Abstract
Purpose
Citation counting can be used to evaluate the impact an article has made on its discipline. This study characterizes the most cited articles related to clinical pediatric neurosurgery as of July 2013.
Methods
A list of search terms was computed using Thomson Reuters Web of Science® (WOS) to capture the 100 most cited articles in the overall literature and the top 50 articles from 2002 to 2012 related to clinical pediatric neurosurgery from non-dedicated pediatric neurosurgical journals. The following information was recorded for each article: number of authors, country of origin, citation count adjusted for number of years in print, topic, and level of evidence.
Results
The 100 most cited articles appeared in 44 journals. Publication dates ranged from 1986 to 2008; two were class 1 evidence, nine class 2, 26 class 3, and 52 class 4. Citations ranged from 90 to 321 (mean=131); average time-adjusted citation count was 10. The 50 most cited articles from 2002 to 2012 appeared in 31 journals; four were class 2 evidence, 15 class 3, and 21 class 4. Citations ranged from 68 to 245 (mean=103); average time-adjusted citation count was 13.
Conclusion
Overall, papers from non-pediatric neurosurgical journals had higher citation counts and improved level of evidence grades compared to articles from pediatric neurosurgical periodicals. An original paper related to clinical pediatric neurosurgery in a non-pediatric neurosurgical journal having a total citation count of 100–150 or more and an average citation count of 10–15 per year or more can be considered a high-impact publication.
Keywords: Citation, Analysis, Articles, Pediatric, Neurosurgery
Introduction
The amount of biomedical information continues to expand at a rapid pace, making it difficult for researchers to stay up-to-date. PubMed, for example, is a free Web literature search engine developed by the National Center for Biotechnology Information (NCBI) that provides access to 38 databases [1, 2]. As of 2013, it contains more than 23 million citations for biomedical literature from MEDLINE, life science journals, and online books [3]. PubMed currently includes citations and abstracts from over 5,000 life science journals for biomedical articles back to 1948. How do researchers make their way through this and other vast repositories of publications to find those that are directly related to their area(s) of interest? Furthermore, is there a way to quantify an article's impact and rank articles based on such a metric? Bibliometrics and citation analysis provide methods to quantitatively analyze, compare, and manage the vast amount of biomedical information in existence. Citation analysis is currently the best way to evaluate a publication's impact upon a research community. Although it has its limitations, citation analysis assumes that an article's citation count is directly related to the interest that article has generated within the scientific community. Those articles that have generated debate, stimulated further research, or altered how we view or treat patients with certain maladies are cited more heavily. PubMed, while easy to use and free, does not perform any computations based on citation analysis and thus cannot provide the user with a dynamic, upto-date measurable assessment of the current and historical research efforts of a particular topic. Although one can refine their search based on certain criteria, the output by PubMed is ultimately volumetric only.
Google Scholar (http://scholar.google.com/), introduced in 2004, is a free online service that ranks search results according to their impact on the field. Although some have been skeptical about the fact that it does not provide a list of its sources and uses a proprietary undisclosed ranking algorithm resulting in a wide coverage [4], studies have shown that most citations are scholarly [5–7]. In July 2013, they released the “2013 Scholar Metrics,” which allows users to gauge the visibility and influence of articles published in scholarly publications between 2008 and 2012. One can browse a ranking of publications based on a specific journal (e.g., Lancet) or research category (e.g., “health and medical sciences”). In addition, Google Scholar can provide a bibliometric measurement for a selected author or journal. In 2006, Plikus et al. created PubFocus (www.pubfocus.org), a citations’ prioritization algorithm based on journal impact factor, forward referencing volume, citation dynamics, and author's contribution level [8]. It enriches MEDLINE/PubMed search queries with two widely used human factor-based bibliometric indicators of publication quality: journal impact factor and volume of forward references (i.e., citations).
Several studies have established landmark articles within various specialties using citation analysis, including anesthesiology [9], critical care [10], dermatology [11], emergency medicine [12], forensic science [13–15], ophthalmology [16], orthopedic surgery [17], otolaryngology [18], pediatric orthopedic surgery [19], plastic surgery [20, 21], urology [22, 23], and neurosurgery [24, 25]. Recently, we published the top 100 overall most cited articles and the top 50 most cited articles over the last decade (2002–2012) from pediatric neurosurgical journals [26]. A comparison was made to time-adjusted and non-time-adjusted citation rankings. We defined a “historical classic” as an article that received at least 100 total citations and a time-adjusted citation count of five citations per year. A “contemporary classic” was defined as an article in the last decade that received a total of 50 or more citations and a time-adjusted citation count of five citations per year. A limitation of our study was that we only analyzed articles from pediatric neurosurgical journals, thus excluding important articles from other “multidisciplinary” sources such as Neurosurgery, Journal of Neurosurgery, JAMA, New England Journal of Medicine, Journal of Clinical Oncology, etc. We present the second part of our pediatric neurosurgery citation analysis research.
Methods
A topic search was performed in July 2013 using Thomson Reuters Web of Science (WOS). Table 1 shows the keywords used in each topic search. These keywords were modified based on the methods of Ponce et al. [24, 25]. A total of 14, 408 articles were identified in this search. Each term was searched along with the word “pediatric” in order to capture articles both related to the topic and to a pediatric population. These articles were then ranked in descending order by citation count and reviewed to determine if they were related to clinical pediatric neurosurgery. All basic science, imaging, histology, pathology, and pharmaceutical articles were excluded. We excluded articles from pediatric neurosurgical journals: Child's Brain, Pediatric Neurosurgery, Child's Nervous System, and Journal of Neurosurgery: Pediatrics. An additional search was performed using the same criteria to identify the top 50 most cited articles over the last 10 years (2002–2012). This search returned a total of 10,335 articles. An “adjusted” citation count or index was calculated for each article by dividing the total number of citations by the years since initial publication. The adjusted citation count can be viewed as the average number of citations that paper has received each year since it was published.
Table 1.
Keywords used in WOS searches
| Topic | Keywords used in WOS topic search |
|---|---|
| General | Brain surgery, neurosurgery, peripheral nerve |
| CSF | Hydrocephalus, arachnoid cyst, ventricular shunt* |
| Vascular | Aneurysm, cavernous malformation, intracranial bypass, intracranial aneurysm, subarachnoid hemorrhage, arteriovenous malformation* |
| Congenital | Craniosynostosis, dysphrasism |
| Tumor | Glioma, medulloblastoma, pineal*, meningioma, radiosurgery, radiotherapy |
| Trauma | Brain injury, coma, head injury, brain damage, spinal injury |
| Functional | Deep brain stimulation, epilepsy surgery, spinal cord stimulation, trigeminal neuralgia, stereotactic, stereotaxic, stereotaxy |
| Spine | Spine fusion, spine fixation, spine surgery, spinal fixation, spinal surgery |
Asterisk represents a wild card character For example, the word “pineal*” would return “pineal” and “pinealblastoma” when used with a wild card character
Data
The following information was obtained from each article: number of authors, country of origin, topic (hydrocephalus, oncology, vascular, trauma, functional/epilepsy/spasticity, congenital spine/tethered cord, congenital cranial/craniosynostosis/arachnoid cyst, and other), and level of evidence (Levels 1–5 using the Oxford Centre for Evidence-Based Medicine—i.e., OCEBM—2011 Levels of Evidence (Table 4 in Appendix 1), http://www.cebm.net/index.aspx?o=5653, and the accompanying table of evidence glossary) [27]. The abstract or—when necessary—the entire article was read in detail to determine these characteristics and categories.
Results
The top 100 overall most cited works within pediatric neurosurgery are listed in Table 2. The top 50 most cited works within pediatric neurosurgery over the past decade (2002–2012) are presented in Table 3.
Table 2.
