Abstract
In October 2010, an employee at Facility A in Alaska that performs fire assay analysis, an industrial technique that uses lead-containing flux to obtain metals from pulverized rocks, was reported to the Alaska Section of Epidemiology (SOE) with an elevated blood lead level (BLL) ≥10 micrograms per deciliter (μg/dL). The SOE initiated an investigation; investigators interviewed employees, offered blood lead screening to employees and their families, and observed a visit to the industrial facility by the Alaska Occupational Safety and Health Section (AKOSH). Among the 15 employees with known work responsibilities, 12 had an elevated BLL at least once from October 2010 through February 2011. Of these 12 employees, 10 reported working in the fire assay room. Four children of employees had BLLs ≥5 μg/dL. Employees working in Facility A's fire assay room were likely exposed to lead at work and could have brought lead home. AKOSH inspectors reported that they could not share their consultative report with SOE investigators because of the confidentiality requirements of a federal regulation, which hampered Alaska SOE investigators from fully characterizing the lead exposure standards.
Occupational lead exposure continues to threaten workers' health.1–3 In the United States, the Occupational Safety and Health Administration (OSHA) prescribes standards for permissible exposure limits for lead in the workplace and specifies that a blood lead level (BLL) of 40 micrograms per deciliter (μg/dL) triggers more frequent (i.e., every two months rather than every six months) blood lead testing. OSHA standards require that workers with a BLL ≥60 μg/dL, or an average BLL for the last three tests or all tests during the previous six months (whichever is longer) of ≥50 μg/dL, be removed from the lead exposure area, unless the most recent test indicated a BLL ≤40 μg/dL.4 However, research has increased concern regarding lead toxicity at lower doses and has supported a reevaluation of the level at which BLLs can be considered safe.5 The National Institute for Occupational Safety and Health (NIOSH) defines an elevated BLL in an adult as ≥10 μg/dL.6 In addition to adverse impacts on the health of the workers themselves, children of lead-exposed workers have disproportionately higher BLLs when compared with other children.7–9
Elevated BLLs among adults are associated with muscle and joint pain, reproductive problems, and neurologic symptoms, including memory loss.10 Negative health effects have been observed among adults with only modestly elevated BLLs,11–13 with increased odds of an ill effect occurring at levels as low as 1.6–2.4 μg/dL.11 Among children, elevated BLLs can result in devastating health effects, including brain and nervous system damage, slow growth, and hearing problems.10 Research indicates that there is no safe level of lead among children.14 Despite considerable data on the deleterious health effects of lead regarding both children and adults, harmful occupational exposures that are inadequately controlled continue to put workers and their families at risk. A BLL of ≥5 μg/dL is the reference level that the Advisory Committee on Childhood Lead Poisoning Prevention has recommended to identify children with elevated BLLs.14 Elevated BLLs ≥10 μg/dL for children and adults are reportable in Alaska under Alaska Administrative Code 27.014.15
INVESTIGATION OF AN ELEVATED BLL
During October 2010, a BLL of 41.1 μg/dL in an Alaska employee (“Employee A”) was reported to the Alaska Division of Public Health, Section of Epidemiology (SOE) Adult Blood Lead Epidemiology and Surveillance (ABLES) program. The SOE maintains data on notifiable conditions, conducts outbreak investigations, and drafts reports related to topics of public health interest. During routine follow-up, SOE determined that Employee A worked at an Alaska facility (“Facility A”) that provides geochemical laboratory services to mining operations, including an analytical process referred to as “fire assay.” Fire assay uses a dry, lead oxide-containing flux to recover metals from samples of pulverized rocks. SOE received a report that a second employee (“Employee B”) at Facility A also had an elevated BLL (75 μg/dL) obtained during October 2010.
When SOE contacted the Facility A manager on the day after the original report, the manager stated that he had removed Employee A from his primary assignment in the fire assay laboratory and reassigned him elsewhere. During the discussion with SOE, the manager requested assistance in developing an environmental health and safety program for the facility. Because the Division of Public Health does not have an industrial hygienist on staff, SOE referred the manager to the Alaska Division of Labor Standards and Safety, Occupational Safety and Health Section (AKOSH). AKOSH is part of the Alaska Department of Labor and Workforce Development and offers consultative, cost-free visits to facilities to help reduce employee lead exposure and other hazards. SOE also recommended that the employer offer blood lead screening to all employees. The employer screened 11 of 18 employees at Facility A during December 2010; the remaining employees had either been tested recently by their own provider or had refused to be tested. At the December 2010 screening, nine employees had BLLs ≥10 μg/dL, the definition of an elevated BLL used by the ABLES program.6 SOE investigated to evaluate potential lead exposures at Facility A, to assess if employees' families had elevated BLLs, and to prevent further cases of elevated BLLs.
