Abstract
Objective
Although a great deal of adolescent smoking research has investigated predictors of initiation, much less has focused on predictors of lapsing during a quit attempt. In particular, the role of social context may deserve greater attention in models of adolescent smoking cessation. Therefore, the present investigation aimed to use ecological momentary assessment (EMA) in order to examine individual differences in social lapsing—the extent to which lapses occur around others vs. when alone.
Methods
Analyses focused on 179 adolescent smokers (aged 14-18) engaged in an unassisted quit attempt. There were two general EMA assessment intervals: pre-quit (1 week) and post-quit (2 weeks). Participants reported every time that they smoked a cigarette and at random, nonsmoking times; in each assessment, participants responded to questions about their current environment, behaviors, and psychological state. A 3-month follow-up assessed longer-term smoking-related outcomes.
Results
Consistent with other adolescent research, the overall rate of lapsing was very high (93%). Social lapsing rates were likewise high (among those who lapsed, 73% reported their first lapse was social), but also varied continuously across individuals. We computed a social lapsing coefficient for each youth, and found that it related to smoking factors at baseline (e.g., lower smoking intensity and dependence) and follow-up (e.g., lower cotinine levels).
Conclusions
These results suggest that higher rates of social lapsing are associated with being a lighter, less dependent smoker and having better eventual cessation prospects. Findings provide evidence that accounting for variability in social lapsing may improve theory and treatment.
Keywords: Smoking Cessation, Adolescents, Ecological Momentary Assessment, Social Lapsing
Introduction
Adolescence is by far the most common period for cigarette smoking initiation to occur. In fact, nearly 90% of adult daily smokers began smoking by the age of 18 (USDHHS, 2012). Investigations into adolescent regular smokers indicate that the majority report a desire to quit smoking and undertake quit attempts (e.g., Bancej et al., 2007; Stanton, Lowe, & Gillespie, 1996; Zhu et al., 1999). Yet while this desire to quit is encouraging, smoking relapse is nearly universal among adolescents: 90-95% of all adolescent quit attempts will fail (Mermelstein, 2003; Killen et al., 2004; Sussman, 2002). Moreover, adolescent smoking relapse is generally quite rapid: Most adolescent relapses occur within the first month of a quit attempt and approximately one third occur within the first week (Bancej et al., 2007; Choi, Ahluwalia, & Nazir, 2002). Given this low success of adolescent smoking cessation, it is important to identify factors early in the quit attempt that may predict relapse.
Models of Adult Smoking Relapse
Numerous studies have characterized the smoking relapse process among adults (Marlatt, Curry, & Gordon, 1988; Shiffman, Hickcox et al., 1996; Shiffman et al., 2006). These works generally describe the process as a series of stages, including: the establishment of initial cessation; lapsing (a smoking event following a period of abstinence); and relapse (a return to the previous pattern of smoking). Within this framework, although lapsing does not necessarily lead to relapse, it is an important part of the relapse process. Indeed, research demonstrates that lapsing (especially the first lapse) is highly predictive of ultimate relapse (Kenford et al., 1994; Shiffman, 2005). Investigations have, accordingly, focused on identifying key risk factors for adult lapsing, and pointed to predictors such as higher tobacco dependence (Shiffman, Waters, & Hickcox, 2004; Sweitzer, Denlinger, & Donny, 2013), higher craving (Bolt et al., 2012; Yeh et al., 2012), indicators of heavier smoking such as salivary cotinine (Powell et al., 2010), low self-efficacy to remain abstinent (Gwaltney et al., 2005), and stress (Slopen et al., 2013).
Beyond individual difference risk factors, substantial evidence also points to the importance of environmental context. For example, lapsing is more likely in the presence of smoking cues (Japuntich et al., 2011; Shiffman, Paty, Gnys, Kassel, & Hickcox, 1996) and when there is a greater proportion of smokers in an individual’s social network (Japuntich et al., 2011). Such risk factors can be incorporated into Person × Environment interaction models (e.g., Niaura et al., 1988; Witkiewitz & Marlatt, 2004), whereby vulnerable individuals are particularly likely to relapse in high-risk situations. A more nuanced version of this perspective additionally posits that certain individuals are particularly vulnerable to certain contexts. One example of this type of specificity is demonstrated by Deiches and colleagues (2013), who used latent class analyses to categorize some adult smokers as “social” lapsers based on their first-lapse behavior. This group (28% of the lapsers) most commonly reported their first lapse as occurring while talking and drinking with friends at a bar or restaurant; compared to other lapsers, they also tended to be younger and to have more smokers in their social networks. Furthermore, compared to those who lapsed when alone (classified as “alone” lapsers), the social lapsers had a higher abstinence rate at the 6-month follow up. Thus, by examining both individual and contextual elements of a lapse, researchers may better understand and treat people who are attempting to quit smoking.
There is no doubt that these advances in theory and research have improved our understanding of smoking relapse among adults. However, the vast majority of studies on smoking relapse have used adult samples, and there are reasons to believe that different processes may underlie cessation and relapse among younger smokers (see Colby & Gwaltney, 2007). Adolescents differ from adults on a number of biological, neurological, psychological, and social dimensions that may cause them to experience smoking cessation and relapse differently than adults (Chambers, Taylor, & Potenza, 2003; Spear, 2000; Somerville, Hare, & Casey, 2011). Additionally, nicotine dependence may not be as well established among adolescents, which could result in a different experience of abstinence and different high-risk contexts. Therefore, rather than extrapolating from adult studies, it is important to directly examine the process of relapse in adolescent populations.
Understanding Adolescent Smoking Cessation
Of the studies examining adolescent smoking cessation, some have identified lapsing predictors that appear to function similarly as among adults. In particular, as with adults, baseline smoking, high craving, and dynamic measures of abstinence self-efficacy have been associated with adolescent smoking lapses (Myers et al., 2011; Van Zundert, Nijhof, & Engels, 2009; Van Zundert, Ferguson, Shiffman, & Engels, 2010). Yet investigations into other potential predictors have also identified differences between adults and adolescents. For example, Van Zundert et al. (2012) reported that nicotine dependence and daily variations in negative affect did not predict time to first lapse or relapse in their adolescent sample.
One component of adult smoking cessation models that remains relatively unexamined for adolescents is the influence of social context on lapsing. This is a significant omission, as the impact of social context can have unique and powerful effects on adolescents. For instance, compared to adults, adolescents are particularly influenced by their social networks (Reifman, Watson, & McCourt, 2006) and are particularly attuned to social evaluation (Somerville, 2013). Furthermore, researchers interested in the early stages of smoking progression have long known that adolescent initiation is strongly associated with social factors (e.g., Chassin et al., 1986); and there is evidence that adolescents are more likely than adults to smoke for social reasons (Ashton & Stepney, 1982; McKennell, 1970). To our knowledge, only one study (Myers et al., 2011) has examined the social context of adolescent lapsing. This study found that 86% of adolescents’ reported lapses were social—a rate that is markedly higher than that reported in adult studies (25% by Shiffman, 1982; 62% by Bliss, Garvey, & Ward, 1999). Such findings suggest that social lapsing may deserve larger emphasis in models of adolescent smoking cessation. However, the Meyers et al. study was also subject to the same methodological limitations as early research on adult smoking: relying on retrospective reporting and, by not using control observations (contexts where the participant is not smoking), failing to identify situations that are uniquely associated with lapsing (Shiffman et al., 1996).
