Abstract
Objective
Stimulant treatment improves impulse control among children with attention-deficit/hyperactivity disorder (ADHD). Decreased aggression often accompanies stimulant pharmacotherapy, suggesting that impulsiveness is integral to their aggressive behavior. However, children with high callous-unemotional (CU) traits and proactive aggression may benefit less from ADHD pharmacotherapy because their aggressive behavior seems more purposeful and deliberate. This study’s objective was to determine if pretreatment CU traits and proactive aggression affect treatment outcomes among aggressive children with ADHD receiving stimulant monotherapy.
Method
We implemented a stimulant optimization protocol with 160 6- to 13-year-olds (mean [SD] age of 9.31 [2.02] years; 78.75% males) with ADHD, oppositional defiant or conduct disorder, and significant aggressive behavior. Family-focused behavioral intervention was provided concurrently. Primary outcome was the Retrospective Modified Overt Aggression Scale. The Antisocial Process Screening Device and the Aggression Scale, also completed by parents, measured CU traits and proactive aggression, respectively. Analyses examined moderating effects of CU traits and proactive aggression on outcomes.
Results
82 children (51%) experienced remission of aggressive behavior. Neither CU traits nor proactive aggression predicted remission (CU traits: odds ratio=0.94, 95% CI=0.80–1.11; proactive aggression, odds ratio=1.05, 95% CI=0.86–1.29). Children whose overall aggression remitted showed decreases in CU traits (effect size=−0.379, 95% CI=−0.60 to −0.16) and proactive aggression (effect size=−0.463, 95% CI=−0.69 to −0.23).
Conclusions
Findings suggest that pretreatment CU traits and proactive aggression do not forecast worse outcomes for aggressive children with ADHD receiving optimized stimulant pharmacotherapy. With such treatment, CU traits and proactive aggression may decline alongside other behavioral improvements.
Keywords: aggression, attention-deficit/hyperactivity disorder (ADHD), CNS stimulants, oppositional defiant disorder, psychopathy
Introduction
Chronic aggressive behavior usually first develops during childhood1–3 and is among the foremost impairments for which children obtain mental health care.4 Different types of aggression, though, are thought to have distinct determinants and may therefore require different treatments.5–7 The leading approach to subtyping aggressive behaviors distinguishes incidents by the aggressor’s motivation.7–11 This framework differentiates aggressive behaviors with mainly defensive aims (reactive) from aggressive behaviors whose goals seem chiefly acquisitive (proactive).
Reactive aggression arises when frustration, annoyance, or perceived threat provokes hostile behaviors to repel them. Observers judge these reactions as aggressive when they are abnormally intense, dyscontrolled, or forceful and seem unwarranted because they follow commonplace triggers that age-mates endure with composure. Reactive aggression is a frequent complication of psychiatric disorders that raise susceptibility to negative affect, especially irritability, that impair impulse control, or that distort one’s detection and appraisal of threat.12–19
Proactive aggression describes harmful volitional behavior that extracts objects of desire (e.g., material goods, social dominance, sexual contact) through unjustified violation of someone else’s rights or well-being. Characteristics that facilitate proactive aggression include impulsiveness and inflated belief in one’s entitlement to satisfaction regardless of its consequences.20–22 Environmental factors that foster proactive aggression include association with milieus that reward and valorize coercive behavior, or that condone aggressive conduct because they regard its victims as adversaries or outsiders.23–25
An important individual factor that contributes to proactive aggression is flattened emotional response to others’ suffering, and, in particular, indifference to the hardship one’s behaviors cause.26 The leading descriptor of these features as callous-unemotional (CU) traits27 evokes well the diminished empathy, lack of remorse, and insincerity they engender. These characteristics are central to most definitions of psychopathy.28–30
While a proactive–reactive dichotomy offers a useful framework for aggressive behaviors, its value as a classification method for individuals is less clear. Many individuals display aggressive behaviors of both types.31,32 Quantitative measures of these behaviors show strong correlations.33–36 Among children, persistent proactive aggression most frequently develops among those with significant reactive aggressive behavior as well.32 The most common behavioral phenotypes involve either reactive aggressive behavior alone or reactive-plus-proactive aggressive behaviors.37
Elevated impulsivity in childhood seems to be a common substrate for both proactive and reactive aggressive behavior, which further reinforces their linkage.35 Psychometric and diagnostic data likewise show that impulsivity’s correlation with CU traits is substantial.2,31,38,39 More broadly, trait impulsivity heightens one’s risk for the “externalizing” disorders (oppositional defiant disorder [ODD], conduct disorder [CD], substance use, etc.) that share weak inhibitory behavioral control.40
Effective pharmacotherapy for the impulsivity, inattention, and hyperactivity associated with attention-deficit/hyperactivity disorder is well-established. Optimized stimulant treatment also often culminates in reduced aggressive behavior among youngsters with attention-deficit/hyperactivity disorder (ADHD), consistent with impulse control problems having an elemental role in childhood aggression.41 However, a common view is that proactive aggression, with roots not only in impulsivity but also in unfavorable socialization, will be less responsive to pharmacotherapy. e.g., 42 High proactive aggression might also signify greater severity and so predict weaker treatment effects for all conduct problems. Similarly, because aggression related to interpersonal callousness seems largely volitional, high CU traits may reduce the likelihood that conduct problems will diminish with pharmacotherapy for ADHD. Indeed, there is concern that improved self-control might contribute to more skillful deceit and coercive behavior.43
This study examined whether baseline CU traits and proactive aggression attenuate favorable changes in aggression and other behavioral outcomes following optimized stimulant pharmacotherapy among 6- to 13-year-old children with ADHD. Changes in CU traits and proactive aggression were also evaluated.
Method
Study Design
This report’s data come from the initial open stimulant titration phase of two clinical trials for children with ADHD, oppositional defiant or conduct disorder, and persistent aggressive behavior. One trial was conducted at Stony Brook University Medical Center (Stony Brook, New York) and at Long Island Jewish Medical Center (New Hyde Park, New York). The University of Texas Health Science Center at San Antonio joined these sites in a second trial.
Both trials implemented the same stimulant titration and monitoring protocol, whose objective was to identify each child’s most effective and best-tolerated stimulant monotherapy regimen. This protocol served as a lead-in phase to determine eligibility for randomized, double-blinded controlled trials of treatments added to stimulant medication for children whose aggressive behavior proved refractory to stimulant monotherapy.41,44
Participants
Participant eligibility criteria for both trials differed only by the required age at enrollment, which was 6-to 13-years-old in the first trial and 6–12 in the second. Boys and girls were eligible who met the following additional inclusion criteria.
Diagnosis: Participants fulfilled DSM-IV-TR criteria for (a) attention-deficit/hyperactivity disorder (any subtype), and (b) either oppositional defiant disorder (ODD) or conduct disorder (CD).
Severity of ADHD and Aggression: Parent ratings yielded scores at least 1.5 standard deviations above the normative mean for the child’s age and gender on both the Restless/Inattentive subscale of the Conners Global Index45,46 (ConnGI-P) and the Aggressive Behavior subscale of the Child Behavior Checklist47 (CBCL). Aggressive behavior during the preceding week had to be clinically significant, gauged by a total score more than 24 on the parent-completed Retrospective Modified Overt Aggression Scale (R-MOAS), as described in an earlier publication.44
Prior Pharmacotherapy: Children needed to have had prior treatment with psychostimulant medication for one month on at least 30 mg per day of methylphenidate or equivalent (e.g., 15 mg of an amphetamine-based compound, 15 mg of dexmethylphenidate).48,49 Requiring this threshold for prior treatment in addition to current symptom severity aimed to increase the likelihood that participants would have incomplete response to stimulant monotherapy and be eligible for the controlled trial of adjunctive medication.
Other: Eligibility required the child to live with a caregiver legally empowered to permit study enrollment and able to complete study assessments.
