0.38 ±0.3 | |
| Median | 0.31 | 0.32 | 0.27 | |
| CJ risk score, no. | 1089 | 866 | 223 | .03 |
| Lowest range, no. (%) | 257 (23.6) | 189 (21.8) | 68 (30.5) | |
| Middle range, no. (%) | 400 (36.7) | 329 (38.0) | 71 (31.8) | |
| Highest range, no. (%) | 432 (39.7) | 348 (40.2) | 84 (37.7) |
Note. CJ = criminal justice.
Calculated using Student t test for continuous variables and χ2 test for categorical variables unless otherwise noted.
Violation of conditional terms includes violation of probation or parole and failure to appear.
Statistical Analysis
A sex-stratified descriptive analysis characterized individuals, incarceration periods, criminal offense charges, and treatment characteristics and outcomes, using the Student t test or the Wilcoxon rank-sum test to compare continuous variables and the χ2 test for categorical variables. We modeled entry viral suppression using logistic regression with random effects (generalized linear mixed models) to account for clustered data among individuals. Models were stacked: model 1 included only key demographic characteristics (age, race/ethnicity, and education); model 2 included demographics and the CJ risk score; model 3 included demographics, the CJ risk score, and key information on medical and psychiatric comorbidities (entry ART regimen and comorbidity score); in model 4, all variables for which P < .1 in the bivariate analyses were entered into a multivariable model stepwise to achieve the most parsimonious model; and model 5 included only key modifiable characteristics. We compared model fit on Akaike and Bayesian information criteria and generated separate models for men and for women. We performed all analyses using SAS version 9.3 (SAS Institute, Cary, NC).
RESULTS
The final sample of 1089 HIV-infected prisoners and jail detainees with 2080 incarceration periods included 866 (79.5%) men with 1619 incarcerations and 223 (20.5%) women with 461 incarcerations. As shown in Table 1, compared with men, women were significantly more likely to be younger and to have medical insurance on entry; a greater proportion of women than men were non-Hispanic White. Overall, women’s incarcerations were shorter than men’s, and they were less likely to be reincarcerated, but we found no significant sex differences in terms of number of incarceration periods per person, interfacility transfers, time spent in the community, or discharge status.
Consistent with national data,39 criminal offense charges differed significantly by sex (Table 3). Compared with 2631 offense charges levied against men, the 611 charges against women were significantly less frequently for violent person crimes and more often for public disorder offenses, the majority of which involved prostitution or technical violation of probation or parole. Although men and women were nearly equally likely to have drug- or alcohol-related offenses, women’s charges more often involved drug possession or purchase with intent to use. The arrest rate for women was also significantly lower than that for men.
TABLE 3—
Treatment and Outcomes of HIV and Other Comorbidities During Incarceration, Stratified by Sex: Connecticut Department of Corrections, 2005–2012
| Characteristics | Total,a No. (%) or Mean ±SD | Men,b No. (%) or Mean ±SD | Women,c No. (%) or Mean ±SD | P |
| HIV treatment and outcomes | ||||
| HIV viral suppressiond | ||||
| On entry | 650 (32.7) | 516 (33.7) | 134 (29.5) | .1 |
| On release | 769 (70.6) | 621 (68.7) | 148 (80.0) | .002 |
| CD4 count | ||||
| On entry | 344.5 ±234.6 | 341.9 ±235.2 | 353.4 ±237.0 | .36 |
| On release | 449.6 ±272.6 | 448.3 ±277.5 | 456.0 ±247.8 | .73 |
| No. of individuals ever prescribed DOT | 582 ±53.4 | 454 ±52.4 | 128 ±57.4 | .18 |
| Type of medication administratione | < .001 | |||
| Never DOT | 794 (72.9) | 682 (75.4) | 112 (60.5) | |
| Transitional DOT | 18 (1.7) | 16 (1.8) | 2 (1.1) | |
| Continuous DOT | 25 (2.3) | 15 (1.7) | 10 (5.4) | |
| Transitional SAT | 252 (23.1) | 191 (21.1) | 61 (33.0) | |
| Entry ART regimen | ||||