The Current Investigation
This project investigated the understudied topic of adolescent smoking relapse. The various lines of research described above led us to suspect that social context plays an important role in the adolescent lapsing/relapsing process. Therefore, the goal of this project was to examine individual differences among adolescents in the relation between social context and smoking lapses. The study followed 205 youths, aged 14-18, who were interested in quitting smoking. For three weeks, these youths completed multiple assessments each day, both at randomly-prompted times and whenever they smoked a cigarette. Our first hypothesis was that social lapsing would present as a relatively stable, continuous, individual difference. Thus, we expected that social lapsing at one event would predict social lapsing at another event. We also expected that the relation between social context and lapsing would vary continuously across participants, rather than be a binary categorization of “social lapsers” vs. “non-social lapsers” (e.g., Deiches et al., 2012; Myers et al., 2011). By using Ecological Momentary Assessment (EMA) methodology, we were able to calculate a continuous metric for each participant that captured the strength of this relation.
We further examined the relation between our computed measure of social lapsing and (a) baseline factors such as age, dependence, and cessation attitudes and (b) cessation-related outcomes such as days spent quit and smoking intensity, which were assessed three months after the end of EMA monitoring. Our second hypothesis was that individual differences in social lapsing would be uniquely associated with our smoking-related factors of interest. More specifically, given evidence in the adult literature of the relation between social smokers and lower smoking intensity (Moran, Wechsler & Rigotti, 2004; Levy, Biener, & Rigotti, 2009) we suspected that our obtained associations would be negative, such that higher social lapsing would relate to lower indicators of dependence and reduced smoking at follow-up. Exploratory analyses additionally tested the relation between social lapsing and sociocognitive factors (e.g., smoking expectancies).
The primary objective of this project was to assess the social context of smoking during a quit attempt (i.e., lapsing). Yet in order to determine how unique our findings were to the quit attempt, we also examined a baseline period just prior to the quit attempt (when participants were smoking as usual). We expected that a measure of pre-quit social smoking would not be as strongly related to our measures of interest. Such results would suggest that social lapsing is a unique product of the quit attempt and argue against an alternative explanation: that social lapsing is merely a reflection of individuals who smoke more in social situations generally.
Methods
Study Overview and Details on EMA
This study used a short-term longitudinal, observational design, in which adolescent smokers self-reported their experiences for 3 weeks in the context of making an attempt to quit smoking without treatment. The study used EMA methodology, one of the more fruitful techniques found for investigating the complexities of smoking cessation and relapse (see Shiffman, Stone & Hufford, 2008; Shiffman, 2009). EMA refers to the real-time collection of data from people in their natural environments. The typical EMA study uses electronic devices such as PDAs or cell phones, on which participants report about their affective states, behaviors, and environments throughout the day. As a method, it is well suited for examining the episodic processes of substance use and researchers have used it to study topics ranging from withdrawal symptoms among heavy smokers (Baker et al., 2012) to crack-cocaine use among the homeless (Freedman, Lester, McNamara, Milby, & Schumacher, 2006). It also overcomes many of the limitations inherent in traditional survey or interview methods by increasing external validity, reducing recall error, and allowing assessment of control observations (Shiffman et al., 2007).
For the present study, there were two general EMA assessment intervals: pre-quit (1 week) and post-quit (2 weeks). Throughout these time periods, participants made entries on a palm-top computer (Teen Experience Diary, or TED) every time that they smoked a cigarette and at random, nonsmoking times. In each assessment, participants responded to questions about their current environment, behaviors, and psychological state. Quit attempts were defined as when participants selected the “I’m Quit” option on their TED. A 3-month follow-up assessed longer-term smoking-related outcomes.
Participants and Recruitment
Participants were recruited through a variety of methods, including information desks in schools, malls, and other public places, as well as flyers and radio advertisements. When recruitment was conducted at schools, administrators were informed about the nature of the study and that participants would be required to interact with an electronic device during the school day. Adolescents recruited outside of school during non-summer months were required to report that carrying an electronic device was acceptable at their school (all students were provided with a letter describing their participation that could be shown to school teachers and administrators).
To be eligible to participate, adolescents had to be between 14-18 years of age, report smoking at least one cigarette per day in the past 30 days, report smoking 100 or more cigarettes in their lifetime, report a desire to quit smoking within 6 months, and report strong overall confidence in their ability and motivation to quit smoking (combined score from two 0-100 scales ≥ 120). The latter was a requirement to ensure that a high proportion of adolescents would attempt to quit during the study period (see Gwaltney et al., 2005). Participants were also excluded if they were in college, planned to use formal aids for smoking cessation (defined as pharmacotherapy, counseling, or internet websites), or if they reported using other types of tobacco products for six or more days in the past 30 days.
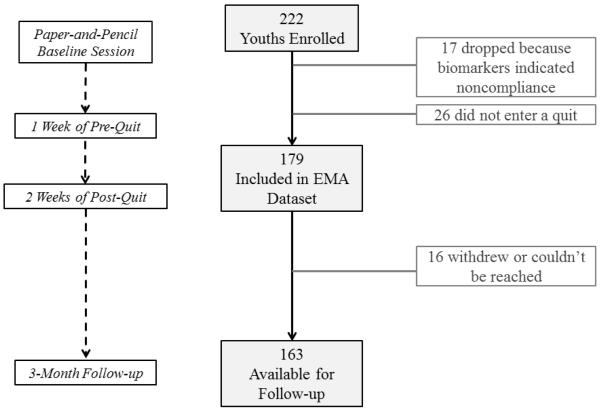
Participants were informed that the general goal of the study was to better understand what happens when adolescents try to quit smoking. Ultimately, we enrolled 222 adolescents; biomarkers (explained in the next section) indicated non-compliance among 17 youths. Another 26 adolescents did not enter a quit during the EMA period (primarily due to low EMA responding), leaving us with a sample of 179 for analysis. The average age of this sample was 16.6 years (SD = 1.2; range 14-18); 64% were male; 82% were non-Hispanic White; 82% were currently attending high school. Sample demographics were comparable to national estimates of adolescent smokers (Johnston, O’Malley, Bachman, Schulenberg, 2014). See Table 1 for descriptive statistics.
Table 1.