We excluded from participation children with major depressive disorder, bipolar I disorder, Tourette’s disorder, psychotic disorders, autistic disorder, and IQs below 70. An anxiety disorder was disqualifying if aggressive behavior was mainly a complication of it (e.g., a child with separation anxiety who became aggressive only in the context of separation situations). Health-related exclusion criteria were seizure disorders, pregnancy, and medical contraindications to treatment with stimulants, risperidone, or divalproex sodium.
After complete description of the study, parents or legal guardians provided written informed permission and children over 8 years old gave written assent. Each site’s Institutional Review approved procedures prior to trial commencement and conducted annual reviews for reapproval.
Recruitment and Evaluation Procedures
Parents interested in their child’s participation completed a screening interview, usually by telephone. Thereafter, eligible families attended an evaluation appointment that included the following components.
Diagnostic assessment comprised interviews with both parent and child utilizing the Schedule of Affective Disorders and Schizophrenia for School-Age Children50 (K[iddie]-SADS) by a clinical child psychologist (J.C.B.) or a child and adolescent psychiatrist (S.R.P., W.B.D., T.M.). Parents and children met for a separate clinical diagnostic evaluation with a child and adolescent psychiatrist (C.A.F., V.K., S.R.P., T.M., W.B.D., J.S., D.M.) or an advanced-practice nurse practitioner in child and adolescent psychiatry (C.S.) who also obtained medical history. The K-SADS interviewer and the clinical assessor conferred to arrive at consensus diagnoses.
Behavioral Outcomes
The primary outcome was the child’s posttreatment RMOAS total aggressive behavior score. Other endpoints were ADHD symptom status (per the ConnGI-P’s Restless/Inattentive subscale) and the CBCL’s Aggressive Behavior factor.
Measures of Proactive-Reactive Aggression and Callous-Unemotional Traits
Parents’ completed ratings on Vitiello and Stoff’s33 16-item Aggression Questionnaire (VAQ). This measure provides scores reflecting how much of the child’s aggressive behavior seems proactive (e.g., items pertaining to control, planning, concealment, care not to injure self) and reactive (e.g., items pertaining to dyscontrol, spontaneity, remorse, self-defeating or self-harmful acts during episodes). The scale emphasizes these elements of conduct disturbances, rather than the frequency of specific types of problem behaviors, making it a more specific assessment of willful/controlled vs. reactive/dyscontrolled aggressive behavior.
Parents also completed the Antisocial Process Screening Device51 (APSD). We used this scale’s 6-item Callous/Unemotional traits (CU) factor, which emphasizes unconcern for others, remorselessness, shallow emotionality, and manipulativeness. Parents completed the full scale, which also yields Narcissism and Impulsivity factors scores. This instrument has been widely used in research on CU traits among youth.
Parents completed these measures at the baseline assessment and at the end of the stimulant monotherapy protocol.
Stimulant Titration and Treatment Protocol
This section summarizes the stimulant monotherapy titration and treatment procedures used in both trials, which prior publications have detailed.41,44
Upon enrollment, children discontinued all nonstimulant psychotropic medications with tapering and duration appropriate to the compound’s elimination time course. Initial stimulant titration in most instances used a triphasic, osmotically-releasing methylphenidate preparation given once daily (MPH-TRI). Children who experienced problems attributable to MPH-TRI’s long duration of action (e.g., insomnia), could switch to a biphasic, bead-released MPH preparation (MPH-BI). Children who gained insufficient benefit for ADHD symptoms with MPH could switch to extended-release mixed amphetamine salts, administered once-daily as a biphasic-release, beaded preparation (MAS-XR).
Adjustments to stimulant agent and dosage concluded when (a) ADHD symptoms resolved, (b) unacceptable or unmanageable adverse effects contraindicated dose escalation, or (c) the agent’s daily ceiling was attained (MPH-TRI: 90 mg/d; MPH-BI: 50 mg/d; MAS-XR: 35 mg/d). Clinicians reviewed data from preceding weeks to identify the best tolerated regimen associated with greatest symptomatic improvement. That regimen was continued or reinstated for a “replication” week, followed by the endpoint assessment. Because the number of agents and dosages undertaken to identify each child’s optimal regimen differed between children, the length of this stimulant monotherapy optimization period varied. In some instances, children who completed this titration protocol during summer school breaks with good response had the final assessment of their regimen’s adequacy deferred, when clinically indicated, until school had resumed. The mean (SD) interval from baseline to stimulant endpoint assessments was 70.22 (37.48) days.
Concurrent Psychosocial Treatment
Families had behaviorally-oriented psychosocial treatment throughout the trial.. Treatment content was the COPE program,52 adapted for trials involving children with ADHD.53 Clinical psychologists or advanced graduate students provided this treatment.
Classification of Remitted vs. Refractory Aggressive Behavior
At the endpoint assessment, children with R-MOAS scores 15 and higher were classified as stimulant refractory. Those with lower scores were classified as having remission of their aggressive behavior, based on prior work indicating this range was associated with no or negligible aggressive behavior.41,44
Data Analysis
Linear and logistic regression, using SAS® PROC GLIMMIX, 54 evaluated demographic variables and study site for their associations with baseline proactive aggression subtype, CU traits and behavioral outcomes so that subsequent analyses could adjust for potential confounds.
Logistic regression tested the influence of baseline proactive aggression and CU trait ratings on the odds that aggression remitted at the end of the stimulant monotherapy protocol.
Analyses of change in the continuous-scale behavioral outcomes used SAS® PROC GLIMMIX,54 treating subjects as random effects, time as a fixed effect, and their interaction as the index of change. The interaction of baseline CU traits with time and of baseline proactive aggression with time tested moderation effects. Further analyses used severity groupings of these covariates as discrete, rather than continuous, predictors.
Results
Participant Sample Derivation and Characteristics
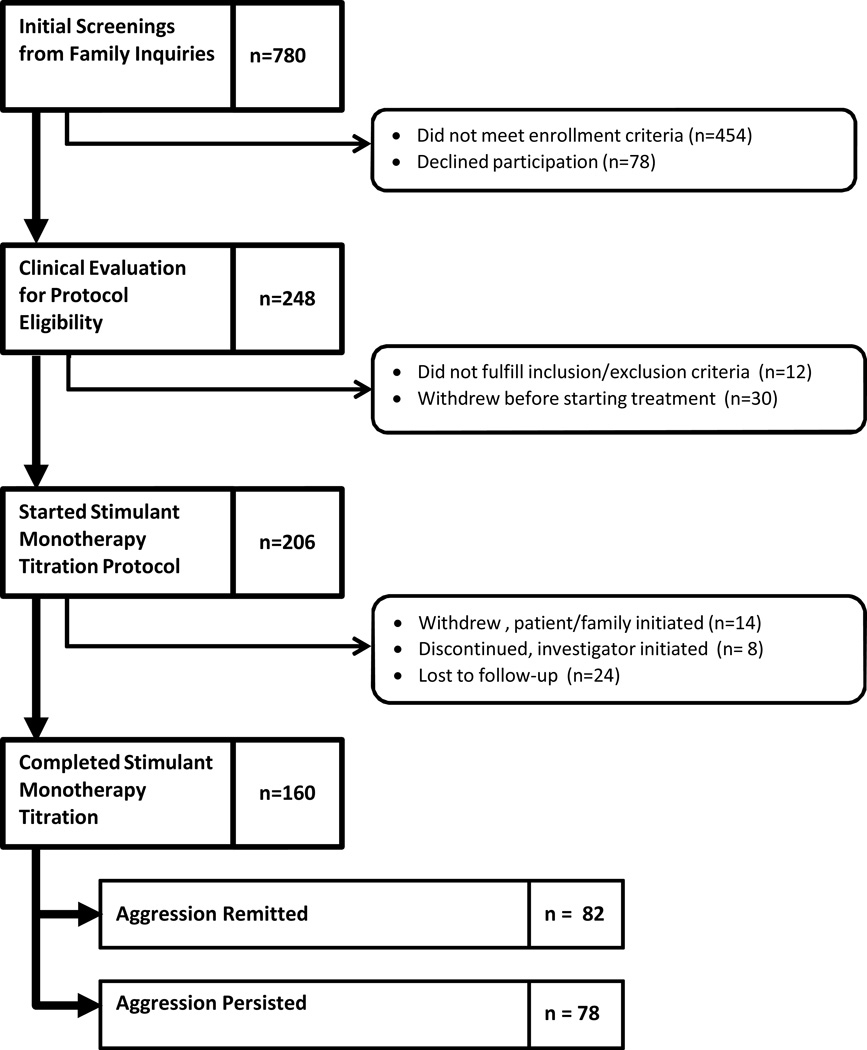
Between January 2004 and September 2012, 780 children were screened for the two trials. Figure 1 contains the CONSORT diagram of this cohort’s progress through the trial’s selection and treatment stages. Table 1 presents demographic and clinical characteristics of the 160 children who furnished data for this report.