| PI-based | 970 (48.8) | 750 (49.0) | 220 (48.5) | .85 |
| nNRTI-based | 730 (36.8) | 554 (36.2) | 176 (38.8) | .31 |
| FDC | 240 (12.1) | 196 (12.8) | 44 (9.7) | .08 |
| NRTI- based | 197 (9.9) | 155 (10.1) | 42 (9.3) | .59 |
| INSTI | 59 (3.0) | 50 (3.3) | 9 (2.0) | .16 |
| Other | 30 (1.5) | 23 (1.5) | 7 (1.5) | .95 |
| Medical and psychiatric comorbidities | ||||
| Intake medical severity | 3.4 ±0.8 | 3.4 ±0.8 | 3.4 ±0.7 | .77 |
| Intake psychiatric severity | 2.8 ±1.3 | 2.8 ±1.3 | 3.1 ±0.9 | |
| Individuals ever prescribed | ||||
| Antipsychotic | 216 (19.8) | 166 (19.2) | 50 (22.4) | .28 |
| Antidepressant | 446 (41.0) | 311 (35.9) | 135 (60.5) | < .001 |
| Both antipsychotic and antidepressant | 164 (15.1) | 123 (14.2) | 41 (18.4) | .12 |
| Individuals ever prescribed medications related to: | ||||
| Hypertension | 371 (34.1) | 314 (36.3) | 57 (25.6) | .003 |
| Diabetes | 126 (11.6) | 114 (13.2) | 14 (6.3) | .004 |
| Dyslipidemia | 117 (10.7) | 103 (11.9) | 14 (6.3) | .02 |
| Seizure disorder | 178 (16.4) | 144 (16.6) | 34 (15.3) | .62 |
| Herpes simplex virus | 213 (19.6) | 156 (18.0) | 57 (25.6) | .01 |
| Asthma | 229 (21.0) | 146 (16.9) | 83 (37.2) | < .001 |
| Neuropathy | 44 (4.0) | 25 (2.9) | 19 (8.5) | < .001 |
| HCV | 20 (1.8) | 18 (2.1) | 2 (0.9) | .4 |
| Opioid dependence | 94 (8.6) | 68 (7.9) | 26 (11.7) | .07 |
| Pregnancy | 13 (1.2) | . . . | 13 (5.8) | . . . |
| Comorbidity score | 1.9 ±1.7 | 1.8 ±1.6 | 2.3 ±1.6 | < .001 |
Note. ART = antiretroviral therapy; DOT = directly observed therapy; FDC = fixed-dose combination; INSTI = integrase strand transfer inhibitor; nNRTI = non-nucleoside reverse transcriptase inhibitor; NRTI = nucleoside reverse transcriptase inhibitor; PI = protease inhibitor; SAT = self-administered therapy.
The sample size was n = 1089 individuals and 2080 incarceration periods.
The sample size was n = 866 men and 1619 incarceration periods.
The sample size was n = 223 women and 461 incarceration periods.
Not all incarceration periods had viral loads available for both entry and release, so the percentage is the number with viral suppression/the number with available viral load on entry or on release, respectively.
Not all pharmacy prescriptions specified whether the medication was provided as DOT or SAT, so the denominator is based on the available information.
Main sex-stratified HIV treatment outcomes are depicted in Table 2. Although men and women were equally likely to have viral suppression on entry, women were significantly more likely to achieve viral suppression prerelease, despite insignificant differences between sexes in terms of entry ART regimen or ART daily pill burden (data not shown). A minority of ART regimens were switched during incarceration (data not shown). When examined by incarceration period, men more often had ART continuously self-administered, but men and women were equally likely to have ever been prescribed ART as directly observed therapy during any observed incarceration period. Women had higher mean intake psychiatric severity scores and were 1.7 times as likely as men to ever have been prescribed antidepressant medications during incarceration. Overall, women had a significantly greater number of non-HIV treated comorbidities than men, the majority of which were mood disorders. When analyzed as continuous variables, comorbidity and CJ risk scores had no significant direct correlation for either men or women (data not shown).
We modeled entry viral suppression for 1532 incarceration periods involving 824 unique men (Table 4). In the best-fit model by stepwise selection (model 4), the adjusted odds of having viral suppression on entry were positively correlated with older age, increasing comorbidity score, and more contemporary intakes. Black and Hispanic men were significantly less likely than White men to have viral suppression on entry, and individuals with the highest calculated CJ risk were half as likely as those with the lowest CJ risk score to have viral suppression on entry.