Participant characteristics (means or percentages), measured with paper-and-pencil at a baseline session. N = 179.
| Baseline Characteristic | M (SD) or % |
|---|---|
| Demographics | |
| Age | 16.6 (1.2) |
| Gender (male) | 64% |
| Race/Ethnicity (white) | 82% |
| Attending High School | 82% |
| Baseline Reports | |
| Years smoked | 3.5 (1.7) |
| Cigarettes smoked per day (past 30 days) | 10.2 (5.5) |
| Smoking days in the past 30 days | 29.3 (1.9) |
| Dependence (mFTQ Score) | 4.9 (1.6) |
| Attempted to quit in the past year | 74% |
Procedure
All study methods were approved by the Brown University IRB. Data collection occurred from 2007 through 2011. Figure 1 provides an outline of the procedure’s sequence of events and their timeframe. Research staff met with participants on 6 occasions during a 3-week period, convening in the participants’ schools, homes, a community center, or at the study offices. Carbon monoxide (CO) and saliva samples were collected at each visit in order to obtain biomarkers of tobacco exposure (CO and cotinine) and to verify smoking at baseline and claims of abstinence post-quit. At the first (baseline) session, participants were instructed on how to use the TED and staff described the different types of assessments. These assessments included smoking assessments (recorded before every cigarette that participants smoked, even if it was just a puff) and nonsmoking assessments (recorded in response to audible prompts from the TED at random times throughout the day). Participants were instructed to turn off (“suspend”) the TED from audibly prompting at any time that it was inappropriate (e.g., during class or church). Participants received $20 or $40 for each session they completed and could earn an additional $20 at certain sessions for excellent compliance with the EMA protocol (up to a total of $320). Gwaltney, Bartolomei, Colby, and Kahler (2008) utilized a very similar procedure and can be referenced for further details.
Figure 1.
Flowchart depicting study design.
Baseline
Prior to EMA data collection, participants responded to a battery of paper-and-pencil questionnaires. Assessed constructs included demographic information and smoking-related beliefs and behaviors.
Pre-Quit Period
Participants practiced using all of the features of the TED software during the first 2 monitoring days. On study day 2, staff reviewed the data and any problems with the monitoring protocol were discussed and resolved with the participant. Participants continued monitoring their ad lib smoking over the next 5 days. Throughout this pre-quit period, participants reported about their environments (including the social context) during smoking and nonsmoking assessments.
Post-Quit Period
At the end of the first week of monitoring, data were uploaded and participants were trained to interact with the TED on and after the quit date. On the morning of study day 8, an “I’m Quit” option was available on the TED main menu; participants selected this option when they decided to initiate their quit attempt. This was the milestone used to demarcate the quit attempt from ad lib smoking (participants could also indicate when they had stopped a quit attempt, or when they were beginning a new attempt). Previous research (e.g., Bancej et al., 2007; Choi et al., 2002) indicates that adolescents who express a desire to quit typically begin to lapse very shortly after initiating a quit attempt. Therefore, there was no minimal amount of abstinence required for participants to be considered as making a quit attempt.
Participants were asked to begin their quit attempt when they woke up on study day 8, but they could initiate the attempt at any time. For the ensuing two weeks of monitoring, participants continued to record episodes of smoking. Throughout this post-quit period, they reported about their environments (including the social context) during smoking and nonsmoking assessments, when they experienced a temptation to smoke, and when they experienced a lapse. Participants met with the study staff at the end of the second and third weeks of monitoring. At the end of the third week, participants returned their TED to the study staff.
Three-month Follow-Up
A final session took place approximately three months following the end of EMA data collection. At this time, participants reported about their recent smoking behaviors. There were 16 participants who either withdrew or could not be reached upon multiple contact attempts, leaving a follow-up sample of 163.
Measures
Baseline Assessment
Demographics
Youths reported their birthday (used to calculate age), gender, and race/ethnicity. The latter item was dichotomized into White (non-Hispanic) vs. non-White.
Smoking history
Youths reported the age at which they smoked their first cigarette. This item was then subtracted from current age to obtain a measure of years smoked. The Smoking Timeline Follow-Back (TLFB; Lewis-Esquerre et al., 2005) was used to determine the number of cigarettes smoked (past 30 days); and the number of smoking days (in the past 30 days); these items were averaged to create a measure of smoking intensity. Dependence was assessed with the 7-item Modified Fagerstrom Tolerance Questionnaire (mFTQ; Prokhorov et al., 1996).
Cessation history
Youths reported if they had tried to quit in the past year (Yes or No).
Friend and family smoking
Youths were asked about the smoking status of their parents/guardians, older siblings, best friend, and boy/girlfriend. In addition, youths’ reports of the number of friends they have who smoke and their number of friends overall was used to compute a measure of the proportion of friends who smoke.
Cessation attitudes
At the screener, youths were asked to report on their motivation to quit and their confidence in quitting (for both single-item measures, 0 = not at all to 100 = extremely; Shiffman et al., 1996). At the second session, youths completed the situational temptations inventory for smokers (Plummer et al., 2001; α = .77). At the third session, participants reported on their commitment to quitting by responding to the Commitment to Quitting Smoking Scale (Kahler et al., 2007; α = .85).
Smoking expectancies
Items assessing youths’ expected consequences of smoking were based on the Adolescent Smoking Consequences Questionnaire (Lewis-Esquerre et al. 2005) and a short form of the Smoking Consequences Questionnaire (Myers, McCarthy, MacPherson, & Brown, 2003). Based on study hypotheses, we were particularly interested in subscales for negative affect reduction (α = .85), boredom reduction (α = .60), social facilitation (α = .73), and negative consequences (α = .70).
EMA Assessment
Social context
Youths were asked to indicate who they were with during smoking and nonsmoking assessments and could check multiple options: mother, father, brother, sister, child, other relatives, boy/girlfriend, friends, and others. The final option of the series was “no one,” which allowed participants to indicate if they were alone. Responses to this final question were used to create a binary measure of whether or not the participant was with someone at the time of the assessment (social vs. non-social). The variable was also used in our calculation of social lapsing (see analysis section).
Youths also reported where they were (home, a friend’s house, etc.) and about the presence of smoking cues (again, they could check multiple options, including smelling smoke and seeing ashtrays). In addition, if they had reported being with others, they were asked whether there were other people smoking (Yes or No). Youths next indicated what they were currently doing, and could check multiple options: using drugs or alcohol, doing schoolwork, eating or drinking, talking on the phone, doing a physical activity, talking, or “nothing”). Finally, a single item asked youths how they were feeling (from 1=very good, to 5=very bad).
Smoking behavior
A smoking lapse was defined as any occurrence of smoking (even a puff) after making an “I’ve Quit” entry on the TED (see Shiffman et al. 2006). Multiple experiences of lapsing could be recorded. The number of minutes between the first “I’ve Quit” entry and the first recorded lapse was also calculated to provide a measure of time to first lapse. Follow-up Assessment
Smoking outcomes
At the three-month follow-up, the TLFB was readministered to determine the number of cigarettes smoked per day (past 90 days); and the number of smoking days (past 90 days). As with baseline, these two items were averaged to create a measure of smoking intensity. We also asked participants for the number of days they spent quit (past 90 days). Dependence was re-assessed with the mFTQ. Salivary cotinine is a metabolite of nicotine; it is currently regarded as the best biomarker of tobacco smoke exposure (CDC, 2013) and, therefore, served as our exposure measure.