List of top 100 most cited journal articles. The first rank represents the descending rank order by raw citations. The second rank (“adjusted rank”) is based on the adjusted citation index (number of citations divided by years since initial publication). The column titled “class” is the class of evidence for the article based on the 2011 Oxford Centre Level of Evidence classification scheme
| Article | Rank | Citations | Adjusted rank | Adjusted citations | Class |
|---|---|---|---|---|---|
| Luerssen TG, Klauber MR, Marshall LF (1988) Outcome from head injury related to patient's age. A longitudinal prospective study of adult and pediatric head injury. Journal of Neurosurgery 68: 409-416 | 1 | 321 | 20 | 12.8 | 3 |
| Levisohn L, Cronin-Golomb A, Schmahmann JD (2000) Neuropsychological consequences of cerebellar tumour resection in children: cerebellar cognitive affective syndrome in a paediatric population. Brain 123: 1041-1050 | 2 | 306 | 4 | 23.5 | 4 |
| Zeltzer PM, Boyett JM, Finlay JL, Albright AL, Rorke LB, Milstein JM, Allen JC, Stevens KR, Stanley P, Li H, Wisoff JH, Geyer JR, McGuire-Cullen P, Stehbens JA, Shurin SB, Packer RJ (1999) Metastasis stage, adjuvant treatment, and residual tumor are prognostic factors for medulloblastoma in children: conclusions from the Children's Cancer Group 921 randomized phase III study. Journal of Clinical Oncology 17: 832-845 | 3 | 294 | 5 | 21.0 | 2 |
| Wyllie E, Comair YG, Kotagal P, Bulacio J, Bingaman W, Ruggieri P (1998) Seizure outcome after epilepsy surgery in children and adolescents. Annals of Neurology 44: 740-748 | 4 | 287 | 7 | 19.1 | 4 |
| Drake JM, Kestle JR, Milner R, Cinalli G, Boop F, Piatt J, Jr., Haines S, Schiff SJ, Cochrane DD, Steinbok P, MacNeil N (1998) Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery 43: 294-303 | 5 | 282 | 8 | 18.8 | 2 |
| Polin RS, Shaffrey ME, Bogaev CA, Tisdale N, Germanson T, Bocchicchio B, Jane JA (1997) Decompressive bifrontal craniectomy in the treatment of severe refractory posttraumatic cerebral edema. Neurosurgery 41: 84-92 | 6 | 251 | 15 | 15.7 | 3 |
| Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE (2004) Late neurocognitive sequelae in survivors of brain tumours in childhood. The Lancet Oncology 5: 399-408 | 7 | 245 | 2 | 27.2 | Review |
| Schachter SC, Saper CB (1998) Vagus nerve stimulation. Epilepsia 39: 677-686 | 8 | 190 | 23 | 12.7 | Other |
| Alberico AM, Ward JD, Choi SC, Marmarou A, Young HF (1987) Outcome after severe head injury. Relationship to mass lesions, diffuse injury, and ICP course in pediatric and adult patients. Journal of Neurosurgery 67: 648-656 | 9 | 180 | 63 | 6.9 | 3 |
| Hutchison JS, Ward RE, Lacroix J, Hebert PC, Barnes MA, Bohn DJ, Dirks PB, Doucette S, Fergusson D, Gottesman R, Joffe AR, Kirpalani HM, Meyer PG, Morris KP, Moher D, Singh RN, Skippen PW, Hypothermia Pediatric Head Injury Trial Investigators and the Canadian Critical Care Trials Group (2008) Hypothermia therapy after traumatic brain injury in children. The New England Journal of Medicine 358: 2447-2456 | 10 | 175 | 1 | 35.0 | 2 |
| Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N (2002) A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology 16: 15-27 | 11 | 174 | 14 | 15.8 | 3 |
| Choux M, Genitori L, Lang D, Lena G (1992) Shunt implantation: reducing the incidence of shunt infection. Journal of Neurosurgery 77: 875-880 | 12 | 170 | 48 | 8.1 | 4 |
| Hadley MN, Zabramski JM, Browner CM, Rekate H, Sonntag VK (1988) Pediatric spinal trauma. Review of 122 cases of spinal cord and vertebral column injuries. Journal of Neurosurgery 68: 18-24 | 13 | 167 | 69 | 6.7 | 4 |
| Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH (2003) A population-based study of inflicted traumatic brain injury in young children. JAMA 290: 621-626 | 14 | 164 | 11 | 16.4 | 3 |
| Pigula FA, Wald SL, Shackford SR, Vane DW (1993) The effect of hypotension and hypoxia on children with severe head injuries. Journal of Pediatric Surgery 28: 310-314 | 15 | 161 | 49 | 8.1 | 3 |
| Sebire G, Tabarki B, Saunders DE, Leroy I, Liesner R, Saint-Martin C, Husson B, Williams AN, Wade A, Kirkham FJ (2005) Cerebral venous sinus thrombosis in children: risk factors, presentation, diagnosis and outcome. Brain 128: 477-489 | 16 | 160 | 6 | 20.0 | 4 |
| Simma B, Burger R, Falk M, Sacher P, Fanconi S (1998) A prospective, randomized, and controlled study of fluid management in children with severe head injury: lactated Ringer's solution versus hypertonic saline. Critical Care Medicine 26: 1265-1270 | 17 | 157 | 32 | 10.5 | 2 |
| Tihan T, Fisher PG, Kepner JL, Godfraind C, McComb RD, Goldthwaite PT, Burger PC (1999) Pediatric astrocytomas with monomorphous pilomyxoid features and a less favorable outcome. Journal of Neuropathology and Experimental Neurology 58: 1061-1068 | 18 | 151 | 30 | 10.8 | 4 |
| Pudenz RH, Foltz EL (1991) Hydrocephalus: overdrainage by ventricular shunts. A review and recommendations. Surgical Neurology 35: 200-212 | 19 | 145 | 72 | 6.6 | Review |
| Scott RM, Smith JL, Robertson RL, Madsen JR, Soriano SG, Rockoff MA (2004) Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. Journal of Neurosurgery 100: 142-149 | 20 | 143 | 12 | 15.9 | 4 |
| Ciricillo SF, Cogen PH, Harsh GR, Edwards MS (1991) Intracranial arachnoid cysts in children. A comparison of the effects of fenestration and shunting. Journal of Neurosurgery 74: 230-235 | 21 | 141 | 76 | 6.4 | 4 |
| Palmer SL, Goloubeva O, Reddick WE, Glass JO, Gajjar A, Kun L, Merchant TE, Mulhern RK (2001) Patterns of intellectual development among survivors of pediatric medulloblastoma: a longitudinal analysis. Journal of Clinical Oncology 19: 2302-2308 | 22 | 140 | 26 | 11.7 | 4 |
| Van Effenterre R, Boch AL (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. Journal of Neurosurgery 97: 3-11 | 22 | 140 | 22 | 12.7 | 4 |
| Ruge JR, Sinson GP, McLone DG, Cerullo LJ (1988) Pediatric spinal injury: the very young. Journal of Neurosurgery 68: 25-30 | 24 | 139 | 82 | 5.6 | 4 |
| Matsushima T, Inoue T, Suzuki SO, Fujii K, Fukui M, Hasuo K (1992) Surgical treatment of moyamoya disease in pediatric patients—comparison between the results of indirect and direct revascularization procedures. Neurosurgery 31: 401-405 | 24 | 139 | 70 | 6.6 | 4 |
| Karavitaki N, Brufani C, Warner JT, Adams CB, Richards P, Ansorge O, Shine B, Turner HE, Wass JA (2005) Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term follow-up. Clinical Endocrinology 62: 397-409 | 24 | 139 | 10 | 17.4 | 4 |
| Anderson V, Moore C (1995) Age at injury as a predictor of outcome following pediatric head injury: a longitudinal perspective. Child Neuropsychology 1: 187-202 | 27 | 138 | 52 | 7.7 | 3 |
| Chumas PD, Armstrong DC, Drake JM, Kulkarni AV, Hoffman HJ, Humphreys RP, Rutka JT, Hendrick EB (1993) Tonsillar herniation: the rule rather than the exception after lumboperitoneal shunting in the pediatric population. Journal of Neurosurgery 78: 568-573 | 28 | 136 | 67 | 6.8 | 4 |
| Khanna S, Davis D, Peterson B, Fisher B, Tung H, O'Quigley J, Deutsch R (2000) Use of hypertonic saline in the treatment of severe refractory posttraumatic intracranial hypertension in pediatric traumatic brain injury. Critical Care Medicine 28: 1144-1151 | 28 | 136 | 33 | 10.5 | 3 |
| Kulkarni AV, Drake JM, Lamberti-Pasculli M (2001) Cerebrospinal fluid shunt infection: a prospective study of risk factors. Journal of Neurosurgery 94: 195-201 | 28 | 136 | 27 | 11.3 | 3 |
| Tong KA, Ashwal S, Holshouser BA, Nickerson JP, Wall CJ, Shutter LA, Osterdock RJ, Haacke EM, Kido D (2004) Diffuse axonal injury in children: clinical correlation with hemorrhagic lesions. Annals of Neurology 56: 36-50 | 28 | 136 | 16 | 15.1 | 2 |
| Fay GC, Jaffe KM, Polissar NL, Liao S, Rivara JB, Martin KM (1994) Outcome of pediatric traumatic brain injury at three years: a cohort study. Archives of Physical Medicine and Rehabilitation 75: 733-741 | 32 | 135 | 59 | 7.1 | 3 |
| Merchant TE, Mulhern RK, Krasin MJ, Kun LE, Williams T, Li C, Xiong X, Khan RB, Lustig RH, Boop FA, Sanford RA (2004) Preliminary results from a phase II trial of conformal radiation therapy and evaluation of radiation-related CNS effects for pediatric patients with localized ependymoma. Journal of Clinical Oncology 22: 3156-3162 | 33 | 131 | 17 | 14.6 | 4 |