TABLE 4—
Correlates of Viral Suppression on Entry Among Men: Connecticut Department of Corrections, 2005–2012
| Covariate | Model 1, AOR (95% CI) | Model 2, AOR (95% CI) | Model 3, AOR (95% CI) | Model 4, AOR (95% CI) |
| Age (continuous) | 1.06* (1.04, 1.09) | 1.06* (1.04, 1.09) | 1.06* (1.03, 1.08) | 1.05* (1.02, 1.07) |
| Race/ethnicity | ||||
| Non-Hispanic White (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Non-Hispanic Black | 0.31* (0.18, 0.52) | 0.30* (0.18, 0.51) | 0.32* (0.19, 0.53) | 0.35* (0.21, 0.58) |
| Hispanic | 0.35* (0.20, 0.61) | 0.35* (0.20, 0.60) | 0.35* (0.21, 0.61) | 0.37* (0.22, 0.62) |
| Education | ||||
| ≤ high school (Ref) | 1.00 | 1.00 | 1.00 | . . . |
| > high school | 0.84 (0.57, 1.23) | 0.83 (0.37, 1.03) | 0.83 (0.57, 1.21) | . . . |
| CJ risk score | ||||
| Lowest range (Ref) | 1.00 | 1.00 | 1.00 | |
| Middle range | . . . | 0.82 (0.48, 1.41) | 0.75 (0.44, 1.27) | 0.81 (0.47, 1.39) |
| Highest range | . . . | 0.62 (0.37, 1.03) | 0.55* (0.33, 0.92) | 0.49* (0.29, 0.82) |
| Entry ART regimen | ||||
| PI based | . . . | . . . | 0.35 (0.11, 1.13) | |
| nNRTI based | . . . | . . . | 0.47 (0.14, 1.57) | |
| FDC | 0.59 (0.34, 1.00) | 0.63 (0.38, 1.03) | ||
| NRTI only | . . . | . . . | 0.34 (0.10, 1.18) | |
| INSTI | . . . | . . . | 1.27 (0.30, 5.43) | 2.11 (0.87, 5.14) |
| Comorbidity score | . . . | . . . | 1.11* (1.00, 1.24) | 1.13* (1.01, 1.26) |
| Incarceration period by intake year | ||||
| 2005–2007 (Ref) | . . . | . . . | . . . | 1.00 |
| 2008–2010 | . . . | . . . | . . . | 2.13* (1.52, 2.97) |
| 2011–2012 | . . . | . . . | . . . | 2.83* (1.74, 4.58) |
| Medical insurance on entry | ||||
| Yes (Ref) | . . . | . . . | . . . | 1.00 |
| No | . . . | . . . | . . . | 0.56 (0.31, 1.03) |
| AIC/BIC | 1815.79/1844.06 | 1815.77/1853.46 | 1806.90/1872.86 | 1788.45/1835.57 |
Note. AOR = adjusted odds ratio; AIC = Akaike information criterion; ART = antiretroviral therapy; BIC = Bayesian information criterion; CI = confidence interval; CJ = criminal justice; DOT = directly observed therapy; FDC = fixed-dose combination; INSTI = integrase strand transfer inhibitor; nNRTI = nonnucleoside reverse transcriptase inhibitor; NRTI = nucleoside reverse transcriptase inhibitor; PI = protease inhibitor; SAT = self-administered therapy. Model 1 includes demographic characteristics only (age, race/ethnicity, education); model 2 includes demographics and CJ risk; model 3 includes demographics, CJ risk, and HIV and other comorbidity severity; model 4 includes all covariates for which P < .1 on bivariate association, followed by stepwise selection. The sample size was n = 824 individuals and n = 1532 incarceration periods.
*P < .05.
We modeled entry viral suppression separately for 454 incarceration periods involving 219 unique women (Table 5). In the best-fit model (model 1) that included only demographic characteristics, each increasing year of age was associated with a 10% increased odds of having viral suppression on entry. Otherwise, among women, viral suppression was not directly associated with our measure of CJ risk, ART regimen, or medical or psychiatric comorbidity. When only modifiable characteristics were included as possible covariates in model 5, women’s entry viral suppression was directly associated with increasing comorbidity score and shorter incarceration duration.
TABLE 5—
Correlates of Viral Suppression on Entry Among Women: Connecticut Department of Corrections; 2005–2012
| Covariate | Model 1, AOR (95% CI) | Model 2, AOR (95% CI) | Model 3, AOR (95% CI) | Model 4, AOR (95% CI) | Model 5, AOR (95% CI) |
| Age (continuous) | 1.10* (1.04, 1.17) | 1.10* (1.04, 1.17) | 1.09* (1.03, 1.16) | 1.09* (1.03, 1.15) | . . . |
| Race/ethnicity | |||||
| Non-Hispanic White (Ref) | 1.00 | 1.00 | 1.00 | . . . | . . . |
| Non-Hispanic Black | 1.17 (0.50, 2.71) | 1.15 (0.49, 2.69) | 1.18 (0.35, 3.28) | . . . | . . . |
| Hispanic | 1.11 (0.37, 3.30) | 1.11 (0.37, 3.31) | 1.08 (0.50, 2.81) | . . . | . . . |
| Education | |||||
| ≤ high school (Ref) | . . . | . . . | . . . | . . . | . . . |
| > high school | 0.75 (0.35, 1.60) | 0.96 (0.43, 2.14) | 0.79 (0.37, 1.69) | . . . | . . . |
| CJ risk score | |||||
| Lowest range (Ref) | . . . | 1.00 | 1.00 | . . . | 1.00 |
| Middle range | . . . | 0.68 (0.25, 1.89) | 0.60 (0.21, 1.71) | . . . | 0.80 (0.30, 2.12) |
| Highest range | . . . | 0.71 (0.29, 1.75) | 0.59 (0.22, 1.56) | . . . | 0.57 (0.23, 1.42) |
| Entry ART regimen | |||||
| PI-based | . . . | . . . | 0.56 (0.06, 4.88) | . . . | . . . |
| nNRTI-based | . . . | . . . | 0.35 (0.04, 3.29) | . . . | . . . |
| FDC | . . . | . . . | 2.02 (0.71, 5.77) | . . . | . . . |
| NRTI only | . . . | . . . | 0.43 (0.04, 4.40) | . . . | . . . |
| INSTI | . . . | . . . | 1.02 (0.05, 19.21) | . . . | . . . |
| Comorbidity score | . . . | . . . | 1.13 (0.89, 1.43) | . . . | 1.24* (0.98, 1.56) |
| Incarceration period by intake year | |||||
| 2005–2007 (Ref) | . . . | . . . | . . . | 1.00 | . . . |
| 2008–2010 | . . . | . . . | . . . | 1.67 (0.90, 3.09) | . . . |
| 2011–2012 | . . . | . . . | . . . | 2.03 (0.77, 5.35) | . . . |
| Medical insurance at entry | |||||
| Yes (Ref) | . . . | . . . | . . . | . . . | 1.00 |
| No | . . . | . . . | . . . | . . . | 0.72 (0.27, 1.91) |
| Time incarcerated, mo | . . . | . . . | . . . | . . . | 0.96* (0.92, 1.00) |
| Discharge status | |||||
| Conditional release (Ref) | . . . | . . . | . . . | . . . | 1.00 |
| Release/death | . . . | . . . | . . . | . . . | 0.97 (0.48, 1.94) |
| Ever prescribed DOT | |||||
| No (Ref) | . . . | . . . | . . . | . . . | 1.00 |
| Yes | . . . | . . . | . . . | . . . | 0.81 (0.39, 1.68) |
| AIC/BIC | 516.39/536.67 | 519.67/546.70 | 527.26/574.58 | 516.69/543.73 | 537.90/568.40 |