METHODS
On January 12, 2011, SOE staff traveled to Facility A to observe a visit to the facility by AKOSH, interview the Facility A manager and employees, and offer blood lead testing to Facility A employees and their household members. The AKOSH inspector collected air samples in the breathing zone of an employee working in the fire assay laboratory to estimate the airborne lead levels to which workers were exposed. The inspector also assessed general laboratory practices, lead and non-lead workplace hazards (e.g., use of respiratory protection during pulverization of rock samples), and the availability of written programs demonstrating compliance with occupational safety standards. SOE investigators used a structured questionnaire to interview employees, to assess both occupational and nonoccupational lead exposures, and to identify symptoms of lead poisoning (e.g., headache, joint pain, and confusion). -Nonoccupational exposures included target shooting or hunting, working with stained glass, use of lead-based paint, making pottery with lead glaze, printmaking, casting fishing sinkers or bullets, lead soldering, and residential remodeling.
Also on January 12, SOE offered blood lead screening to Facility A employees and their families; venous blood was drawn from adults and capillary specimens were taken from children. Household member blood draws were conducted at the local public health center. The definition of an elevated BLL was ≥10 μg/dL among people aged ≥16 years6 and, at the time of the investigation, also among children.16 However, a revised CDC recommendation for elevated BLL among children, issued in early 2012, set the level at ≥5 μg/dL.14 This revised definition is used for results presented in this report. Children with BLLs ≥10 μg/dL were retested using venous samples because capillary samples can be contaminated during blood collection. SOE offered a second round of blood lead screening to employees and their families during February 2011. All blood lead testing was performed at the Alaska State Public Health Laboratory using inductively coupled plasma mass spectrometry17,18 (Figure 1).
Figure 1.
Timeline of events during the Alaska Section of Epidemiology and Alaska Occupational Safety and Health investigations of possible lead exposures at Facility A in Interior Alaska,a October 2010 through February 2011
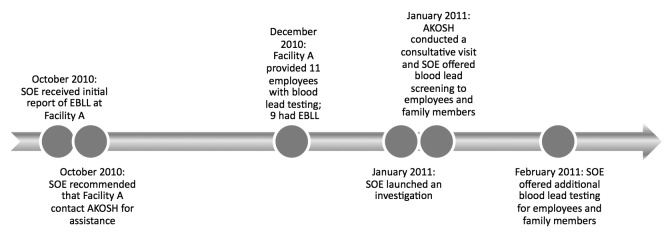
aFacility A performs fire assay analysis, an industrial technique that uses lead-containing flux to obtain metals from pulverized rocks.
SOE = Alaska Section of Epidemiology
EBLL = elevated blood lead level
AKOSH = Alaska Division of Labor Standards and Safety, Occupational Safety and Health Section
RESULTS
During the AKOSH visit at Facility A on January 12, investigators noted that Facility A did not have a written lead compliance program. A written lead compliance program is required by OSHA and must include a description of operations in which lead is emitted and the means by which the facility will achieve compliance with OSHA standards. Additionally, no documentation was available to indicate that the ventilation hoods in the fire assay laboratory were functioning properly, which OSHA also requires. The mixing of the pulverized rock and dry, lead oxide-containing flux took place in a plastic bag, and the resulting mixture was distributed into crucibles under a ventilation hood. The crucibles were then heated in a furnace, and the resulting product was then analyzed to determine the composition of the original rock sample. Personal protective equipment used by employees working in the fire assay laboratory included half-mask respirators and coveralls. Employees did not have a lead-free area in which to store their nonwork clothes or a lead-free area in which to shower. AKOSH reported that it was unable to share its air quality testing results or its full report with SOE, citing a federal regulation that ensures confidentiality of consultative documents.19
The Facility A manager reported that when he had started working at the facility in early 2010, workers were not wearing coveralls (i.e., they wore their street clothes) and were mixing together the rock samples and lead-containing flux without wearing fit-tested respirators. Fourteen employees were interviewed (13 in January and one in February), 11 of whom had an elevated BLL; the employees not interviewed were either unavailable or refused to be interviewed. Nine of the 11 employees with elevated BLLs reported working in the fire assay room at that time or in the past, compared with zero of three employees without an elevated BLL. The employee who was initially reported to SOE with an elevated BLL had reported working in fire assay, but no longer worked at Facility A and was unable to be interviewed. Approximately one-third of all employees reported a potential nonoccupational lead exposure. Five employees reported residing in a home that was constructed before 1978 (the year that lead-based paint was banned in the United States), six were unsure when their residence had been built, and three knew that their home had been built after 1978 (Table).
