Abstract
Objectives
Latinos are at an elevated risk for HIV infection. Continued HIV/AIDS stigma presents barriers to HIV testing and affects the quality of life of HIV-positive individuals, yet few interventions addressing HIV/AIDS stigma have been developed for Latinos.
Methods
An intervention led by community health workers (promotores de salud, or promotores) targeting underserved Latinos in three southwestern U.S. communities was developed to decrease HIV/AIDS stigma and increase HIV knowledge and perception of risk. The intervention was led by HIV-positive and HIV-affected (i.e., those who have, or have had, a close family member or friend with HIV/AIDS) promotores, who delivered interactive group-based educational sessions to groups of Latinos in Spanish and English. To decrease stigma and motivate behavioral and attitudinal change, the educational sessions emphasized positive Latino cultural values and community assets. The participant pool comprised 579 Latino adults recruited in El Paso, Texas (n=204); San Ysidro, California (n=175); and Los Angeles, California (n=200).
Results
From pretest to posttest, HIV/AIDS stigma scores decreased significantly (p<0.001). Significant increases were observed in HIV/AIDS knowledge (p<0.001), willingness to discuss HIV/AIDS with one's sexual partner (p<0.001), and HIV risk perception (p=0.006). Willingness to test for HIV in the three months following the intervention did not increase. Women demonstrated a greater reduction in HIV/AIDS stigma scores when compared with their male counterparts, which may have been related to a greater increase in HIV/AIDS knowledge scores (p=0.016 and p=0.007, respectively).
Conclusion
Promotores interventions to reduce HIV/AIDS stigma and increase HIV-related knowledge, perception of risk, and willingness to discuss sexual risk with partners show promise in reaching underserved Latino communities.
Human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) has disproportionately affected U.S. Latinos during the last 25 years. Although Latinos constitute 16% of the U.S. population, they account for 19% of those living with HIV and 21% of new HIV infections.1 Since 2006, the Centers for Disease Control and Prevention (CDC) has recommended HIV testing for all people aged 13–64 years.2 However, nearly half (46%) of Latino adults aged 18–64 years have never been tested, compared with 23% of black and 50% of white adults.3 Additionally, HIV testing often occurs at a late stage among HIV-positive Latinos. More than one-third (36%) of HIV-positive Latinos were diagnosed with AIDS within one year of learning their HIV status, compared with 32% of white people and 31% of black people.3 Late HIV testing hinders treatment options and may contribute to unknowing HIV transmission.
Factors contributing to low HIV testing rates among Latinos include poverty, lack of health-care access, and limited availability of culturally and linguistically responsive services.1,4–6 HIV/AIDS stigma is another factor.7,8 UNAIDS (Joint United Nations Programme on AIDS) defines HIV stigma as the “devaluation of people either living with or associated with HIV/AIDS.”9 Stigma often results from fears about HIV as well as the associations of HIV with stigmatized groups such as homosexuals, sex workers, and injection drug users.9,10
HIV/AIDS stigma has negative consequences both at a population level and for individuals who are its targets, including people living with HIV/AIDS. Stigmatizing attitudes toward people living with HIV/AIDS are associated with decreased HIV testing, limited utilization of HIV prevention services, and high-risk sexual behaviors.7,10,11 Additionally, for people living with HIV/AIDS, the stigma associated with HIV/AIDS contributes to unwillingness to disclose HIV status, unsafe sexual behaviors, delays in care seeking, reduced treatment adherence, mental health issues, and difficulties obtaining social support.9,11–14
Despite significant implications, few interventions have been developed to reduce HIV/AIDS stigma.10,11,15 Existing interventions have often focused on specific populations (e.g., university students and health-care providers), with few interventions focused on Latinos,11,15,16 who have high levels of stigmatizing attitudes toward people living with HIV/AIDS1,17,18 that contribute to negative outcomes.7,19
Among Latinos, research indicates that community health workers (promotores de salud, hereinafter “promotores”) are an effective and culturally acceptable means of reaching the population with health information and motivating health behaviors.20,21 Promotores are well positioned to promote changes in their communities because they share language and cultural values, are held in high esteem, and are perceived as role models.21 Promotores have been used to address health conditions ranging from chronic diseases to preventive screenings.20–22 Several interventions have incorporated promotores into HIV prevention, finding significant changes in HIV risk behaviors, HIV counseling and testing, and other psychosocial constructs important to prevention.16,23–29 To date, few studies have used promotores in interventions to reduce HIV stigma among Latinos.16
We describe and report findings of an intervention using promotores to reduce HIV/AIDS stigma and increase willingness to seek HIV testing among Latinos in three communities in the southwestern United States: Los Angeles, California; San Ysidro, California; and El Paso, Texas.
PROGRAM DESCRIPTION
Our intervention was informed by Airhihenbuwa and Webster's PEN-3 model30 and Elder et al.'s framework for promoting Latino health through communication.21 The PEN-3 model was created to guide the development of culturally competent HIV prevention programs. The model includes three primary domains: cultural identity, relationships, and cultural empowerment.30 For the project, the model was used to guide the inclusion of cultural components in the formative and development phases, including cultural values, beliefs, and important icons, as well as an emphasis on cultural strengths. Elder's framework outlines the importance of using clear and effective communication messages for individuals, family, peers, organizations, and communities.21 This framework was used to ensure that the project addressed the different socio-environmental influences that have a role in the health of Latinos. We chose as our study's name “Salud es Cultura: ¡Protégete!” (Health Is Culture: Protect Yourself!) to emphasize positive cultural attributes and motivate HIV prevention by emphasizing Latino cultural values, such as the importance of family (familismo), community (communidad), respect (respeto), and trust (confianza). HIV/AIDS prevention was framed using a positive, community, and action-oriented perspective to increase cultural pride, self-care through increased knowledge, and behavior change to reduce the risk for HIV.