Note. AIC = Akaike information criterion; AOR = adjusted odds ratio; ART = antiretroviral therapy; BIC = Bayesian information criterion; CI = confidence interval; CJ = criminal justice; DOT = directly observed therapy; FDC = fixed-dose combination; INSTI = integrase strand transfer inhibitor; nNRTI = nonnucleoside reverse transcriptase inhibitor; NRTI = nucleoside reverse transcriptase inhibitor; PI = protease inhibitor. Model 1 includes demographic characteristics only (age, race/ethnicity, education); model 2 includes demographics and CJ risk; model 3 includes demographics, CJ risk, and HIV and other comorbidity severity; model 4 includes all covariates for which P < .1 on bivariate association, followed by stepwise selection; model 5 includes only modifiable characteristics. The sample size was n = 219 individuals and n = 454 incarceration periods.
*P < .05.
DISCUSSION
In this retrospective longitudinal cohort of 1089 prisoners and jail detainees with HIV on ART with 2080 incarceration periods spanning more than 7 years, we identified key differences between the sampled men and women in terms of major CJ characteristics and HIV treatment outcomes. Compared with men, women were detained for significantly shorter periods and had lower calculated criminogenic risk. Men and women entered the CTDOC with similar levels of viral suppression, reflective of their (suboptimal) community HIV treatment, but a higher proportion of women achieved viral suppression during incarceration, despite women having a higher burden of medical and psychiatric comorbidities. Findings illuminate the need for gender-informed HIV treatment strategies that can achieve maximal effectiveness among CJ-involved PLWHA.
By incorporating, for the first time to our knowledge, an in-depth examination of criminal offense charges and HIV-related health outcomes, we uncovered some striking contrasts between men and women. Specifically, women were significantly more likely than their male counterparts to be charged with public disorder offenses, the majority of which were for prostitution or violation of conditional terms. These lower level charges might serve as a targeted opportunity to effectively engage these women in communities and better align safety goals related to correctional supervision (i.e., probation or parole) with public health goals related to retention in HIV care and ART adherence. This specific finding would otherwise have been missed in most analyses that rely more broadly on incarceration data to reflect the extent of CJ involvement.
Overall, compared with national data from the Bureau of Justice Statistics, violent crimes (including murder, rape and sexual assault, robbery, and assault) were markedly lower in this cohort of PLWHA (15% vs 54% for men and 10% vs 37% for women).39 As has been shown elsewhere,40 PLWHA are more likely to be incarcerated for minor offenses, especially those that can be more effectively addressed in the community.41
Community-based strategies have the additional benefit of reducing public spending because incarceration, especially of patients with multiple medical and psychiatric comorbidities, is expensive, and conditions are more cost effectively addressed in community settings.42 Community-based alternatives to incarceration strategies, which include drug and mental health courts, have key public policy implications for curbing the United States’ astronomical incarceration rate. Existing evidence has suggested that drug court participation significantly reduces relapse to substance use and rates of criminal behavior and durably and cost-effectively improves overall quality of life.43 Little to no data are available, however, on the effects of drug courts on health outcomes, leading some to suggest that drug courts lack transparency or are not sufficiently health centered.44 Rather than exclude individuals with co-occurring disorders, which is common practice,45 drug courts will be maximally effective when they align public safety and public health by incorporating treatment of other medical and social comorbidities such as HIV, psychiatric disorders, and homelessness. This shift will likely preferentially affect women who, as shown here, experience a significantly higher burden of comorbidity than men. Instead of using drug courts to off-load prisons, alternatives to incarceration strategies can be leveraged to help stabilize chaotic lives in a more effective and enduring way than imprisonment, in which HIV treatment outcomes are temporarily optimized, then deteriorate rapidly after release.14,16
Previous published literature from the criminology and legal fields has suggested that individuals with untreated medical comorbidities are more likely to commit crimes and ultimately become CJ involved. In a study of 915 offenders in Canada, for example, diabetes was twice as prevalent as in the general population, was mostly undiagnosed or untreated at the time of offense, and was most frequent among violent and sex offenders whose victims were children.33 From a legal perspective, uncontrolled diabetes has historically been considered a disease of the mind and within the scope of the insanity defense,46 although the association between medical comorbidity severity and criminality or aggression has more recently been suggested in relation to epilepsy,47 dyslipidemia,48 and other diseases, mostly in men. Missing from these studies has been consideration of race/ethnicity, neighborhood, and socioeconomic status as confounders that likely contribute both to serious health disparities and to CJ risk.49 We found, for example, that Black and Hispanic men were significantly less likely than their White counterparts to have viral suppression on entry. Even after we controlled for these potential confounders in multivariable models, however, men with the highest levels of CJ risk were consistently and least likely to have viral suppression.