Table.
Characteristics reported by Facility A employees (n=14) during in-person interviews conducted in an investigation of elevated blood lead levels in Interior Alaska, 2011
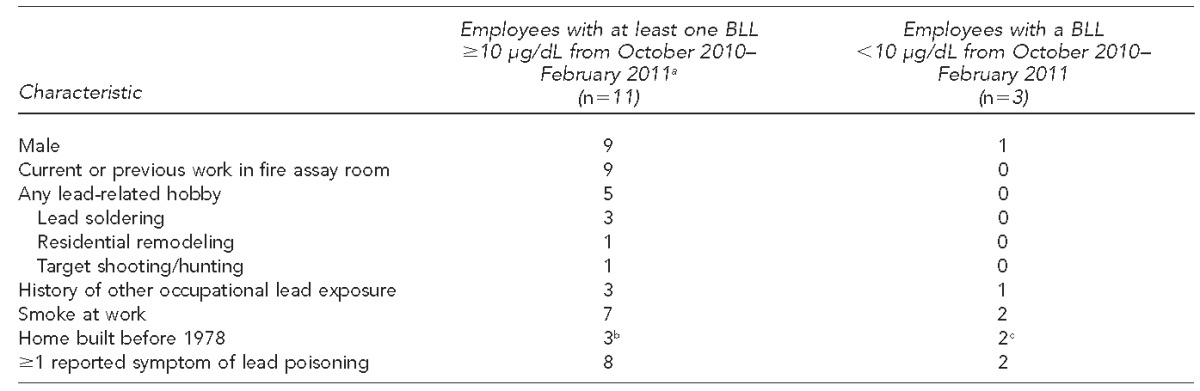
aOne additional employee (Employee A) no longer worked at the facility and was unavailable for interview; he is excluded from this table. During his original contact with the Alaska Section of Epidemiology, he reported that he had worked in the fire assay room.
bFive employees were unsure what year their homes were built.
cOne employee was unsure when his home was built.
BLL = blood lead level
μg/dL = microgram/deciliter
On January 12, SOE also collected blood samples from seven current employees and four family members (i.e., two children and two adults) for lead testing. Three other employees had received independent lead testing in January. BLLs of the 10 employees tested during January ranged from 6.0 to 37.7 μg/dL. Seven employees met the case definition for an elevated BLL; six had been tested previously and four had BLLs that had decreased since their previous test (Figure 2). Three of these four employees had been removed from the fire assay laboratory after having been identified as having an elevated BLL in October or December. The BLLs of three other employees had increased since December 2010 (Figure 2); all three employees were working in the fire assay laboratory.
Figure 2.
Employee blood lead levels at Facility A, by employees' exposure to the fire assay room and month of blood lead level testing, Interior Alaska, October 2010 through February 2011
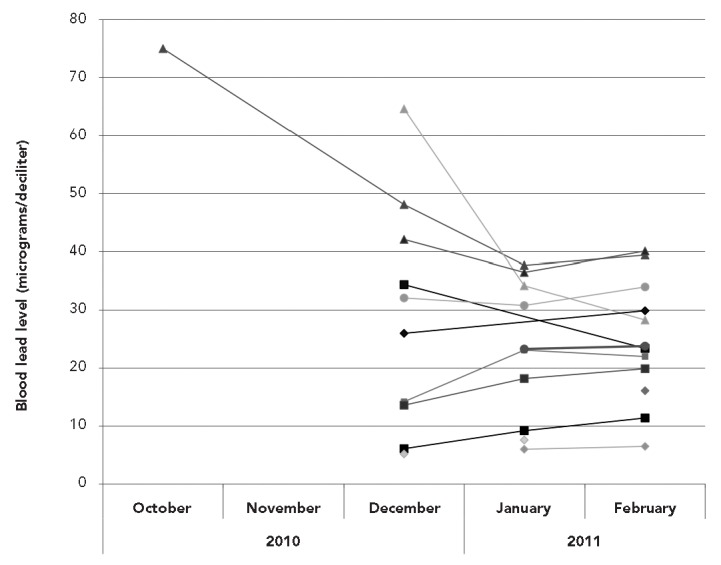
■ Current work in fire assay
▲ Removed from fire assay following previous elevated blood lead level
● History of working in fire assay or moderate presence in fire assay room
◆ History of no or minimal work in fire assay
Capillary blood lead measures were obtained for two children, Child A and Child C, on January 12. Child A, aged <5 years, had a BLL of 26.7 μg/dL and was the child of an employee who had been removed from the fire assay laboratory because of an elevated BLL. Confirmatory testing—using venous samples—was then conducted for Child A and a younger sibling, Child B, who had not been previously tested, in late January. Child A had a BLL of 9.7 μg/dL and Child B had a BLL of 11.4 μg/dL (Figure 3). The other child tested during screening in January (Child C) was aged <5 years and had a BLL of 7.0 μg/dL. Child C was the child of an employee who did not work in the fire assay laboratory and did not have an elevated BLL. Neither spouse of the two employees whose children had an elevated BLL had elevated BLLs.