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) Diagram.
Table 1.
Participants’ Demographic and Clinical Characteristics (N=160)
| Age, m (SD) | ||
| Years | 9.31 | (2.20) |
| Gender, n (%) | ||
| Male | 126 | (78.75) |
| Female | 34 | (21.25) |
| Race or Ethnic Group, n (%) | ||
| White | 94 | (58.75) |
| African-American | 25 | (15.63) |
| Hispanic | 31 | (19.38) |
| Other or mixed heritage | 10 | (6.25) |
| Diagnoses Comorbid with ADHD, n (%) | ||
| Oppositional defiant disorder | 143 | 89.38 |
| Conduct disorder | 17 | 10.63 |
| Anxiety disorder | 39 | 24.53 |
| Mood disorder | 18 | 11.32 |
| Optimized Stimulant Monotherapy Regimen, n (%) | ||
| Stimulant Preparation | ||
| Methylphenidate, triphasic release | 100 | 62.50 |
| Methylphenidate, biphasic release | 16 | 10.00 |
| Mixed amphetamine salts, extended release | 38 | 23.75 |
| Other | 6 | 3.75 |
| Total daily dose in MPH equivalent, m (SD) | ||
| Complete sample | 43.07 | 15.63 |
| Aggression-remitted group | 42.02 | 16.06 |
| Aggression-refractory group | 44.61 | 16.58 |
| Days from baseline assessment to final stimulant monotherapy endpoint assessment, m (SD) | ||
| Complete sample | 70.22 | 37.47 |
| Aggression-remitted group | 67.90 | 35.73 |
| Aggression-refractory group | 72.66 | 39.30 |
Note: ADHD = attention-deficit/hyperactivity disorder; MPH = methylphenidate
Age showed a significant association with overall aggression ratings. Older children had lower R-MOAS parent ratings averaged over time (BAge/Yrs = −1.99, t[147]= −2.17, p =.032), but reduction from baseline to endpoint was unrelated to age (BAge/Yrs × Time = 1.29, t[147] = 1.18, p = .24). Children at one site obtained lower aggression ratings than the other two (BSite = −10.77, t[147] = −2.23, p = .027). Subsequent analyses included age, the random effects of site, and their interactions with time as covariates.
Behavioral Outcomes
Table 2 summarizes behavioral rating scales data obtained at baseline and at the conclusion of the stimulant optimization trial. The table also contains standardized mean differences (SMD) from baseline to endpoint assessment55 and their 95% CI.
Table 2.
Behavioral Ratings and Standardized Mean Differences from Baseline to Endpoint
| Full Sample | Stimulant Monotherapy Outcome Groups | |||||||
|---|---|---|---|---|---|---|---|---|
| (N = 160) | Aggression Remitted (n=82) | Aggression Refractory (n=78) | ||||||
|
Baseline, m (SD) |
Stim End, m (SD) |
Baseline, m (SD) |
Stim End, m (SD) |
Difference Standardized (95% CI) |
Baseline, m (SD) |
Stim End, m (SD) |
Difference Standardized (95% CI) |
|
| Overt Aggression Total (RMOAS) | 52.65 (23.72) | 22.74 (24.14) | 47.30 (21.88) | 5.07 (5.32) | −1.769 (−2.58 to −0.96) | 58.28 (24.46) | 41.32 (22.17) | −0.711 (−1.73 to 0.31] |
| Proactive Aggression (VAQ) | 2.46 (1.58) | 2.16 (1.57) | 2.51 (1.60) | 1.77 (1.30) | −0.460 (−1.33 to 0.41) | 2.41 (1.57) | 2.58 (1.74) | 0.106 (−0.83 to 1.04) |
| Reactive Aggression (VAQ) | 3.86 (1.54) | 2.97 (1.99) | 3.73 (1.56) | 2.04 (1.76) | −1.065 (−2.24 to 0.11) | 3.99 (1.55) | 3.95 (1.77) | −0.029 (−0.88 to 0.82) |
| Callous-Unemotional (APSD) | 5.48 (2.01) | 5.10 (2.02) | 5.36 (1.95) | 4.64 (1.87) | −0.358 (−1.20 to 0.48) | 5.60 (2.05) | 5.59 (2.06) | −0.007 (−0.76 to 0.75) |
| Narcissism (APSD) | 6.45 (3.07) | 4.59 (2.77) | 6.79 (3.25) | 3.93 (2.59) | −0.916 (−1.73 to −0.10) | 6.10 (2.83) | 5.27 (2.80) | −0.263 (−0.95 to 0.43) |
| Impulsivity (APSD) | 7.14 (1.72) | 5.53 (2.20) | 7.07 (1.63) | 4.74 (2.14) | −1.340 (−2.45 to −0.23) | 7.22 (1.81) | 6.37 (1.94) | −0.486 (−1.25 to 0.28) |
| Restless/Inattentive, T (ConnGI) | 82.72 (9.15) | 64.68 (13.59) | 82.87 (9.65) | 59.61 (12.88) | −2.499 (−3.62 to −1.37) | 82.56 (8.63) | 70.01 (12.21) | −1.348 (−2.58 to −0.12) |
| Emotional Lability, T (ConnGI) | 79.48 (9.57) | 63.65 (15.10) | 78.95 (10.04) | 55.70 (12.88) | −2.412 (−3.58 to −1.24 ) | 80.03 (9.10) | 72.01 (12.50) | −0.832 (−2.00 to 0.34) |
| Externalizing Behavior, T (CBCL) | 71.50 (6.84) | 61.55 (10.17) | 70.82 (7.00) | 56.98 (9.84) | −1.922 (−3.02 to −0.83) | 72.20 (6.81) | 66.35 (8.08) | −0.812 (−1.76 to 0.14) |
Note: APSD = Antisocial Process Screening Device; CBCL = Child Behavior Checklist; ConnGI-P = Conners Global Index (Parent Version); R-MOAS = Retrospective-Modified Overt Aggression Scale; Stim = stimulant; VAQ = Vitiello Aggression Scale.
Just over half (82 of 160; 51%) experienced remission of their aggressive behavior. Children whose aggression remitted showed statistically reliable reductions from baseline on all measures (i.e., confidence intervals for the SMDs exclude zero), including proactive aggression and callous-unemotional traits.
Children whose overall aggressive behavior did not remit showed no statistically reliable changes from baseline (i.e., CIs included zero) on proactive aggression, reactive aggression, and callous-unemotional ratings. Their other behavioral outcomes reflected improvements, but SMDs were only 34% to 53% the magnitude found for the remitter group.
Effects of Baseline Proactive Aggression and CU Traits Scores on Behavioral Outcomes
Neither baseline proactive aggression nor CU traits affected the likelihood that a child would remit (Table 3). Likewise, interactions of baseline proactive aggression and CU traits with time were not statistically significant for any continuous-scale behavioral outcome, indicating that neither variable affected changes on these outcomes.
Table 3.