Our findings suggest that the association, though not causative, between CJ risk and poor health outcomes extends to include HIV. Unlike diabetes or epilepsy, HIV is a chronic disease that is generally asymptomatic. HIV differs from other chronic diseases in a more important way because when it is inadequately treated and viral suppression is not achieved, the virus can be transmitted to others in the setting through risk behaviors.50 We identify here a population of PLWHA who are disengaged from major systems of health care and social support, putting them at higher risk of CJ involvement and suboptimal HIV treatment outcomes. Criminogenic risk and HIV viral suppression are each modifiable characteristics amenable to targeted interventions. Correctional community supervision—that is, probation or parole—may provide an opportunity for intervention from both public health and public safety perspectives. Costs and criminal behaviors decrease when people can be successfully maintained in the community.
For women in this cohort, the array of available data was insufficient to fully explain viral suppression on entry using various analytical methods. Although the smaller sample of women may have underpowered our analyses, we suspect instead that a number of unmeasured confounders may have biased results toward the null. Women’s pathways to substance use, criminality, and incarceration, unlike those of their male counterparts, are more often related to lack of social or economic capital.51–54 Thus, for women, CJ risk is most strongly associated with comorbid conditions and involvement in sex work as well as related partner dependency, partner violence,26 and homelessness—factors that were not well represented or measured in the databases we used.
Compared with CJ-involved men, CJ-involved women have a higher prevalence of unrecognized or untreated psychiatric and substance use disorders,55 which may contribute to their criminal behavior. To disentangle this association, we first have to understand the extent to which untreated comorbidities in the community contribute to the relatively low proportion of women with viral suppression on entry into the CJ setting,19 and develop detailed assessments during incarceration and after release. We have previously reported that women released from jail were significantly more likely than men to report ongoing cocaine use and were half as likely as men to sustain viral suppression 6 months after release.19
Given the synergistic effect of substance use, violence, psychiatric disorders, and social instability on HIV-related health outcomes of CJ-involved women, sex-specific and culturally relevant interventions will incorporate a syndemic approach that collectively addresses social and medical conditions.23,56 Although several previous syndemic HIV prevention interventions have been described,57–59 lack of sustainability remains a major concern.60 To maximize immediate and durable benefits for health and CJ outcomes, evidence-based interventions could be adapted and incorporated into existing structural systems, such as probation and parole.61
Limitations
Although this retrospective cohort study provides important new insight into multidimensional and sex-specific factors affecting prisoner health, analyses were necessarily restricted by available data. In some cases, unvalidated scales were used, either because they are routinely used by correctional systems to manage custodial populations and determine service needs (e.g., intake medical or psychiatric severity scores) or because they were calculated composite scales (e.g., comorbidity score, CJ risk score) that required imputations for missing data. Although we used all available data to sufficiently represent offense history, we could not account for federal offense charges or charges acquired out of state that may have affected outcomes, though we suspect this represented a minority of the sample; community-based data on health outcomes or service utilization were also not available. Our findings likely overestimate the proportion of inmates with HIV who achieve viral suppression because data were restricted only to those diagnosed and prescribed ART. Finally, generalizability might be limited to this state’s correctional health system, though we suspect, given the large sample size and long period of observation, that critical issues raised here are likely relevant to other systems of CJ and health care delivery.
Conclusions
To our knowledge, from the largest contemporary cohort of HIV-infected inmates on ART, women's incarceration and HIV treatment outcomes differed in critical and dynamic ways from men’s, providing insight into addressing sex-related health disparities. Women’s higher prevalence of nonviolent offenses and increased medical and psychiatric comorbidities, especially treatable substance use disorders, supports alternatives to incarceration strategies to holistically provide treatment. Interventions for HIV-infected CJ populations should be sex specific to effectively align health and justice goals.