Analyses
Our objective was to assess individual differences in the relation between social context and lapsing during the quit attempt. We first ran descriptive statistics that characterized the sample and their lapsing events; descriptive statistics focused specifically on the context of youth’s first lapse, as this event is often considered the most important lapse (Shiffman, 2005) and would also have the largest N. The first lapse was defined as the first instance of smoking reported on EMA following the “I’ve Quit” entry.
Hypothesis 1: There are Individual Differences in Social Lapsing
The next step was to garner support for there being relatively stable individual differences in the extent to which adolescents lapse in social vs. non-social contexts. We conducted a series of two-way Pearson chi-square tests of to examine whether there were relations among the contexts of the first few lapses—for example, is the context of first lapse (social vs. non-social) associated with the context of second lapse (social vs. non-social)? Results could potentially range anywhere from no relation (indicating no individual differences) to a perfect relation (indicating a binary split between those who were always social lapsers and those who were always non-social lapsers). Yet based on our hypothesis, we expected the results to fall between these two extremes and indicate a continuous individual difference, such that youths who experienced a social lapse (compared to a non-social lapse) at one event were more likely to experience a social lapse at another event.
In order to examine the distribution of social lapsing in our sample, we also planned to compute a measure of individual differences in social lapsing (i.e., a single measure representing youths’ overall degree of social lapsing). We computed, within each participant, the correlation between observation type (smoking vs. non-smoking) and its corresponding context (social vs. non-social). To ensure the results reflected lapsing during a quit attempt, data were only used from the post-quit EMA period and only from assessments where participants were in a quit phase. Thus, data were excluded for periods when a participant smoked for three or more consecutive days (a common cut-off for relapse; Van Zundert et al., 2010; Hoeppner et al., 2014) or where participants reported that they were no longer trying to quit. Data were also excluded from participants who did not report both social and non-social entries and both lapsing and non-lapsing entries (correlations could not be computed for these individuals; n = 13). As both the observation type and context variables were dichotomous, we used a phi (ϕ) coefficient to index the correlation.
Hypothesis 2: Social Lapsing Propensity Relates to Baseline Measures and Cessation Outcomes
Assuming our first hypothesis was supported, we planned to (1) determine whether our social lapsing social lapsing (ϕ) coefficient was uniquely associated with baseline factors, and (2) determine whether this social lapsing measure was uniquely associated with smoking behavior at the three-month follow-up. Therefore, the social lapsing coefficient was used in a series of correlations, to determine the extent to which it was related to our measures of interest at baseline (demographics, smoking and cessation history, friend and family smoking, cessation attitudes, smoking expectancies) and during the quit attempt (smoking context, time to first lapse). Next, we correlated the social lapsing coefficient with our follow-up outcomes of interest (smoking intensity, days quit, dependence, cotinine), in order to test whether individual differences in social lapsing predict key smoking and cessation outcomes; these were followed by multivariable regressions, which allowed us to control for other variables (age, gender, and baseline smoking variables) that could potentially confound the effects. Our expectation throughout these analyses was that higher social lapsing would relate to lower indicators of dependence and better cessation outcomes.
In additional analyses, we sought to determine how the context of lapsing during a quit attempt differed from the context of smoking prior to the quit attempt. Therefore, we also calculated individuals’ pre-quit social smoking coefficient using data from the pre-quit EMA period. We then assessed the relation between this smoking coefficient and the social lapsing coefficient, as well as our other measures of interest.
Results
Descriptive Statistics
All 179 participants met our a priori criteria for EMA compliance (responding to more than 80% of nonsmoking assessments). Baseline reports indicated that the youths smoked an average of 10 cigarettes per day (SD = 5.5) and that in the past 30 days, youths had smoked on nearly every day (M number of smoking days = 29.3, SD = 1.9) Seventy-four percent of the youths had tried to quit in the past. Mean mFTQ scores averaged 4.9 (SD = 1.6) at baseline, suggesting a moderate level of nicotine dependence.
Following their target quit date, 166 (93%) of the youths reported at least one lapse. Over 79% of participants experienced their first lapse within 24 hours of their first quit attempt. Before implementing our criteria to exclude cases of relapse, we found that the number of lapses reported over the measurement period ranged from 0 to 43 (among those who lapsed, M = 8.5, SD = 6.8, Mode = 2). Only 37 (21%) of the youths reported at any time during EMA data collection that they were no longer trying to quit smoking.
Among those who lapsed, 121 (73%) reported that their first lapse was in the presence of other people (i.e., a social lapse). Lapsing with friends was by far the most common form of social lapse: 72% of social first lapses were with friends; other common social lapses were with boy/girlfriends (14%), brothers and/or sisters (13%), and mothers (11%). Sixty percent of those with a social first lapse reported that other people were smoking at the time. Among all first lapses, the most common location was home (34%); only 11% occurred in conjunction with drug or alcohol use (9% marijuana, ≤1% other drugs, alcohol, or a combination).
Stability of Individual Differences in Social Lapsing
Figure 2 illustrates the number of youths reporting social vs. non-social contexts at their first, second, and third smoking lapses. When comparing youths who reported at least two lapses (n = 159), chi-square results indicated that the number reporting a social (vs. non-social) second lapse varied by whether they had reported a social first lapse, χ2 (1, N = 159) = 12.30, p < .001. In fact, of the 115 youths who reported a social first lapse, 94 (82%) reported a social second lapse. Similar patterns were found when comparing second and third lapses, and first and third lapses (ps ≤ .01). Thus, youths who experienced a social (compared to a non-social) lapse at one event were much more likely to experience a social lapse at another event.
Figure 2.
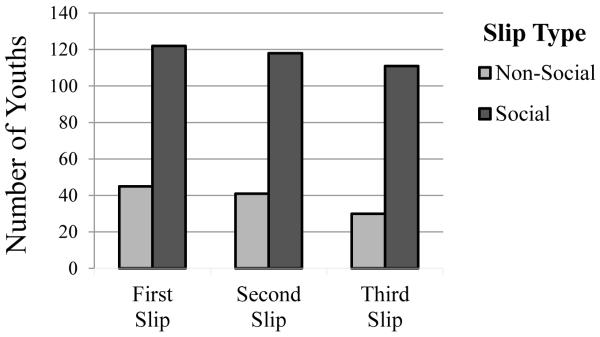
Context of participants’ first, second, and third smoking cessation lapses (coded as non-social or social), illustrating the high degree of stability in social lapsing.
Are Baseline Factors Associated with Individual Differences in Social Lapsing?