Effects of Baseline Measures of Proactive Aggression and Callous-Unemotional Traits on Trial Outcomes
| Effects | ||||||
|---|---|---|---|---|---|---|
| Time | Baseline Proactive Aggression |
Baseline Callous-Unemotional Traits |
||||
| Outcomes | Main Effect |
Main Effect |
Interaction with Time |
Main Effect |
Interaction with Time |
|
| Remission of Aggressive Behavior | or | 1.042 | 0.941 | |||
| 95% CI | 0.904–1.20 | 0.840–1.054 | ||||
| t | 0.564 | −1.049 | ||||
| Overt Aggression Total | B | −37.987 | 2.454 | −2.315 | 0.994 | 1.376 |
| t | −5.616*** | 2.060* | −1.664 | 1.019 | 1.202 | |
| Restless/Inattentive, T | B | −15.318 | 1.237 | −0.711 | 1.182 | −0.490 |
| t | −4.630*** | 2.641** | −0.994 | 3.282*** | −0.863 | |
| Emotional Lability, T | B | −13.029 | 0.756 | −0.694 | 0.480 | −0.506 |
| t | −3.646*** | 1.596 | −0.916 | 1.270 | −0.828 | |
| Externalizing Behavior, T | B | −11.780 | 2.066 | −0.438 | 0.918 | 0.338 |
| t | −5.171*** | 6.329*** | −0.869 | 3.170** | 0.860 | |
| Callous-Unemotional Traits | B | −0.201 | 0.332 | −0.076 | ||
| t | −0.721 | 3.400*** | −0.789 | |||
| Proactive Aggression | B | 0.385 | 0.218 | −0.124 | ||
| t | 0.935 | 3.435*** | −1.741 | |||
Note: OR = odds ratio.
p ≤ 0.05,
p ≤ 0.01,
p ≤ 0.001
Baseline proactive aggression was associated with greater severity on several measures averaged over assessments. There were significant main effects on overt aggression, restless/inattentive symptoms, CBCL Externalizing Behavior, and CU traits. Baseline CU traits showed main effects for restless/inattentive symptoms, CBCL Externalizing Behavior, and proactive aggression ratings, signifying in a similar manner their association with severity.
We tested the joint effects of proactive aggression and CU traits by including both of these covariates and their interaction. There were no significant interactions of proactive aggression and CU traits on any outcome.
We tested whether CU traits predict less improvement in proactive aggression specifically. The bottom row of Table 3 shows a meager CU traits by Time interaction on proactive aggression (p=.08). However, this effect is toward larger reductions in proactive aggression as a function of baseline CU traits.
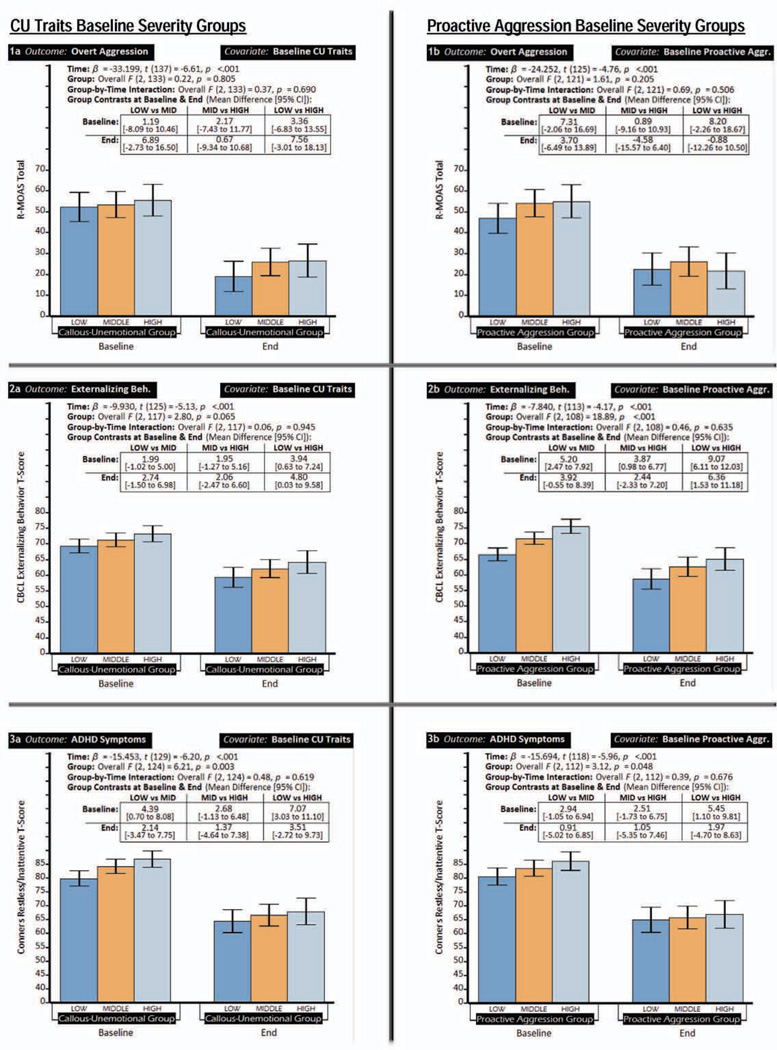
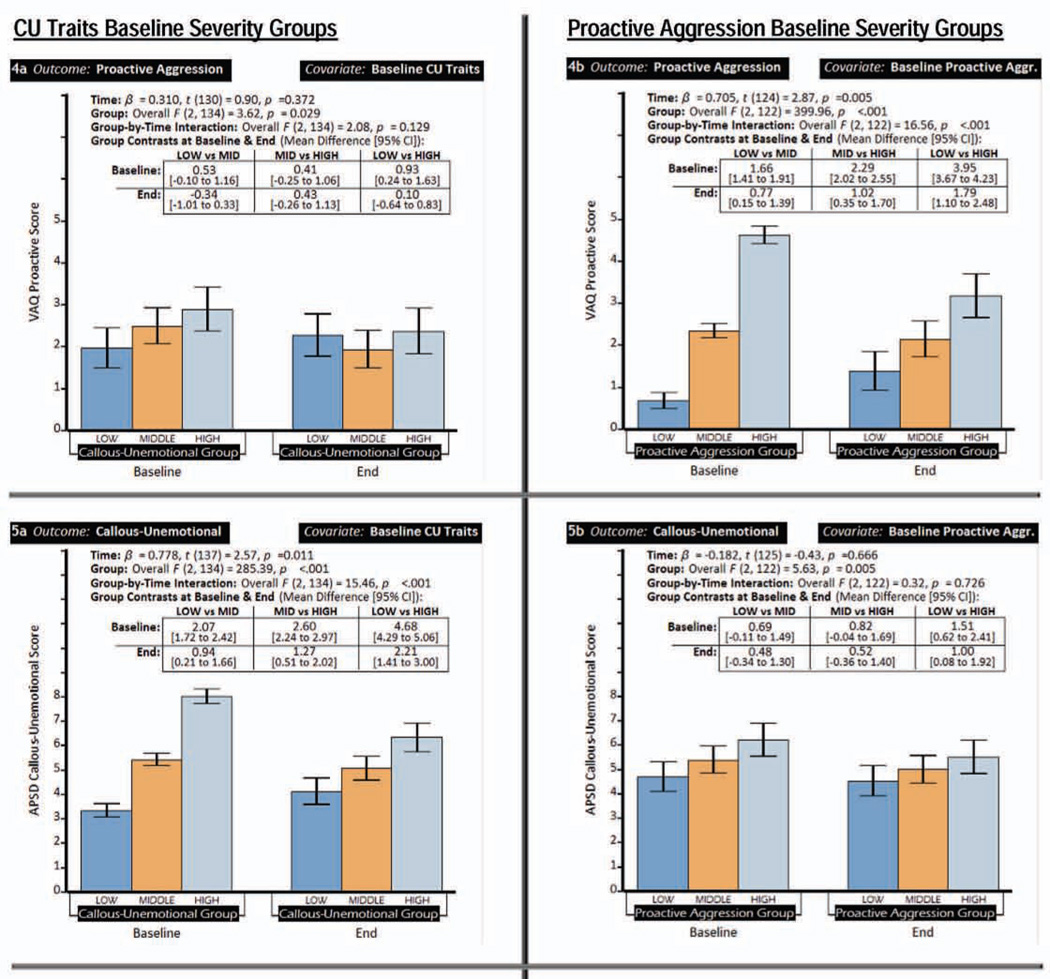
Effects of Severity Groupings for Baseline Proactive Aggression and CU Traits
Scores of 0 or 1 on the VAQ’s proactive subscale captured the lower 30.3%; of 2 or 3 were the middle 42.3%; and 4 through 7 were the upper 27.4%. Scores of 0 through 4 on the APSD’s CU subscale captured the lower 32.8%, 5 or 6 were the middle 42.2%, and 7 or above the upper 27.1%.