Acknowledgments
Funding for this research was provided through a Bristol Myers-Squibb Virology Fellows Award and a Patterson Trust Award in Clinical Research (to J. P.M.) and from the National Institute on Drug Abuse (K23 DA033858 to J. P.M., F31 DA035709 to J.C., K24 DA017072 to F. L.A., and R01 DA030768 to F. L. A. and F. S.T.).
This project was performed in collaboration with the Connecticut Department of Correction and University of Connecticut Correctional Managed Health Care. We are particularly indebted to Edward Pesanti, Mary Lansing, Colleen Gallagher, Bob Cosgrove, and PeiTi Lee for their assistance with data collection and Robert Trestman and Johnny Wu for administrative support; no compensation was received for these contributions.
Note. The funding sources played no role in study design; data collection, analysis, or interpretation; writing of the article; or the decision to submit the article for publication. The authors have no competing interests to declare.
Human Participant Protection
All procedures were independently approved by Yale’s institutional review board and the Connecticut Department of Corrections Research Advisory Committee.
References
- 1.Pew Center on the States. One in 31: The Long Reach of American Corrections. Washington, DC: Pew Charitable Trusts; 2009. [Google Scholar]
- 2.International Centre for Prison Studies. World Prison Brief. London, UK: International Centre for Prison Studies; 2014. Available at: http://www.prisonstudies.org/world-prison-brief. Accessed January 21, 2014. [Google Scholar]
- 3.Maruschak L. Medical Problems of Jail Inmates. Washington, DC: US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2006. Bureau of Justice Statistics Special Report NCJ 210696. [Google Scholar]
- 4.Cropsey KL, Binswanger IA, Clark CB, Taxman FS. The unmet medical needs of correctional populations in the United States. J Natl Med Assoc. 2012;104(11–12):487–492. doi: 10.1016/s0027-9684(15)30214-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith A Committee on Causes and Consequences of High Rates of Incarceration, Committee on Law and Justice, Division of Behavioral and Social Sciences and Education, National Research Council, Board on the Health of Select Populations, Institute of Medicine. Health and Incarceration: A Workshop Summary. Washington, DC: National Academies Press; 2013. [Google Scholar]
- 6.Youmans E, Burch J, Moran R, Smith L, Duffus WA. Disease progression and characteristics of HIV-infected women with and without a history of criminal justice involvement. AIDS Behav. 2013;17(8):2644–2653. doi: 10.1007/s10461-011-0057-1. [DOI] [PubMed] [Google Scholar]
- 7.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS ONE. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pew Center on the States. State of Recidivism: The Revolving Door of America’s Prisons. Washington, DC: Pew Charitable Trusts; 2011. [Google Scholar]
- 9.Altice FL, Marinovich A, Khoshnood K, Blankenship KM, Springer SA, Selwyn PA. Correlates of HIV infection among incarcerated women: implications for improving detection of HIV infection. J Urban Health. 2005;82(2):312–326. doi: 10.1093/jurban/jti055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White House Council on Women and Girls. Women in America: Indicators of Social and Economic Well-Being. Washington, DC: US Department of Commerce, Economics and Statistics Administration, and Executive Office of the President, Office of Management and Budget; 2011. [Google Scholar]
- 11.Maruschak L, Beavers R. Washington, DC: US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2009. HIV in Prisons, 2007-2008. Bureau of Justice Statistics Bulletin NCJ 228307. [Google Scholar]
- 12.Castilho JL, Melekhin VV, Sterling TR. Sex differences in HIV outcomes in the highly active antiretroviral therapy era: a systematic review. AIDS Res Hum Retroviruses. 2014;30(5):446–456. doi: 10.1089/aid.2013.0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Springer SA, Pesanti E, Hodges J, Macura T, Doros G, Altice FL. Effectiveness of antiretroviral therapy among HIV-infected prisoners: reincarceration and the lack of sustained benefit after release to the community. Clin Infect Dis. 2004;38(12):1754–1760. doi: 10.1086/421392. [DOI] [PubMed] [Google Scholar]
