Abstract
Objective
We evaluated the extent to which children and adolescents were not vaccinated against measles (“unvaccinated”), clustering within U.S. counties, and factors associated with unvaccination, including parents' vaccine-related beliefs and missed opportunities.
Methods
We analyzed data from the 2010–2013 National Immunization Survey (NIS) and NIS-Teen Survey of households with 19- to 35-month-old children and 13- to 17-year-old adolescents, respectively. We used provider-reported vaccination histories to assess measles vaccination status.
Results
In 2013, 7.5% of children and 4.5% of adolescents were unvaccinated against measles. Four-fifths (80.0%) of unvaccinated children lived in counties containing 41.9% of the nation's children, and 80.0% of unvaccinated adolescents lived in counties containing 30.4% of the nation's adolescents. Multivariable statistical analyses found that 74.6% of children who were unvaccinated against measles missed being vaccinated for reasons other than parents' negative vaccine-related beliefs, and 89.6% could be deemed as having at least one missed opportunity for being vaccinated against measles because they were administered at least one dose of other recommended vaccines after 12 months of age. Among adolescents, multivariable analyses found that only demographic factors, not vaccine-related parental beliefs, were independently associated with being unvaccinated.
Conclusions
Reasons other than negative vaccine-related beliefs, including missed opportunities, accounted for the vast majority of unvaccinated children and adolescents.
In 2000, the Centers for Disease Control and Prevention (CDC) declared measles to be eliminated in the United States,1 an accomplishment achieved because of the high levels of population immunity resulting from high measles vaccination coverage levels across the United States.2 Despite the elimination of endemic measles in the United States, sporadic outbreaks have continued as a consequence of importations from countries where measles is endemic.3–17
High national and state measles vaccination coverage rates may mask considerable variability in vaccination rates at the county or community level.18 Geographic clustering of susceptible children and adolescents increases the risk of outbreaks and could lead to reestablishment of endemic measles transmission.19
In this article, we evaluate the extent to which children and adolescents who are unvaccinated against measles cluster within U.S. counties. Also, although the popular media20,21 and scientific literature22–27 have reported an association between lower vaccination coverage and negative vaccine-related parental beliefs, some literature suggests that under-immunization may result primarily from missed opportunities to vaccinate rather than from negative vaccine-related beliefs.28 We assessed the associations among not being vaccinated against measles, parents' vaccine-related beliefs, and missed opportunities, and evaluated the extent to which not being vaccinated against measles is attributable to factors other than negative vaccine-related beliefs.
METHODS
Our analyses used the most recent data from the National Immunization Survey (NIS)29 and NIS-Teen30 to address our scientific objectives that provide statistically reliable estimates. The target populations of the two surveys were 19- to 35-month-old children (hereinafter referred to as children) (NIS) and 13- to 17-year-old adolescents (hereinafter referred to as adolescents) (NIS-Teen). Both surveys included a random-digit-dial survey of households with landline telephone numbers; in 2011–2013, both surveys included a random-digit-dial survey of cell phone numbers. We analyzed data from sampled children and adolescents who had adequate provider-reported vaccination histories to assess their vaccination status. We defined children and adolescents as being unvaccinated if their providers reported that no doses of measles-containing vaccine were administered. For this article, children not vaccinated against measles were deemed and defined as having a missed opportunity to be vaccinated against measles if, after 12 months of age (when eligibility for the recommendation for routine administration of the measles vaccine begins), vaccination provider records confirmed that they were administered doses of other recommended childhood vaccines but remained unvaccinated against measles. Detailed descriptions of the NIS and NIS-Teen have been published elsewhere.31–38