Figure 3.
Blood lead levels of employees' children from samples collected during an investigation of elevated blood lead levels in employees of Facility A, Interior Alaska, January through February 2011
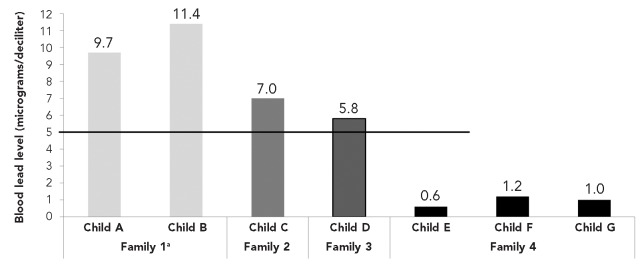
Note: The line at 5 micrograms/deciliter reflects the current Centers for Disease Control and Prevention standard for an elevated blood lead level (BLL) in children.
aThe mother of these children (not an employee at Facility A) was tested and did not have an elevated BLL.
On February 3, 2011, SOE collected blood samples from 18 people, including eight previously tested employees, four employees not tested by SOE during the January visit, and six previously untested family members (i.e., four children and two adults). BLLs from employees tested that day ranged from 6.5 to 40.1 μg/dL (Figure 2). The BLLs of the four children (children D–G) tested ranged from 0.6 to 5.8 μg/dL (Figure 3). Child D, an infant from the household of an employee with a history of working in fire assay, had an elevated BLL of 5.8 μg/dL. Neither of the two adults tested from the employees' households had elevated BLLs (range: 1.2–3.7 μg/dL).
SOE made recommendations to Facility A to assist the employer in reducing lead exposure in the -workplace. These recommendations included thoroughly cleaning the fire assay room after remediation of the ventilation system and ensuring that employees' nonwork clothes and shoes were not stored in the same space as contaminated work clothes and shoes. SOE advised Facility A employees to help protect themselves and their families by practicing rigorous hygiene at work and removing lead from their homes and vehicles using approved methods.
DISCUSSION
This investigation identified 12 Facility A employees with elevated BLLs; the majority of these employees had worked in the facility's fire assay room, where lead-containing flux was used to recover metals from pulverized rock samples, a process that generates lead dust and fumes. Given that employees with elevated BLLs were unlikely to report nonoccupational exposures, Facility A was the likely source of exposure. Ten of 12 employees with an elevated BLL either worked or had worked in the fire assay laboratory. These lead exposures might have been exacerbated by historical practices (e.g., mixing the flux with the rock samples without adequate personal protective equipment) and might have been prevented had Facility A established a written lead compliance program, which OSHA requires at all facilities where occupational exposure to lead occurs.
According to the current standard for an elevated BLL in children (≥5 μg/dL),14 four employees' children also had elevated BLLs. The major sources of lead exposure among children aged <6 years in the contiguous United States include the ingestion of lead-contaminated dust—often from deteriorated lead-based paint—and exposure to lead-contaminated soil,20 both of which are uncommon in Alaska, where the primary risk factors are immigration, air gun pellets, and pica.21 The percentage of children in Alaska with elevated BLLs on the basis of the initial definition (≥10 μg/dL) is lower than the national percentage.22 Moreover, children of lead-exposed workers have been reported to have disproportionately higher BLLs than children of nonexposed workers.7–9 This information, along with the history of Facility A employees routinely going home without changing their clothes and the lack of a lead-free area in which to store their nonwork clothes during work hours, suggests that the primary source of exposure among the Facility A workers' children with elevated BLLs was likely lead brought home from work by their parents.