Promotores' participation
We partnered with three community-based organizations to develop and implement the intervention. Partners included two Federally Qualified Health Centers serving predominantly Spanish-speaking Latino immigrants (San Ysidro and El Paso) and a nonprofit agency dedicated to HIV prevention serving all Latinos, but focused on the Latino lesbian, gay, bisexual, and transgender population (Los Angeles). HIV-positive and HIV-affected promotores delivered the intervention. Those personally affected by HIV had family or friends who were HIV positive. Staff from the partner agencies identified the promotores. In total, 20 promotores were recruited (five from El Paso, 10 from San Ysidro, and five from Los Angeles). Most of the promotores were bilingual in English and Spanish, and all had demonstrated leadership experience in reaching their respective communities. Eleven promotores were HIV positive, 12 were born in Mexico, and eight were born in the United States. Using community-based participatory research (CBPR) techniques, promotores and staff at collaborating organizations provided input on content development, intervention delivery, and the evaluation protocol through focus groups and group discussions throughout the project.
Based on their extensive experience and high percentage of HIV seropositivity, promotores from San Ysidro participated in two focus groups to collect formative data regarding how to approach stigma. Content analysis revealed stigma as being complex and intertwined with religion and stigmata, potentiating the belief that HIV status could be perceived as divine punishment for sinful behavior. Promotores recommended that the concept of stigma be introduced at the end of the interactive group education sessions, or charlas, only after HIV transmission was clearly defined, as it is often misinterpreted in Spanish as estigmata, or “marks of God.” Introducing the concept of stigma later ensured that participants would not confuse someone with AIDS as having been punished or marked by God, thus exacerbating the overall effects of stigma. Although San Ysidro promotores participated in focus groups, promotores from all sites participated in informal group discussions during preliminary project meetings to review materials, recommend changes, and assist in finalizing the intervention and evaluation.
Modifications to the project title and content of the interactive group education sessions were made based on the promotores' recommendations and their insight regarding the respective target communities. The promotores suggested a title without the word stigma and one that promoted cultural positivity. Based on the promotores' feedback, the interactive group education sessions were adapted to incorporate cultural icons, including famous individuals from diverse Latin American countries, thus reinforcing Latino identity, contributions to society, and cultural pride. Promotores advised avoidance of fear-based messaging due to the daily vulnerabilities faced by underserved Latino communities. Recommendations from all sites stressed that by promoting cultural pride during the interactive group education sessions, common discriminatory myths and stereotypes contributing to HIV risk behavior could be abated to facilitate participants' intake of important HIV-related information. Promotores also recommended using appealing packaging colors and layout to ensure community appeal.
Following final development, all promotores participated in a one-day skills-based training on the study protocol, ethical issues, and intervention delivery techniques. All promotores received a study manual outlining procedures and expectations of promotores, including guidelines for recruitment and interactive group education sessions content delivery. To aid in the delivery of the interactive group education sessions, promotores were trained to use a rotafolio, a full-color, bilingual HIV prevention flip chart developed to incorporate promotores' insights and recommendations. Contents of the flip chart mirrored the topics outlined previously and included a detailed script followed at each interactive group education session. The script allowed promotores to deliver the same content at each interactive group education session and actively engage participants in a sequenced dialogue throughout the session. Role-play, active demonstration, observation, and feedback throughout the training by the research team and site-specific coordinators ensured that all promotores were skilled in interactive group education session delivery and research protocol prior to participant recruitment.
Participant recruitment and eligibility criteria
The promotores used standardized scripts, including an introduction to the promotores and project, and the interactive group education session components to recruit participants from community locations. Participants were recruited in Latino-dominant neighborhoods from public transportation stops, outdoor marketplaces, community centers and events, and laundromats. Individuals were eligible to participate if they were at least 18 years of age, self-identified as Latino/Hispanic, and resided in the service areas of the partnering community-based organizations. After introducing the study, the promotores asked potential participants about their availability and interest in participating in an interactive group education session, which was held from one day to one week following recruitment. On the day of the interactive group education session, all participants provided consent prior to participating and received a hard copy of the consent form. Participants were given t-shirts for their involvement.
Intervention
The intervention consisted of one 60- to 90-minute interactive group education session held at a variety of accessible locations, including community health clinics, community centers, housing complexes, schools, and churches from April to June 2008. Teams of promotores delivered a total of 53 interactive group education sessions, which were given to groups comprising 3–25 participants, with an average of 13 participants per group. To facilitate interactive group education session effectiveness, ensure adequate time and personnel to respond to each participant's questions, and create an opportunity for dialogue, collaborating agencies assiged 2–4 promotores per session, depending on the number of recruits. The majority of interactive group education sessions held in San Ysidro and El Paso were conducted in Spanish. In Los Angeles, half were in English.