Figure 2’s histograms and analyses show overall higher behavioral symptoms as a function of baseline proactive aggression and CU traits severity grouping. However, a child’s severity group was unrelated to the magnitude of improvement on behavioral outcomes. The only significant interaction between baseline proactive aggression group and time was for proactive aggression itself (2a); those in the high group showed larger reductions after treatment. Baseline CU traits showed a similar pattern (4b).
Figure 2.
Behavioral outcomes for groups with low, middle, and high scores at baseline on proactive aggression and callous-unemotional traits. Note: Each row shows associations between one behavioral outcome and baseline severity groups (low, middle, high) of proactive aggression and callous-nemotional traits. Panels on the left show behavioral outcomes with participants stratified by proactive aggression group. Panels on the right show callous-unemotional traits groups. The table within each chart shows the contrasts between the 3 severity groups (the differences in least-squares means and the 95% CI for that difference) at baseline and at the end of the stimulant monotherapy protocol. APSD C-U = Antisocial Process Screening Device Callous-Unemotional scale; CBCL = Child Behavior Checklist; ConnGI-P = Conners Global Index (Parent Version); R-MOAS = Retrospective-Modified Overt Aggression Scale; VAQ = Vitiello Aggression Scale.
Effects of Categorical Callous-Unemotional CD Subtype Criteria
A new specifier for the diagnosis of CD, “With Significant Callous-Unemotional Traits”, designates individuals who manifest at least two of four CU cardinal features.56 Using baseline APSD CU ratings to apply these criteria,57 we identified 26 children (16.25%) as specifier-positive (diagnosis of conduct disorder, however, was not required). At the endpoint assessment, eleven (42.2%) met aggression-remission criteria, compared with 71 of 126 (53%) of the other participants. This difference is not statistically significant (OR [95% CI], 0.8 [0.52 – 1.26). Most (17 [62.4%]) children who fulfilled specifier-positive criteria at baseline did not at the endpoint assessment. Ten who were specifier-negative at baseline (7.46%) became specifier-positive at the endpoint.
Discussion
We examined whether elevated baseline CU traits or proactive aggression would diminish the effectiveness of stimulant monotherapy in reducing aggressive behavior among children with ADHD. These findings indicate that they do not. The possibility that CU traits selectively keep proactive aggression elevated was not supported.
Baseline ratings of proactive aggression and CU traits correlated with severity of behavioral disturbance. However, children who experienced remission of overt aggressive behavior also showed substantial reductions in post-treatment ratings of both CU traits and proactive aggression.
The assumption that successful coercive control over others perpetuates proactive aggression has implied that pharmacotherapy would be unhelpful in ameliorating it. Proactive aggression might also signify a more pernicious pattern of overall conduct problems that would prove refractory to treatment. Our results, in contrast, show that optimized treatment for ADHD warrants strong consideration as first-line intervention for children who present with significant aggression whether or not informants perceive that such behaviors are often volitional. This inference might not apply to children with ADHD whose aggressive behaviors are exclusively proactive, but preadolescents with this presentation in clinical settings are uncommon.
Mechanisms through which improved impulse control may lead to reduced proactive aggression warrant examination. Possible mechanisms may include improved capacity to delay gratification and, relatedly, to redirect one’s behavior away from high-intensity, high-reward situations that have unfavorable consequences.58,59 While pharmacotherapy may affect one or more “substrates” of childhood aggression (e.g., impulsiveness), environmental factors are probably important to changes in behavior. To delay gratification is not to forgo it entirely. Accordingly, devising alternative pathways to reward is a core element of behavioral interventions, including the one used in this trial. Peer group facilitation and reinforcement of antisocial behavior is a common feature of adolescent misconduct.60,61 Pharmacotherapy for underlying vulnerabilities, such as impulsivity, may be ineffective in reducing adolescent conduct disturbances unless disengagement from problematic peers also occurs.62
Earlier studies of CU traits and treatment response in this age group reported mixed results. Among 4-to 8-year-old children with ODD, but not ADHD, CU ratings predicted less benefit from behavioral management training for parents.63 In a full-day treatment program for 7- to 12-year-olds with ADHD and ODD/CD, those with higher CU ratings appeared to require stimulant treatment to ameliorate their conduct problems; children with lower CU ratings had consistently low daily conduct problems with or without stimulant treatment.64 In contrast, outpatient treatment for ODD or CD showed no influence of CU traits on outcomes adjusted for baseline severity, although teachers provided CU rating while parents supplied outcome data.65
The present report resolves some of these ambiguities. High CU ratings correlated with overall severity, but, in this cohort with significant persistent aggression, they did not work against treatment response to stimulant pharmacotherapy and behavioral intervention. Moreover, CU traits themselves improved along with reduced overt aggressive behavior.
Consistent with their conceptualization as traits, CU ratings display moderate consistency over time.66–69 Treatment studies that evaluated changes in children’s CU traits reported decreases, as we have.70, p. 138 These sets of findings are not incompatible. Although they decline when aggressive behavior improves, CU ratings among aggression remitters still corresponded to the 75th–95th percentiles of the normative sample.51, p. 36 Although it is encouraging that high CU trait ratings did not militate against treatment, the longer-term impact of persistently high CU traits is uncertain.
Still, our finding that CU ratings decline alongside other symptoms after stimulant monotherapy is not an obvious corollary of prevailing ideas about interpersonal callousness. This topic’s literature emphasizes the separability of CU traits from other factors that influence aggressive and antisocial behavior.71 But CU’s distinctiveness does not exclude a role for other factors in generating the behaviors associated with it. Some studies support a distinction between “primary” and “secondary” psychopathic traits 72,73. Primary psychopathy designates callous and harmful individuals who nevertheless show high social adeptness, confidence, and few psychiatric symptoms. In the secondary variant, psychopathic features result from psychopathology or adverse experiences, and so may be more responsive to treatment. Emotional instability and abuse have drawn attention in the genesis of secondary psychopathy.72 Likewise, the impulse control deficits that epitomize ADHD may identify those whose apparent callousness develops as a complication of long-term interpersonal conflict. CU features might then recede when timely treatment curbs the impulsive behavior that instigates these clashes.
An important limitation of this study is that measurement of proactive aggression and CU traits involves parents’ attributions and inferences concerning child motives. This method is susceptible to biases relating to parent-child relationships and parents’ explanatory frameworks for their children’s difficulties. Misspecification of aggression proactivity and CU traits is therefore possible. Relatedly, reductions in one salient characteristic such as aggression may evoke in raters a tendency to overestimate other positive changes, such as in CU traits. Such “halo effects,” however, seem tempered by findings that the effects sizes for CU traits are smaller than for overt aggression and ADHD symptoms.cf 74
Clinical trials, like other treatment encounters, provide participants information about diagnosis and treatment. This trial also included behavioral therapy intended to improve parent–child interactions. These psychoeducational and behavioral interventions may have led parents to attach less blame to the child as a willful protagonist of upsetting behavior.75 One might then expect that ratings of proactivity and CU traits would show meaningful reductions even if behavioral symptoms remained high. However, such reductions were not apparent among children whose aggression did not improve. Another limitation, common among short-term trials for chronic disturbances, is that their significance for long-term outcomes is uncertain.