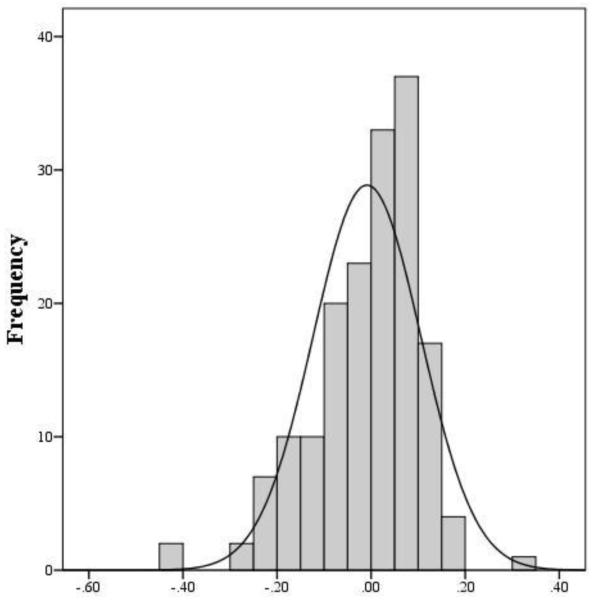
The social lapsing coefficient, representing the association between lapsing and social context ranged from −.43 (negative coefficients indicating that lapsing was more likely in non-social settings) to .35 (positive coefficients indicating that lapsing was more likely in social settings). The distribution is depicted in Figure 3. Mean score was zero (SD = .11). The social lapsing coefficient was not related to demographic characteristics, including age, gender, and White vs. non-White ethnicity (see Table 2 for all correlations of interest). Social lapsing was also unrelated to number of years smoked, friend and family smoking, and number of prior quit attempts; however, it had a significant negative association with measures of cotinine (r = −.21, p = .006), smoking intensity (r = −.19, p = .02) and dependence (r = −.21, p = .008), suggesting that youths who were heavier smokers and youths who had higher dependence were lapsing to a greater extent in non-social contexts.
Figure 3.
Distribution of the social lapsing coefficient. M = 0, SD = .11, Median = .02.
Table 2.
Sample means (SD) or percentages and correlations among variables of interest.
| M (SD) or % |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 16.6 (1.2) |
|||||||||||
| 2. Gender (male) | 64% | −.15* | ||||||||||
| Baseline Reports | ||||||||||||
| 3. Smoking intensity | 0.0 (0.8) | .08 | .05 | |||||||||
| 4. Attempted to quit in the past year |
74% | −.07 | .09 | −.07 | ||||||||
| 5. Dependence | 4.9 (1.6) | −.08 | −.07 | .44*** | .11 | |||||||
| EMA Pre-Quit Period | ||||||||||||
| 6. Pre-quit social smoking coefficient |
0.0 (.2) | .03 | −.00 | −.06 | −.12 | .02 | ||||||
| EMA Post-Quit Period | ||||||||||||
| 7. Social lapsing coefficient |
0.0 (0.1) | −.02 | .02 | −.19* | −.09 | −.21** | .09 | |||||
| 8. Time to first lapse, in minutes |
1321.0 (2778.9) |
.07 | .05 | −.17* | .08 | −.24** | −.06 | .09 | ||||
| 3-month Follow-Up | ||||||||||||
| 9. Smoking intensitya | 0.0 (0.9) | .04 | −.10 | .52*** | −.15 | .36*** | −.01 | −.19* | −.26** | |||
| 10. Days quit | 13.4 (24.0) |
.04 | .03 | −.38*** | .12 | −.23** | .05 | .15 | .27** | −.88*** | ||
| 11. Dependenceb | 5.5 (1.7) |
−.06 | −.08 | .34*** | −.04 | .66*** | .02 | −.14 | −.15 | .50*** | −.33*** | |
| 12. Cotinine (Ng/ml)b | 230.5 (172.9) |
.06 | −.15 | .40*** | .04 | .35*** | −.03 | −.31*** | −.04 | .48*** | −.44*** | .34*** |
No statistically significant change in variable from baseline to follow-up.
Variable showed a statistically significant increase from baseline to follow-up.
p < .05,
p < .01,
p < .001. Gender was coded as 0 = female, 1 = male.
For attitudes, there was no relation between social lapsing and confidence in quitting, motivation to quit, or commitment to quitting (ps > .2). Social lapsing was related to the smoking expectancy dimensions of negative affect reduction (r = −.17, p = .03) and negative consequences (r = .16, p = .04); however, there was no relation with the dimensions of boredom reduction, or social facilitation (ps > .16). Time to first lapse was not associated with social lapsing. Social lapsing was related to a greater presence of smoking cues at the first lapse (r = .31, p < .001), and was not significantly related to how participants were feeling at first lapse (r = .13, p = .08).
Do Individual Differences in Social Lapsing Predict 3-Month Cessation Outcomes?
Data from 163 participants were available for the follow-up session. Over this 90-day period, only two participants had maintained complete smoking abstinence. Youths reported smoking an average of 7.2 cigarettes per day (SD = 5.0). In the past 90 days, they had smoked on approximately 75 of the days (SD = 24.5). The social lapsing coefficient was correlated with several follow-up items. Specifically, social lapsing was related to lower smoking intensity (r = −.19, p = .02) and lower cotinine (r = −.31, p < .001); it was also marginally related to more days quit (r = .15, p = .07). There was not a significant relation with dependence. In a multivariable regression controlling for age, gender, and baseline smoking variables (smoking intensity, any quit attempt in the past year, and dependence), the effect of the social lapsing coefficient was not significant for smoking intensity or days quit, but remained significant for cotinine (p = .015; see Table S1). Thus, youths who had been lapsing more in social contexts showed some indication of better cessation outcomes three months later.
The pre-quit social smoking coefficient ranged from −.46 to .42 (M = 0, SD = .16). It was not related to the social lapsing coefficient (r = −.04, p = .59), or to any other constructs analyzed. Thus, the degree of lapsing in a social context, compared to a non-social context, appears to be unique to the quit attempt experience.
Discussion
The goal of this project was to improve models of adolescent smoking cessation by examining individual differences in social lapsing—i.e., the extent to which lapses occur around others vs. when alone. Our approach drew from smoking cessation Person × Environment interaction models (e.g., Witkiewitz & Marlatt, 2004; Deiches et al., 2013), which point to certain individuals being particularly vulnerable to lapsing in certain contexts; we also drew from adolescent research (e.g., Reifman et al., 2006; Somerville, 2013), which point to the important role that social factors play during that developmental period. Our methodology capitalized on the benefits of EMA, including its ability to continually collect data in real-time, during both lapsing and non-lapsing situations, as people go about their normal lives.