- 14.Meyer JP, Cepeda J, Wu J, Trestman RL, Altice FL, Springer SA. Optimization of human immunodeficiency virus treatment during incarceration: viral suppression at the prison gate. JAMA Intern Med. 2014;174(5):721–729. doi: 10.1001/jamainternmed.2014.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stephenson BL, Wohl DA, Golin CE, Tien HC, Stewart P, Kaplan AH. Effect of release from prison and re-incarceration on the viral loads of HIV-infected individuals. Public Health Rep. 2005;120(1):84–88. doi: 10.1177/003335490512000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meyer JP, Cepeda J, Springer SA, Wu J, Trestman RL, Altice FL. HIV in people reincarcerated in Connecticut prisons and jails: an observational cohort study. Lancet HIV. 2014;1(2):e77–e84. doi: 10.1016/S2352-3018(14)70022-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baillargeon J, Giordano T, Harzke A et al. Predictors of reincarceration and disease progression among released HIV-infected inmates. AIDS Patient Care STDS. 2010;24(6):389–394. doi: 10.1089/apc.2009.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clements-Nolle K, Marx R, Pendo M, Loughran E, Estes M, Katz M. Highly active antiretroviral therapy use and HIV transmission risk behaviors among individuals who are HIV infected and were recently released from jail. Am J Public Health. 2008;98(4):661–666. doi: 10.2105/AJPH.2007.112656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meyer JP, Zelenev A, Wickersham JA, Williams CT, Teixeira PA, Altice FL. Gender disparities in HIV treatment outcomes following release from jail: results from a multicenter study. Am J Public Health. 2014;104(3):434–441. doi: 10.2105/AJPH.2013.301553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen NE, Meyer JP, Avery AK et al. Adherence to HIV treatment and care among previously homeless jail detainees. AIDS Behav. 2013;17(8):2654–2666. doi: 10.1007/s10461-011-0080-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baillargeon J, Giordano TP, Rich JD et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301(8):848–857. doi: 10.1001/jama.2009.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Althoff AL, Zelenev A, Meyer JP et al. Correlates of retention in HIV care after release from jail: results from a multi-site study. AIDS Behav. 2013;17(suppl 2):156–170. doi: 10.1007/s10461-012-0372-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the SAVA syndemic. J Womens Health (Larchmt) 2011;20(7):991–1006. doi: 10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meyer JP, Chen NE, Springer SA. HIV treatment in the criminal justice system: critical knowledge and intervention gaps. AIDS Res Treat. 2011;2011:680617. doi: 10.1155/2011/680617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams CT, Kim S, Meyer J et al. Gender differences in baseline health, needs at release, and predictors of care engagement among HIV-positive clients leaving jail. AIDS Behav. 2013;17(suppl 2):195–202. doi: 10.1007/s10461-012-0391-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meyer JP, Wickersham JA, Fu JJ et al. Partner violence and health among HIV-infected jail detainees. Int J Prison Health. 2013;9(3):124–141. doi: 10.1108/IJPH-03-2013-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bonczar TP. Table 4. New court commitments to state prison, 2009: offense, by sex, race, and Hispanic origin. Available at: http://www.bjs.gov/index.cfm?ty=pbdetail&iid=2065. Accessed May 23, 2014.
- 28.Mustard DB. Racial, ethnic, and gender disparities in sentencing: evidence from the US federal courts. J Law Econ. 2001;44(1):285–314. [Google Scholar]
- 29.Starr S. Estimating Gender Disparities in Federal Criminal Cases. Ann Arbor, MI: University of Michigan Law School, Law and Economics Working Papers Repository; 2012. [Google Scholar]
- 30.Rodriguez SF, Curry T, Lee G. Gender differences in criminal sentencing: do effects vary across violent, property, and drug offenses? Soc Sci Q. 2006;87(2):318–339. [Google Scholar]
- 31.Carson EA. Prisoners in 2013. Washington, DC: US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2014. NCJ 247282. [Google Scholar]
- 32.Bloom B, Owen B, Covington S, Raeder M. Gender Responsive Strategies: Research, Practice, and Guiding Principles for Women Offenders. Washington, DC: National Institute of Corrections, US Department of Justice; 2002. [Google Scholar]
- 33.Langevin R, Langevin M, Curnoe S, Bain J. The prevalence of diabetes among sexual and violent offenders and its co-occurrence with cognitive impairment, mania, psychotic symptoms and aggressive behavior. Int J Prison Health. 2008;4(2):83–95. doi: 10.1080/17449200802038215. [DOI] [PubMed] [Google Scholar]
- 34.Connecticut Department of Correction. Statistics. 2013. Available at: http://www.ct.gov/doc/cwp/view.asp?a=1492&Q=270036&docNav. Accessed June 21, 2013.
- 35.Bureau of Justice Statistics. Terms and definitions: corrections. Available at: http://www.bjs.gov/index.cfm?ty=tdtp&tid=1. Accessed February 23, 2015.