Primary interactive group education session components included (1) project introduction; (2) an interactive activity emphasizing healthy Latino cultural values such as familismo, personalismo, and respeto; (3) HIV/AIDS transmission, prevention, and testing information including discussion questions; (4) overview of general Latino cultural attitudes about sexuality, including homosexuality, and an activity to discuss cultural myths and stereotypes; (5) information about how to discuss sex with children; (6) information about the concept of HIV/AIDS stigma; (7) a novelita (story) about an HIV-positive neighbor that was used to stimulate discussion of HIV/AIDS and how HIV stigma can affect prevention; (8) ways to eliminate HIV/AIDS stigma; and (9) strategies to maintain personal and family health.
The majority of participants actively engaged in discussions, shared their experiences, and asked follow-up questions. Each site exceeded its target enrollment, demonstrating high community interest. Additionally, promotores disseminated eight different target group-specific brochures in Spanish and English to each interactive group education session with stories on HIV prevention focused on families, men, women, and young people, as well as outreach cards containing facts about the impact of HIV/AIDS on Latino communities and contact information for local HIV testing sites, including addresses, phone numbers, and HIV testing and counseling services.
METHODS
The evaluation consisted of pretest and posttest surveys immediately before and after the intervention. Surveys were self- or verbally administered (for low literacy) and could be completed in English or Spanish. Details on survey measures, which were adapted from a previous study,16 are shown (Table 1). Items were measured on a five-point Likert scale ranging from 1 (very uncomfortable/completely disagree) to 5 (very comfortable/completely agree). To measure sexual risk behaviors, we asked participants to report the number and sex of their sexual partners in the previous 12 months (i.e., male, female, or both male and female). We also asked participants to report if they had engaged in vaginal and anal sex in the previous six months, how frequently they had used condoms during vaginal and anal sex in the previous six months, and whether or not they had had any HIV-positive sexual partners in the previous six months. We used a six-month rather than 12-month time frame because we anticipated better recall of these behaviors.
Table 1.
Description of HIV-related knowledge, risk, communication, and stigma survey measures included on pretest and posttest surveys conducted with adult Latinos who participated in a community health worker HIV/AIDS intervention in three southwestern U.S. cities, April–June 2008
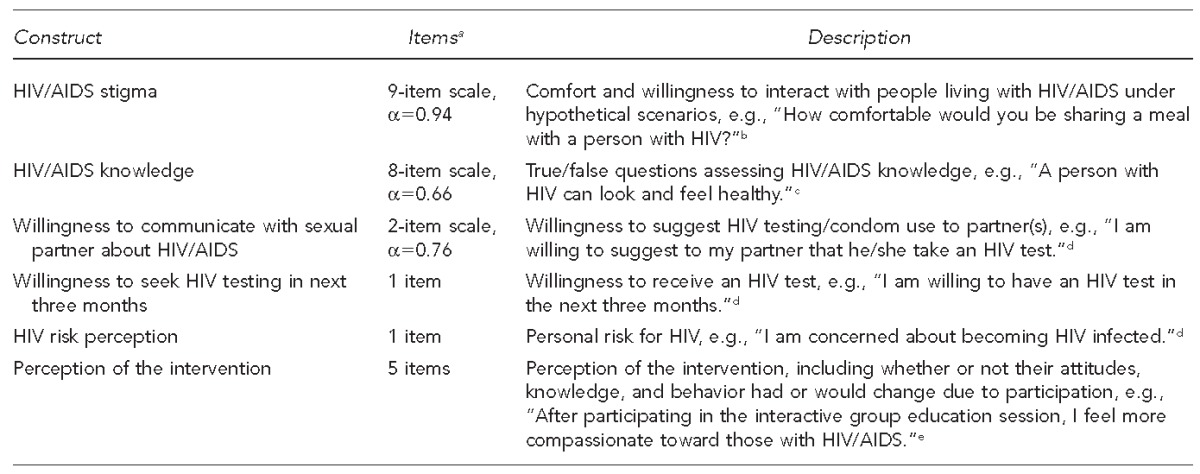
aCronbach's alpha is shown for all variables that were measured using multi-item scales, with the exception of “perception of the intervention,” in which items were not combined into a scale because they measured distinct variables.
bItems were measured on a five-point scale ranging from 1 (very uncomfortable/completely disagree) to 5 (very comfortable/completely agree). Items were reverse coded so that higher scores indicate greater stigma.
cCorrect responses were coded as “1” and incorrect responses were coded as “0.” Scale scores were created by averaging the number of correct responses for nonmissing items and then multiplying that number by 8. Higher scores indicate greater knowledge.
dResponses were scored on a five-point scale from 1 (completely disagree) to 5 (completely agree).
eItems measuring perception of the intervention were included on the posttest only.
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
Data were entered into a database and descriptive statistics (i.e., means and percentages) were estimated to present baseline characteristics of the sample. We compared demographic characteristics and sexual risk behaviors across sites at baseline using the chi-square test. Next, we estimated paired t-tests to compare pretest vs. posttest scores on HIV knowledge, HIV/AIDS stigma, willingness to be tested for HIV, willingness to communicate about HIV with sexual partners, and HIV risk perception. We tested for differences in intervention outcomes across sites, by age group, and by sex by performing analysis of variance or t-tests on gain scores. We calculated gain scores by subtracting pretest from posttest scores.31 Finally, we estimated descriptive statistics for items measured on the posttest only that measured participants' perceptions of the intervention. All analyses were performed using Stata® version 11.2.32
RESULTS
Sample profile
A total of 579 participants attended the interactive group education sessions: 204 in El Paso, 200 in Los Angeles, and 175 in San Ysidro. More than half (57%) were women, most (62%) participants were aged 25–44 years, and 55% were born outside of the United States, of which 97% were from Mexico. On average, foreign-born participants had lived in the United States for 14.8 years (standard deviation [SD] = 11.8). More than one-third (35%) were single, 34% were married, and 14% were cohabiting. Most (67%) had children. Slightly less than half of participants reported Spanish as their preferred language. About one-fifth of participants reported ≤middle school as their highest education level, while 36% had at least some college. Forty-eight percent were uninsured (Table 2).