Data collected during the quit period revealed a very high rate of lapsing (93%); furthermore, only two participants had maintained complete smoking abstinence at the end of follow-up. These outcomes are consistent with the nearly universal adolescent relapse rates reported by others (Mermelstein, 2003; Killen et al., 2004; Sussman, 2002). Data additionally revealed a high rate of social lapsing: among those who lapsed, 73% reported that their first lapse was in the presence of other people. This high rate of social lapsing is comparable to Myers and colleagues’ (2011) adolescent sample (86%) and much higher than those reported in adult studies (e.g., 25% by Shiffman, 1982). In our sample, social lapsing occurred most commonly with friends, but did not appear to be entirely an issue of accessibility, as friends were not always smoking: only 60% of those with a social first lapse reported that other people were smoking at the time. Likewise, 11% of first lapses occurred in conjunction with alcohol use; this percentage is a concern given the age of the sample, but it is not so high as to suggest that alcohol is a driving factor for smoking lapses.
In support of our first hypothesis, individual differences in social lapsing appeared to be relatively stable. For example, among the youths who reported a social first lapse, 82% reported a social second lapse. Chi-square analyses confirmed this pattern, indicating that youths who experienced a social lapse (compared to a non-social lapse) at one event were much more likely to experience a social lapse at another event. Furthermore, the social lapsing coefficient (our continuous, computed measure of social lapsing) assumed a relatively normal distribution in our adolescent population.
Consistent with the second hypothesis, correlational analyses indicted that the social lapsing coefficient was negatively related to several baseline factors: smoking intensity, dependence, and cotinine (as well as negative affect reduction expectancies). It was not, however, related to any measures of demographics, friend and family smoking, motivation and confidence to quit, or commitment to quitting. Overall, this pattern of associations with baseline measures suggests that social lapsing is most strongly associated with being a lighter, less dependent smoker. Results from the 3-month follow-up succeeded from this pattern: social lapsing was related to lower smoking intensity and cotinine, and was marginally related to more quit days. To phrase it conversely, having a stronger relation between lapsing and being alone is associated with being a heavier, more dependent smoker, with less quitting success.
By examining associations with social smoking during a baseline pre-quit period, we also argued against alternative explanations that these socially-lapsing adolescents merely smoke more in social situations. Indeed, the social smoking coefficient, computed with pre-quit data, was not related to the social lapsing coefficient or to any other constructs analyzed. Such findings suggest that whereas the likelihood of smoking around others during the quit attempt is influenced by individual differences, the likelihood of smoking around others during ad lib smoking is more heavily based on chance. Results also support arguments (e.g., Moolchan, 2007) that the factors predicting smoking cessation are not identical to those predicting maintenance.
Our findings also provide some preliminary evidence of why social lapsing may be so pronounced among adolescents. Specifically, we found evidence that social lapsing was related to indicators of lower smoking intensity, exposure (cotinine), and nicotine dependence. This finding is partially consistent with the adult literature, which indicates an association between social smoking and lower smoking intensity (Moran, Wechsler & Rigotti, 2004; Levy, Biener, & Rigotti, 2009). Thus, the reason why adolescents, compared to adults, demonstrate higher rates of social lapsing (and, consequently, lower rates of lapsing when alone) could be partly attributable to the fact that adolescents have been smoking for fewer years, are lighter smokers, and have lower dependence. As dependence develops, factors such as negative affect, withdrawal symptoms, and craving may play a larger role in driving lapsing than social context (Colby & Gwaltney, 2007). Furthermore, it is likely that the differences between adults and adolescents are also partly attributable to differences in developmental age. Further work is needed to better understand this adult vs. adolescent difference. For instance, future studies might test whether social lapsing is related to factors known to be heightened during adolescence, such as the desire to affiliate with smoking peers.
Regarding the multivariable regression analyses, it is unclear why cotinine was significantly negatively related to social lapsing while smoking intensity and dependence were not. Cotinine is a measure of nicotine exposure; due to its half life of 15-17 hours, this measure may be indexing higher, more regular or consistent nicotine levels in adolescent smokers that are not reflected in self-reported measures of daily smoking or dependence. Our findings are suggestive that adolescents with higher cotinine levels may be smoking (or, in this study, lapsing) more for the reinforcing effects of nicotine than for the social aspects of smoking—a hypothesis that can be tested in future work.
Limitations and Future Directions
It is important to note that the present findings are in many ways preliminary. More specifically, the results contribute to the understudied topic of adolescent smoking cessation by pointing to the importance of social lapsing, yet they tell us nothing about the triggers for social lapsing. Thus, an important next step is to determine what factors lead certain adolescents to be more likely to engage in social lapsing (vs. non-social lapsing). Our analyses were unable to test the role of additional factors that were not assessed in the current study but that could be of potential importance. For example, youths high on extreme peer orientation or social anxiety may be more vulnerable to smoking as a way to affiliate with others. Further work is, therefore, also needed to determine the role of these unmeasured factors. Future work should also test whether the nature of our obtained relations change as a result of formal cessation treatment.
By asking adolescents to complete multiple entries throughout the day, our assessments needed to be relatively brief. Consequently, our measurement of social context was fairly simple. The brief assessments necessitated by EMA was a limitation to this study. The fact that we obtained significant results with a limited assessment suggests that this is an important factor in adolescent relapse; however, this work needs to be followed-up by future studies that have a more extensive focus on social context (e.g., what circumstances led adolescents to smoke alone vs. with others). Current effect sizes were small, but may increase with a more sensitive measure. Our findings are also based on a rather homogenous sample, in terms of age, education, etc. Therefore, it is important to replicate the results with adolescents of different ages and backgrounds.
Implications
The adult smoking literature has previously used analytical approaches that categorize people as either social lapsers or non-social lapsers. However, the present findings indicate that, at least among adolescents, the propensity for social lapsing ranges more continuously across individuals. Moreover, we found that individual differences in social lapsing subsequently predicted cessation-related outcomes at follow-up. The present study thus provides evidence that taking this distinction in social lapsing into account may improve theoretical models predicting adolescent smoking lapse/relapse.
By advancing theory, social lapsing may, consequently, also have implications for improving adolescent smoking cessation treatments. Interventions could, for instance, incorporate modules that are tailored for adolescents high on social lapsing and that target their social-lapsing triggers. However, as discussed above, further research is necessary to identify such triggers and understand their effects. This line of research is particularly important given that treatment efficacy is consistently lower among adolescents than adults (Colby & Gwaltney, 2007). A more thorough understanding of the processes underlying adolescent relapse— including a greater appreciation for the role of social context—could go far in improving the effectiveness of available adolescent treatments.
Supplementary Material
Acknowledgments
This study was supported by grants R01 DA021677, K23 DA033302, and T32 DA016184 from the National Institute on Drug Abuse.
Contributor Information
Megan E. Roberts, Center for Alcohol and Addiction Studies Brown University Providence, RI
L. Cinnamon Bidwell, Center for Alcohol and Addiction Studies, Brown University Division of Behavioral Genetics, Rhode Island Hospital Providence, RI.