| Kazak AE, Alderfer M, Rourke MT, Simms S, Streisand R, Grossman JR (2004) Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. Journal of Pediatric Psychology 29: 211-219 | 33 | 131 | 17 | 14.6 | 3 |
| Kuroda S, Houkin K (2008) Moyamoya disease: current concepts and future perspectives. Lancet Neurology 7: 1056-1066 | 35 | 130 | 3 | 26.0 | Review |
| Kraus JF, Fife D, Cox P, Ramstein K, Conroy C (1986) Incidence, severity, and external causes of pediatric brain injury. American Journal of Diseases of Children 140: 687-693 | 36 | 129 | 92 | 4.8 | 4 |
| Duff J, Meyer FB, Ilstrup DM, Laws ER, Jr., Schleck CD, Scheithauer BW (2000) Long-term outcomes for surgically resected craniopharyngiomas. Neurosurgery 46: 291-302 | 37 | 128 | 34 | 9.8 | 4 |
| Vining EP, Freeman JM, Pillas DJ, Uematsu S, Carson BS, Brandt J, Boatman D, Pulsifer MB, Zuckerberg A (1997) Why would you remove half a brain? The outcome of 58 children after hemispherectomy—the Johns Hopkins experience: 1968 to 1996. Pediatrics 100: 163-171 | 37 | 128 | 50 | 8.0 | 4 |
| Grill J, Renaux VK, Bulteau C, Viguier D, Levy-Piebois C, Sainte-Rose C, Dellatolas G, Raquin MA, Jambaquel, Kalifa C (1999) Long-term intellectual outcome in children with posterior fossa tumors according to radiation doses and volumes. International Journal of Radiation Oncology, Biology, Physics 45: 137-145 | 39 | 127 | 38 | 9.1 | 4 |
| Adelson PD, Ragheb J, Kanev P, Brockmeyer D, Beers SR, Brown SD, Cassidy LD, Chang Y, Levin H (2005) Phase II clinical trial of moderate hypothermia after severe traumatic brain injury in children. Neurosurgery 56: 740-754 | 39 | 127 | 13 | 15.9 | 2 |
| Pollack IF, Claassen D, al-Shboul Q, Janosky JE, Deutsch M (1995) Low-grade gliomas of the cerebral hemispheres in children: an analysis of 71 cases. Journal of Neurosurgery 82: 536-547 | 41 | 126 | 61 | 7.0 | 4 |
| Hargrave D, Bartels U, Bouffet E (2006) Diffuse brainstem glioma in children: critical review of clinical trials. The Lancet Oncology 7: 241-248 | 41 | 126 | 9 | 18.0 | 1 |
| Janss AJ, Grundy R, Cnaan A, Savino PJ, Packer RJ, Zackai EH, Goldwein JW, Sutton LN, Radcliffe J, Molloy PT, et al. (1995) Optic pathway and hypothalamic/chiasmatic gliomas in children younger than age 5 years with a 6-year follow-up. Cancer 75: 1051-1059 | 43 | 124 | 64 | 6.9 | 4 |
| Cascino GD, Jack CR, Jr., Parisi JE, Marsh WR, Kelly PJ, Sharbrough FW, Hirschorn KA, Trenerry MR (1992) MRI in the presurgical evaluation of patients with frontal lobe epilepsy and children with temporal lobe epilepsy: pathologic correlation and prognostic importance. Epilepsy Research 11: 51-59 | 44 | 122 | 80 | 5.8 | 4 |
| Pollack IF, Albright AL, Adelson PD (1999) A randomized, controlled study of a programmable shunt valve versus a conventional valve for patients with hydrocephalus. Hakim-Medos Investigator Group. Neurosurgery 45: 1399-1408 | 44 | 122 | 41 | 8.7 | 2 |
| Tubbs RS, McGirt MJ, Oakes WJ (2003) Surgical experience in 130 pediatric patients with Chiari I malformations. Journal of Neurosurgery 99: 291-296 | 44 | 122 | 24 | 12.2 | 4 |
| Taylor HG, Yeates KO, Wade SL, Drotar D, Klein SK, Stancin T (1999) Influences on first-year recovery from traumatic brain injury in children. Neuropsychology 13: 76-89 | 47 | 120 | 43 | 8.6 | 3 |
| Wisoff JH, Boyett JM, Berger MS, Brant C, Li H, Yates AJ, McGuire-Cullen P, Turski PA, Sutton LN, Allen JC, Packer RJ, Finlay JL (1998) Current neurosurgical management and the impact of the extent of resection in the treatment of malignant gliomas of childhood: a report of the Children's Cancer Group trial no. CCG-945. Journal of Neurosurgery 89: 52-59 | 47 | 120 | 50 | 8.0 | 4 |
| Wyllie E, Comair YG, Kotagal P, Raja S, Ruggieri P (1996) Epilepsy surgery in infants. Epilepsia 37: 625-637 | 47 | 120 | 60 | 7.1 | 4 |
| Ommaya AK, Goldsmith W, Thibault L (2002) Biomechanics and neuropathology of adult and paediatric head injury. British Journal of Neurosurgery 16: 220-242 | 50 | 119 | 29 | 10.8 | Review |
| Gilbertson R, Wickramasinghe C, Hernan R, Balaji V, Hunt D, Jones-Wallace D, Crolla J, Perry R, Lunec J, Pearson A, Ellison D (2001) Clinical and molecular stratification of disease risk in medulloblastoma. British Journal of Cancer 85: 705-712 | 51 | 116 | 35 | 9.7 | 4 |
| Barlow KM, Minns RA (2000) Annual incidence of shaken impact syndrome in young children. Lancet 356: 1571-1572 | 51 | 116 | 39 | 8.9 | 3 |
| Yeates KO, Swift E, Taylor HG, Wade SL, Drotar D, Stancin T, Minich N (2004) Short- and long-term social outcomes following pediatric traumatic brain injury. Journal of the International Neuropsychological Society 10: 412-426 | 53 | 115 | 21 | 12.8 | 3 |
| Walter AW, Mulhern RK, Gajjar A, Heideman RL, Reardon D, Sanford RA, Xiong X, Kun LE (1999) Survival and neurodevelopmental outcome of young children with medulloblastoma at St Jude Children's Research Hospital. Journal of Clinical Oncology 17: 3720-3728 | 54 | 114 | 47 | 8.1 | 4 |
| Zemack G, Romner B (2000) Seven years of clinical experience with the programmable Codman Hakim valve: a retrospective study of 583 patients. Journal of Neurosurgery 92: 941-948 | 54 | 114 | 40 | 8.8 | 4 |
| Raffel C, McComb JG (1988) To shunt or to fenestrate: which is the best surgical treatment for arachnoid cysts in pediatric patients? Neurosurgery 23: 338-342 | 56 | 113 | 99 | 4.5 | 4 |
| Kraus JF, Fife D, Conroy C (1987) Pediatric brain injuries: the nature, clinical course, and early outcomes in a defined United States’ population. Pediatrics 79: 501-507 | 56 | 113 | 100 | 4.3 | 4 |
| Paolicchi JM, Jayakar P, Dean P, Yaylali I, Morrison G, Prats A, Resnik T, Alvarez L, Duchowny M (2000) Predictors of outcome in pediatric epilepsy surgery. Neurology 54: 642-647 | 58 | 112 | 42 | 8.6 | 4 |
| Grill J, Le Deley MC, Gambarelli D, Raquin MA, Couanet D, Pierre-Kahn A, Habrand JL, Doz F, Frappaz D, Gentet JC, Edan C, Chastagner P, Kalifa C, French Society of Pediatric Oncology (2001) Postoperative chemotherapy without irradiation for ependymoma in children under 5 years of age: a multicenter trial of the French Society of Pediatric Oncology. Journal of Clinical Oncology 19: 1288-1296 | 59 | 111 | 37 | 9.3 | 4 |
| Lustig RH, Post SR Srivannaboon K, Rose SR, Danish RK, Burghen GA, Xiong X, Wu S, Merchant TE (2003) Risk factors for the development of obesity in children surviving brain tumors. The Journal of Clinical Endocrinology and Metabolism 88: 611-616 | 60 | 110 | 28 | 11.0 | 4 |
| Huang MH, Gruss JS, Clarren SK, Mouradian WE, Cunningham ML, Roberts TS, Loeser JD, Cornell CJ (1996) The differential diagnosis of posterior plagiocephaly: true lambdoid synostosis versus positional molding. Plastic and Reconstructive Surgery 98: 765-774 | 61 | 109 | 75 | 6.4 | 4 |
| Skippen P, Seear M, Poskitt K, Kestle J, Cochrane D, Annich G, Handel J (1997) Effect of hyperventilation on regional cerebral blood flow in head-injured children. Critical Care Medicine 25: 1402-1409 | 61 | 109 | 66 | 6.8 | 3 |
| Tuli S, Drake J, Lawless J, Wigg M, Lamberti-Pasculli M (2000) Risk factors for repeated cerebrospinal shunt failures in pediatric patients with hydrocephalus. Journal of Neurosurgery 92: 31-38 | 63 | 108 | 44 | 8.3 | 3 |
| Packer RJ, Boyett JM, Zimmerman RA, Albright AL, Kaplan AM, Rorke LB, Selch MT, Cherlow JM, Finlay JL, Wara WM (1994) Outcome of children with brain stem gliomas after treatment with 7800 cGy of hyperfractionated radiotherapy. A Childrens Cancer Group Phase I/II Trial. Cancer 74: 1827-1834 | 64 | 105 | 83 | 5.5 | 4 |
| Mulhern RK, Reddick WE, Palmer SL, Glass JO, Elkin TD, Kun LE, Taylor J, Langston J, Gajjar A (1999) Neurocognitive deficits in medulloblastoma survivors and white matter loss. Annals of Neurology 46: 834-841 | 64 | 105 | 54 | 7.5 | 3 |
| Jaffe KM, Polissar NL, Fay GC, Liao S (1995) Recovery trends over three years following pediatric traumatic brain injury. Archives of Physical Medicine and Rehabilitation 76: 17-26 | 66 | 104 | 81 | 5.8 | 3 |
| Bouffet E, Perilongo G, Canete A, Massimino M (1998) Intracranial ependymomas in children: a critical review of prognostic factors and a plea for cooperation. Medical and Pediatric Oncology 30: 319-329 | 67 | 102 | 67 | 6.8 | Review |