Table 2.
Social and demographic characteristics of participants in a community health worker HIV/AIDS intervention conducted in three southwestern U.S. cities showing differences across sites in participant characteristics, April–June 2008
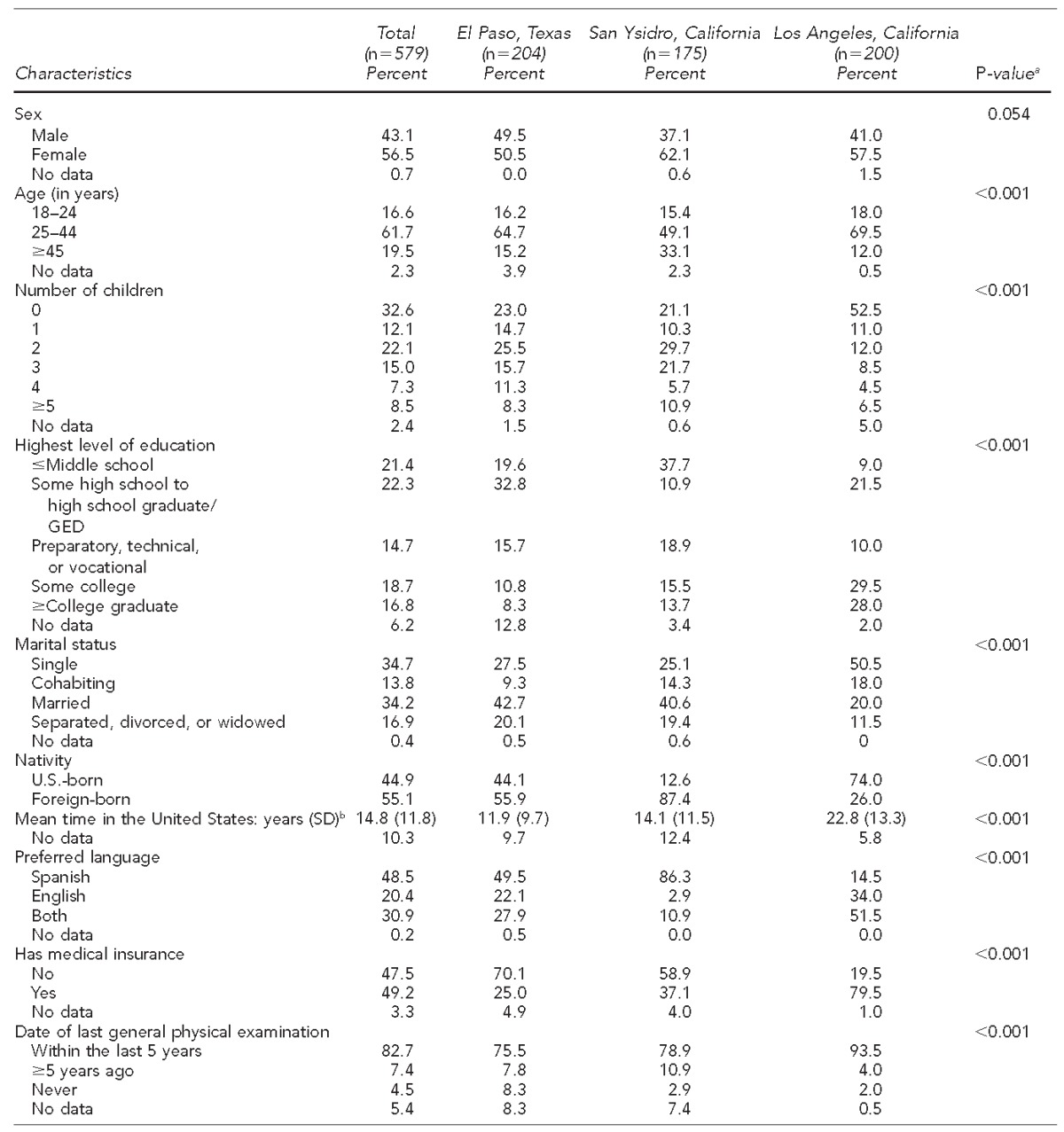
aP-values obtained from Pearson's chi-squared test and one-way analysis of variance to test for statistically significant differences in means or proportions among sites
bAmong participants who were foreign-born
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
GED = general educational development
SD = standard deviation
We found significant differences in baseline characteristics across sites. A higher percentage of participants in Los Angeles vs. San Ysidro and El Paso were single and had no children. Foreign-born participants constituted the majority (87%) of those in San Ysidro, more than half (56%) in El Paso, and about one-quarter (26%) in Los Angeles. Education levels also varied, with participants in Los Angeles reporting the highest education levels and those in San Ysidro the lowest. The percentage of participants aged ≥45 years was more than twice as high in San Ysidro as in the other two sites (Table 2).