The national number and percentage of unvaccinated children and adolescents were estimated using data from 13,611 children sampled by the 2013 NIS and 18,264 adolescents sampled by the 2013 NIS-Teen. To obtain statistically reliable county-level estimates of the percentage and number of children and adolescents not vaccinated against measles, we used three consecutive years of NIS and NIS-Teen data, required the sample sizes for counties to be ≥35 for the three years combined, and used James-Stein statistical estimation methodology.39 Because of reduced national sample sizes for both the 2013 NIS and NIS-Teen, county-level sample sizes for that survey year were smaller than for previous years, resulting in fewer counties achieving the sample size requirement. Among counties that achieved the sample size requirement, many county-level estimates had low precision. Because of that imprecision, we used data from 31,176 children and 38,749 adolescents sampled from the 2010–2012 NIS and NIS-Teen, respectively, to obtain county-level estimates.
Vaccine-related parental beliefs were collected in the 2011 NIS and the 2010 NIS-Teen and organized using the Health Belief Model.22,40 Multivariable recursive partitioning (i.e., a multivariable statistical method that creates a decision tree that attempts to classify members of the population based on several independent variables) analyses41,42 were used (1) to identify independent predictors of being unvaccinated against measles, (2) to segment the populations of children and adolescents into groups characterized by increasing risk of not being vaccinated against measles, and (3) to derive the percentages of children and adolescents who were unvaccinated against measles that could be attributed43 to reasons other than parents' negative vaccine-related beliefs. All analyses accounted for the surveys' sampling weights and sampling design.44 Estimated percentages and numbers are reported along with their 95% confidence intervals (CIs). Differences between estimates were statistically significant at p<0.05.
RESULTS
Children unvaccinated against measles (unvaccinated children)
In 2013, the estimated number and percentage of unvaccinated 19- to 35-month-old children in the United States were 429,915 (95% CI 376,857, 482,973) and 7.5% (95% CI 6.6, 8.4), respectively. Among all counties in the United States in 2013, approximately 80.0% of the unvaccinated children lived in counties containing 41.9% of the national population of 19- to 35-month-old children (data not shown in tables or figures).
A total of 210 counties had combined sample sizes ≥35 across 2010–2012 for both the NIS and NIS-Teen. In 2013, children living in the 210 counties comprised 50.7% of all children nationally. Among the 210 counties, the highest decile of estimated number of unvaccinated children ranged from 18,610 in Los Angeles County, California, to 2,135 in Wake County, North Carolina, and the highest decile of the estimated percentage of unvaccinated children ranged from 18.0% in Boulder County, Colorado, to 10.3% in Allen County, Indiana, and Clackamas County, Oregon (Table 1).
Table 1.
Estimated number and percentage of unvaccinateda children and adolescents in selected counties in the United States,b 2010–2012 NIS and 2010–2012 NIS-Teen
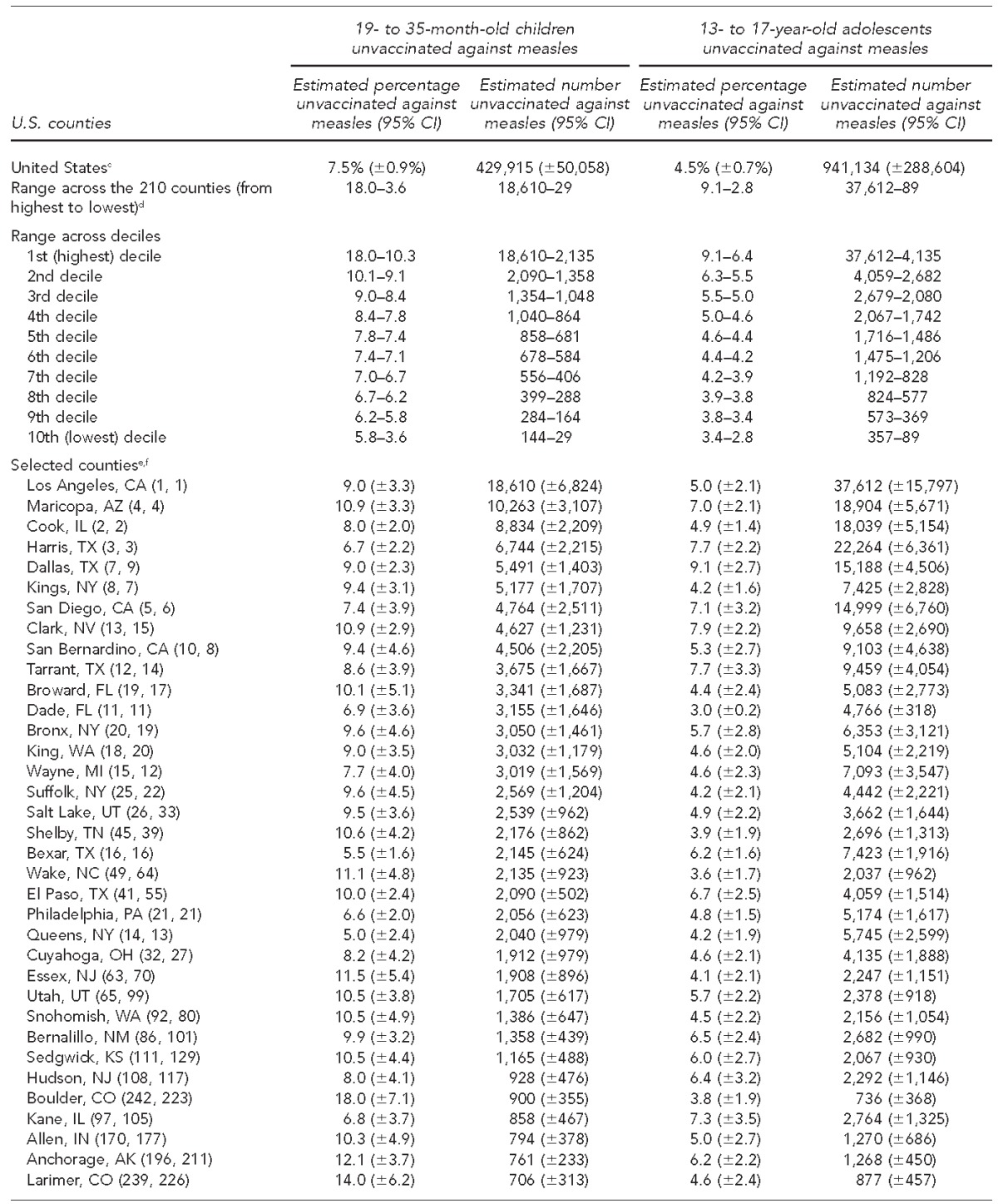
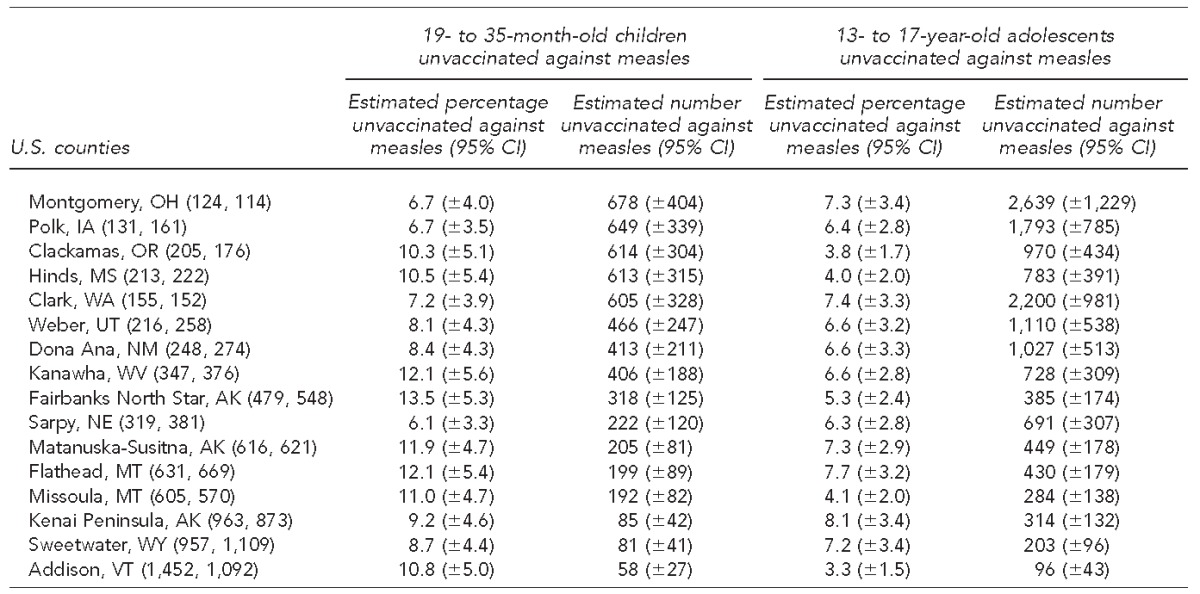
Unvaccinated against measles refers to those administered no doses of measles-containing vaccine.