| Freeman CR, Krischer JP, Sanford RA, Cohen ME, Burger PC, del Carpio R, Halperin EC, Munoz L, Friedman HS, Kun LE (1993) Final results of a study of escalating doses of hyperfractionated radiotherapy in brain stem tumors in children: a Pediatric Oncology Group study. International Journal of Radiation Oncology, Biology, Physics 27: 197–206 | 67 | 102 | 88 | 5.1 | 3 |
| Albanese A, Barnes MP, Bhatia KP, Fernandez-Alvarez E, Filippini G, Gasser T, Krauss JK, Newton A, Rektor I, Savoiardo M, Valls-Sole J (2006) A systematic review on the diagnosis and treatment of primary (idiopathic) dystonia and dystonia plus syndromes: report of an EFNS/MDS-ES Task Force. European Journal of Neurology 13: 433-444 | 69 | 101 | 19 | 14.4 | 1 |
| Armonda RA, Citrin CM, Foley KT, Ellenbogen RG (1994) Quantitative cine-mode magnetic resonance imaging of Chiari I malformations: an analysis of cerebrospinal fluid dynamics. Neurosurgery 35: 214-223 | 70 | 100 | 85 | 5.3 | Other |
| Pollack IF, Hoffman HJ, Humphreys RP, Becker L (1993) The long-term outcome after surgical treatment of dorsally exophytic brain-stem gliomas. Journal of Neurosurgery 78: 859-863 | 70 | 100 | 90 | 5.0 | 4 |
| Hamilton MG, Myles ST (1992) Pediatric spinal injury: review of 174 hospital admissions. Journal of Neurosurgery 77: 700-704 | 70 | 100 | 93 | 4.8 | 4 |
| Larson JJ, Ball WS, Bove KE, Crone KR, Tew JM, Jr. (1998) Formation of intracerebral cavernous malformations after radiation treatment for central nervous system neoplasia in children. Journal of Neurosurgery 88: 51-56 | 73 | 99 | 71 | 6.6 | 4 |
| Jaffe KM, Fay GC, Polissar NL, Martin KM, Shurtleff H, Rivara JB, Winn HR (1992) Severity of pediatric traumatic brain injury and early neurobehavioral outcome: a cohort study. Archives of Physical Medicine and Rehabilitation 73: 540-547 | 74 | 98 | 96 | 4.7 | 3 |
| Brown RL, Brunn MA, Garcia VF (2001) Cervical spine injuries in children: a review of 103 patients treated consecutively at a level 1 pediatric trauma center. Journal of Pediatric Surgery 36: 1107-1114 | 74 | 98 | 46 | 8.2 | 4 |
| Kondziolka D, Humphreys RP, Hoffman HJ, Hendrick EB, Drake JM (1992) Arteriovenous malformations of the brain in children: a forty year experience. The Canadian Journal of Neurological Sciences 19: 40-45 | 74 | 98 | 96 | 4.7 | 4 |
| Mandell LR, Kadota R, Freeman C, Douglass EC, Fontanesi J, Cohen ME, Kovnar E, Burger P, Sanford RA, Kepner J, Friedman H, Kun LE (1999) There is no role for hyperfractionated radiotherapy in the management of children with newly diagnosed diffuse intrinsic brainstem tumors: results of a Pediatric Oncology Group phase III trial comparing conventional vs. hyperfractionated radiotherapy. International Journal of Radiation Oncology, Biology, Physics 43: 959-964 | 74 | 98 | 61 | 7.0 | 2 |
| Poretti A, Grotzer MA, Ribi K, Schonle E, Boltshauser E (2004) Outcome of craniopharyngioma in children: long-term complications and quality of life. Developmental Medicine and Child Neurology 46: 220-229 | 78 | 97 | 31 | 10.8 | 4 |
| deVeber G, Chan A, Monagle P, Marzinotto V, Armstrong D, Massicotte P, Leaker M, Andrew M (1998) Anticoagulation therapy in pediatric patients with sinovenous thrombosis: a cohort study. Archives of Neurology 55: 1533-1537 | 78 | 97 | 74 | 6.5 | 3 |
| Partington MD, Davis DH, Laws ER, Jr., Scheithauer BW (1994) Pituitary adenomas in childhood and adolescence. Results of transsphenoidal surgery. Journal of Neurosurgery 80: 209-216 | 78 | 97 | 87 | 5.1 | 4 |
| Gobel U, Schneider DT, Calaminus G, Haas RJ, Schmidt P, Harms D (2000) Germ-cell tumors in childhood and adolescence. GPOH MAKEI and the MAHO study groups. Annals of Oncology 11: 263-271 | 81 | 96 | 57 | 7.4 | Review |
| Mathern GW, Giza CC, Yudovin S, Vinters HV, Peacock WJ, Shewmon DA, Shields WD (1999) Postoperative seizure control and antiepileptic drug use in pediatric epilepsy surgery patients: the UCLA experience, 1986–1997. Epilepsia 40: 1740-1749 | 81 | 96 | 65 | 6.9 | 3 |
| Fisher B, Thomas D, Peterson B (1992) Hypertonic saline lowers raised intracranial pressure in children after head trauma. Journal of Neurosurgical Anesthesiology 4: 4-10 | 81 | 96 | 98 | 4.6 | 2 |
| Calaminus G, Bamberg M, Baranzelli MC, Benoit Y, di Montezemolo LC, Fossati-Bellani F, Jurgens H, Kuhl HJ, Lenard HG, Curto ML, et al. (1994) Intracranial germ cell tumors: a comprehensive update of the European data. Neuropediatrics 25: 26-32 | 81 | 96 | 89 | 5.1 | Review |
| Brown CA, Lenke LG, Bridwell KH, Geideman WM, Hasan SA, Blanke K (1998) Complications of pediatric thoracolumbar and lumbar pedicle screws. Spine 23: 1566-1571 | 81 | 96 | 77 | 6.4 | 4 |
| Eleraky MA, Theodore N, Adams M, Rekate HL, Sonntag VK (2000) Pediatric cervical spine injuries: report of 102 cases and review of the literature. Journal of Neurosurgery 92: 12-17 | 81 | 96 | 57 | 7.4 | 4 |
| Fang A, Hu SS, Endres N, Bradford DS (2005) Risk factors for infection after spinal surgery. Spine 30: 1460-1465 | 87 | 95 | 25 | 11.9 | 4 |
| Jaffe KM, Fay GC, Polissar NL, Martin KM, Shurtleff HA, Rivara JM, Winn HR (1993) Severity of pediatric traumatic brain injury and neurobehavioral recovery at one year—a cohort study. Archives of Physical Medicine and Rehabilitation 74: 587-595 | 87 | 95 | 94 | 4.8 | 3 |
| Kaufmann PM, Fletcher JM, Levin HS, Miner ME, Ewing-Cobbs L (1993) Attentional disturbance after pediatric closed head injury. Journal of Child Neurology 8: 348-353 | 89 | 94 | 95 | 4.7 | 3 |
| Gajjar A, Sanford RA, Heideman R, Jenkins JJ, Walter A, Li Y, Langston JW, Muhlbauer M, Boyett JM, Kun LE (1997) Low-grade astrocytoma: a decade of experience at St. Jude Children's Research Hospital. Journal of Clinical Oncology 15: 2792-2799 | 90 | 93 | 79 | 5.8 | 4 |
| Grimwood K, Anderson VA, Bond L, Catroppa C, Hore RL, Kerr EH, Nolan T, Roberton DM (1995) Adverse outcomes of bacterial meningitis in school-age survivors. Pediatrics 95: 646-656 | 90 | 93 | 86 | 5.2 | 3 |
| Hall JR, Reyes HM, Meller JL, Loeff DS, Dembek R (1996) The outcome for children with blunt trauma is best at a pediatric trauma center. Journal of Pediatric Surgery 31: 72-76 | 90 | 93 | 84 | 5.5 | 4 |
| King WJ, MacKay M, Sirnick A, Canadian Shaken Baby Study Group (2003) Shaken baby syndrome in Canada: clinical characteristics and outcomes of hospital cases. Canadian Medical Association Journal 168: 155-159 | 90 | 93 | 36 | 9.3 | 4 |
| Greenes DS, Schutzman SA (1999) Clinical indicators of intracranial injury in head-injured infants. Pediatrics 104: 861-867 | 94 | 92 | 73 | 6.6 | 3 |
| Coffey RJ, Edgar TS, Francisco GE, Graziani V, Meythaler JM, Ridgely PM, Sadiq SA, Turner MS (2002) Abrupt withdrawal from intrathecal baclofen: recognition and management of a potentially life-threatening syndrome. Archives of Physical Medicine and Rehabilitation 83: 735-741 | 95 | 91 | 45 | 8.3 | 4 |
| Grindel SH, Lovell MR, Collins MW (2001) The assessment of sport-related concussion: the evidence behind neuropsychological testing and management. Clinical Journal of Sport Medicine 11: 134-143 | 95 | 91 | 53 | 7.6 | Review |
| Adelson PD, Kochanek PM (1998) Head injury in children. Journal of Child Neurology 13: 2-15 | 97 | 90 | 78 | 6.0 | Review |
| Mohamed A, Wyllie E, Ruggieri P, Kotagal P, Babb T, Hilbig A, Wylie C, Ying Z, Staugaitis S, Najm I, Bulacio J, Foldvary N, Luders H, Bingaman W (2001) Temporal lobe epilepsy due to hippocampal sclerosis in pediatric candidates for epilepsy surgery. Neurology 56: 1643-1649 | 97 | 90 | 54 | 7.5 | 4 |
| Otsubo H, Ochi A, Elliott I, Chuang SH, Rutka JT, Jay V, Aung M, Sobel DF, Snead OC (2001) MEG predicts epileptic zone in lesional extrahippocampal epilepsy: 12 pediatric surgery cases. Epilepsia 42: 1523-1530 | 97 | 90 | 54 | 7.5 | 4 |
| Sharpies PM, Stuart AG, Matthews DS, Aynsley-Green A, Eyre JA (1995) Cerebral blood flow and metabolism in children with severe head injury. Part 1: relation to age, Glasgow coma score, outcome, intracranial pressure, and time after injury. Journal of Neurology, Neurosurgery, and Psychiatry 58: 145-152 | 97 | 90 | 90 | 5.0 | 4 |
Table 3.
