Abstract
Background In elderly patients, distal radius fractures frequently occur in osteoporotic bone and may be nonreconstructable. It is our hypothesis that a hemiarthroplasty replacment of the articular surface can provide satisfactory results in terms of range of motion, pain, and function for immediate salvage of a fracture that is not amenable to internal fixation.
Methods Between July 2009 and January 2012, eight elderly patients were treated with insertion of a Sophia distal radius implant (Biotech, Paris, France). Inclusion criteria consisted of an isolated AO type C2 distal radius fracture in patients over 70 years old. All patients were reviewed by an independent surgeon.
Results The mean follow-up was 25 months (range, 17–36 months). Mean wrist range of motion (ROM) was 45° (40–50°) of flexion, 44° (40–50°) of extension, and a mean pronation-supination arc of 160°. Mean grip force was 18 kgf. The mean QuickDASH (Disabilities of the Arm, Shoulder and Hand) was 18.2/100 (6.82–29.55), and the mean visual analog scale (VAS) was 2.33 (0–4). X-ray images did not demonstrate implant loosening or ulnar translation of the carpus.
Conclusions The Sophia hemiarthroplasty provided rapid recovery of independence in elderly patients with a nonreconstructable comminuted distal radius fracture.
Keywords: distal radius fractures, prosthesis, epiphyseal comminution
Displaced distal radius fractures are becoming more frequent and remain a public health problem.1 Treatment options are numerous.2 3 4 Although malunion may be tolerated in the elderly,5 some authors still strive for a restoration of the bony alignment.4 6 Complex articular fractures in the knee or elbow are often treated with primary prosthetic replacement.7
These concerns prompted us to investigate the use of a resurfacing prosthesis for comminuted nonreconstructable distal radius fractures in elderly patients, as first described by Roux.8
Materials and Methods
Patients
Eight elderly patients with complex articular distal radius fractures underwent a primary hemiarthroplasty of the comminuted articular surface from 2009 to 2012 using the Sophia implant (Biotech) (Fig. 1). This anatomic prosthesis is composed of a radial stem and an epiphyseal-metaphyseal block that articulates with both the carpus and the ulnar head. The purpose of this implant is to restore the length of the radius and replace the radiocarpal and distal radioulnar joint while providing immediate stability. The same surgeon performed all of the procedures. Inclusion criteria were fractures with metaphyseal comminution, significant radial shortening, and articular comminution (AO type C-2) in patients over 70 years old. Patients with a distal ulna fracture were excluded because the cutting guide relies on an intact ulnar head.
Fig. 1.
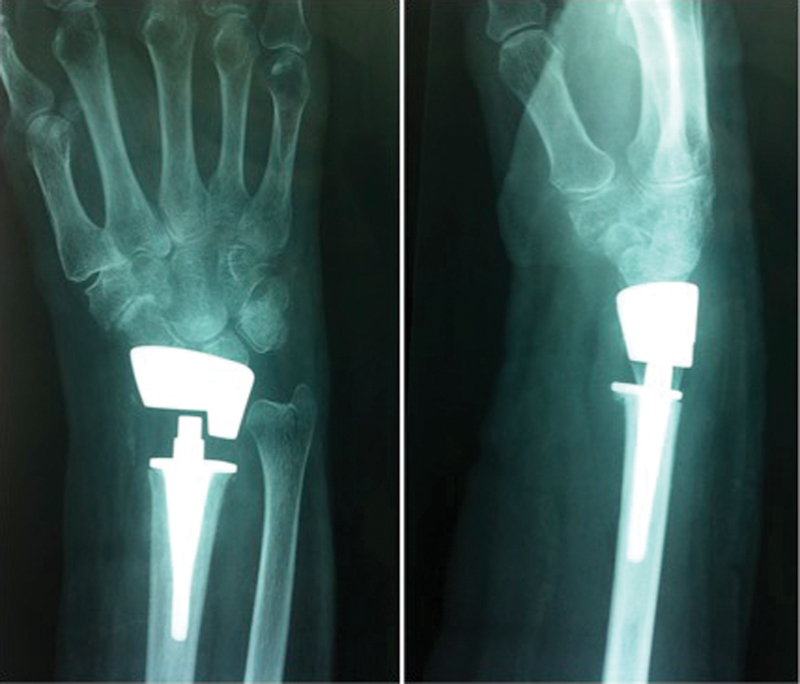
Example of wrist hemiarthroplasty (Sophia, Biotech France).