Among the 210 counties for which county-level estimates were obtained, selected counties included those that were at least one of the following: (1) in the highest decile of the estimated percentage of children unvaccinated against measles, (2) in the highest decile of the estimated number of children unvaccinated against measles, (3) in the highest decile of the estimated percentage of adolescents who were unvaccinated against measles, or (4) in the highest decile of the estimated number of adolescents who were unvaccinated against measles.
cNational estimates are based on 2013 data from the NIS and NIS-Teen.
dTwo hundred ten counties had combined sample sizes of ≥35 across 2010–2012 for both the NIS and NIS-Teen.
eCounty population rank of 19- to 35-month-old children among 3,141 counties comprising the United States
fCounty population rank of 13- to 17-year-old adolescents among 3,141 counties comprising the United States
NIS = National Immunization Survey
CI = confidence interval
Bivariable analyses found that compared with vaccinated children, unvaccinated children were significantly more likely to lack health insurance coverage and to have other statistically significant differences with respect to maternal and household characteristics that are generally associated with lower socioeconomic status (Table 2). Also, unvaccinated children were found to have parents with significantly lower assessments of (1) their child's risk of getting a vaccine-preventable disease (VPD), (2) VPDs as a concern that makes vaccinations relevant, and (3) vaccines' efficacy to reduce the threat of a VPD. Compared with parents of vaccinated children, parents of unvaccinated children were also significantly less likely to report that their decision to vaccinate their child was favorably influenced by a health-care provider (HCP) and significantly more likely to report concerns about vaccine safety (Table 3).
Table 2.
Bivariable analyses of the percentage of children unvaccinated against measles, by demographic characteristic and age group, in the United States: 2011 NIS (quarters 1–4) and 2010 NIS-Teen (quarters 3–4)
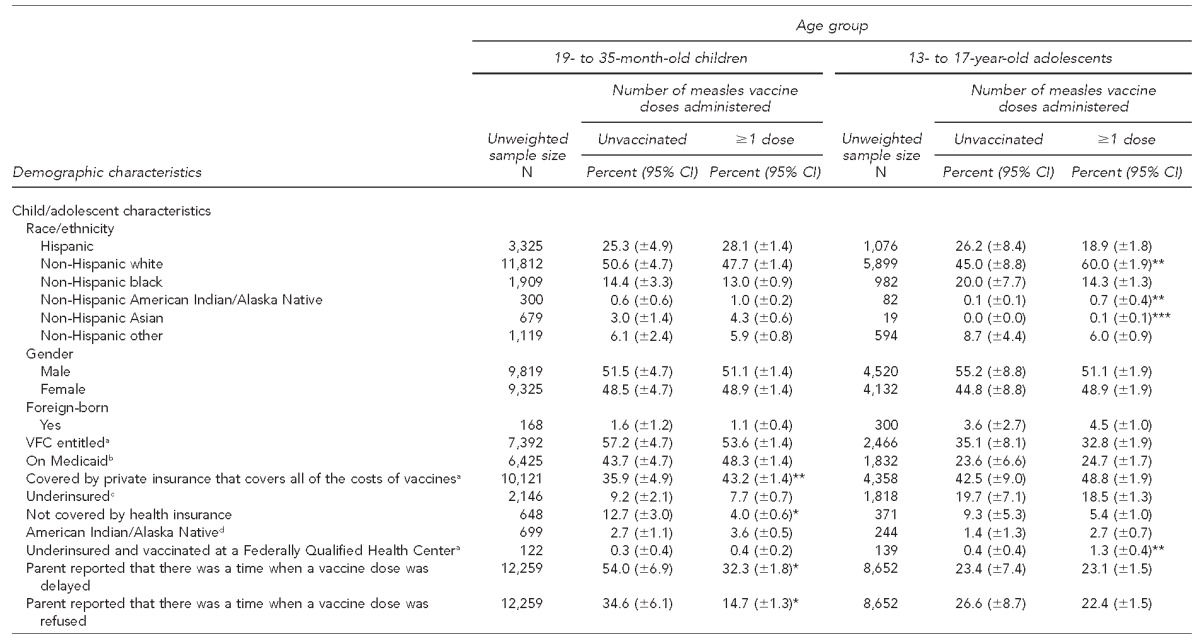
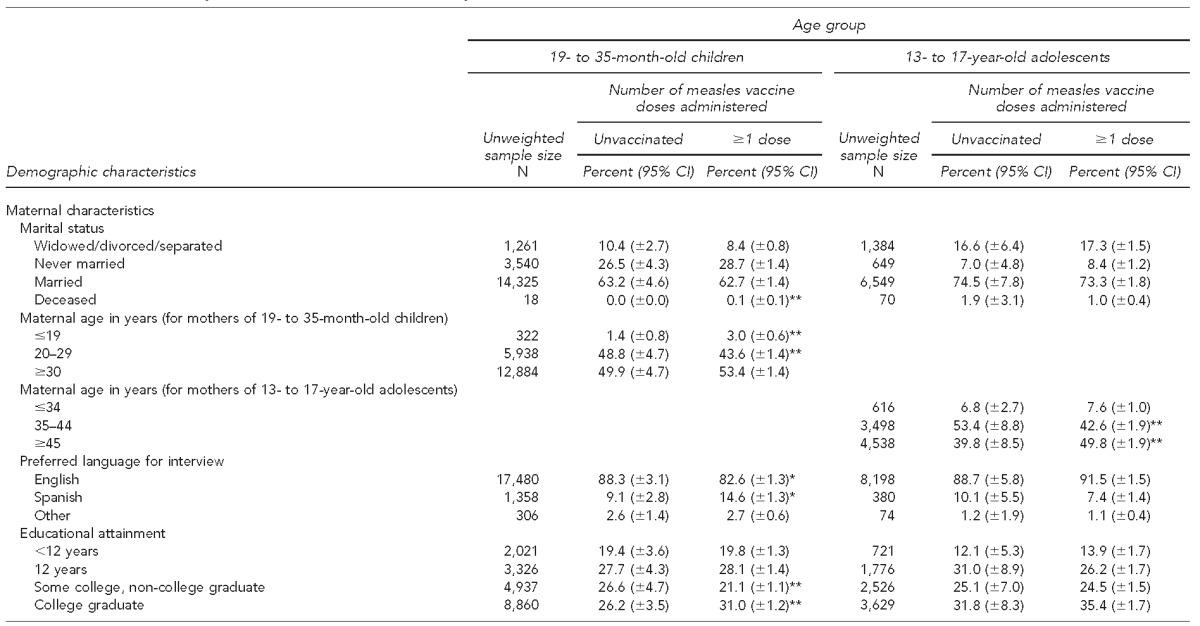
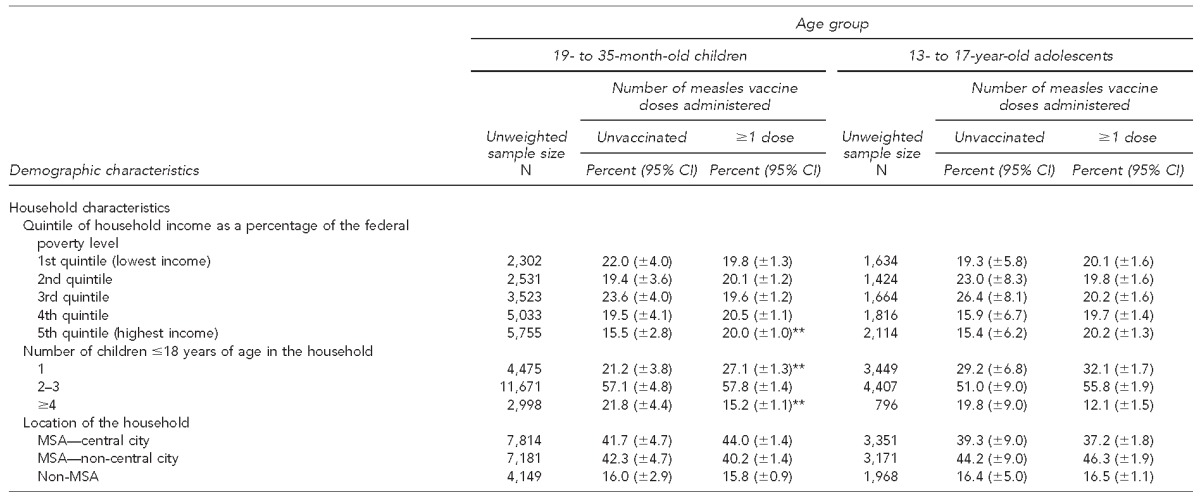
*Estimated percentage is significantly different from the estimated percentage in the same row among unvaccinated respondents in the selected age group, p<0.001.
**Estimated percentage is significantly different from the estimated percentage in the same row among unvaccinated respondents in the selected age group, 0.001≤p<0.01.
***Estimated percentage is significantly different from the estimated percentage in the same row among unvaccinated respondents in the selected age group, 0.01≤p<0.05.
aVFC entitlement status is based on parental report that their child/adolescent is either eligible for Medicaid, not covered by health insurance, American Indian/Alaska Native, or covered by private health insurance that does not cover all of the cost of vaccines and administered doses at a Federally Qualified Health Center or Rural Health Center.
bParental report of health insurance status and health insurance type is among the childhood/adolescent characteristics collected in the telephone interview of the NIS and NIS-Teen.
cUnderinsured children are reported by their parents to be covered by private health insurance that does not cover all of the cost of all recommended vaccines.
dIncludes both Hispanic and non-Hispanic American Indian/Alaska Natives
NIS = National Immunization Survey
CI = confidence interval
VFC = Vaccines for Children program
MSA = metropolitan statistical area
Table 3.
Percentage of parents agreeing with statements read to them, by Health Belief Model domain,a age group, and number of measles vaccine doses administered to their children: United States, 2011 NIS (quarters 1–4) and 2010 NIS-Teen (quarters 3–4)
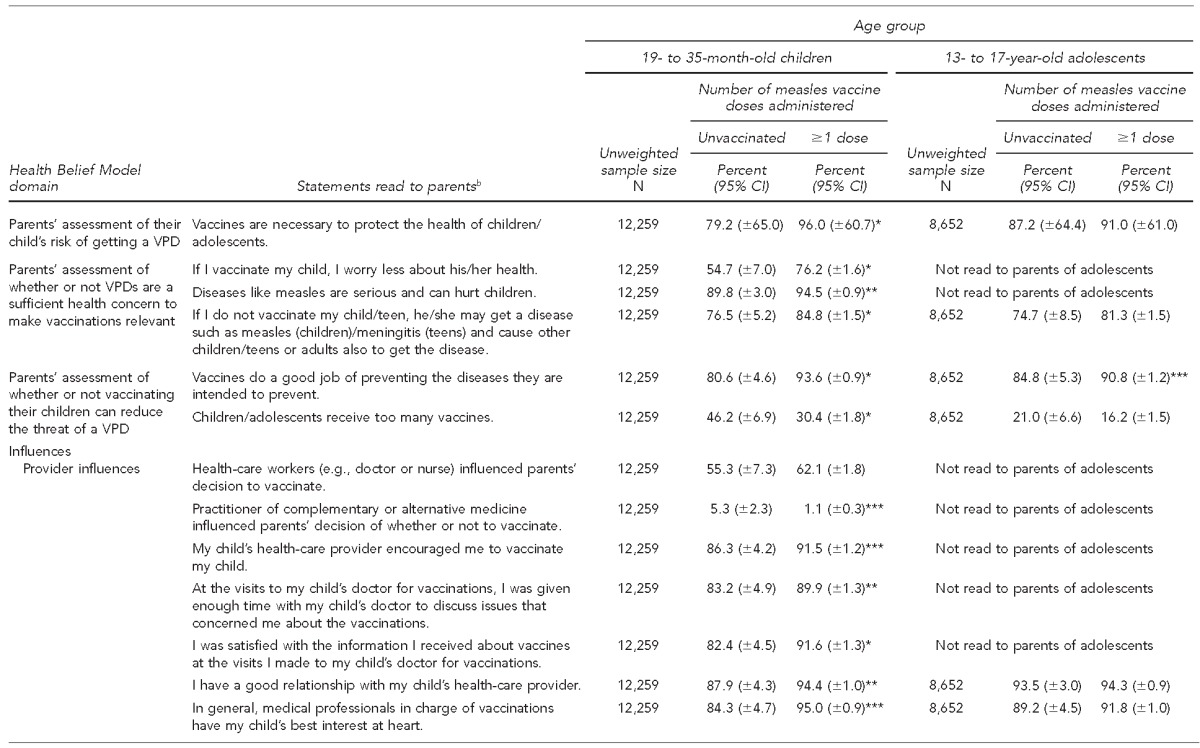
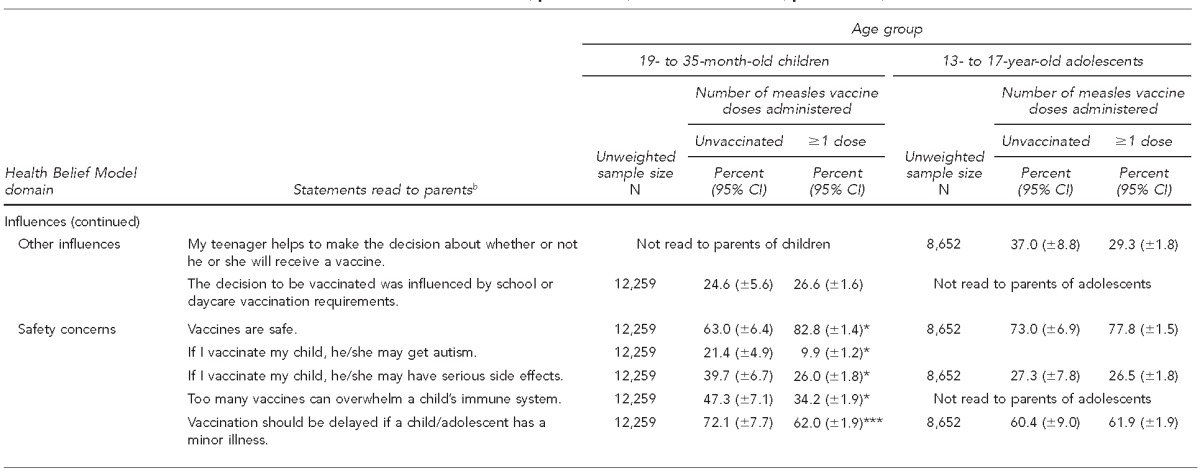
*Estimated percentage is significantly different from the estimated percentage in the same row among unvaccinated respondents in the selected age group, p<0.001.