- 36.Taxman FS, Cropsey KL, Young DW, Wexler H. Screening, assessment, and referral practices in adult correctional settings: a national perspective. Crim Justice Behav. 2007;34(9):1216–1234. doi: 10.1177/0093854807304431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rhodes AG, Taxman FS, Friedmann PD, Cropsey KL. HCV in incarcerated populations: an analysis of gender and criminality on risk. J Psychoactive Drugs. 2008;40(4):493–501. doi: 10.1080/02791072.2008.10400655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Andrews D, Bonta J. The LSI-R: The Level of Service Inventory–Revised. Toronto, Canada: Multi-Health Systems; 1995. [Google Scholar]
- 39.Carson E, Sabol W.Prisoners in 2011 Washington, DC: US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2012NCJ 239808. [Google Scholar]
- 40.Zahari MM, Hwan Bae W, Zainal NZ, Habil H, Kamarulzaman A, Altice FL. Psychiatric and substance abuse comorbidity among HIV seropositive and HIV seronegative prisoners in Malaysia. Am J Drug Alcohol Abuse. 2010;36(1):31–38. doi: 10.3109/00952990903544828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aberg JA, Kaplan JE, Libman H et al. Primary care guidelines for the management of persons infected with human immunodeficiency virus: 2009 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2009;49(5):651–681. doi: 10.1086/605292. [DOI] [PubMed] [Google Scholar]
- 42.Ettner SL, Huang D, Evans E et al. Benefit-cost in the California Treatment Outcome Project: does substance abuse treatment “pay for itself”? Health Serv Res. 2006;41(1):192–213. doi: 10.1111/j.1475-6773.2005.00466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rossman S, Roman J, Zweig J, Rempel M, Lindquist C. The Multi-Site Adult Drug Court Evaluation: Executive Summary. Washington, DC: Urban Institute, Justice Policy Center; 2011. [Google Scholar]
- 44.Drug Policy Alliance. Drug Courts Are Not the Answer: Toward a Health-Centered Approach to Drug Use. New York, NY: Drug Policy Alliance; 2011. [Google Scholar]
- 45.National Association of Drug Court Professionals. Adult Drug Court Best Practice Standards, Volume I. Alexandria, VA: National Association of Drug Court Professionals; 2013. [Google Scholar]
- 46.Maher G, Pearson J, Frier BM. Diabetes mellitus and criminal responsibility. Med Sci Law. 1984;24(2):95–101. doi: 10.1177/002580248402400206. [DOI] [PubMed] [Google Scholar]
- 47.Pandya NS, Vrbancic M, Ladino LD, Tellez-Zenteno JF. Epilepsy and homicide. Neuropsychiatr Dis Treat. 2013;9:667–673. doi: 10.2147/NDT.S45370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Olson MB, Kelsey SF, Matthews KA et al. Lipid-lowering medication use and aggression scores in women: a report from the NHLBI-sponsored WISE study. J Womens Health (Larchmt) 2008;17(2):187–194. doi: 10.1089/jwh.2007.0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gaskin DJ, Thorpe RJ, Jr, McGinty EE et al. Disparities in diabetes: the nexus of race, poverty, and place. Am J Public Health. 2014;104(11):2147–2155. doi: 10.2105/AJPH.2013.301420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cohen MS, Chen YQ, McCauley M et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Salisbury EJ, Van Voorhis P. Gendered pathways: a quantitative investigation of women probationers’ paths to incarceration. Crim Justice Behav. 2009;36(6):541–566. [Google Scholar]
- 52.Daly K. Gender, Crime, and Punishment. New Haven, CT: Yale University Press; 1994. [Google Scholar]
- 53.Simpson SS, Yahner JL, Dugan L. Understanding women’s pathways to jail: analysing the lives of incarcerated women. Aust N Z J Criminol. 2008;41(1):84–108. [Google Scholar]
- 54.Fuentes CM. Nobody’s child: the role of trauma and interpersonal violence in women’s pathways to incarceration and resultant service needs. Med Anthropol Q. 2014;28(1):85–104. doi: 10.1111/maq.12058. [DOI] [PubMed] [Google Scholar]
- 55.Epperson MW, Khan MR, Miller DP, Perron BE, El-Bassel N, Gilbert L. Assessing criminal justice involvement as an indicator of human immunodeficiency virus risk among women in methadone treatment. J Subst Abuse Treat. 2010;38(4):375–383. doi: 10.1016/j.jsat.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.El-Bassel N, Wechsberg WM, Shaw SA. Dual HIV risk and vulnerabilities among women who use or inject drugs: no single prevention strategy is the answer. Curr Opin HIV AIDS. 2012;7(4):326–331. doi: 10.1097/COH.0b013e3283536ab2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Havens JR, Leukefeld CG, Oser CB et al. Examination of an interventionist-led HIV intervention among criminal justice-involved female prisoners. J Exp Criminol. 2009;5(3):245–272. doi: 10.1007/s11292-009-9081-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Knudsen HK, Staton-Tindall M, Oser CB, Havens JR, Leukefeld CG. Reducing risky relationships: a multisite randomized trial of a prison-based intervention for reducing HIV sexual risk behaviors among women with a history of drug use. AIDS Care. 2014;26(9):1071–1079. doi: 10.1080/09540121.2013.878779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fasula AM, Fogel CI, Gelaude D, Carry M, Gaiter J, Parker S. Project Power: adapting an evidence-based HIV/STI prevention intervention for incarcerated women. AIDS Educ Prev. 2013;25(3):203–215. doi: 10.1521/aeap.2013.25.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lichtenstein B, Malow R. A critical review of HIV-related interventions for women prisoners in the United States. J Assoc Nurses AIDS Care. 2010;21(5):380–394. doi: 10.1016/j.jana.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Taxman FS, Henderson CE, Belenko S. Organizational context, systems change, and adopting treatment delivery systems in the criminal justice system. Drug Alcohol Depend. 2009;103(suppl 1):S1–S6. doi: 10.1016/j.drugalcdep.2009.03.003. [DOI] [PubMed] [Google Scholar]