List of top 50 most cited journal articles in pediatric neurosurgery from the years 2002–2012
| Article | Rank | Citations | Adjusted rank | Adjusted citations | Class |
|---|---|---|---|---|---|
| Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE (2004) Late neurocognitive sequelae in survivors of brain tumours in childhood. The Lancet Oncology 5: 399-408 | 1 | 245 | 2 | 27.2 | Review |
| Hutchison JS, Ward RE, Lacroix J, Hebert PC, Barnes MA, Bohn DJ, Dirks PB, Doucette S, Fergusson D, Gottesman R, Joffe AR, Kirpalani HM, Meyer PG, Morris KP, Moher D, Singh RN, Skippen PW, Hypothermia Pediatric Head Injury Trial Investigators and the Canadian Critical Care Trials Group (2008) Hypothermia therapy after traumatic brain injury in children. The New England Journal of Medicine 358: 2447-2456 | 2 | 175 | 1 | 35.0 | 2 |
| Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N (2002) A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology 16: 15-27 | 3 | 174 | 12 | 15.8 | 3 |
| Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH (2003) A population-based study of inflicted traumatic brain injury in young children. JAMA 290: 621-626 | 4 | 164 | 9 | 16.4 | 4 |
| Sebire G, Tabarki B, Saunders DE, Leroy I, Liesner R, Saint-Martin C, Husson B, Williams AN, Wade A, Kirkham FJ (2005) Cerebral venous sinus thrombosis in children: risk factors, presentation, diagnosis and outcome. Brain 128: 477-489 | 5 | 160 | 4 | 20.0 | 4 |
| Scott RM, Smith JL, Robertson RL, Madsen JR, Soriano SG, Rockoff MA (2004) Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. Journal of Neurosurgery 100: 142-149 | 6 | 143 | 10 | 15.9 | 4 |
| Van Effenterre R, Boch AL (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. Journal of Neurosurgery 97: 3-11 | 7 | 140 | 20 | 12.7 | 4 |
| Karavitaki N, Brufani C, Warner JT, Adams CB, Richards P, Ansorge O, Shine B, Turner HE, Wass JA (2005) Craniopharyngiomas in children and adults: systematic analysis of121 cases with long-term follow-up. Clinical Endocrinology 62: 397-409 | 8 | 139 | 6 | 17.4 | 4 |
| Tong KA, Ashwal S, Holshouser BA, Nickerson JP, Wall CJ, Shutter LA, Osterdock RJ, Haacke EM, Kido D (2004) Diffuse axonal injury in children: clinical correlation with hemorrhagic lesions. Annals of Neurology 56: 36-50 | 9 | 136 | 13 | 15.1 | 2 |
| Merchant TE, Mulhern RK, Krasin MJ, Kun LE, Williams T, Li C, Xiong X, Khan RB, Lustig RH, Boop FA, Sanford RA (2004) Preliminary results from a phase II trial of conformal radiation therapy and evaluation of radiation-related CNS effects for pediatric patients with localized ependymoma. Journal of Clinical Oncology 22: 3156-3162 | 10 | 131 | 14 | 14.6 | 3 |
| Kazak AE, Alderfer M, Rourke MT, Simms S, Streisand R, Grossman JR (2004) Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. Journal of Pediatric Psychology 29: 211-219 | 10 | 131 | 14 | 14.6 | 4 |
| Kuroda S, Houkin K (2008) Moyamoya disease: current concepts and future perspectives. Lancet Neurology 7: 1056-1066 | 12 | 130 | 3 | 26.0 | Review |
| Adelson PD, Ragheb J, Kanev P, Brockmeyer D, Beers SR, Brown SD, Cassidy LD, Chang Y, Levin H (2005) Phase II clinical trial of moderate hypothermia after severe traumatic brain injury in children. Neurosurgery 56: 740-754 | 13 | 127 | 10 | 15.9 | 2 |
| Hargrave D, Bartels U, Bouffet E (2006) Diffuse brainstem glioma in children: critical review of clinical trials. The Lancet Oncology 7: 241-248 | 14 | 126 | 5 | 18.0 | Review |
| Tubbs RS, McGirt MJ, Oakes WJ (2003) Surgical experience in 130 pediatric patients with Chiari I malformations. Journal of Neurosurgery 99: 291-296 | 15 | 122 | 22 | 12.2 | 4 |
| Ommaya AK, Goldsmith W, Thibault L (2002) Biomechanics and neuropathology of adult and paediatric head injury. British Journal of Neurosurgery 16: 220-242 | 16 | 119 | 28 | 10.8 | Review |
| Yeates KO, Swift E, Taylor HG, Wade SL, Drotar D, Stancin T, Minich N (2004) Short- and long-term social outcomes following pediatric traumatic brain injury. Journal of the International Neuropsychological Society 10: 412-426 | 17 | 115 | 18 | 12.8 | 3 |
| Lustig RH, Post SR, Srivannaboon K, Rose SR, Danish RK, Burghen GA, Xiong X, Wu S, Merchant TE (2003) Risk factors for the development of obesity in children surviving brain tumors. The Journal of Clinical Endocrinology and Metabolism 88: 611-616 | 18 | 110 | 26 | 11.0 | 4 |
| Albanese A, Barnes MP, Bhatia KP, Fernandez-Alvarez E, Filippini G, Gasser T, Krauss JK, Newton A, Rektor I, Savoiardo M, Valls-Sole J (2006) A systematic review on the diagnosis and treatment of primary (idiopathic) dystonia and dystonia plus syndromes: report of an EFNS/MDS-ES Task Force. European Journal of Neurology 13: 433-444 | 19 | 101 | 16 | 14.4 | 4 |
| Poretti A, Grotzer MA, Ribi K, Schonle E, Boltshauser E (2004) Outcome of craniopharyngioma in children: long-term complications and quality of life. Developmental Medicine and Child Neurology 46: 220-229 | 20 | 97 | 28 | 10.8 | 3 |
| Fang A, Hu SS, Endres N, Bradford DS (2005) Risk factors for infection after spinal surgery. Spine 30: 1460-1465 | 21 | 95 | 23 | 11.9 | 4 |
| King WJ, MacKay M, Sirnick A, Canadian Shaken Baby Study Group (2003) Shaken baby syndrome in Canada: clinical characteristics and outcomes of hospital cases. Canadian Medical Association Journal 168: 155-159 | 22 | 93 | 36 | 9.3 | 4 |
| Greenes DS, Schutzman SA (1999) Clinical indicators of intracranial injury in head-injured infants. Pediatrics 104: 861-867 | 23 | 92 | 49 | 6.6 | 3 |
| Coffey RJ, Edgar TS, Francisco GE, Graziani V, Meythaler JM, Ridgely PM, Sadiq SA, Turner MS (2002) Abrupt withdrawal from intrathecal baclofen: recognition and management of a potentially life-threatening syndrome. Archives of Physical Medicine and Rehabilitation 83: 735-741 | 24 | 91 | 43 | 8.3 | Review |
| Jonas R, Nguyen S, Hu B, Asarnow RF, LoPresti C, Curtiss S, de Bode S, Yudovin S, Shields WD, Vinters HV, Mathern GW (2004) Cerebral hemispherectomy: hospital course, seizure, developmental, language, and motor outcomes. Neurology 62: 1712-1721 | 24 | 91 | 32 | 10.1 | 3 |
| Kirkwood MW, Yeates KO, Wilson PE (2006) Pediatric sport-related concussion: a review of the clinical management of an oft-neglected population. Pediatrics 117: 1359-1371 | 26 | 87 | 21 | 12.4 | 4 |
| Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T (2003) Long-term behavior problems following pediatric traumatic brain injury: prevalence, predictors, and correlates. Journal of Pediatric Psychology 28: 251-263 | 27 | 86 | 39 | 8.6 | 3 |
| Carli M, Ferrari A, Mattke A, Zanetti I, Casanova M, Bisogno G, Cecchetto G, Alaggio R, De Sio L, Koscielniak E, Sotti G, Treuner J (2005) Pediatric malignant peripheral nerve sheath tumor: the Italian and German soft tissue sarcoma cooperative group. Journal of Clinical Oncology 23: 8422-8430 | 28 | 83 | 31 | 10.4 | 3 |
| Puget S, Garnett M, Wray A, Grill J, Habrand JL, Bodaert N, Zerah M, Bezerra M, Renier D, Pierre-Kahn A, Sainte-Rose C (2007) Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. Journal of Neurosurgery 106: 3-12 | 28 | 83 | 17 | 13.8 | 4 |