**Estimated percentage is significantly different from the estimated percentage in the same row among unvaccinated respondents in the selected age group, 0.001≤p<0.01.
***Estimated percentage is significantly different from the estimated percentage in the same row among unvaccinated respondents in the selected age group, 0.01≤p<0.05.
NIS = National Immunization Survey
Rosenstock IM, Derryberry M, Carriger BK. Why people fail to seek poliomyelitis vaccination. Public Health Rep 1959;74:98-104.
bParents were read the listed statements and asked about their level of agreement on a scale from 0 to 10. Responses of ≥7 were interpreted as agreement.
CI = confidence interval
VPD = vaccine-preventable disease
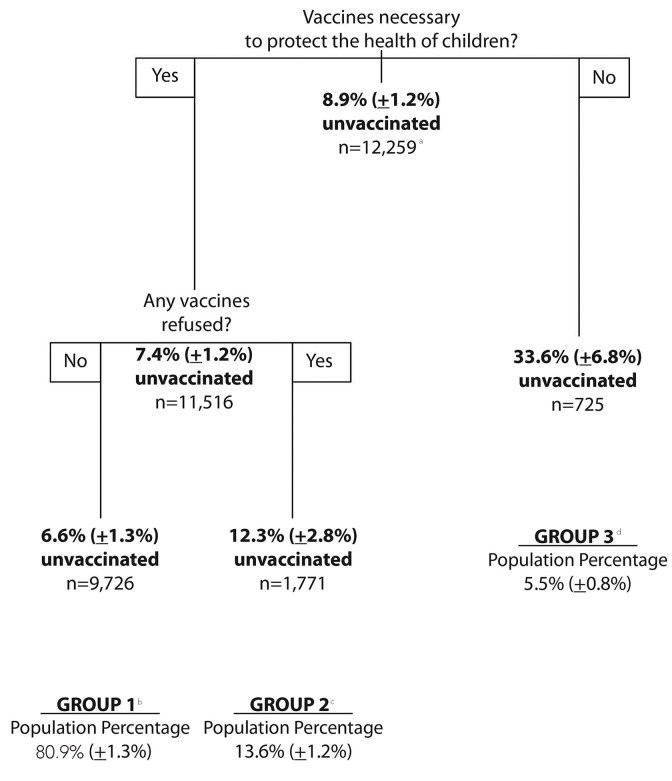
Multivariable recursive partitioning analyses (Figure 1) found that none of the 19 demographic factors and only two of the 20 vaccine-related parental belief factors (Table 3) were independently associated with a child being unvaccinated against measles. Specifically, the multivariable analysis found that the independent predictors of an unvaccinated child were (1) parents' belief about the necessity of vaccines to protect the health of children and (2) among parents who believed in the necessity of vaccines, whether or not parents reported refusing vaccine dose administration for their child (Figure 1).
Figure 1.
Percentage of 19- to 35-month-old children unvaccinated against measles, by vaccine-related parental beliefs found to be the independent factors associated with being unvaccinated, 2011 National Immunization Survey
an = unweighted sample size associated with the listed percentage. Sample sizes at daughter nodes may not add to the sample size at the parent node because of missing values in the variable defining splits at the daughter node.
bGroup 1 consists of children whose parents believed that vaccines are necessary to protect the health of children and did not report refusing the administration of any vaccines.
cGroup 2 consists of children whose parents believed that vaccines are necessary to protect the health of children and reported refusing the administration of ≥1 vaccine dose of any vaccine type.
dGroup 3 consists of children whose parents did not believe that vaccines are necessary to protect the health of children.
The multivariable analysis segmented the U.S. population of children into three groups (Figure 1). Group 1 included children whose parents believe that vaccines are necessary to protect their children's health and did not report vaccine refusal. Group 2 included children whose parents believe that vaccines are necessary to protect their children's health and reported refusing ≥1 vaccine dose of any type. Group 3 included children whose parents do not believe that vaccines are necessary to protect their children's health. In the continuum from group 1 to group 3, there was (1) a statistically significant decrease in the percentages of children belonging to the groups as a percentage of the population of 19- to 35-month-old children (80.9% in group 1, to 13.6% in group 2, and to 5.5% in group 3, p<0.05) and (2) a statistically significant increase in the percentage of children unvaccinated against measles (from 6.6% in group 1, to 12.3% in group 2, and to 33.6% in group 3, p<0.05).
The percentage of children with parents who had negative vaccine-related beliefs also increased across the three groups. Compared with parents of children in group 1, parents of children in group 2 differed significantly on 10 of 20 vaccine-related belief factors. Parents of children in group 2 were significantly less likely than parents of children in group 1 to report that their child's HCP encouraged them to vaccinate their child, to have been satisfied with information received from their child's HCP about vaccines, and to think that vaccines are safe. Also, parents of children in group 2 were significantly more likely than parents of children in group 1 to believe that children receive too many vaccines, that their children may get autism if they vaccinate, that their children may have serious side effects if they vaccinate, that too many vaccines can overwhelm a child's immune system, and that vaccinations should be delayed if a child has a minor illness (Table 4).
Table 4.
Percentage of parents agreeing with statements read to them, by Health Belief Modela domain, age group, and group defined by recursive partioning:b 2011 NIS (quarters 1–4) and 2010 NIS-Teen (quarters 3–4)
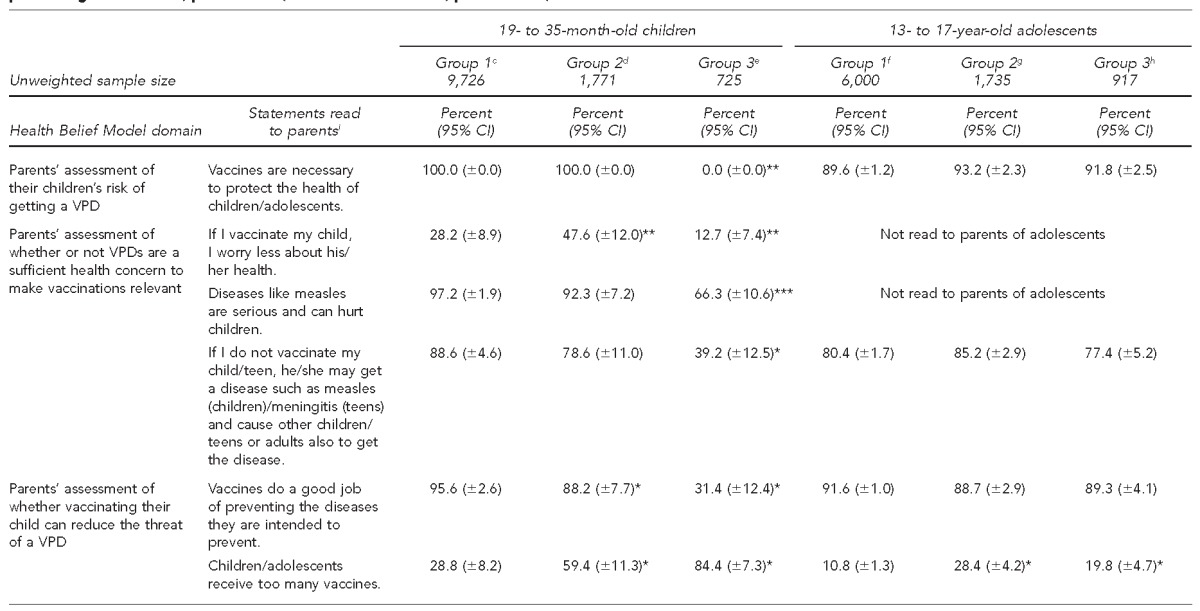
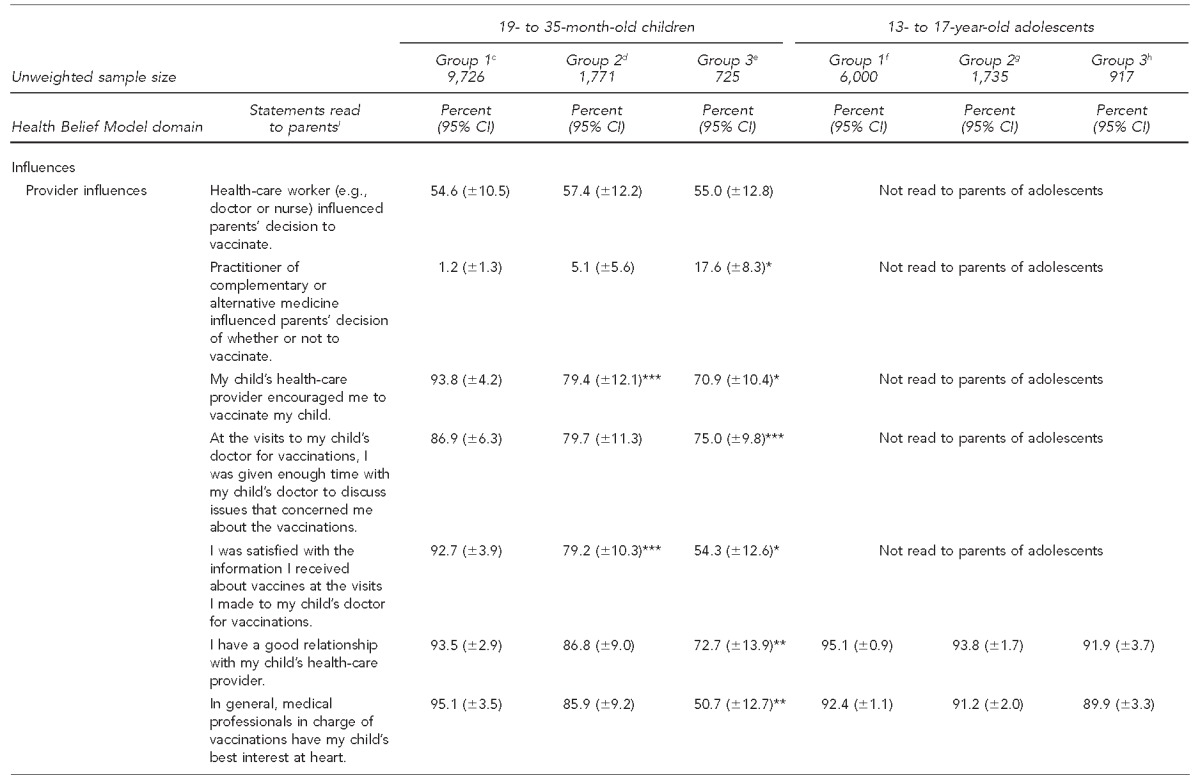
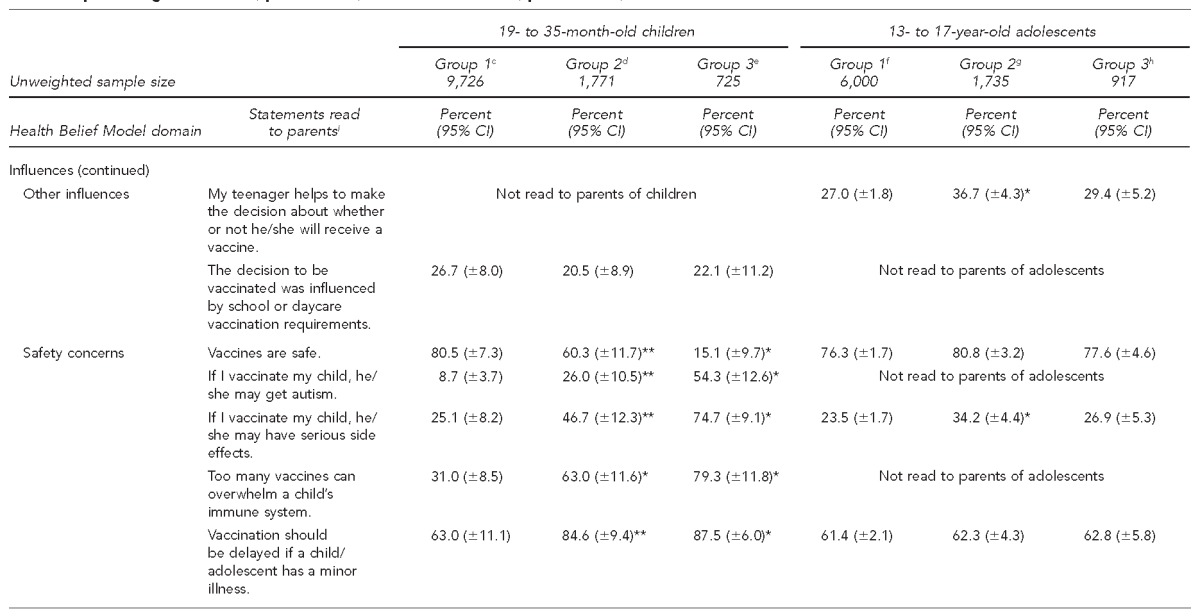
*Estimated percentage is significantly different from the estimated percentage in the same row among respondents in Group 1 and in the selected age group, p<0.001.