Most participants reported either one (54%), no (11%), or two (10%) sexual partners in the previous 12 months; however, 6% reported ≥6 partners. We found significant differences across sites in the number of sexual partners reported in the last 12 months, with those in Los Angeles reporting a higher number of partners (p<0.001). More than three-quarters of participants (77%) reported only heterosexual partners in the previous 12 months, while 20% reported any same-sex partners. The type of sexual partners also varied by site, with a higher percentage of Los Angeles participants (41%) reporting any same-sex partners compared with the other two sites (p<0.001). More than two-thirds (66%) reported having had vaginal sex in the previous six months, and 18% reporting having had anal sex during the same time period. Significant differences were found across sites regarding these measures. In Los Angeles, 31% of participants reported anal sex in the previous six months compared with 12% of participants in El Paso and 11% of participants in San Ysidro (p<0.001). Among participants reporting vaginal sex, 16% reported consistent use of condoms during sex, while 38% of those reporting anal sex reported consistent condom use. Overall, 62% of participants reported ever having been tested for HIV, but this percentage varied significantly across sites, with the highest percentage in Los Angeles (p=0.004). Among those tested, 5% reported not knowing or not receiving their last HIV test result. Two percent of participants reported an HIV-positive sexual partner in the last six months (Table 3).
Table 3.
Recent sexual behaviors reported by participants in a community health worker HIV/AIDS intervention conducted in three southwestern U.S. cities showing differences across sites in sexual behaviors, April–June 2008
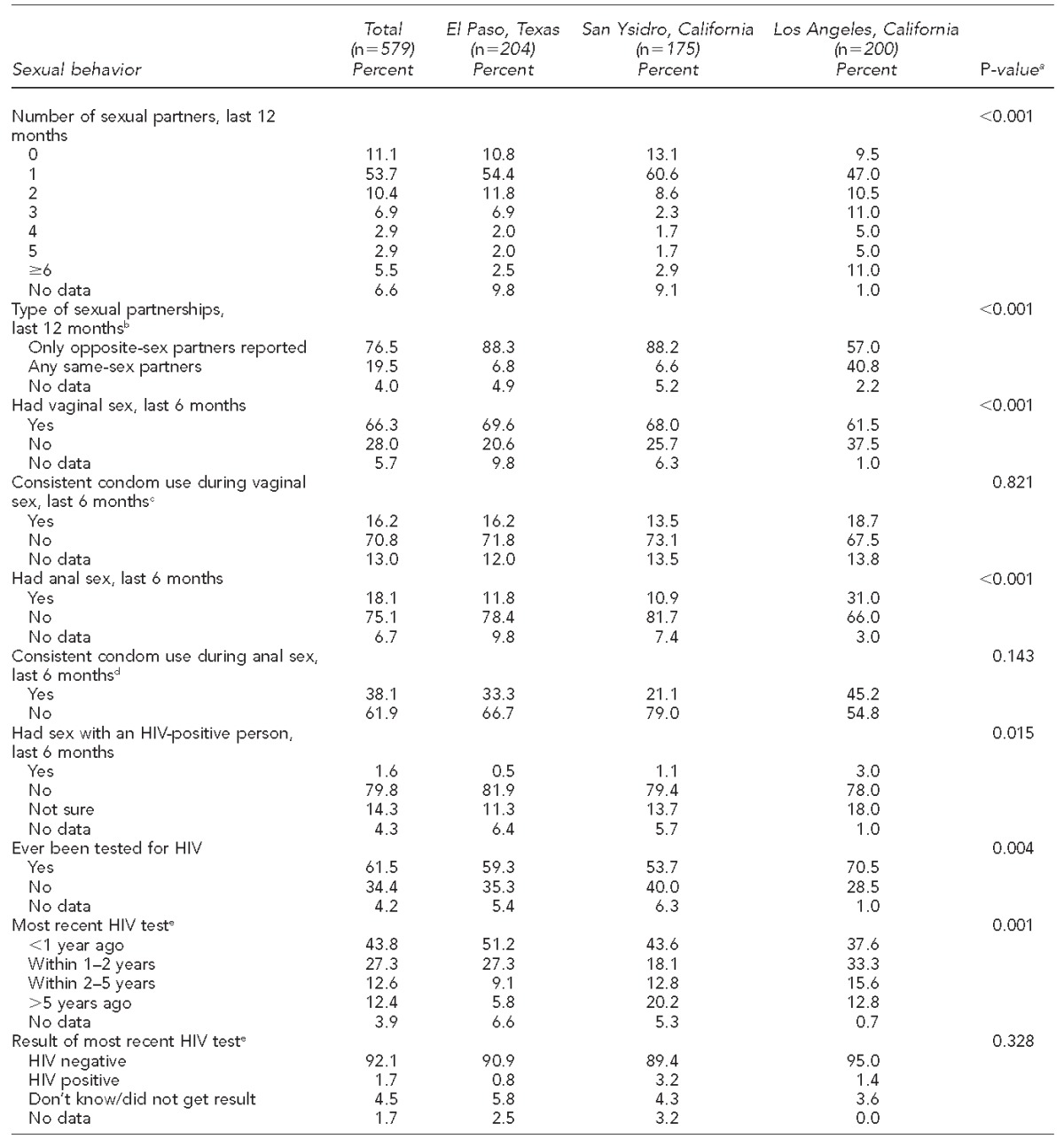
aP-values obtained from Pearson's chi-squared to test for statistically significant differences in proportions
bAmong participants who reported being sexually active in the last 12 months
cAmong participants who reported having vaginal sex in the last 6 months
dAmong participants who reported having anal sex in the last 6 months
eAmong participants who reported ever being tested for HIV
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
Change in outcomes from pretest to posttest
HIV/AIDS stigma scores decreased from pretest to posttest (2.5 vs. 2.2; t=11.2, p<0.001). HIV/AIDS knowledge scores increased significantly from pretest to posttest (6.0 vs. 7.1; t=–15.8, p<0.001), as did perceptions of HIV risk (3.7 vs. 3.9; t=–2.8, p=0.006) and willingness to communicate with one's sexual partner about HIV/AIDS (4.0 vs. 4.2; t=–3.8, p<0.001). No significant differences were found in willingness to seek HIV testing in the next three months for the sample overall (Table 4).