Suzanne M. Colby, Center for Alcohol and Addiction Studies Brown University Providence, RI
Chad J. Gwaltney, Center for Alcohol and Addiction Studies Brown University Providence, RI and ERT, inc. 1818 Market St., Suite 1000 Philadelphia, PA
References
- Ashton H, Stepney R. Smoking: Psychology and pharmacology. Tavistock Publications; New York: 1982. [Google Scholar]
- Baker TB, Piper ME, Schlam TR, Cook JW, Smith SS, Loh WY, Bolt D. Are tobacco dependence and withdrawal related amongst heavy smokers? Relevance to conceptualizations of dependence. Journal of Abnormal Psychology. 2012;121(4):909. doi: 10.1037/a0027889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bancej C, O’Loughlin J, Platt RW, Paradis G, Gervais A. Smoking cessation attempts among adolescent smokers: a systematic review of prevalence studies. Tobacco Control. 2007;16(6):e8–e8. doi: 10.1136/tc.2006.018853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bliss RE, Garvey AJ, Ward KD. Resisting temptations to smoke: Results from within-subjects analyses. Psychology of Addictive Behaviors. 1999;13(2):143. [Google Scholar]
- Bolt DM, Piper ME, Theobald WE. Why two smoking cessation agents work better than one: role of craving suppression. Journal of Consulting and Clinical Psychology. 2012;80(1):54. doi: 10.1037/a0026366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC [Nov. 2014];Biomonitoring summary: Cotinine. 2013 Retrieved from http://www.cdc.gov/biomonitoring/Cotinine_BiomonitoringSummary.html.
- Chambers RA, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: a critical period of addiction vulnerability. American Journal of Psychiatry. 2003;160(6):1041–1052. doi: 10.1176/appi.ajp.160.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Presson CC, Sherman SJ, Montello D, McGrew J. Changes in peer and parent influence during adolescence: Longitudinal versus cross-sectional perspectives on smoking initiation. Developmental Psychology. 1986;22(3):327. [Google Scholar]
- Choi WS, Ahluwalia JS, Nazir N. Adolescent smoking cessation: implications for relapse-sensitive interventions. Archives of Pediatrics & Adolescent Medicine. 2002;156(6):625–626. doi: 10.1001/archpedi.156.6.625. [DOI] [PubMed] [Google Scholar]
- Colby SM, Gwaltney CJ. Pharmacotherapy for adolescent smoking cessation. JAMA: The Journal of the American Medical Association. 2007;298(18):2182–2184. doi: 10.1001/jama.298.18.2182. [DOI] [PubMed] [Google Scholar]
- Deiches JF, Baker TB, Lanza S, Piper ME. Early lapses in a Cessation attempt: lapse Contexts, Cessation success, and Predictors of early lapse. Nicotine & Tobacco Research. 2013;15(11):1883–1891. doi: 10.1093/ntr/ntt074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman MJ, Lester KM, McNamara C, Milby JB, Schumacher JE. Cell phones for ecological momentary assessment with cocaine-addicted homeless patients in treatment. Journal of Substance Abuse Treatment. 2006;30(2):105–111. doi: 10.1016/j.jsat.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Gwaltney CJ, Bartolomei R, Colby SM, Kahler CW. Ecological momentary assessment of adolescent smoking cessation: A feasibility study. Nicotine & Tobacco Research. 2008;10(7):1185–1190. doi: 10.1080/14622200802163118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwaltney CJ, Shiffman S, Balabanis MH, Paty JA. Dynamic self-efficacy and outcome expectancies: prediction of smoking lapse and relapse. Journal of Abnormal Psychology. 2005;114(4):661. doi: 10.1037/0021-843X.114.4.661. [DOI] [PubMed] [Google Scholar]
- Hoeppner BB, Kahler CW, Gwaltney CJ. Relationship between momentary affect states and self-efficacy in adolescent smokers. Health Psychology. 2014 doi: 10.1037/hea0000075. Advance online publication. http://dx.doi.org/10.1037/hea0000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Japuntich SJ, Leventhal AM, Piper ME, Bolt DM, Roberts LJ, Fiore MC, Baker TB. Smoker characteristics and smoking-cessation milestones. American Journal of Preventive Medicine. 2011;40(3):286–294. doi: 10.1016/j.amepre.2010.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman PM, Schulenberg JE. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2013. University of Michigan, Institute for Social Research; Ann Arbor (MI): 2014. [Google Scholar]
- Kahler CW, LaChance HR, Strong DR, Ramsey SE, Monti PM, Brown RA. The commitment to quitting smoking scale: Initial validation in a smoking cessation trial for heavy social drinkers. Addictive Behaviors. 2007;32(10):2420–2424. doi: 10.1016/j.addbeh.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenford SL, Fiore MC, Jorenby DE, Smith SS, Wetter DW, Baker TB. Predicting smoking cessation: who will quit with and without the nicotine patch. Journal of the American Medical Association. 1994;271:589–594. doi: 10.1001/jama.271.8.589. [DOI] [PubMed] [Google Scholar]
- Killen JD, Robinson TN, Ammerman S, Hayward C, Rogers J, Stone C, Schatzberg AF. Randomized clinical trial of the efficacy of bupropion combined with nicotine patch in the treatment of adoles-cent smokers. Journal of Consulting and Clinical Psychology. 2004;72(4):729–735. doi: 10.1037/0022-006X.72.4.729. [DOI] [PubMed] [Google Scholar]
- Levy DE, Biener L, Rigotti NA. The natural history of light smokers: a population-based cohort study. Nicotine & Tobacco Research. 2009;11(2):156–163. doi: 10.1093/ntr/ntp011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis-Esquerre JM, Colby SM, Tevyaw TOL, Eaton CA, Kahler CW, Monti PM. Validation of the timeline follow-back in the assessment of adolescent smoking. Drug and Alcohol Dependence. 2005;79(1):33–43. doi: 10.1016/j.drugalcdep.2004.12.007. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Curry S, Gordon JR. A longitudinal analysis of unaided smoking cessation. Journal of Consulting and Clinical Psychology. 1988;56(5):715. doi: 10.1037//0022-006x.56.5.715. [DOI] [PubMed] [Google Scholar]
- McKennell AC. Smoking motivation factors. British Journal of Social and Clinical Psychology. 1970;9(1):8–22. doi: 10.1111/j.2044-8260.1970.tb00632.x. [DOI] [PubMed] [Google Scholar]
- Mermelstein R. Teen smoking cessation. Tobacco Control. 2003;12(suppl 1):i25–i34. doi: 10.1136/tc.12.suppl_1.i25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moolchan ET, Fagan P, Fernander AF, Velicer WF, Hayward MD, King G, Clayton RR. Addressing tobacco-related health disparities. Addiction. 2007;102(s2):30–42. doi: 10.1111/j.1360-0443.2007.01953.x. [DOI] [PubMed] [Google Scholar]
- Moran S, Wechsler H, Rigotti NA. Social smoking among US college students. Pediatrics. 2004;114(4):1028–1034. doi: 10.1542/peds.2003-0558-L. [DOI] [PubMed] [Google Scholar]