**Estimated percentage is significantly different from the estimated percentage in the same row among respondents in Group 1 and in the selected age group, 0.001≤p<0.01.
***Estimated percentage is significantly different from the estimated percentage in the same row among respondents in Group 1 and in the selected age group, 0.01≤p<0.05.
Rosenstock IM, Derryberry M, Carriger BK. Why people fail to seek poliomyelitis vaccination. Public Health Rep 1959;74:98-104.
Recursive partitioning is a multivariable statistical method that creates a decision tree that attempts to classify members of the population based on several independent variables.
cFor 19- to 35-month-old children, Group 1 consists of children whose parents believe that vaccines are necessary to protect the health of children and did not report refusing the administration of any vaccines.
dFor 19- to 35-month-old children, Group 2 consists of children whose parents believe that vaccines are necessary to protect the health of children and reported refusing the administration of ≥1 vaccine dose of any vaccine type.
eFor 19- to 35-month-old children, Group 3 consists of children whose parents did not believe that vaccines are necessary to protect the health of children.
fFor 13- to 17-year-old adolescents, Group 1 consists of non-Hispanic white, American Indian/Alaska Native, and non-Hispanic Asian adolescents.
gFor 13- to 17-year-old adolescents, Group 2 consists of Hispanic, non-Hispanic black, and people of other races/ethnicities who live in a household with an annual income in either the lower quintile or upper two quintiles of the distribution of household income, adjusted for household composition.
hFor 13- to 17-year-old adolescents, Group 3 consists of Hispanic, non-Hispanic black, and people of other races/ethnicities who live in a household with an annual income in either the second or third quintiles of the distribution of household income, adjusted for household composition.
iParents were read the listed statements and asked about their level of agreement on a scale from 0 to 10. Responses of ≥7 were interpreted as agreement.
NIS = National Immunization Survey
CI = confidence interval
VPD = vaccine-preventable disease
Compared with parents of children in group 1, parents of children in group 3 differed on 17 of 20 vaccine-related belief factors (Table 4). In addition to differing from group 1 concerning the same vaccine-related belief factors about which group 2 differed, parents of children in group 3 were significantly less likely to believe that diseases such as measles are serious and can hurt children; that if they do not vaccinate their child, the child may get a disease such as measles; that vaccines do a good job of preventing diseases; and that medical professionals in charge of vaccinations have their child's best interest at heart. They were also less likely to report that they were given enough time with their child's doctor to discuss issues that concerned them about vaccinations and to report that they have a good relationship with their child's HCP. Also, parents of children in group 3 were significantly more likely than parents of children in group 1 to report that their decision of whether or not to vaccinate their child was influenced by a practitioner of complementary or alternative medicine (Table 4). Among unvaccinated children in group 3, 77.6% (95% CI 65.6, 89.6) had parents who reported refusing the administration of vaccine doses for their child (data not shown).
For children in group 1, the multivariable analysis found that the independent factors associated with not being vaccinated against measles did not include negative parental beliefs measured by the NIS (Figure 1).
Children in group 2 were 1.9 times more likely (95% CI 1.4, 2.5) to be unvaccinated against measles than children in group 1. Additionally, children in group 2 were 5.7 percentage points (12.3% minus 6.6%) more likely to not be vaccinated against measles than children in group 1. Among children unvaccinated against measles in group 2, the percentage unvaccinated that was attributable to factors other than the negative parental belief factors associated with group 2 was 53.8% (95% CI 40.6, 71.4) (data not shown).
Children in group 3 were 5.1 times more likely (95% CI 3.8, 6.7) to be unvaccinated against measles than children in group 1 (data not shown). Also, children in group 3 were 27.0 percentage points (33.6% minus 6.6%) more likely to not be vaccinated against measles than children in group 1 (Figure 1). Among children unvaccinated against measles in group 3, the percentage unvaccinated that was attributable to factors other than the negative parental belief factors that were associated with group 3 was 19.7% (95% CI 14.9, 26.1) (data not shown).