Table 4.
Changes from pretest to posttest scores in HIV/AIDS-related knowledge, attitudes, and intentions among participants in a community health worker HIV/AIDS intervention in three southwestern U.S. cities, April–June 2008
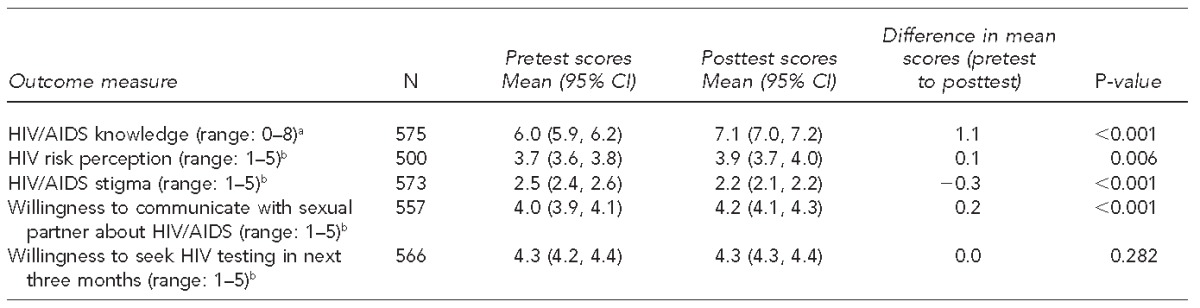
aOn a scale from 0 to 8, where 0 = low and 8 = high
bOn a scale from 1 to 5, where 1 = low and 5 = high
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
CI = confidence interval
Differences in gain scores across sites and participant characteristics
We found differences in gain scores by sex for two outcomes (Table 5). There was a greater decrease in mean HIV/AIDS stigma scores from pretest to posttest among women than among men (–0.4 vs. –0.2, t=–2.4, p=0.016). Additionally, the increase in mean HIV/AIDS knowledge score from pretest to posttest was greater among women than among men (1.3 vs. 0.9, t=2.7, p=0.007). There were no differences in gain scores by site or age group.
Table 5.
Differences between males and females in HIV/AIDS knowledge score changes and HIV/AIDS stigma score changes following participation in a community health worker HIV/AIDS intervention conducted in three southwestern U.S. cities, April–June 2008
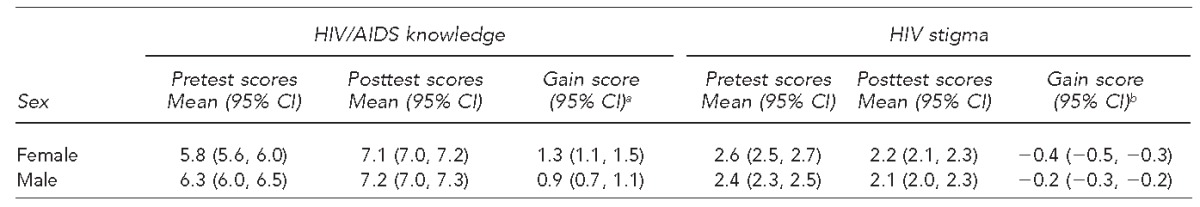
aDifference in gain score, t=2.7, p=0.007
bDifference in gain score, t=−2.4, p=0.016
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
CI = confidence interval
Participant evaluation of the intervention
On the posttest survey, 28% agreed and 64% completely agreed that they understood a lot more about HIV/AIDS after the intervention. Additionally, 26% agreed and 63% completely agreed that they felt more compassion toward those with HIV/AIDS, and 27% agreed and 62% completely agreed that they felt more comfortable talking about sex and sexuality after the intervention. When asked whether or not they thought that their health behavior would change as a result of their participation, 82% indicated that they would be more likely to practice safe sex and 79% indicated that they would be more likely to help or be associated with an HIV-positive person (data not shown).
LESSONS LEARNED
Results suggest that a promotores-led intervention is a promising strategy to reduce HIV/AIDS stigma and improve HIV/AIDS knowledge, increase comfort communicating about HIV/AIDS with sexual partners, and increase HIV risk perception, all of which are relevant for HIV prevention. However, we did not find changes in participants' willingness to test for HIV within the next three months.
The lack of measurable change in willingness to be tested for HIV may reflect participants' perceptions of low personal risk for HIV. High percentages of participants reported having had only one or no sexual partners in the previous 12 months, and half were married or cohabiting, perhaps contributing to a low perception (real or perceived) of HIV risk. Importantly, consistent condom use was low, so even participants with one sexual partner may have been at risk for HIV, depending on partners' sexual behavior. Another explanation for the lack of change in this measure may be that other structural or social factors play a role in participants' willingness to be tested for HIV, factors that were not addressed by the intervention.