| Palchak MJ, Holmes JF, Vance CW, Gelber RE, Schauer BA, Harrison MJ, Willis-Shore J, Wootton-Gorges SL, Derlet RW, Kuppermann N (2003) A decision rule for identifying children at low risk for brain injuries after blunt head trauma. Annals of Emergency Medicine 42: 492-506 | 30 | 81 | 45 | 8.1 | 3 |
| Cohen-Gadol AA, Ozduman K, Bronen RA, Kim JH, Spencer DD (2004) Long-term outcome after epilepsy surgery for focal cortical dysplasia. Journal of Neurosurgery 101: 55-65 | 30 | 81 | 37 | 9.0 | 4 |
| Kestle JR, Drake JM, Cochrane DD, Milner R, Walker ML, Abbott R, 3rd, Boop FA, Endoscopic Shunt Insertion Trial participants (2003) Lack of benefit of endoscopic ventriculoperitoneal shunt insertion: a multicenter randomized trial. Journal of Neurosurgery 98: 284-290 | 30 | 81 | 45 | 8.1 | 2 |
| Geddes JF, Tasker RC, Hackshaw AK, Nickols CD, Adams GG, Whitwell HL, Scheimberg I (2003) Dural haemorrhage in non-traumatic infant deaths: does it explain the bleeding in ‘shaken baby syndrome’? Neuropathology and Applied Neurobiology 29: 14-22 | 33 | 80 | 48 | 8.0 | 4 |
| Fletcher JM, Copeland K, Frederick JA, Blaser SE, Kramer LA, Northrup H, Hannay HJ, Brandt ME, Francis DJ, Villarreal G, Drake JM, Laurent JP, Townsend I, Inwood S, Boudousquie A, Dennis M (2005) Spinal lesion level in spina bifida: a source of neural and cognitive heterogeneity. Journal of Neurosurgery 102: 268-279 | 34 | 78 | 34 | 9.8 | 3 |
| Robertson PL, Muraszko KM, Holmes EJ, Sposto R, Packer RJ, Gajjar A, Dias MS, Allen JC, Children's Oncology Group (2006) Incidence and severity of postoperative cerebellar mutism syndrome in children with medulloblastoma: a prospective study by the Children's Oncology Group. Journal of Neurosurgery 105: 444-451 | 35 | 77 | 26 | 11.0 | 4 |
| Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF (2004) A population-based comparison of clinical and outcome characteristics of young children with serious inflicted and noninflicted traumatic brain injury. Pediatrics 114: 633-639 | 35 | 77 | 39 | 8.6 | 4 |
| Schwartz DM, Auerbach JD, Dormans JP, Flynn J, Drummond DS, Bowe JA, Laufer S, Shah SA, Bowen JR, Pizzutillo PD, Jones KJ, Drummond DS (2007) Neurophysiological detection of impending spinal cord injury during scoliosis surgery. The Journal of Bone and Joint Surgery (American Volume) 89: 2440-2449 | 35 | 77 | 18 | 12.8 | 4 |
| Moore BD, 3rd (2005) Neurocognitive outcomes in survivors of childhood cancer. Journal of Pediatric Psychology 30: 51-63 | 38 | 76 | 35 | 9.5 | Review |
| Broniscer A, Gajjar A (2004) Supratentorial high-grade astrocytoma and diffuse brainstem glioma: two challenges for the pediatric oncologist. The Oncologist 9: 197-206 | 38 | 76 | 42 | 8.4 | Review |
| Cross JH, Jayakar P, Nordli D, Delalande O, Duchowny M, Wieser HG, Guerrini R, Mathern GW, International League against Epilepsy, Subcommission for Paediatric Epilepsy Surgery, Commissions of Neurosurgery and Paediatrics (2006) Proposed criteria for referral and evaluation of children for epilepsy surgery: recommendations of the Subcommission for Pediatric Epilepsy Surgery. Epilepsia 47: 952-959 | 40 | 75 | 30 | 10.7 | Other |
| Cirak B, Ziegfeld S, Knight VM, Chang D, Avellino AM, Paidas CN (2004) Spinal injuries in children. Journal of Pediatric Surgery 39: 607-612 | 41 | 74 | 44 | 8.2 | 4 |
| Ewing-Cobbs L, Barnes M, Fletcher JM, Levin HS, Swank PR, Song J (2004) Modeling of longitudinal academic achievement scores after pediatric traumatic brain injury. Developmental Neuropsychology 25: 107-133 | 42 | 73 | 45 | 8.1 | 3 |
| Wyllie E, Lachhwani DK, Gupta A, Chirla A, Cosmo G, Worley S, Kotagal P, Ruggieri P, Bingaman WE (2007) Successful surgery for epilepsy due to early brain lesions despite generalized EEG findings. Neurology 69: 389-397 | 43 | 71 | 24 | 11.8 | 4 |
| Starr PA, Turner RS, Rau G, Lindsey N, Heath S, Volz M, Ostrem JL, Marks WJ, Jr. (2006) Microelectrode-guided implantation of deep brain stimulators into the globus pallidus internus for dystonia: techniques, electrode locations, and outcomes. Journal of Neurosurgery 104: 488-501 | 43 | 71 | 32 | 10.1 | 3 |
| Freitag H, Tuxhorn I (2005) Cognitive function in preschool children after epilepsy surgery: rationale for early intervention. Epilepsia 46: 561-567 | 45 | 70 | 38 | 8.8 | 3 |
| Merchant TE, Li C, Xiong X, Kun LE, Boop FA, Sanford RA (2009) Conformal radiotherapy after surgery for paediatric ependymoma: a prospective study. The Lancet Oncology 10: 258-266 | 46 | 69 | 7 | 17.3 | 3 |
| Lerner JT, Salamon N, Hauptman JS, Velasco TR, Hemb M, Wu JY, Sankar R, Donald Shields W, Engel J, Jr., Fried I, Cepeda C, Andre VM, Levine MS, Miyata H, Yong WH, Vinters HV, Mathern GW (2009) Assessment and surgical outcomes for mild type I and severe type II cortical dysplasia: a critical review and the UCLA experience. Epilepsia 50: 1310-1335 | 46 | 69 | 7 | 17.3 | Review |
| Grundy RG, Wilne SA, Weston CL, Robinson K, Lashford LS, Ironside J, Cox T, Chong WK, Campbell RH, Bailey CC, Gattamaneni R, Picton S, Thorpe N, Mallucci C, English MW, Punt JA, Walker DA, Ellison DW, Machin D, Children's Cancer and Leukaemia Group Brain Tumour Committee (2007) Primary postoperative chemotherapy without radiotherapy for intracranial ependymoma in children: the UKCCSG/SIOP prospective study. The Lancet Oncology 8: 696-705 | 48 | 68 | 25 | 11.3 | 3 |
| McNeil DE, Cote TR, Clegg L, Rorke LB (2002) Incidence and trends in pediatric malignancies medulloblastoma/primitive neuroectodermal tumor: a SEER update. Surveillance Epidemiology and End Results. Medical and Pediatric Oncology 39: 190-194 | 48 | 68 | 50 | 6.2 | Other |
| Warf BC (2005) Hydrocephalus in Uganda: the predominance of infectious origin and primary management with endoscopic third ventriculostomy. Journal of Neurosurgery 102: 1-15 | 48 | 68 | 41 | 8.5 | 4 |
Top 100 articles
Demographics
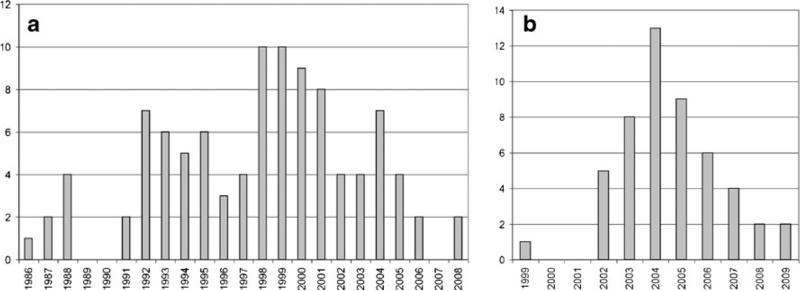
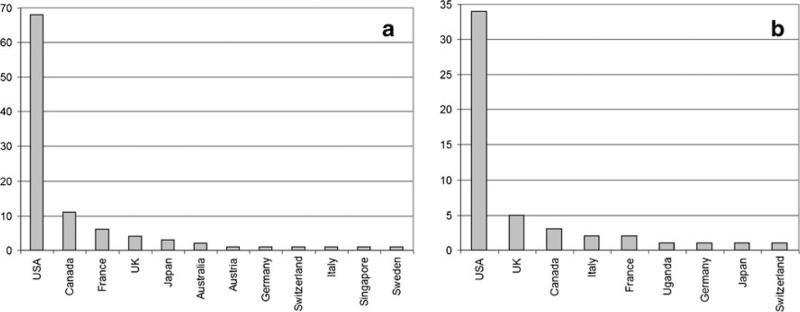
Forty-four journals provided all the articles in the top 100 list: Journal of Neurosurgery (20 articles), Neurosurgery (eight articles), and Journal of Clinical Oncology (six articles) contained the most articles in the top 100. Articles were published from 1986 to 2008, with the most productive years being 1998 and 1999 (n =10 each) (Fig. 1a). The number of authors ranged from 2 to 38 with a mean, median, and mode of 7, 6, and 5, respectively. The country of origin for the first author was most frequently the USA (n =68), followed by Canada (n =11) and France (n =6) (Fig. 2a).
Fig. 1.
Articles per year for a the top 100 list and b the top 50 list
Fig. 2.
Article counts by country of origin for a the top 100 list and b the top 50 list
Topic of research, study design, and level of evidence
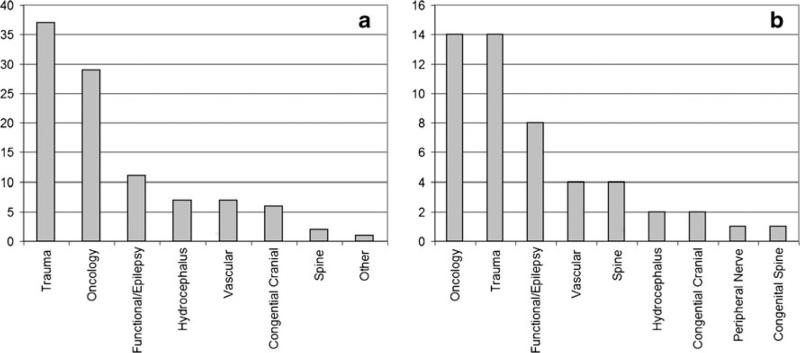
The most popular topic was trauma (n =37), followed by oncology (n =29) and then functional/epilepsy (n =11) (Fig. 3a). Based on the OCEBM 2011 Levels of Evidence Classification System, two articles were classified as grade 1, nine articles were classified as grade 2, 26 articles were classified as grade 3, and 52 articles were classified as grade 4. There were nine review articles and two articles that were categorized as “other”: a description of vagal nerve stimulation (#8) and an analysis of fluid dynamics in Chiari malformations (#70).
Fig. 3.