Among all children unvaccinated against measles in the U.S. population, the percentage unvaccinated that was attributable to factors other than parents' negative beliefs about the necessity of vaccines or vaccine refusal was 74.6% (95% CI 71.3, 77.9). Among children who were unvaccinated against measles, the percentages across the three groups of children who had missed opportunities were 97.3% (95% CI 93.5, 100.0) in group 1, 98.2% (95% CI 96.5, 100.0) in group 2, and 59.6% (95% CI 48.0, 71.2) in group 3. The overall percentage was 89.6% (95% CI 86.1, 93.1). Also, among all 19- to 35-month-old children unvaccinated against measles, only 34.6% (95% CI 28.5, 40.7) had a parent who reported refusing the administration of any vaccine doses (data not shown).
Adolescents unvaccinated against measles (unvaccinated adolescents)
In 2013, the estimated number and percentage of unvaccinated 13- to 17-year-old adolescents was 941,134 (95% CI 796,832, 1,085,436) and 4.5% (95% CI 3.8, 5.2) (Table 1). The number and percentage of adolescents not administered two doses of measles-containing vaccine were 1,642,293 (95% CI 1,472,783, 1,811,803) and 7.9% (95% CI 7.1, 8.7). Among the 3,141 counties that the United States comprised in 2013, approximately 80.0% of unvaccinated adolescents lived in counties containing 30.4% of the national population of adolescents (data not shown).
In 2013, children living in the 210 counties comprised 53.5% of all adolescents nationally. The upper decile of the number of adolescents unvaccinated against measles ranged from 37,612 in Los Angeles County, California, to 4,135 in Cuyahoga County, Ohio. The upper decile of the percentage of unvaccinated adolescents ranged from 9.1% in Dallas County, Texas, to 6.4% in Hudson County, New Jersey, and Polk County, Iowa (Table 1).
Bivariable analyses found that compared with adolescents vaccinated against measles, unvaccinated adolescents (1) were significantly more likely to be Hispanic, non-Hispanic American Indian/Alaska Native, or non-Hispanic Asian; (2) were more likely to have other statistically significant differences with respect to maternal characteristics, insurance status, and the likelihood of having a parent who reported ever refusing vaccines (Table 2); but (3) were not statistically significantly different with respect to any of the 10 vaccine-related factors measured (Table 3).
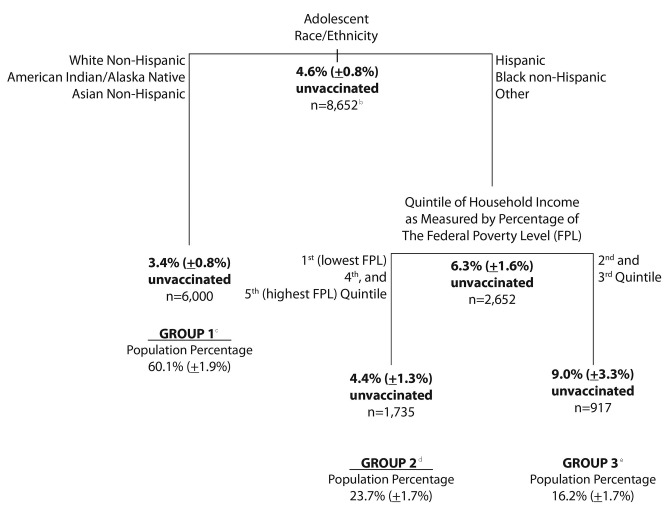
Multivariable analyses found that among the 19 demographic and 10 vaccine-related belief factors measured on parents of adolescents, no vaccine-related parental belief factors and only two demographic factors (i.e., race/ethnicity and household income) were independently associated with vaccination of adolescents (Figure 2). In particular, compared with non-Hispanic white, American Indian/Alaska Native, and non-Hispanic Asian adolescents, Hispanic and non-Hispanic black adolescents were significantly less likely to be vaccinated against measles by 2.9 (95% CI 1.1, 4.7) percentage points. The multivariable analysis segmented the population of adolescents into three groups. However, few significant differences in vaccine-related parental beliefs and no increasing pattern of negative parental beliefs were found across these groups (Table 4).
Figure 2.
Percentage of 13- to 17-year-old unvaccinated adolescents, by independent factors associated with being unvaccinated determined from the multivariable recursive partitioninga analysis, 2010 NIS-Teen
aRecursive partitioning is a multivariable statistical method that creates a decision tree that attempts to classify members of the population based on several independent variables.
bn = unweighted sample size associated with the listed percentage
cGroup 1 consists of adolescents who were either non-Hispanic white, American Indian/Alaska Native, or non-Hispanic Asian.
dGroup 2 consists of adolescents who were either Hispanic, non-Hispanic black, or of another race/ethnicity and lived in a household with an annual income in the first, fourth, or fifth income quintile.
eGroup 3 consists of adolescents who were either Hispanic, non-Hispanic black, or of another race/ethnicity and lived in a household with an annual income in the second or third income quintile.
DISCUSSION
In the United States in 2013, 7.5% of 19- to 35-month-old children and 4.5% of 13- to 17-year-old adolescents were unvaccinated against measles. Our analyses found that unvaccinated children and adolescents clustered within certain U.S. counties disproportionately with respect to the fraction of the national populations of children and adolescents that those counties represent. Among 210 selected counties representing more than a majority of the U.S. population of children and adolescents, the percentage of children and adolescents unvaccinated against measles was as high as 18.0% and 9.1%, respectively. Additionally, the upper decile of the number of children and adolescents unvaccinated against measles ranged from several tens of thousands to several thousands. Our data and other data45 highlight appreciable levels of measles susceptibility despite high levels of population immunity to measles nationally,37,38 and suggest a substantial risk of large measles outbreaks with the potential for reestablishment of sustained measles transmission in these communities if measles is introduced.
Although the popular media20,21 have suggested that parents' decision not to vaccinate their children against measles is a manifestation of the influence from the anti-vaccine movement, our analyses found that (1) the percentage of children who were unvaccinated that was attributable to factors other than parents' negative beliefs about the necessity of vaccines or vaccine refusal was 74.6% and (2) among all children unvaccinated against measles, 89.6% were deemed to have had missed opportunities because they were administered at least one dose of another recommended childhood vaccine after 12 months of age. Also, our study found that among all 19- to 35-month-old children unvaccinated against measles, only 34.6% had a parent who reported refusing vaccine doses. These findings suggest that missed opportunities to vaccinate are the main factor associated with not being vaccinated against measles and support the use of standards of care for pediatric immunization practices recommending that providers review children's vaccination records at every visit to assess the need for catch-up doses of measles and other vaccines.46 Client reminder and recall systems47,48 have been shown to be effective as part of a strategy to administer missed doses of all recommended vaccines.
Children affected by the measles resurgence of the late 1980s and early 1990s were often unvaccinated against measles because of financial or other barriers.49 Similarly, our data suggest that compared with children who are vaccinated against measles, children who are unvaccinated against measles are significantly less likely to be covered by health insurance. Although children who are not covered by health insurance are entitled to publicly purchased vaccines at no cost from providers enrolled in their state's Vaccines for Children Program (VFC), VFC-entitled children and adolescents are known to live in lower socioeconomic conditions50,51 and other barriers to vaccination may remain.52
Also, we found that a relatively small percentage (5.5%) of children had parents who believed that vaccines are not necessary to protect the health of children. Among those children, a relatively high percentage (33.6%) were unvaccinated against measles, and more than a majority (77.6%) had parents who deliberately refused the administration of vaccine doses for their children and held many unfavorable vaccine-related beliefs. Special advice is available to vaccination providers for communicating with parents who have unfavorable vaccine-related beliefs.53,54 That advice includes listening to parents to understand and address their concerns and making a clear, strong, and unambiguous recommendation to vaccinate. It is especially important to keep the lines of communication open with those parents and to revisit the conversation on subsequent visits, because the majority of children who acquire measles in the United States have parents with unfavorable vaccine-related beliefs.4,14,19 The higher risk may be due to (1) their traveling internationally or having international visitors from countries where measles continues to be endemic and/or (2) their clustering to a greater degree because of shared interests that may include participating in educational, social, and religious events with other children whose parents are like-minded.
Among adolescents, multivariable analysis found that vaccine-related parental beliefs were not independently associated with being unvaccinated, but that being Hispanic or non-Hispanic black was associated with a higher rate of being unvaccinated. These findings support the use of standards of care for pediatric immunization practices46 recommending that providers review vaccination records at every adolescent visit and provide catch-up doses of measles and other vaccines for the purposes of increasing measles vaccination coverage among adolescents and for decreasing the racial/ethnic disparity our analysis identified.
Limitations
This study was subject to several limitations. First, while all of the annual surveys of the NIS and NIS-Teen used in our study collected data from households with a landline telephone, the 2011–2013 surveys also collected data from households with cell phones. Although the response rates of the telephone portions of the NIS and NIS-Teen can be low, the analysis described in the Appendix shows that NIS and NIS-Teen estimates compare favorably with vaccination coverage estimates from the National Health Interview Survey, which has a response rate of approximately 90%.55 A further limitation was that some states with large populations (e.g., California) were allocated a disproportionately small percentage of the national NIS and NIS-Teen sample, thereby limiting our ability to obtain precise estimates among some counties where the population is large. A final limitation was that the NIS and NIS-Teen record dates on visits to primary HCPs only for dates on which vaccinations are administered. Other visit dates may have existed for a purpose other than vaccine administration. Because children and adolescents may have been eligible but were not administered routinely recommended vaccine doses at those visits, our estimates of the percentage who had a missed opportunity may be underestimated. However, as our point estimate for that percentage (89.6%) and the upper bound of its 95% CI (93.1%) were very high, the degree to which our statistics underestimated the percentage of children who had a missed opportunity could not be appreciable.