Numerous studies have explored the psychophysiological, cognitive, neurofunctional, and neuroanatomical, correlates of aggression and CU traits, e.g., 76–79 with several focusing on youth.80 Stimulant treatment is likely to affect several of the brain systems implicated. This study suggests that the association between treatment-related neural changes and behavioral response may be a useful avenue to advance research on the emergence, differentiation, and curtailment of severe conduct problems among youth.
Acknowledgments
This work was supported by grants to Dr. Blader from the National Institute of Mental Health (K23MH064975 and R01MH080050), the National Alliance for Research on Schizophrenia and Depression (NARSAD; now Brain and Behavior Research Foundation), Abbott Laboratories (investigator-initiated research), and by grants from the National Center for Research Resources to Stony Brook University (MO1RR10710) and to the Feinstein Institute for Medical Research of North Shore–LIJ Health System (M01RR018535).
Dr. Blader served as the statistical expert for this research.
The authors are grateful to Jennifer Alexander, B.A., Gregory Carlson, B.A., Lauren Chorney, Ph.D., Ashley Conway, B.S., Alisa Jahns, B.A., Jennifer Puig, M.A., and Marcela Torres, Ph.D., at Stony Brook University, Stony Brook, NY; Ingrid Fuentes, B.A., and Michele Gonen, B.A., at Long Island Jewish Medical Center; and Michelle Perez, B.A., and Candy B. Rhine at the University of Texas HSC at San Antonio for their service as project coordinators.
Dr. Blader has received research grant support from the National Institutes of Health (NIH), NARSAD (now Brain and Behavior Research Foundation), Abbott Laboratories, and Supernus Pharmaceuticals; has served as a consultant to Shire and Supernus Pharmaceuticals; and has received research and service funding from the Texas State Health and Human Services Commission. Dr. Pliszka has received research grant support from NIH; research grant support and consultant honoraria from Johnson and Johnson, and Shire; and has received research and service funding from the Texas State Health and Human Services Commission. Dr. Kafantaris has received research support from NIH, Eli Lilly and Co., Pfizer, and Merck, and donation of study medication and matching placebo from AstraZeneca, GlaxoSmithKline, Janssen, Eli Lilly and Co., and Pfizer. Dr. Crowell has received research grant support from the National Institutes of Health. Dr. Carlson has received research support or honoraria from Pfizer, GlaxoSmithKline, Otsuka America, and Merck. Dr. Daviss has received research support from NIH, the U.S. Administration for Children and Families, NARSAD (now Brain and Behavior Research Foundation), and Lexicor, and consultant honoraria from Next Wave Pharmaceuticals, AvaCat, and Lexicor.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplemental material cited in this article is available online.
Disclosure: Drs. Foley, Sverd, Margulies, Matthews, and Bailey, Mr. Sauder, and Ms. Sinha report no biomedical financial interests or potential conflicts of interest.
References
- 1.Coie JD, Lochman JE, Terry R, Hyman C. Predicting early adolescent disorder from childhood aggression and peer rejection. J Consult Clin Psychol. 1992;60(5):783–792. doi: 10.1037//0022-006x.60.5.783. [DOI] [PubMed] [Google Scholar]
- 2.Byrd AL, Loeber R, Pardini DA. Understanding desisting and persisting forms of delinquency: The unique contributions of disruptive behavior disorders and interpersonal callousness. J Child Psychol Psychiatry. 2012;53(4):371–380. doi: 10.1111/j.1469-7610.2011.02504.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lahey BB, Loeber R, Burke JD, Applegate B. Predicting future antisocial personality disorder in males from a clinical assessment in childhood. J Consult Clin Psychol. 2005;73(3):389–399. doi: 10.1037/0022-006X.73.3.389. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Public Health Service. Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Washington, DC: U.S0 Department of Health and Human Services; 2000. [PubMed] [Google Scholar]
- 5.Ollendick TH, Jarrett MA, Wolff JC, Scarpa A. Reactive and proactive aggression: Cross-informant agreement and the clinical utility of different informants. J Psychopathol Behav Assess. 2009;31(1):51–59. [Google Scholar]
- 6.Fite PJ, Colder CR, Lochman JE, Wells KC. Developmental trajectories of proactive and reactive aggression from fifth to ninth grade. J Clin Child Adolesc Psychol. 2008;37(2):412–421. doi: 10.1080/15374410801955920. [DOI] [PubMed] [Google Scholar]
- 7.Card NA, Little TD. Proactive and reactive aggression in childhood and adolescence: A meta-analysis of differential relations with psychosocial adjustment. Int J Behav Dev. 2006;30(5):466–480. [Google Scholar]
- 8.Barker ED, Vitaro F, Lacourse E, Fontaine NM, Carbonneau R, Tremblay RE. Testing the developmental distinctiveness of male proactive and reactive aggression with a nested longitudinal experimental intervention. Aggress Behav. 2010;36(2):127–140. doi: 10.1002/ab.20337. [DOI] [PubMed] [Google Scholar]
- 9.Poulin F, Boivin M. The role of proactive and reactive aggression in the formation and development of boys' friendships. Dev Psychol. 2000;36(2):233–240. doi: 10.1037//0012-1649.36.2.233. [DOI] [PubMed] [Google Scholar]
- 10.Dodge KA, Lochman JE, Harnish JD, Bates JE, Pettit GS. Reactive and proactive aggression in school children and psychiatrically impaired chronically assaultive youth. J Abnorm Psychol. 1997;106(1):37–51. doi: 10.1037//0021-843x.106.1.37. [DOI] [PubMed] [Google Scholar]
- 11.Dodge KA, Coie JD. Social-information-processing factors in reactive and proactive aggression in children's peer groups. J Pers Soc Psychol. 1987;53(6):1146–1158. doi: 10.1037//0022-3514.53.6.1146. [DOI] [PubMed] [Google Scholar]
- 12.Blader JC, Jensen PS. Aggression in children: An integrative approach. In: Martin A, Volkmar FR, editors. Lewis’ Child and Adolescent Psychiatry: A Comprehensive Textbook. 4th ed. Baltimore: Lippincott, Williams, and Wilkins; 2007. pp. 467–483. [Google Scholar]
- 13.Klein RG, Mannuzza S, Olazagasti MA, et al. Clinical and functional outcome of childhood attentiondeficit/ hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69(12):1295–1303. doi: 10.1001/archgenpsychiatry.2012.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cassidy F, Forest K, Murry E, Carroll BJ. A factor analysis of the signs and symptoms of mania. Arch Gen Psychiatry. 1998;55(1):27–32. doi: 10.1001/archpsyc.55.1.27. [DOI] [PubMed] [Google Scholar]
- 15.Corrigan PW, Watson AC. Findings from the National Comorbidity Survey on the frequency of violent behavior in individuals with psychiatric disorders. Psychiatry Res. 2005;136(2-3):153–162. doi: 10.1016/j.psychres.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 16.Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: A 20-year prospective community-based study. Am J Psychiatry. 2009;166(9):1048–1054. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burke JD, Hipwell AE, Loeber R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. J Am Acad Child Adolesc Psychiatry. 2010;49(5):484–492. doi: 10.1097/00004583-201005000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rowe R, Costello EJ, Angold A, Copeland WE, Maughan B. Developmental pathways in oppositional defiant disorder and conduct disorder. J Abnorm Psychol. 2010;119(4):726–738. doi: 10.1037/a0020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Towbin K, Axelson D, Leibenluft E, Birmaher B. Differentiating bipolar disorder–not otherwise specified and severe mood dysregulation. J Am Acad Child Adolesc Psychiatry. 2013;52(5):466–481. doi: 10.1016/j.jaac.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Calvete E, Orue I. Social information processing as a mediator between cognitive schemas and aggressive behavior in adolescents. J Abnorm Child Psychol. 2012;40(1):105–117. doi: 10.1007/s10802-011-9546-y. [DOI] [PubMed] [Google Scholar]
