Dear Editor:
Atopic dermatitis (AD) is a relapsing chronic inflammatory pruritic skin disorder that has been partially attributed to skin barrier dysfunction. Skin barrier function was previously estimated by measuring skin hydration and transepidermal water loss (TEWL), and low levels of skin hydration along with high levels of TEWL were reported in AD patients1,2. N-acetylcysteine (NAC) is a thiol derivative that stimulates the synthesis of glutathione, an internal antioxidant. NAC has been clinically used as a mucolytic agent as well as an antidote for acetaminophen toxicity. NAC was previously reported to be useful in the treatment of skin diseases including toxic epidermal necrolysis and lamellar ichthyosis3,4. NAC may exert beneficial effects in skin diseases by: (1) reacting with oxidative intermediates and replenishing intracellular cysteine levels; (2) inhibiting the production of proinflammatory cytokines and factors; and (3) regulating epidermal proliferation. In the present study, we assessed the clinical effects of topical NAC on skin hydration and TEWL in healthy volunteers and AD patients.
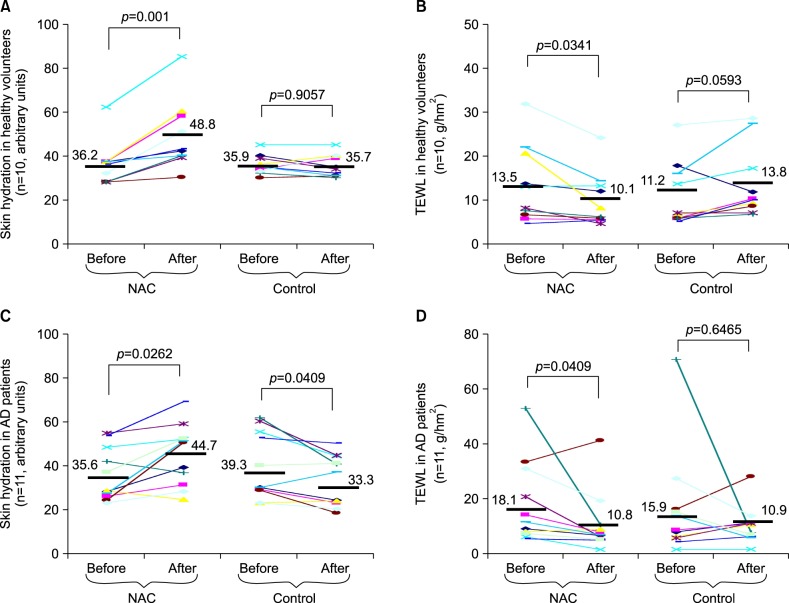
We enrolled 10 healthy volunteers (6 males and 4 females, age range: 28 to 76 years) and 11 AD patients (6 males and 5 females, age range: 31 to 73 years). AD patients had been receiving topical treatments including corticosteroids and tacrolimus ointment. Patients were not receiving cyclosporine or methotrexate. Patients with severe co-existing conditions as well as those with a heavy smoking status and/or high alcohol consumption were excluded. Informed consent was obtained from all patients. This study was approved by the Ethics Committee of the Faculty of Medicine, Kagawa University (No. 20-14). A NAC solution (20 w/v%; Senju Pharmaceutical Co., Ltd., Osaka, Japan) or its control vehicle was applied to the forearm skin twice a day for 4 weeks. Forearm skin hydration and TEWL were measured before and after the topical NAC application. Skin hydration and TEWL were measured using a Corneometer and Tewameter (Courage+Khazaka Electronic GmbH, Cologne, Germany). The topical application of NAC for 4 weeks increased skin hydration in 9/10 healthy volunteers (Fig. 1A, increase from 36.2±9.9 to 48.8±15.7 arbitrary units, p=0.001) and decreased TEWL in 8/10 healthy volunteers (Fig. 1B, decrease from 13.5±8.9 to 10.1±6.1 g/hm2, p= 0.0341). Topical application of the control vehicle for 4 weeks decreased skin hydration in 8/11 AD patients (Fig. 1C, decrease from 39.3±15.1 to 33.3±11.6 arbitrary units, p=0.0409). The topical application of NAC increased skin hydration in 9/11 AD patients (Fig. 1C, increase from 35.6±12.0 to 44.7±13.9 arbitrary units, p=0.0262) and decreased TEWL in 9 AD patients (Fig. 1D, decrease from 18.1±15.1 to 10.8±11.2 g/hm2, p=0.0409).
Fig. 1. (A, B) Effects of the topical application of N-acetylcysteine (NAC) (for 4 weeks) on skin hydration and transepidermal water loss (TEWL) in healthy volunteers. (C, D) Effects of the topical application of NAC on skin hydration and TEWL in atopic dermatitis (AD) patients. Skin hydration and TEWL were measured before and 4 weeks after the twice daily application of NAC or its control vehicle. Statistical analysis was performed using the Wilcoxon signed-rank test.
In a mouse model of AD, NAC was reported to restore the expression of some cell adhesion molecules that contribute to skin barrier formation by reducing oxidative stress5. Therefore, the topical application of NAC may increase skin hydration and decrease TEWL by strengthening the function of this barrier. Lamellar ichthyosis exhibits abnormal keratinization due to TGM1 gene mutations and a differential pattern of filaggrin expression, which implies that the success of NAC treatment in lamellar ichthyosis may be attributed to NAC-induced amelioration of abnormal keratinization and improvements in skin barrier function. Our results also support the possibility of skin barrier function restoration by NAC. Although AD patients generally have low levels of skin hydration and high levels of TEWL1,2, we could not obtain consistent results. Some AD patients have been shown to have normal skin barrier function6, and these values can be affected by various factors such as seasonality, exercise, and lifestyle. Thus, future studies involving a larger number of patients and excluding skin barrier-deteriorating factors are required to accurately assess the effects of NAC on AD.
References
- 1.Werner Y. The water content of the stratum corneum in patients with atopic dermatitis. Measurement with the Corneometer CM 420. Acta Derm Venereol. 1986;66:281–284. [PubMed] [Google Scholar]
- 2.Werner Y, Lindberg M. Transepidermal water loss in dry and clinically normal skin in patients with atopic dermatitis. Acta Derm Venereol. 1985;65:102–105. [PubMed] [Google Scholar]
- 3.Vélez A, Moreno JC. Toxic epidermal necrolysis treated with N-acetylcysteine. J Am Acad Dermatol. 2002;46:469–470. doi: 10.1067/mjd.2002.118557. [DOI] [PubMed] [Google Scholar]
- 4.Redondo P, Bauzá A. Topical N-acetylcysteine for lamellar ichthyosis. Lancet. 1999;354:1880. doi: 10.1016/S0140-6736(99)04245-2. [DOI] [PubMed] [Google Scholar]
- 5.Nakai K, Yoneda K, Hosokawa Y, Moriue T, Presland RB, Fallon PG, et al. Reduced expression of epidermal growth factor receptor, E-cadherin, and occludin in the skin of flaky tail mice is due to filaggrin and loricrin deficiencies. Am J Pathol. 2012;181:969–977. doi: 10.1016/j.ajpath.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Tokura Y. Extrinsic and intrinsic types of atopic dermatitis. J Dermatol Sci. 2010;58:1–7. doi: 10.1016/j.jdermsci.2010.02.008. [DOI] [PubMed] [Google Scholar]