CONCLUSION
Through a successful measles vaccination program, the United States has eliminated year-round endemic measles transmission and the accompanying heavy annual health burden from measles and its complications.56 However, sustaining elimination requires maintaining high measles vaccine coverage rates, particularly among preschool and school-aged children and among adolescents, to provide sufficiently high population immunity (>93%) to result in herd immunity,3,57 which would decrease the risk of measles exposure and afford protection to those who cannot be vaccinated. In 2013, 17 states had <90% coverage for ≥1 measles-mumps-rubella dose for 19- to 35-month-old children.37 Achieving and maintaining very high vaccination coverage for measles in all communities is the most effective strategy to reduce the risk of measles outbreaks and reestablish endemic disease transmission. Approaches to achieving higher vaccine coverage should account for our findings that (1) unvaccinated children and adolescents cluster within certain counties, (2) reasons other than parents' negative vaccine-related beliefs account for the majority of children and adolescents unvaccinated against measles, and (3) most children unvaccinated against measles have been administered doses of other recommended vaccines after 12 months of age. Strategies to address missed opportunities should be addressed.
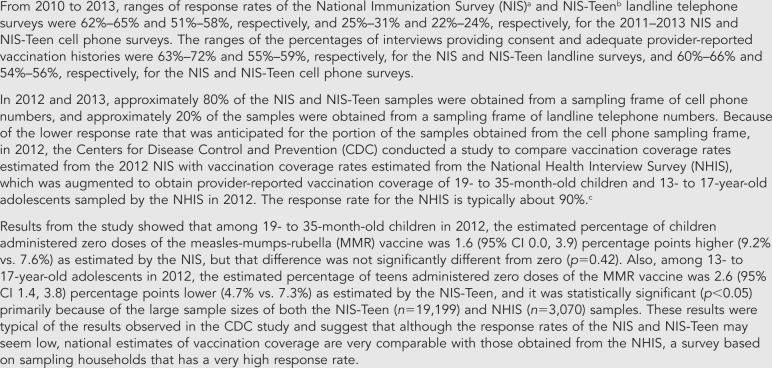
Appendix.
Comparisons of vaccination coverage estimates from the NIS and NIS-Teen with estimates from the National Health Interview Survey, 2012
aSmith PJ, Battaglia MP, Huggins VJ, Hoaglin DC, Roden A, Khare M, et al. Overview of the sampling design and statistical methods used in the National Immunization Survey. Am J Prev Med 2001;20(4 Suppl):17-24.
bJain N, Singleton JA, Montgomery M, Skalland B. Determining accurate vaccination coverage rates for adolescents: the National Immunization Survey-Teen 2006. Public Health Rep 2009;124:642-51.
cCenters for Disease Control and Prevention (US). About the National Health Interview Survey [cited 2015 Apr 6]. Available from: URL: http://www.cdc.gov/nchs/nhis/about_nhis.htm
NIS = National Immunization Survey
Footnotes
The authors have written permission to thank and acknowledge Drs. Alan B. Bloch and Holly A. Hill for their careful reading and editing of the manuscript. Also, the authors have written permission to thank and acknowledge Dr. Kennon Copeland, Ms. Wei Zeng, and Ms. Michele Koppelman at the National Center for Opinion Research for providing estimates of differences in vaccination coverage obtained between the National Health Interview Survey and the National Immunization Survey (NIS) and NIS-Teen.
The NIS and NIS-Teen have been approved annually by the Ethics and Research Review Board of the National Center for Health Statistics.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Orenstein WA, Papania MJ, Wharton ME. Measles elimination in the United States. J Infect Dis. 2004;189(Suppl 1):S1–3. doi: 10.1086/377693. [DOI] [PubMed] [Google Scholar]
- 2.Black CL, Yankey D, Kolasa M. National, state, and local area vaccination coverage among children aged 19–35 months—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(35):689–96. [PubMed] [Google Scholar]
- 3.Gay NJ. The theory of measles elimination: implications for the design of elimination strategies. J Infect Dis. 2004;189(Suppl 1):S27–35. doi: 10.1086/381592. [DOI] [PubMed] [Google Scholar]
- 4.Gastanaduy PA, Redd SB, Parker Fiebelkorn A, Rota JS, Rota PA, Bellini WJ, et al. Measles—United States, January 1–May 23, 2014. MMWR Morb Mortal Wkly Rep. 2014;63(22):496–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Parker Fiebelkorn A, Redd SB, Gallagher K, Rota PA, Rota J, Bellini W, et al. Measles in the United States during the postelimination era. J Infect Dis. 2010;202:1520–8. doi: 10.1086/656914. [DOI] [PubMed] [Google Scholar]
- 6.Green M, Levin J, Michaels M, Vasbinder S, Voorhees R, Lute J, et al. Hospital-associated measles outbreak—Pennsylvania, March–April 2009. MMWR Morb Mortal Wkly Rep. 2012;61(02):30–2. [PubMed] [Google Scholar]
- 7.Grigg MA, Brzezny AL, Dawson J, Rietberg K, DeBolt C, Linchangco P, et al. Update: measles—United States, January–July 2008. MMWR Morb Mortal Wkly Rep. 2008;57(33):893–6. [PubMed] [Google Scholar]
- 8.Hassidim A, Waters-Montijo K, Wooten W, Sawyer M, Sidelinger D, Harriman K, et al. Outbreak of measles—San Diego, California, January–February 2008. MMWR Morb Mortal Wkly Rep. 2008;57(08):203–6. [PubMed] [Google Scholar]
- 9.Sugerman DE, Barskey AE, Delea MG, Ortega-Sanchez IR, Bi D, Ralston KJ, et al. Measles outbreak in a highly vaccinated population, San Diego, 2008: role of the intentionally undervaccinated. Pediatrics. 2010;125:747–55. doi: 10.1542/peds.2009-1653. [DOI] [PubMed] [Google Scholar]
- 10.Cocoros N, Hernandez R, Harrington N, Rausch-Phung E, Schulte CR, Blog D, et al. Notes from the field: measles transmission associated with international air travel—Massachusetts and New York, July–August 2010. MMWR Morb Mortal Wkly Rep. 2010;59(33):1073. [Google Scholar]
- 11.Notes from the field: measles outbreak—Hennepin County, Minnesota, February–March 2011. MMWR Morb Mortal Wkly Rep. 2011;60(13):421. [PubMed] [Google Scholar]
- 12.Notes from the field: measles outbreak—Indiana, June–July 2011. MMWR Morb Mortal Wkly Rep. 2011;60(34):1169. [PubMed] [Google Scholar]
- 13.Notes from the field: measles among U.S.-bound refugees from Malaysia—California, Maryland, North Carolina, and Wisconsin, August–September 2011. MMWR Morb Mortal Wkly Rep. 2011;60(37):1281–2. [PubMed] [Google Scholar]
- 14.Kodagoda D, El Amin NA, Nguyen V, Holguin J, Zipprich J, Harriman K, et al. Measles outbreak associated with an arriving refugee—Los Angeles County, California, August–September 2011. MMWR Morb Mortal Wkly Rep. 2012;61(21):385–9. [PubMed] [Google Scholar]
- 15.Measles—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(15):253–7. [PubMed] [Google Scholar]
- 16.Notices to readers: final 2011 reports of nationally notifiable infectious diseases [published erratum appears in MMWR Morb Mortal Wkly Rep 2012;61(46):954] MMWR Morb Mortal Wkly Rep. 2012;61(32):624–37. [Google Scholar]
- 17.Gahr P, DeVries AS, Wallace G, Miller C, Kenyon C, Sweet K, et al. An outbreak of measles in an undervaccinated community. Pediatrics. 2014;134:e229–39. doi: 10.1542/peds.2013-4260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith PJ, Singleton JA. County-level trends in vaccination coverage among children aged 19–35 months—United States, 1995–2008. MMWR Surveill Summ. 2011;60(4):1–92. [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (US), National Center for Immunization and Respiratory Diseases, Division of Viral Diseases. Documentation and verification of measles, rubella and congenital rubella syndrome elimination in the Region of the Americas: United States national report. 2012 Mar 28 [cited 2014 Dec 10] Available from: URL: http://www.cdc.gov/measles/downloads/report-elimination-measles-rubella-crs.pdf.