- Myers MG, Gwaltney CJ, Strong DR, Ramsey SE, Brown RA, Monti PM, Colby SM. Adolescent first lapse following smoking cessation: Situation characteristics, precipitants and proximal influences. Addictive Behaviors. 2011;36(12):1253–1260. doi: 10.1016/j.addbeh.2011.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers MG, McCarthy DM, MacPherson L, Brown SA. Constructing a short form of the Smoking Consequences Questionnaire with adolescents and young adults. Psychological Assessment. 2003;15(2):163. doi: 10.1037/1040-3590.15.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niaura RS, Rohsenow DJ, Binkoff JA, Monti PM, Pedraza M, Abrams DB. Relevance of cue reactivity to understanding alcohol and smoking relapse. Journal of Abnormal Psychology. 1988;97(2):133. doi: 10.1037//0021-843x.97.2.133. [DOI] [PubMed] [Google Scholar]
- Plummer BA, Velicer WF, Redding CA, Prochaska JO, Rossi JS, Pallonen UE, Meier KS. Stage of change, decisional balance, and temptations for smoking: Measurement and validation in a large, school-based population of adolescents. Addictive Behaviors. 2001;26(4):551–571. doi: 10.1016/s0306-4603(00)00144-1. [DOI] [PubMed] [Google Scholar]
- Powell J, Dawkins L, West R, Powell J, Pickering A. Relapse to smoking during unaided cessation: clinical, cognitive and motivational predictors. Psychopharmacology. 2010;212(4):537–549. doi: 10.1007/s00213-010-1975-8. [DOI] [PubMed] [Google Scholar]
- Prokhorov AV, Pallonen UE, Fava JL, Ding L, Niaura R. Measuring nicotine dependence among high-risk adolescent smokers. Addictive Behaviors. 1996;21(1):117–127. doi: 10.1016/0306-4603(96)00048-2. [DOI] [PubMed] [Google Scholar]
- Reifman A, Watson WK, McCourt A. Social networks and college drinking: Probing processes of social influence and selection. Personality and Social Psychology Bulletin. 2006;32(6):820–832. doi: 10.1177/0146167206286219. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Relapse following smoking cessation: a situational analysis. Journal of Consulting and Clinical Psychology. 1982;50(1):71. doi: 10.1037//0022-006x.50.1.71. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Dynamic influences on smoking relapse process. Journal of Personality. 2005;73(6):1715–1748. doi: 10.1111/j.0022-3506.2005.00364.x. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychological Assessment. 2009;21(4):486. doi: 10.1037/a0017074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Hickcox M, Paty JA, Gnys M, Kassel JD, Richards TJ. Progression from a smoking lapse to relapse: prediction from abstinence violation effects, nicotine dependence, and lapse characteristics. Journal of Consulting and Clinical Psychology. 1996;64(5):993. doi: 10.1037//0022-006x.64.5.993. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Scharf DM, Shadel WG, Gwaltney CJ, Dang Q, Paton SM, Clark DB. Analyzing milestones in smoking cessation: illustration in a nicotine patch trial in adult smokers. Journal of Consulting and Clinical Psychology. 2006;74(2):276. doi: 10.1037/0022-006X.74.2.276. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: within-subjects analysis of real-time reports. Journal of Consulting and Clinical Psychology. 1996;64(2):366. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Balabanis MH, Gwaltney CJ, Paty JA, Gnys M, Kassel JD, Paton SM. Prediction of lapse from associations between smoking and situational antecedents assessed by ecological momentary assessment. Drug and Alcohol Dependence. 2007;91(2):159–168. doi: 10.1016/j.drugalcdep.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Waters AJ, Hickcox M. The nicotine dependence syndrome scale: a multidimensional measure of nicotine dependence. Nicotine & Tobacco Research. 2004;6(2):327–34. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- Slopen N, Kontos EZ, Ryff CD, Ayanian JZ, Albert MA, Williams DR. Psychosocial stress and cigarette smoking persistence, cessation, and relapse over 9–10 years: a prospective study of middle-aged adults in the United States. Cancer Causes & Control. 2013;24(10):1849–1863. doi: 10.1007/s10552-013-0262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville LH. The Teenage Brain Sensitivity to Social Evaluation. Current Directions in Psychological Science. 2013;22(2):121–127. doi: 10.1177/0963721413476512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville LH, Hare T, Casey BJ. Frontostriatal maturation predicts cognitive control failure to appetitive cues in adolescents. Journal of Cognitive Neuroscience. 2011;23(9):2123–2134. doi: 10.1162/jocn.2010.21572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP. The adolescent brain and age-related behavioral manifestations. Neuroscience & Biobehavioral Reviews. 2000;24(4):417–463. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- Stanton WR, Lowe JB, Gillespie AM. Adolescents’ experiences of smoking cessation. Drug and Alcohol Dependence. 1996;43(1):63–70. doi: 10.1016/s0376-8716(97)84351-7. [DOI] [PubMed] [Google Scholar]
- Sussman S. Effects of sixty-six adolescent tobacco use cessation trial and sev-enteen prospective studies of self-initiated quitting. Tobacco Induced Disease. 2002;1(1):35–81. doi: 10.1186/1617-9625-1-1-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweitzer MM, Denlinger RL, Donny EC. Dependence and withdrawal-induced craving predict abstinence in an incentive-based model of smoking relapse. Nicotine & Tobacco Research. 2013;15(1):36–43. doi: 10.1093/ntr/nts080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDS . Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2012. [Google Scholar]
- Van Zundert RM, Ferguson SG, Shiffman S, Engels RC. Dynamic effects of self-efficacy on smoking lapses and relapse among adolescents. Health Psychology. 2010;29(3):246. doi: 10.1037/a0018812. [DOI] [PubMed] [Google Scholar]
- Van Zundert RM, Ferguson SG, Shiffman S, Engels R. Dynamic effects of craving and negative affect on adolescent smoking relapse. Health Psychology. 2012;31(2):226. doi: 10.1037/a0025204. [DOI] [PubMed] [Google Scholar]
- Van Zundert RM, Nijhof LM, Engels RC. Testing social cognitive theory as a theoretical framework to predict smoking relapse among daily smoking adolescents. Addictive Behaviors. 2009;34(3):281–286. doi: 10.1016/j.addbeh.2008.11.004. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. American Psychologist. 2004;59(4):224. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Yeh VM, McCarthy DE, Baker TB. An ecological momentary assessment analysis of prequit markers for smoking-cessation failure. Experimental and Clinical Psychopharmacology. 2012;20(6):479. doi: 10.1037/a0029725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu SH, Sun J, Billings SC, Choi WS, Malarcher A. Predictors of smoking cessation in US adolescents. American Journal of Preventive Medicine. 1999;16(3):202–207. doi: 10.1016/s0749-3797(98)00157-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.