A recent study that examined the correlates of past voluntary HIV testing and counseling among 135 middle-aged and older Latinas in South Florida found that the strongest predictors of receiving a previous HIV test were a health-care provider's endorsement and having a clinic as a regular source of health care.5 It may be that for Latinos in the general population who perceive themselves to be at low risk for HIV, health-care providers would be more compelling messengers than promotores to motivate HIV testing behavior. It may also be that Latinos lack access to a regular source of health care, which is a major barrier to HIV testing.
We found a greater reduction in HIV/AIDS stigma scores from pretest to posttest among women than among men, and a greater pretest to posttest increase in HIV/AIDS knowledge scores among women. This finding may reflect higher levels of HIV/AIDS stigma and lower HIV/AIDS knowledge among women at baseline, and, therefore, a greater impact on these outcomes as a result of the intervention. At posttest, the knowledge and stigma scores were comparable for men and women.
Limitations
This study was subject to several limitations. We were unable to include a control group in our study due to resource constraints. Furthermore, because the posttest survey was conducted immediately after the intervention, we do not know if the changes observed persisted over time, and we were unable to measure actual HIV testing behavior after the intervention. It is also possible that social desirability bias may have influenced participants' responses. Finally, the generalizability of our results was limited. Our sample included participants who were available to take part in a group session, so those who were too busy to participate or not willing to participate in a group session were not represented. Furthermore, the sample was predominantly of Mexican descent, reflecting the characteristics of the Latino populations in the southwestern United States. As such, the results may have been different if the study were conducted with other subgroups of Latinos in other geographic regions.
CONCLUSION
This study contributes to the growing literature doc-u-menting promotores as effective messengers of HIV prevention to Latinos. Future studies should evaluate this model using experimental or quasi-experimental study designs. It is important that future studies try to learn more about the components of this type of intervention that are critical to its success. One element that may have contributed to the changes observed in this intervention was the use of HIV-positive and -affected promotores to deliver the intervention. Contact with HIV-affected groups has been identified as an important strategy in efforts to reduce HIV/AIDS stigma.10 Further research should test whether HIV-unaffected promotores are as effective as HIV-affected promotores at delivering this type of intervention. Another factor of potential importance is an emphasis on positive cultural traits. While the majority of research regarding Latino culture has emphasized machismo and marianismo, two negatively perceived cultural traits, positive Latino values and culture may help to build feelings of self-worth and dignity and contribute to participant receptivity and motivation to take action. Other scholars have also commented on the importance of building on positive aspects of culture in HIV interventions.30
Given the high risks of HIV infection, low rates of testing, and continued HIV/AIDS-related stigma, new approaches for reaching Latinos, particularly recent immigrants and others with lower access to health care, are critically needed.
Footnotes
All study procedures were approved by the California State University Long Beach Institutional Review Board.
The authors thank Rosana Escolari and Brenda Huerta of the San Ysidro Health Center, Ana Danciger of Centro de Salud Familiar La Fe, Richard Zaldivar of The Wall/Las Memorias, and the dedicated teams of promotores de salud that made this work possible. The authors also thank Frank Beadle de Palomo for his visionary work on HIV/AIDS-related stigma. His recognition of stigma as a multifaceted issue that manifests distinctly among diverse populations living with, or at risk for, HIV, facilitated the development of this work.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) HIV among Hispanics/Latinos in the United States and dependent areas. 2013 [cited 2014 Apr 11] Available from: URL: http://www.cdc.gov/hiv/pdf/risk_latino.pdf.
- 2.Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 3.Kaiser Family Foundation. HIV testing in the United States. 2015 [cited 2015 Jul 16] Available from: URL: http://kff.org/hivaids/fact-sheet/hiv-testing-in-the-united-states.
- 4.Chen N, Erbelding E, Yeh HC, Page K. Predictors of HIV testing among Latinos in Baltimore City. J Immigr Minor Health. 2010;12:867–74. doi: 10.1007/s10903-009-9297-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Craig SL, Beaulaurier RL, Newman FL, De La Rosa M, Brennan DJ. Health and cultural determinants of voluntary HIV testing and counseling among middle-aged and older Latina women. J Women Aging. 2012;24:97–112. doi: 10.1080/08952841.2012.639650. [DOI] [PubMed] [Google Scholar]
- 6.Santos G, Puga AM, Medina C. HAART, adherence, and cultural issues in the US Latino community. AIDS Read. 2004;14(10 Suppl):S26–9. [PubMed] [Google Scholar]
- 7.Brooks RA, Etzel MA, Hinojos E, Henry CL, Perez M. Preventing HIV among Latino and African American gay and bisexual men in a context of HIV-related stigma, discrimination, and homophobia: perspectives of providers. AIDS Patient Care STDS. 2005;19:737–44. doi: 10.1089/apc.2005.19.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gilbert PA, Rhodes SD. HIV testing among immigrant sexual and gender minority Latinos in a US region with little historical Latino presence. AIDS Patient Care STDS. 2013;27:628–36. doi: 10.1089/apc.2013.0232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.UNAIDS. Fact sheet: stigma and discrimination. 2003 [cited 2014 Apr 11] Available from: URL: http://data.unaids.org/publications/fact-sheets03/fs_stigma_discrimination_en.pdf?preview_true.