- 20.Chen PW. Putting us all at risk for measles. New York Times 2014 Jun 26 [cited 2014 Dec 8] Available from: URL: http://well.blogs.nytimes.com/2014/06/26/putting-us-all-at-risk-for-measles/?module=Search&mabReward=relbias%3As%2C%7B%222%22%3A%22RI%3A18%22%7D&_r=0.
- 21.Public Broadcasting Service (PBS) The vaccine war. Frontline 2015 Mar 24 [cited 2015 Apr 6] Available from: URL: http://www.pbs.org/wgbh/pages/frontline/the-vaccine-war.
- 22.Smith PJ, Humiston SG, Marcuse EK, Zhao Z, Dorell CG, Howes C, et al. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Rep. 2011;126(Suppl 2):135–46. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gust DA, Strine TW, Maurice E, Smith P, Yusuf H, Wilkinson M, et al. Underimmunization among children: effects of vaccine safety concerns on immunization status. Pediatrics. 2004;114:e16–22. doi: 10.1542/peds.114.1.e16. [DOI] [PubMed] [Google Scholar]
- 24.Salmon DA, Moulton LH, Omer SB, DeHart MP, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines among parents of school-aged children: a case-control study. Arch Pediatr Adolesc Med. 2005;59:470–6. doi: 10.1001/archpedi.159.5.470. [DOI] [PubMed] [Google Scholar]
- 25.Smith PJ, Kennedy AM, Wooten K, Gust DA, Pickering LK. Association between health care providers' influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics. 2006;118:e1287–92. doi: 10.1542/peds.2006-0923. [DOI] [PubMed] [Google Scholar]
- 26.Salmon DA, Sotir MJ, Pan WK, Berg JL, Omer SB, Stokley S, et al. Parental vaccine refusal in Wisconsin: a case-control study. WMJ. 2009;108:17–23. [PMC free article] [PubMed] [Google Scholar]
- 27.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics. 2010;125:654–9. doi: 10.1542/peds.2009-1962. [DOI] [PubMed] [Google Scholar]
- 28.Szilagyi PG, Rodewald LE. Missed opportunities for immunizations: a review of the evidence. J Public Health Manag Pract. 1996;2:18–25. doi: 10.1097/00124784-199600210-00005. [DOI] [PubMed] [Google Scholar]
- 29.Smith PJ, Battaglia MP, Huggins VJ, Hoaglin DC, Roden A, Khare M, et al. Overview of the sampling design and statistical methods used in the National Immunization Survey. Am J Prev Med. 2001;20(4 Suppl):17–24. doi: 10.1016/s0749-3797(01)00285-9. [DOI] [PubMed] [Google Scholar]
- 30.Jain N, Singleton JA, Montgomery M, Skalland B. Determining accurate vaccination coverage rates for adolescents: the National Immunization Survey-Teen 2006. Public Health Rep. 2009;124:642–51. doi: 10.1177/003335490912400506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Black CL, Wooten KG, Yankey D, Kolasa M. National and state vaccination coverage among children aged 19–35 months—United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(34):1157–63. [PubMed] [Google Scholar]
- 32.Black CL, Yankey D, Kolasa M. National, state, and local area vaccination coverage among children aged 19–35 months—United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(36):733–40. [PMC free article] [PubMed] [Google Scholar]
- 33.Black CL, Yankey D, Kolasa M. National, state, and local area vaccination coverage among children aged 19–35 months—United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(36):733–40. [PMC free article] [PubMed] [Google Scholar]
- 34.Dorell C, Stokley S, Yankey D, Liang JL, Markowitz L. National and state vaccination coverage among adolescents aged 13 through 17 years—United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(33):1117–23. [PubMed] [Google Scholar]
- 35.Dorell C, Stokley S, Yankey D, Jeyarajah J, MacNeil J, Markowitz L. National and state vaccination coverage among adolescents aged 13–17 years—United States, 2011 [published erratum appears in MMWR Morb Mortal Wkly Rep 2012;61(41):844] MMWR Morb Mortal Wkly Rep. 2012;61(34):671–7. [Google Scholar]
- 36.Robinette Curtis C, Yankey D, Jeyarajah J, Stokley S, MacNeil J, Hariri S. National and state vaccination coverage among adolescents aged 13–17 years—United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(34):685–93. [PMC free article] [PubMed] [Google Scholar]
- 37.Elam-Evans LD, Yankey D, Singleton JA, Kolasa M. National, state, and selected local area vaccination coverage among children aged 19–35 months—United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(34):741–8. [PMC free article] [PubMed] [Google Scholar]
- 38.Elam-Evans LD, Yankey D, Jeyarajah J, Singleton JA, Robinette Curis C, MacNeil J, et al. National, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(29):625–33. [PMC free article] [PubMed] [Google Scholar]
- 39.Smith PJ, Singleton JA. Vaccination coverage for selected counties: attainment of Healthy People 2010 goals and association with indices of access to care, economic conditions, and demographic composition. Public Health Rep. 2008;123:155–72. doi: 10.1177/003335490812300208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rosenstock IM, Derryberry M, Carriger BK. Why people fail to seek poliomyelitis vaccination. Public Health Rep. 1959;74:98–104. [PMC free article] [PubMed] [Google Scholar]
- 41.Breiman L, Friedman J, Stone CJ, Olshen RA. Boca Raton (FL): Chapman & Hall/CRC; 1984. Classification and regression trees. [Google Scholar]
- 42.Zhang H, Singer B. 2nd ed. New York: Springer; 1999. Recursive partitioning in the health sciences. [Google Scholar]
- 43.Cole P, MacMahon B. Attributable risk percent in case-control studies. Brit J Prev Soc Med. 1971;25:242–4. doi: 10.1136/jech.25.4.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lumley T. Analysis of complex survey samples. J Stat Software. 2004;9:1–19. [Google Scholar]
- 45.Lieu TA, Ray GT, Klein NP, Chung C, Kulldorff M. Geographic clusters in underimmunization and vaccine refusal. Pediatrics. 2015;135:280–9. doi: 10.1542/peds.2014-2715. [DOI] [PubMed] [Google Scholar]
- 46.National Vaccine Advisory Committee. Standards for pediatric immunization practices. MMWR Recomm Rep. 1993;42(RR-5) 001. [PubMed] [Google Scholar]
- 47.Szilagyi PG, Bordley C, Vann JC, Chelminski A, Kraus RM, Margolis PA, et al. Effect of patient reminder/recall interventions on immunization rates: a review. JAMA. 2000;284:1820–7. doi: 10.1001/jama.284.14.1820. [DOI] [PubMed] [Google Scholar]
- 48.Saville AW, Beaty B, Dickinson LM, Lockhart S, Kempe A. Novel immunization reminder/recall approaches: rural and urban differences in parent perceptions. Acad Pediatr. 2014;14:249–55. doi: 10.1016/j.acap.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Orenstein WA, Atkinson W, Mason D, Bernier RH. Barriers to vaccinating preschool children. J Health Care Poor Underserved. 1990;1:315–30. doi: 10.1353/hpu.2010.0324. [DOI] [PubMed] [Google Scholar]
- 50.Smith PJ, Lindley MC, Rodewald LE. Vaccination coverage among U.S. children aged 19–35 months entitled by the Vaccines for Children Program, 2009. Public Health Rep. 2011;126(Suppl 2):109–23. doi: 10.1177/00333549111260S213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lindley MC, Smith PJ, Rodewald LE. Vaccination coverage among U.S. adolescents aged 13–17 years entitled by the Vaccines for Children Program, 2009. Public Health Rep. 2011;126(Suppl 2):124–34. doi: 10.1177/00333549111260S214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lannon C, Brack V, Stuart J, Caplow M, McNeill A, Bordley WC, et al. What mothers say about why poor children fall behind on immunizations. Arch Pediatr Adolesc Med. 1995;149:1070–5. doi: 10.1001/archpedi.1995.02170230024003. [DOI] [PubMed] [Google Scholar]
- 53.Diekema DS American Academy of Pediatrics Committee on Bioethics. Responding to parental refusals of immunization of children. Pediatrics. 2005;115:1428–31. doi: 10.1542/peds.2005-0316. [DOI] [PubMed] [Google Scholar]
- 54.Diekema DS. Improving childhood vaccination rates. N Engl J Med. 2012;366:391–3. doi: 10.1056/NEJMp1113008. [DOI] [PubMed] [Google Scholar]
- 55.Centers for Disease Control and Prevention (US) About the National Health Interview Survey [cited 2015 Apr 6] Available from: URL: http://www.cdc.gov/nchs/nhis/about_nhis.htm.
- 56.Bloch AB, Orenstein WA, Stetler HC, Wassilak SG, Amler RW, Bart KJ, et al. Health impact of measles vaccination in the United States. Pediatrics. 1985;76:524–32. [PubMed] [Google Scholar]
- 57.Fine P, Eames, Heymann DL. “Herd immunity”: a rough guide. Clin Infect Dis. 2011;52:911–6. doi: 10.1093/cid/cir007. [DOI] [PubMed] [Google Scholar]