Article counts by topic for a the top 100 list and b the top 50 list
Citation analysis
The top 100 overall most cited articles were referenced an average of 131±49 times (median 118, range 90–321). Two papers had greater than 300 citations, five had greater than 200, 11 had 151–200, and 54 had 100–150. The average adjusted citation count was 9.8±5.5 (median 8, range 4.3–35). When comparing the adjusted ranking to the overall, the change in position ranged from −58 to +62, with a mean absolute rank change of 21±17. Of the 18 papers with greater than 150 citations, 14 (78 %) had an adjusted citation count greater than 10. The original contribution papers with the highest combined score (i.e., total citation count × adjusted citation count) were by Levisohn et al. (rank #2), published in 2000, on the neuropsychological consequences of cerebellar tumor resection (score=7,191) and Zeltzer et al., published in 1999, on prognostic factors in children with medulloblastoma (rank #3, score=6,174).
Top 50 articles in the last decade (2002–2012)
Demographics
Thirty-one journals provided all the articles in the top 50 list. Journal of Neurosurgery (ten articles) and Lancet Oncology (four articles) contained the most articles in the top 50. The largest number of articles (n =13) was published in 2004 (Fig. 1b). The number of authors ranged from 1 to 19, with a mean, median, and mode of 7, 6, and 6, respectively. The country of origin of the first author was most frequently the USA (n =34), followed by UK (n =5) and Canada (n =3) (Fig. 2b).
Topic of research, study design, and level of evidence
Oncology (n =14), trauma (n =14), and functional/epilepsy-related research (n =8) were the most common topics (Fig. 3b). There were four articles classified as grade 2, 15 articles classified as grade 3, and 21 articles classified as grade 4 papers (OCEM levels of evidence). There were eight review articles and two “other” articles: a study on criteria and guidelines used to evaluate children for epilepsy surgery (#40) and an epidemiological update on medulloblastoma/PNET tumors (#48).
Citation analysis
The top 50 articles over the last decade were cited an average of 103±37 times (median 89, range 68–245). One paper had greater than 200 citations, four papers had 151–200 citations, and 14 papers had 100–150 citations. The average adjusted citation count was 13±5.5 (median 11, range 6.2–35). When comparing the adjusted ranking to the overall, the change in position ranged from −26 to +39, with a mean absolute rank change of 9±9. Of the 19 papers with greater than 100 citations, 11 (58 %) had an adjusted citation count of greater than 15. The original contribution papers with the highest combined score (total citation count × adjusted citation count) were by Hutchison et al. (rank #2), published in 2008, on hypothermia and traumatic brain injury (score=6,125) and by Sebire et al., published in 2005, on cerebral venous sinus thrombosis (rank #5, score=3,200).
Discussion
Citation analysis is a useful method of quantifying the impact an article has made upon a scientific community. Although correlating an original contribution paper with a high citation count as being of high “quality” is, in general, a reasonable conclusion, we rather view citations as an indicator of “interest” generated by that article within academia. The question of “quality” is one that is answered with the passage of time and comes from the collective voice from members within the scientific community.
Our results
In this study, we found an average citation count of 131±49 (median 118, range 90–321) in the top 100 overall and 103±37 times (median 89, range 68–245) in the top 50 over the last decade. In comparison to our previous study which included only pediatric neurosurgery journals, the average citation count was 90±26 (median 81, range 65–193) in the top 100 overall and 54±15 (median 49, range 41–125) in the top 50 over the last decade [26]. There are several reasons for this. The first is that pediatric neurosurgery is a young and very small field compared to others. Publication of pediatric neurosurgery journals began no more than 50 years ago, the readership is small, and consequently the impact factors (IF) of the journals are low: Childs Nervous System (1.24), Pediatric Neurosurgery (0.42), and Journal of Neurosurgery: Pediatrics (1.62). The second reason is that many of the articles that we found in this current study were authored by non-neurosurgeons (e.g., medical oncologists, radiation oncologists, intensivists, or a mixture) and, therefore, appeal to physicians of various subspecialties. The journals they chose to publish in have a much wider audience and higher IFs than pediatric neurosurgery journals. For example, the IF for Lancet Oncology, Journal of Clinical Oncology, Brain, and Critical Care is 25.20, 18.04, 9.92, and 4.72, respectively. Nonetheless, many of the articles in our two lists were published in neurosurgery journals: 30 in the top 100 list and 12 in the top 50 list. This marked difference in journal impact factors demonstrates the need to be responsible when performing citation analysis. Much in the same way as it is inappropriate to compare the bibliometric profiles of different researchers (e.g., pediatric neurosurgeons vs. medical oncologists vs. basic science researchers), it is also incorrect to compare the citation history of papers published in journals with different target audiences (highly specialized compared to multidisciplinary journals) [28].
In 2004, the Journal of Neurosurgery–Pediatrics was created as a sister journal to the Journal of Neurosurgery. Many of the Journal of Neurosurgery articles in the top 100 and top 50 lists in this paper would likely be published in Journal of Neurosurgery–Pediatrics today. By comparison, Neurosurgery has not subdivided into subsidiary sister journals. In our top 100 list for this current study, there were eight articles published in Neurosurgery, with an average citation count of 158 (range, 100–282), much higher than the average citation count of 90 for the top 100 list of only pediatric neurosurgery journals. Also, there were no Journal of Neurosurgery–Pediatrics articles in the previous top 100 list and only one in the top 50 list. These findings would suggest that there was a loss of readership when the Journal of Neurosurgery–Pediatrics was created.
The topics that appeared most frequently in the top articles in dedicated pediatric neurosurgical journals were hydrocephalus and oncology. By comparison, oncology and trauma were the most common topics in this study. This is an expected finding. Hydrocephalus is a disease that is treated almost exclusively by neurosurgeons, unlike other multidisciplinary areas such as trauma and oncology. The levels of evidence based on the OCEBM guidelines were generally higher in this study as compared to our first study. Thirty-seven papers were levels 1, 2, or 3 compared with only 12 in our first study. One major reason for this is that the competition to get a paper accepted in a high-impact journal is intense, forcing authors to increase the quality of their submission.
Limitations
Specific search terms were used to delineate articles related to pediatrics and neurosurgery. These terms are subject to variations in terminology and spelling, for example, “AVM,” “arterio-venous malformation,” and “AV-malformation.” Our study accounted for these types of instances by including similar terms as we saw appropriate; however, the subjective nature of the search criteria likely did not capture some articles due to this reason. We excluded articles related to basic science, histology, radiology, and pharmaceutical sciences. The process of excluding articles is inherently subjective and was done by consensus. There is no doubt that some of the excluded articles, while not directly related to clinical pediatric neurosurgery, have influenced the practice of pediatric neurosurgery. A notable example would be the growing literature on the molecular profiling of pediatric brain tumors [29–31].
Conclusion
The top 100 overall articles in pediatric neurosurgery from non-pediatric neurosurgical journals and the top 50 most cited articles over the last decade are presented in this paper. The number of citations for these lists of articles is on average higher than articles from pediatric neurosurgery journals due to the fact that many of these articles are intended for a broader audience and are published in journals with higher impact factors. Furthermore, there is some evidence to suggest that pediatric-specific articles may have lost some exposure within the academic community when placed into pediatric-specific journals compared to when they were kept in general neurosurgical journals. The responsible use of citation analysis should involve comparing journals with similar intended audiences. Caution should be used when equating “quality” with citation volume.
Acknowledgments
The authors wish to thank Andrew J. Gienapp for technical and copy editing, preparation of the manuscript, and publication assistance with this manuscript.
Appendix
Table 4.
The 2011 Oxford Centre for Evidence-Based Medicine Levels of Evidence [27]
| Question | Level 1a | Level 2a | Level 3a | Level 4a | Level 5 |
|---|---|---|---|---|---|
| How common is the problem? | Local and current random sample surveys (or censuses) | Systematic review of surveys that allow matching to local circumstancesb | Local non-random sampleb | Case seriesb | n/a |
| Is this diagnostic or monitoring test accurate? (diagnosis) | Systematic review of cross sectional studies with consistently applied reference standard and blinding | Individual cross sectional studies with consistently applied reference standard and blinding | Non-consecutive studies or studies without consistently applied reference standardsb | Case–control studies or “poor or non-independent reference standard”b | Mechanism-based reasoning |
| What will happen if we do not add a therapy? (prognosis) | Systematic review of inception cohort studies | Inception cohort studies | Cohort study or control arm of randomized triala | Case series or case–control studies or poor-quality prognostic cohort studyb | n/a |
| Does this intervention help? (treatment benefits) | Systematic review of randomized trials or n-of-1 trials | Randomized trial or observational study with dramatic effect | Non-randomized controlled cohort/follow-up studyb | Case series, case–control studies, or historically controlled studiesb | Mechanism-based reasoning |
| What are the COMMON harms? (treatment harms) | Systematic review of randomized trials, systematic review of nested case–control studies, n-of-1 trial with the patient you are raising the question about, or observational study with dramatic effect | Individual randomized trial or (exceptionally) observational study with dramatic effect | Non-randomized controlled cohort/follow-up study (post-marketing surveillance) provided there are sufficient numbers to rule out a common harm (for long-term harms, the duration of follow-up must be sufficient)b | Case series, case–control, or historically controlled studiesb | Mechanism-based reasoning |
| What are the rare harms? (treatment harms) | Systematic review of randomized trials or n-of-1 trial | Randomized trial or (exceptionally) observational study with dramatic effect | |||
| Is this (early detection) test worthwhile? (screening) | Systematic review of randomized trials | Randomized trial | Non-randomized controlled cohort/follow-up studyb | Case series, case–control, or historically controlled studiesb | Mechanism-based reasoning |
Level may be graded down on the basis of study quality, imprecision, and indirectness (study PICO does not match questions PICO) because of inconsistency between studies or because the absolute effect size is very small. Level may be graded up if there is a large or very large effect size
As always, a systematic review is generally better than an individual study
Contributor Information
Nickalus R. Khan, Department of Neurosurgery, University of Tennessee Health Science Center, Memphis, TN, USA
Tyler Auschwitz, Department of Neurosurgery, University of Tennessee Health Science Center, Memphis, TN, USA.