AKOSH was unable to share its report, which included the air quality data and the AKOSH recommendations for remediation, with SOE, citing 29 C.F.R. 1908.6(g)(2), a federal regulation that ensures confidentiality of consultative documents.19 States such as Alaska that develop their own occupational safety and health plans must follow federal regulations related to OSHA. The prohibition of AKOSH consultants from sharing information with SOE poses a dilemma, and this situation likely is disadvantageous for other health departments without the resources or expertise (e.g., an industrial hygienist) to conduct environmental investigations in occupational settings. Although NIOSH, a nonregulatory part of the Centers for Disease Control and Prevention, provided guidance to SOE by telephone, the Facility A manager elected not to request that NIOSH conduct a health hazard evaluation, the results of which would have been made available to SOE. Health hazard evaluations are workplace assessments, conducted either remotely or through onsite visits, that aim to identify and characterize any dangerous materials or conditions. Workers can also request a health hazard evaluation, although such a request was not made to NIOSH in this case. Ensuring that workers understand their access to this resource will be a priority during future investigations. Public health investigators should explain to employees the differences between the types of investigations the agencies can provide and give them written information on the health hazard evaluation program, including how to request a health hazard evaluation.
Whereas Facility A management cooperated during the investigation and implemented changes in a timely manner to help protect employees, they chose not to share the AKOSH report with SOE and declined to share their more recent air-quality testing (although they reported improvements in the air quality). Facility A's decision not to provide this information prevents comparable facilities from learning how they can protect their own employees by using similar remediation measures, and prevents collaborative public health action to help exposed employees and their families. In the future, public health investigators should discuss the importance of sharing the findings with facility management before a consultative visit. In the longer term, although it is important to encourage facilities to participate in the consultative process by protecting their confidentiality, adjustments to the regulations could be considered that would allow information sharing between agencies involved in these types of investigations.
Limitations
This study was subject to several limitations. One limitation of the SOE investigation was the omission of questions on the questionnaire administered to employees about detailed information on job responsibilities and the total number of household members. Additionally, at the time of the AKOSH visit, SOE staff could have collected more environmental information themselves, such as the types of respirators worn in the fire assay room.
CONCLUSION
Lead exposure, identified by both elevated BLLs and air sampling, during fire assay analysis was documented in the occupational health literature approximately two decades ago.23 This report serves as a reminder to employers in this industry that lead exposure during fire assay analysis continues to pose a substantial health hazard to workers and underscores the importance of ensuring that fire assay workers and their families are adequately protected against lead exposure. Employers should repeatedly educate all employees who might come in contact with lead in the workplace about the dangers of lead exposure and effective ways to reduce the risk of exposure for themselves and their families.
Footnotes
The authors thank Diana Bensyl, PhD, C. Kay Smith, and M. Paul Reid for their helpful and thorough review of the manuscript; and David Kern, MD, for assisting with the preparation of the manuscript by providing relevant literature. This study was considered exempt from Institutional Review Board review.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Rabito FA, Perry S, Salinas O, Hembling J, Schmidt N, Parsons PJ, et al. A longitudinal assessment of occupation, respiratory symptoms, and blood lead levels among Latino day laborers in a non-agricultural setting. Am J Ind Med. 2011;54:366–74. doi: 10.1002/ajim.20919. [DOI] [PubMed] [Google Scholar]
- 2.Kar-Purkayastha I, Balasegaram S, Sen D, Rehman AJ, Dargan PI, Johnston D, et al. Lead: ongoing public and occupational health issues in vulnerable populations: a case study. J Public Health (Oxf) 2012;34:176–82. doi: 10.1093/pubmed/fdr077. [DOI] [PubMed] [Google Scholar]
- 3.Wu Y, Liu Y, Ni N, Bao B, Zhang C, Lu L. High lead exposure is associated with telomere length shortening in Chinese battery manufacturing plant workers. Occup Environ Med. 2012;69:557–63. doi: 10.1136/oemed-2011-100478. [DOI] [PubMed] [Google Scholar]
- 4. 29 C.F.R. 1910.1025 App. C (1995)
- 5.Kosnett MJ, Wedeen RP, Rothenberg SJ, Hipkins KL, Materna BL, Schwartz BS, et al. Recommendations for medical management of adult lead exposure. Environ Health Perspect. 2007;115:463–71. doi: 10.1289/ehp.9784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (US) Adult blood lead epidemiology and surveillance (ABLES) [cited 2012 Sep 1] Available from: URL: http://www.cdc.gov/niosh/topics/ABLES/description.html.