- 21.Pardini DA, Lochman JE, Frick PJ. Callous/unemotional traits and social-cognitive processes in adjudicated youths. J Am Acad Child Adolesc Psychiatry. 2003;42(3):364–371. doi: 10.1097/00004583-200303000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Nestor PG. Mental disorder and violence: Personality dimensions and clinical features. Am J Psychiatry. 2002;159(12):1973–1978. doi: 10.1176/appi.ajp.159.12.1973. [DOI] [PubMed] [Google Scholar]
- 23.Gelfand M, Shteynberg G, Lee T, et al. The cultural contagion of conflict. Philos Trans R Soc Lond B Biol Sci. 2012;367(1589):692–703. doi: 10.1098/rstb.2011.0304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fite PJ, Vitulano M, Wynn P, Wimsatt A, Gaertner A, Rathert J. Influence of perceived neighborhood safety on proactive and reactive aggression. J Community Psychol. 2010;38(6):757–768. [Google Scholar]
- 25.Lickel B, Miller N, Stenstrom DM, Denson TF, Schmader T. Vicarious retribution: The role of collective blame in intergroup aggression. Pers Soc Psychol Rev. 2006;10(4):372–390. doi: 10.1207/s15327957pspr1004_6. [DOI] [PubMed] [Google Scholar]
- 26.Frick PJ, Morris AS. Temperament and developmental pathways to conduct problems. J Clin Child Adolesc Psychol. 2004;33(1):54–68. doi: 10.1207/S15374424JCCP3301_6. [DOI] [PubMed] [Google Scholar]
- 27.Frick PJ, White SF. Research Review: The importance of callous-unemotional traits for developmental models of aggressive and antisocial behavior. J Child Psychol Psychiatry. 2008;49(4):359–375. doi: 10.1111/j.1469-7610.2007.01862.x. [DOI] [PubMed] [Google Scholar]
- 28.Viding E. Annotation: Understanding the development of psychopathy. J Child Psychol Psychiatry. 2004;45(8):1329–1337. doi: 10.1111/j.1469-7610.2004.00840.x. [DOI] [PubMed] [Google Scholar]
- 29.Glenn AL, Raine A. The neurobiology of psychopathy. Psychiatr Clin North Am. 2008;31(3):463–475. doi: 10.1016/j.psc.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Kiehl KA. A cognitive neuroscience perspective on psychopathy: Evidence for paralimbic system dysfunction. Psychiatry Res. 2006;142:107–128. doi: 10.1016/j.psychres.2005.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Waschbusch DA, Willoughby MT, Pelham WE., Jr Criterion validity and the utility of reactive and proactive aggression: Comparisons to attention deficit hyperactivity disorder, oppositional defiant disorder, conduct disorder, and other measures of functioning. J Clin Child Psychol. 1998;27(4):396–405. doi: 10.1207/s15374424jccp2704_3. [DOI] [PubMed] [Google Scholar]
- 32.Atkins MS, Stoff DM, Osborne ML, Brown K. Distinguishing instrumental and hostile aggression: Does it make a difference? J Abnorm Child Psychol. 1993;21(4):355–365. doi: 10.1007/BF01261598. [DOI] [PubMed] [Google Scholar]
- 33.Vitiello B, Stoff DM. Subtypes of aggression and their relevance to child psychiatry. J Am Acad Child Adolesc Psychiatry. 1997;36(3):307–315. doi: 10.1097/00004583-199703000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Barratt ES, Stanford MS, Dowdy L, Liebman MJ, Kent TA. Impulsive and premeditated aggression: A factor analysis of self-reported acts. Psychiatry Res. 1999;86(2):163–173. doi: 10.1016/s0165-1781(99)00024-4. [DOI] [PubMed] [Google Scholar]
- 35.Raine A, Dodge K, Loeber R, et al. The Reactive–Proactive Aggression Questionnaire: Differential correlates of reactive and proactive aggression in adolescent boys. Aggress Behav. 2006;32(2):159–171. doi: 10.1002/ab.20115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Poulin F, Boivin M. Reactive and proactive aggression: Evidence of a two-factor model. Psychol Assess. 2000;12(2):115–122. doi: 10.1037//1040-3590.12.2.115. [DOI] [PubMed] [Google Scholar]
- 37.Yeh MT, Chen P, Raine A, Baker LA, Jacobson KC. Child psychopathic traits moderate relationships between parental affect and child aggression. J Am Acad Child Adolesc Psychiatry. 2011;50(10):1054–1064. doi: 10.1016/j.jaac.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fowler T, Langley K, Rice F, et al. Psychopathy trait scores in adolescents with childhood ADHD: The contribution of genotypes affecting MAOA, 5HTT and COMT activity. Psychiatr Genet. 2009;19(6):312–319. doi: 10.1097/YPG.0b013e3283328df4. [DOI] [PubMed] [Google Scholar]
- 39.Connor DF, Chartier KG, Preen EC, Kaplan RF. Impulsive aggression in attention-deficit/hyperactivity disorder: Symptom severity, co-morbidity, and attention-deficit/hyperactivity disorder subtype. J Child Adolesc Psychopharmacol. 2010;20(2):119–126. doi: 10.1089/cap.2009.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krueger RF, Markon KE, Patrick CJ, Iacono WG. Externalizing psychopathology in adulthood: A dimensionalspectrum conceptualization and its implications for DSM-V. J Abnorm Psychol. 2005;114(4):537–550. doi: 10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blader JC, Pliszka SR, Jensen PS, Schooler NR, Kafantaris V. Stimulant-responsive and stimulant-refractory aggressive behavior among children with ADHD. Pediatr. 2010;126(4):e796–e806. doi: 10.1542/peds.2010-0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Connor DF, Carlson GA, Chang KD, et al. Juvenile maladaptive aggression: A review of prevention, treatment, and service configuration and a proposed research agenda. J Clin Psychiatry. 2006;67(5):808–820. [PubMed] [Google Scholar]
- 43.Kahn J. Trouble, age 9: Can you call a 9-year-old a psychopath? The New York Times Magazine. 2012 May 11;:32. [Google Scholar]
- 44.Blader JC, Schooler NR, Jensen PS, Pliszka SR, Kafantaris V. Adjunctive divalproex sodium vs. placebo for children with ADHD and aggression refractory to stimulant monotherapy. Am J Psychiatry. 2009;166(12):1392–1401. doi: 10.1176/appi.ajp.2009.09020233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Conners CK. Conners 3rd Edition™ Manual. Toronto: Multi-Health Systems; 2008. [Google Scholar]
- 46.Conners CK. Conners' Rating Scales - Revised Technical Manual. North Tonawanda, NY: Multi-Health Systems; 1997. [Google Scholar]
- 47.Achenbach TM. The Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: ASEBA, University of Vermont; 2001. [Google Scholar]
- 48.Pelham WE, Aronoff HR, Midlam JK, et al. A comparison of Ritalin and Adderall: Efficacy and time-course in children with attention-deficit/hyperactivity disorder. [Accessed July 17, 2013];Pediatr. 1999 103(4):e43. doi: 10.1542/peds.103.4.e43. Available at http://pediatrics.aappublications.org/content/103/4/e43.full.html. [DOI] [PubMed] [Google Scholar]
- 49.Pliszka SR. Pharmacologic treatment of attention-deficit/hyperactivity disorder: Efficacy, safety and mechanisms of action. Neuropsychol Rev. 2007;17(1):61–72. doi: 10.1007/s11065-006-9017-3. [DOI] [PubMed] [Google Scholar]
- 50.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 51.Frick PJ, Hare RD. The Antisocial Process Screening Device. Toronto: Multi-Health Systems; 2001. [Google Scholar]