Joseph H. McAbee, School of Medicine, Wake Forest University, Winston-Salem, NC, USA
Frederick A. Boop, Department of Neurosurgery, University of Tennessee Health Science Center, Memphis, TN, USA Le Bonheur Neuroscience Institute, Le Bonheur Children's Hospital, 50 N. Dunlap Street, Memphis, TN 38103, USA; Semmes-Murphey Neurologic and Spine Institute, Memphis, TN, USA.
Paul Klimo, Jr, Department of Neurosurgery, University of Tennessee Health Science Center, Memphis, TN, USA; Le Bonheur Neuroscience Institute, Le Bonheur Children's Hospital, 50 N. Dunlap Street, Memphis, TN 38103, USA; Semmes-Murphey Neurologic and Spine Institute, Memphis, TN, USA.
References
- 1.Lu Z. PubMed and beyond: a survey of web tools for searching biomedical literature. Database (Oxford) 2011;2011:baq036. doi: 10.1093/database/baq036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sayers EW, Barrett T, Benson DA, Bolton E, Bryant SH, Canese K, Chetvernin V, Church DM, DiCuccio M, Federhen S, Feolo M, Fingerman IM, Geer LY, Helmberg W, Kapustin Y, Landsman D, Lipman DJ, Lu Z, Madden TL, Madej T, Maglott DR, Marchler-Bauer A, Miller V, Mizrachi I, Ostell J, Panchenko A, Phan L, Pruitt KD, Schuler GD, Sequeira E, Sherry ST, Shumway M, Sirotkin K, Slotta D, Souvorov A, Starchenko G, Tatusova TA, Wagner L, Wang Y, Wilbur WJ, Yaschenko E, Ye J. Database resources of the national center for biotechnology information. Nucleic Acids Res. 2011;39:D38–D51. doi: 10.1093/nar/gkq1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jinha AE. Article 50 million: an estimate of the number of scholarly articles in existence. Learned Publ. 2010;23:258–263. [Google Scholar]
- 4.Bakkalbasi N, Bauer K, Glover J, Wang L. Three options for citation tracking: google scholar, scopus and web of science. Biomed Digit Libr. 2006;3:7. doi: 10.1186/1742-5581-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harzing A-W. The publish or perish book: Your guide to effective and responsible citation analysis. Tarma Software Research Pty Ltd; Melbourne: 2011. [Google Scholar]
- 6.Harzing A-W, Wal R. Google Scholar as a new source for citation analysis? Ethics Sci Environ Polit. 2008;8:62–71. [Google Scholar]
- 7.Vaughan L, Shaw D. A new look at evidence of scholarly citations in citation indexes and from web sources. Scientometrics. 2008;74:317–330. [Google Scholar]
- 8.Plikus MV, Zhang Z, Chuong C-M. PubFocus: semantic MEDLINE/PubMed citations analytics through integration of controlled biomedical dictionaries and ranking algorithm. BMC Bioinforma. 2006;7:424–439. doi: 10.1186/1471-2105-7-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tripathi RS, Blum JM, Papadimos TJ, Rosenberg AL. A bibliometric search of citation classics in anesthesiology. BMC Anesthesiol. 2011;11:24. doi: 10.1186/1471-2253-11-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenberg AL, Tripathi RS, Blum J. The most influential articles in critical care medicine. J Crit Care. 2010;25:157–170. doi: 10.1016/j.jcrc.2008.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dubin D, Hafner AW, Arndt KA. Citation classics in clinical dermatologic journals. Citation analysis, biomedical journals, and landmark articles, 1945–1990. Arch Dermatol. 1993;129:1121–1129. [PubMed] [Google Scholar]
- 12.Tsai YL, Lee CC, Chen SC, Yen ZS. Top-cited articles in emergency medicine. Am J Emerg Med. 2006;24:647–654. doi: 10.1016/j.ajem.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Jones AW. Creme de la creme in forensic science and legal medicine. The most highly cited articles, authors and journals 1981–2003. Int J Legal Med. 2005;119:59–65. doi: 10.1007/s00414-004-0512-x. [DOI] [PubMed] [Google Scholar]
- 14.Jones AW. Impact of JAT publications 1981–2003: the most prolific authors and the most highly cited articles. J Anal Toxicol. 2004;28:541–545. doi: 10.1093/jat/28.7.541. [DOI] [PubMed] [Google Scholar]
- 15.Jones AW. Which articles and which topics in the forensic sciences are most highly cited? Sci Justice. 2005;45:175–182. doi: 10.1016/S1355-0306(05)71661-0. [DOI] [PubMed] [Google Scholar]
- 16.Ohba N, Nakao K, Isashiki Y, Ohba A. The 100 most frequently cited articles in ophthalmology journals. Arch Ophthalmol. 2007;125:952–960. doi: 10.1001/archopht.125.7.952. [DOI] [PubMed] [Google Scholar]
- 17.Lefaivre KA, Shadgan B, O'Brien PJ. 100 most cited articles in orthopaedic surgery. Clin Orthop Relat Res. 2011;469:1487–1497. doi: 10.1007/s11999-010-1604-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fenton JE, Roy D, Hughes JP, Jones AS. A century of citation classics in otolaryngology–head and neck surgery journals. J Laryngol Otol. 2002;116:494–498. doi: 10.1258/002221502760132557. [DOI] [PubMed] [Google Scholar]
- 19.Baldwin KD, Kovatch K, Namdari S, Sankar W, Flynn JM, Dormans JP. The 50 most cited articles in pediatric orthopedic surgery. J Pediatr Orthop B. 2012;21:463–468. doi: 10.1097/BPB.0b013e328354b0cf. [DOI] [PubMed] [Google Scholar]
- 20.Zhang WJ, Li YF, Zhang JL, Xu M, Yan RL, Jiang H. Classic citations in main plastic and reconstructive surgery journals. Ann Plast Surg. 2012;71:103–108. doi: 10.1097/SAP.0b013e31824189ba. [DOI] [PubMed] [Google Scholar]
- 21.Loonen MP, Hage JJ, Kon M. Plastic surgery classics: characteristics of 50 top-cited articles in four plastic surgery journals since 1946. Plast Reconstr Surg. 2008;121:320e–327. doi: 10.1097/PRS.0b013e31816b13a9. [DOI] [PubMed] [Google Scholar]
- 22.Thomas K, Moore CM, Gerharz EW, O'Brien T, Emberton M. Classic papers in urology. Eur Urol. 2003;43:591–595. doi: 10.1016/s0302-2838(03)00143-x. [DOI] [PubMed] [Google Scholar]
- 23.Heldwein FL, Rhoden EL, Morgentaler A. Classics of urology: a half century history of the most frequently cited articles (1955–2009). Urology. 2010;75:1261–1268. doi: 10.1016/j.urology.2009.09.043. [DOI] [PubMed] [Google Scholar]
- 24.Ponce FA, Lozano AM. Highly cited works in neurosurgery. Part I: the 100 top-cited papers in neurosurgical journals. J Neurosurg. 2010;112:223–232. doi: 10.3171/2009.12.JNS091599. [DOI] [PubMed] [Google Scholar]
- 25.Ponce FA, Lozano AM. Highly cited works in neuro-surgery. Part II: the citation classics. J Neurosurg. 2010;112:233–246. doi: 10.3171/2009.12.JNS091600. [DOI] [PubMed] [Google Scholar]
- 26.Wilcox MA, Khan NR, McAbee JH, Boop FA, Klimo P., Jr Highly cited publications in pediatric neurosurgery. Childs Nerv Syst. 2013 doi: 10.1007/s00381-013-2228-z. doi:10.1007/s00381-013-2228-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.OCEBM Levels of Evidence Working Group = Jeremy Howick ICJLL. Glasziou Paul, Greenhalgh Trish, Heneghan Carl, Liberati Alessandro, Moschetti Ivan, Phillips Bob, Thornton Hazel, Goddard Olive, Hodgkinson Mary. OCEBM. 2013 [Google Scholar]
- 28.Bornmann L, Mutz R, Neuhaus C, Daniel H-D. Citation counts for research evaluation: standards of good practice for analyzing bibliometric data and presenting and interpreting results. Ethics Sci Environ Polit. 2008;8:93–102. [Google Scholar]
- 29.Johnson R, Wright KD, Gilbertson RJ. Molecular profiling of pediatric brain tumors: insight into biology and treatment. Curr Oncol Rep. 2009;11:68–72. doi: 10.1007/s11912-009-0011-9. [DOI] [PubMed] [Google Scholar]
- 30.Northcott PA, Korshunov A, Witt H, Hielscher T, Eberhart CG, Mack S, Bouffet E, Clifford SC, Hawkins CE, French P, Rutka JT, Pfister S, Taylor MD. Medulloblastoma comprises four distinct molecular variants. J Clin Oncol. 2011;29:1408–1414. doi: 10.1200/JCO.2009.27.4324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Northcott PA, Shih DJ, Remke M, Cho YJ, Kool M, Hawkins C, Eberhart CG, Dubuc A, Guettouche T, Cardentey Y, Bouffet E, Pomeroy SL, Marra M, Malkin D, Rutka JT, Korshunov A, Pfister S, Taylor MD. Rapid, reliable, and reproducible molecular subgrouping of clinical medulloblastoma samples. Acta Neuropathol. 2012;123:615–626. doi: 10.1007/s00401-011-0899-7. [DOI] [PMC free article] [PubMed] [Google Scholar]