- 7.Gulson BL, Mizon KJ, Korsch MJ, Howarth D. Importance of monitoring family members in establishing sources and pathways of lead in blood. Sci Total Environ. 1996;188:173–82. doi: 10.1016/0048-9697(96)05170-4. [DOI] [PubMed] [Google Scholar]
- 8.Whelan EA, Piacitelli GM, Gerwel B, Schnorr TM, Mueller CA, Gittleman J, et al. Elevated blood lead levels in children of construction workers. Am J Public Health. 1997;87:1352–5. doi: 10.2105/ajph.87.8.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan J, Sim M, Golec R, Forbes A. Predictors of lead absorption in children of lead workers. Occup Med (Lond) 2000;50:398–405. doi: 10.1093/occmed/50.6.398. [DOI] [PubMed] [Google Scholar]
- 10.Environmental Protection Agency (US) Lead in paint, dust, and soil basic information [cited 2012 Jul 2] Available from: URL: http://www.epa.gov/lead/pubs/leadinfo.htm.
- 11.Navas-Acien A, Tellez-Plaza M, Guallar E, Muntner P, Silbergeld E, Jaar B, et al. Blood cadmium and lead and chronic kidney disease in US adults: a joint analysis. Am J Epidemiol. 2009;170:1156–64. doi: 10.1093/aje/kwp248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lustberg M, Silbergeld E. Blood lead levels and mortality. Arch Intern Med. 2002;162:2443–9. doi: 10.1001/archinte.162.21.2443. [DOI] [PubMed] [Google Scholar]
- 13.Menke A, Muntner P, Batuman V, Silbergeld EK, Guallar E. Blood lead below 0.48 micromol/L (10 microg/dL) and mortality among US adults. Circulation. 2006;114:1388–94. doi: 10.1161/CIRCULATIONAHA.106.628321. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention (US) Low level lead exposure harms children: a renewed call for primary prevention [cited 2012 Jul 2] Available from: URL: http://www.cdc.gov/nceh/lead/acclpp/final_document_030712.pdf.
- 15. 7 Alaska Administrative Code, 27.014 (2007)
- 16.Centers for Disease Control and Prevention (US) Lead [cited 2012 Jul 2] Available from: URL: http://www.cdc.gov/nceh/lead.
- 17.Barany E, Bergdahl IA, Schütz A, Skerfving S, Oskarsson A. Inductively coupled plasma mass spectrometry for direct multi-element analysis of diluted human blood and serum. J Anal At Spectrom. 1997;12:1005–9. [Google Scholar]
- 18.Centers for Disease Control and Prevention (US) Laboratory procedure manual [cited 2012 Jul 2] Available from: URL: http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/pbcd_d_met_lead_cadmium.pdf.
- 19. 29 C.F.R. 1908.6(g)(2) (2000)
- 20.Advisory Committee on Childhood Lead Poisoning Prevention. Interpreting and managing blood lead levels <10 microg/dL in children and reducing childhood exposures to lead: recommendations of CDC's Advisory Committee on Childhood Lead Poisoning Prevention [published erratum appears in MMWR Morb Mortal Wkly Rep 2007;56(47):1241] MMWR Recomm Rep. 2007;56(RR-8):1–16. [PubMed] [Google Scholar]
- 21.Alaska Department of Health and Social Services, Division of Public Health. Updated recommendations on blood lead screening for Medicaid-eligible children. State of Alaska Epidemiology Bulletin 2010 Jan 21 [cited 2012 Jul 2] Available from: URL: http://www.epi.hss.state.ak.us/bulletins/docs/b2010_01.pdf.
- 22.Meyer PA, Pivetz T, Dignam TA, Homa DM, Schoonover J, Brody D. Surveillance for elevated blood lead levels among children—United States, 1997–2001. MMWR Surveill Summ. 2003;5(10):1–21. [PubMed] [Google Scholar]
- 23.Kern DG. Lead poisoning in precious metals refinery assayers: a failure to notify workers at high risk. Am J Ind Med. 1994;25:759–67. doi: 10.1002/ajim.4700250515. [DOI] [PubMed] [Google Scholar]