- 10.Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS Educ Prev. 2003;15:49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- 11.Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dang BN, Giordano TP, Kim JH. Sociocultural and structural barriers to care among undocumented Latino immigrants with HIV infection. J Immigr Minor Health. 2012;14:124–31. doi: 10.1007/s10903-011-9542-x. [DOI] [PubMed] [Google Scholar]
- 13.Carr RL, Gramling LF. Stigma: a health barrier for women with HIV/AIDS. J Assoc Nurses AIDS Care. 2004;15:30–9. doi: 10.1177/1055329003261981. [DOI] [PubMed] [Google Scholar]
- 14.Courtenay-Quirk C, Wolitski RJ, Parsons JT, Gomez CA Seropositive Urban Men's Study Team. Is HIV/AIDS stigma dividing the gay community? Perceptions of HIV-positive men who have sex with men. AIDS Educ Prev. 2006;18:56–67. doi: 10.1521/aeap.2006.18.1.56. [DOI] [PubMed] [Google Scholar]
- 15.Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav. 2011;15:1075–87. doi: 10.1007/s10461-010-9847-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rios-Ellis B, Espinoza L, Bird M, Garcia M, D'Anna LH, Bellamy L, et al. Increasing HIV-related knowledge, communication, and testing intentions among Latinos: Protege tu Familia: Hazte la Prueba. J Health Care Poor Underserved. 2010;21(3 Suppl):148–68. doi: 10.1353/hpu.0.0360. [DOI] [PubMed] [Google Scholar]
- 17.Diaz NV, Rivera SM, Bou FC. AIDS stigma combinations in a sample of Puerto Rican health professionals: qualitative and quantitative evidence. P R Health Sci J. 2008;27:147–57. [PubMed] [Google Scholar]
- 18.Sanchez EL. US Latinos struggle with HIV stigma. Al Jazeera 2013 Dec 9 [cited 2015 May 3] Available from: URL: http://www.aljazeera.com/indepth/features/2013/12/us-latinos-struggle-with-hiv-stigma-201312817215705199.html.
- 19.Varas-Diaz N, Serrano-Garcia I, Toro-Alfonso J. AIDS-related stigma and social interaction: Puerto Ricans living with HIV/AIDS. Qual Health Res. 2005;15:169–87. doi: 10.1177/1049732304272059. [DOI] [PubMed] [Google Scholar]
- 20.Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. Am J Prev Med. 2007;33:418–27. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 21.Elder JP, Ayala GX, Parra-Medina D, Talavera GA. Health communication in the Latino community: issues and approaches. Annu Rev Public Health. 2009;30:227–51. doi: 10.1146/annurev.publhealth.031308.100300. [DOI] [PubMed] [Google Scholar]
- 22.WestRasmus EK, Pineda-Reyes F, Tamez M, Westfall JM. Promotores de salud and community health workers: an annotated bibliography. Fam Community Health. 2012;35:172–82. doi: 10.1097/FCH.0b013e31824991d2. [DOI] [PubMed] [Google Scholar]
- 23.Rhodes SD, Kelley C, Siman F, Cashman R, Alonzo J, McGuire J, et al. Using community-based participatory research (CBPR) to develop a community-level HIV prevention intervention for Latinas: a local response to a global challenge. Womens Health Issues. 2012;22:e293–301. doi: 10.1016/j.whi.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rhodes SD, Hergenrather KC, Bloom FR, Leichliter JS, Montano J. Outcomes from a community-based, participatory lay health adviser HIV/STD prevention intervention for recently arrived immigrant Latino men in rural North Carolina. AIDS Educ Prev. 2009;21(5 Suppl):103–8. doi: 10.1521/aeap.2009.21.5_supp.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramos RL, Hernandez A, Ferreira-Pinto JB, Ortiz M, Somerville GG. Promovision: designing a capacity-building program to strengthen and expand the role of promotores in HIV prevention. Health Promot Pract. 2006;7:444–9. doi: 10.1177/1524839905278868. [DOI] [PubMed] [Google Scholar]
- 26.Ramos RL, Green NL, Shulman LC. Pasa la voz: using peer driven interventions to increase Latinas' access to and utilization of HIV prevention and testing services. J Health Care Poor Underserved. 2009;20:29–35. doi: 10.1353/hpu.0.0124. [DOI] [PubMed] [Google Scholar]
- 27.Ramos RL, Ferreira-Pinto JB, Rusch ML, Ramos ME. Pasa la voz (spread the word): using women's social networks for HIV education and testing. Public Health Rep. 2010;125:528–33. doi: 10.1177/003335491012500407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McQuiston C, Flaskerud JH. “If they don't ask about condoms, I just tell them”: a descriptive case study of Latino lay health advisers' helping activities. Health Educ Behav. 2003;30:79–96. doi: 10.1177/1090198102239260. [DOI] [PubMed] [Google Scholar]
- 29.Martin M, Camargo M, Ramos L, Lauderdale D, Krueger K, Lantos J. The evaluation of a Latino community health worker HIV prevention program. Hispanic J Behav Sci. 2005;27:371–84. [Google Scholar]
- 30.Airhihenbuwa CO, Webster JD. Culture and African contexts of HIV/AIDS prevention, care and support. SAHARA J. 2004;1:4–13. doi: 10.1080/17290376.2004.9724822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dimitrov DM, Rumrill P., Jr Pretest-posttest designs and measurement of change. Work. 2003;20:159–65. [PubMed] [Google Scholar]
- 32.StataCorp. College Station (TX): StataCorp; 2009. Stata®: Version 11.2. [Google Scholar]