- 52.Cunningham CE, Bremner RB, Secord-Gilbert M. COPE: The Community Parent Education Program: A School-Based, Family-Systems Oriented Workshop for Parents of Children with Disruptive Behavior Disorders. Hamilton, Ont.: COPE Works; 2000. [Google Scholar]
- 53.Pelham WE, Gnagy EM, Burrows-Maclean L, et al. Once-a-day Concerta methylphenidate versus three-timesdaily methylphenidate in laboratory and natural settings. Pediatr. 2001;107(6 [online edition]):e105. doi: 10.1542/peds.107.6.e105. [DOI] [PubMed] [Google Scholar]
- 54.SAS Institute Inc. SAS/STAT® 93 User’s Guide. Cary, NC: SAS Institute; 2011. [Google Scholar]
- 55.Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychol Methods. 1996;1(2):170–177. [Google Scholar]
- 56.Frick PJ, Moffitt TE. Proposed Draft Revisions to DSM Disorders and Criteria (DSM-5 Task Force, ed) Washington, DC: American Psychiatric Association; 2010. A proposal to the DSM-V Childhood Disorders and the ADHD and Disruptive Behavior Disorders Work Groups to include a specifier to the diagnosis of conduct disorder based on the presence of callous-unemotional traits. [Google Scholar]
- 57.Kahn RE, Frick PJ, Youngstrom E, Findling RL, Youngstrom JK. The effects of including a callous-unemotional specifier for the diagnosis of conduct disorder. J Child Psychol Psychiatry. 2012;53(3):271–282. doi: 10.1111/j.1469-7610.2011.02463.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sonuga-Barke EJ. The dual pathway model of AD/HD: An elaboration of neuro-developmental characteristics. Neurosci Biobehav Rev. 2003;27(7):593–604. doi: 10.1016/j.neubiorev.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 59.Killeen PR, Tannock R, Sagvolden T. The four causes of ADHD: A framework. In: Stanford C, Tannock R, editors. Current Topics in Behavioral Neurosciences. Vol 9. Berlin: Springer-Verlag; 2012. pp. 391–425. [DOI] [PubMed] [Google Scholar]
- 60.Dishion TJ, Veronneau MH, Myers MW. Cascading peer dynamics underlying the progression from problem behavior to violence in early to late adolescence. Dev Psychopathol. 2010;22(3):603–619. doi: 10.1017/S0954579410000313. [DOI] [PubMed] [Google Scholar]
- 61.Henry DB, Tolan PH, Gorman-Smith D, Schoeny ME. Risk and direct protective factors for youth violence: Results from the Centers for Disease Control and Prevention's Multisite Violence Prevention Project. Am J Prev Med. 2012;43(2 Suppl 1):S67–S75. doi: 10.1016/j.amepre.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 62.Huey SJ, Jr, Henggeler SW, Brondino MJ, Pickrel SG. Mechanisms of change in multisystemic therapy: Reducing delinquent behavior through therapist adherence and improved family and peer functioning. J Consult Clin Psychol. 2000;68(3):451–467. [PubMed] [Google Scholar]
- 63.Hawes DJ, Dadds MR. The treatment of conduct problems in children with callous-unemotional traits. J Consult Clin Psychol. 2005;73(4):737–741. doi: 10.1037/0022-006X.73.4.737. [DOI] [PubMed] [Google Scholar]
- 64.Waschbusch DA, Carrey NJ, Willoughby MT, King S, Andrade BF. Effects of methylphenidate and behavior modification on the social and academic behavior of children with disruptive behavior disorders: The moderating role of callous/unemotional traits. J Clin Child Adolesc Psychol. 2007;36(4):629–644. doi: 10.1080/15374410701662766. [DOI] [PubMed] [Google Scholar]
- 65.Kolko DJ, Pardini DA. ODD dimensions, ADHD, and callous-unemotional traits as predictors of treatment response in children with disruptive behavior disorders. J Abnorm Psychol. 2010;119(4):713–725. doi: 10.1037/a0020910. [DOI] [PubMed] [Google Scholar]
- 66.Frick PJ, Kimonis ER, Dandreaux DM, Farell JM. The 4 year stability of psychopathic traits in non-referred youth. Behav Sci Law. 2003;21(6):713–736. doi: 10.1002/bsl.568. [DOI] [PubMed] [Google Scholar]
- 67.Obradović J, Pardini DA, Long JD, Loeber R. Measuring interpersonal callousness in boys from childhood to adolescence: An examination of longitudinal invariance and temporal stability. J Clin Child Adolesc Psychol. 2007;36(3):276–292. doi: 10.1080/15374410701441633. [DOI] [PubMed] [Google Scholar]
- 68.Loney BR, Taylor J, Butler MA, Iacono WG. Adolescent psychopathy features: 6-year temporal stability and the prediction of externalizing symptoms during the transition to adulthood. Aggress Behav. 2007;33(3):242–252. doi: 10.1002/ab.20184. [DOI] [PubMed] [Google Scholar]
- 69.Lynam DR, Caspi A, Moffitt TE, Loeber R, Stouthamer-Loeber M. Longitudinal evidence that psychopathy scores in early adolescence predict adult psychopathy. J Abnorm Psychol. 2007;116(1):155–165. doi: 10.1037/0021-843X.116.1.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Loeber R, Burke J, Pardini DA. Perspectives on oppositional defiant disorder, conduct disorder, and psychopathic features. J Child Psychol Psychiatry. 2009;50(1-2):133–142. doi: 10.1111/j.1469-7610.2008.02011.x. [DOI] [PubMed] [Google Scholar]
- 71.Poythress NG, Edens JF, Skeem JL, et al. Identifying subtypes among offenders with antisocial personality disorder: A cluster-analytic study. J Abnorm Psychol. 2010;119(2):389–400. doi: 10.1037/a0018611. [DOI] [PubMed] [Google Scholar]
- 72.Skeem J, Johansson P, Andershed H, Kerr M, Louden JE. Two subtypes of psychopathic violent offenders that parallel primary and secondary variants [published correction appears in J Abnorm Psychol 2007;116:853] J Abnorm Psychol. 2007;116(2):395–409. doi: 10.1037/0021-843X.116.2.395. [DOI] [PubMed] [Google Scholar]
- 73.Kimonis ER, Skeem JL, Cauffman E, Dmitrieva J. Are secondary variants of juvenile psychopathy more reactively violent and less psychosocially mature than primary variants? Law Hum Behav. 2011;35(5):381–391. doi: 10.1007/s10979-010-9243-3. [DOI] [PubMed] [Google Scholar]
- 74.Pingault JB, Tremblay RE, Vitaro F, et al. Childhood trajectories of inattention and hyperactivity and prediction of educational attainment in early adulthood: a 16-year longitudinal population-based study. Am J Psychiatry. 2011;168(11):1164–1170. doi: 10.1176/appi.ajp.2011.10121732. [DOI] [PubMed] [Google Scholar]
- 75.Johnston C, Hommersen P, Seipp CM. Maternal attributions and child oppositional behavior: A longitudinal study of boys with and without attention-deficit/hyperactivity disorder. J Consult Clin Psychol. 2009;77(1):189–195. doi: 10.1037/a0014065. [DOI] [PubMed] [Google Scholar]
- 76.Gregory S, ffytche D, Simmons A, et al. The antisocial brain: Psychopathy matters. Arch Gen Psychiatry. 2012;69(9):962–972. doi: 10.1001/archgenpsychiatry.2012.222. [DOI] [PubMed] [Google Scholar]
- 77.Anderson NE, Kiehl KA. The psychopath magnetized: Insights from brain imaging. Trends Cogn Sci. 2012;16(1):52–60. doi: 10.1016/j.tics.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lorber MF. Psychophysiology of aggression, psychopathy, and conduct problems: A meta-analysis. Psychol Bull. 2004;130(4):531–552. doi: 10.1037/0033-2909.130.4.531. [DOI] [PubMed] [Google Scholar]
- 79.Sadeh N, Verona E. Psychopathic personality traits associated with abnormal selective attention and impaired cognitive control. Neuropsychology. 2008;22(5):669–680. doi: 10.1037/a0012692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Patrick CJ, Durbin CE, Moser JS. Reconceptualizing antisocial deviance in neurobehavioral terms. Dev Psychopathol. 2012;24(3):1047–1071. doi: 10.1017/S0954579412000533. [DOI] [PubMed] [Google Scholar]