Surgical Technique8
The preoperative planning included posteroanterior (PA) and lateral view X-ray images as well as computed tomography (CT). The procedure (Fig. 2) was performed under regional anesthesia (axillary block). The fracture was approached through a 5–6-cm dorsal incision with exposure of the distal radius though the interval between the extensor digitorum communis and the extensor pollicis longus. A subperiosteal dissection was performed as described by Roux8 so that the periosteum was in direct contact with the implant at the completion of the procedure to help maintain stability. The posterior interosseous nerve was coagulated and resected. Once all of the free epiphyseal fragments were removed, the radius was resected proximally to create a negative ulnar variance, using a cutting guide positioned with a stem that sat on the distal portion of the ulnar head. Resection was performed using an oscillating saw. Rasps of increasing size were then used to enlarge the medullary canal, followed by insertion of trial implants under radiographic control. The stainless steel head of the implant comes in four sizes, whereas the metaphyseal polyethylene insert is available in three thicknesses. Ten degrees of longitudinal rotation is possible to reduce the risk of loosening. After the correct trial implant size was determined, the definitive implant was cemented into the radius. Patients were immobilized in a below-elbow cast for 3 weeks to allow soft tissue healing, followed by a home program for 3 weeks, then 15 formal physical therapy sessions.
Fig. 2.
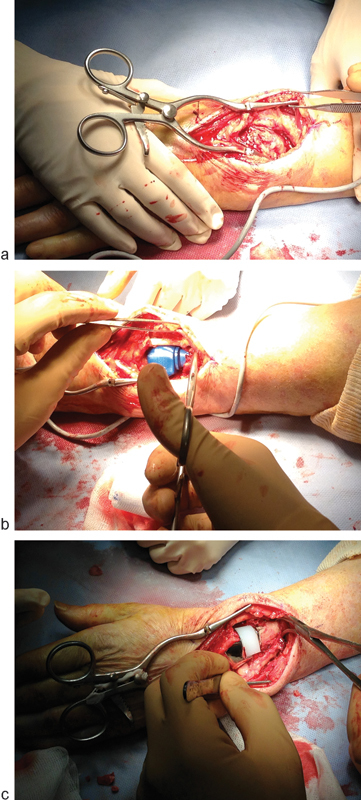
(a–c) Perioperative pictures of surgical technique.
Radiographic Examination and Clinical Evaluation
An independent surgeon reviewed all of the patients at the final follow-up. Wrist motion and grip strength using a a Jamar dynamometer were recorded. Subjective and objective data were graded using the Herzberg scoring system,9 (Fig. 3), DASH (Disabilities of the Arm, Shoulder and Hand) score,10 VAS (visual analog scale), and patient satisfaction form. X-ray images were taken to look for prosthetic loosening.
Fig. 3.
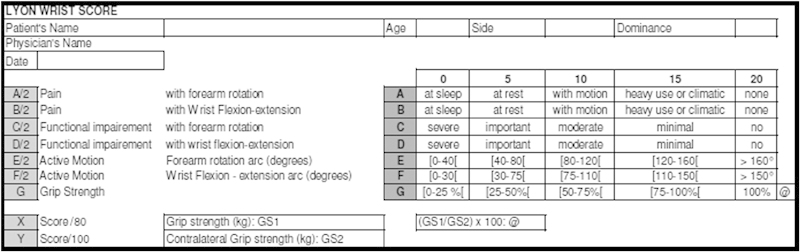
The Herzberg scoring system.
Results
The mean follow-up was 25 months (range 17–36 months). All eight patients (100%) were female. The Mean age of patients was 80 years old at the time of the injury (range: 74–85 years). The dominant side was involved in five of the cases. All of the fractures were AO type C2, with metaphyseal and epiphyseal comminution and without distal ulnar fractures (except ulnar styloid fracture). The mean delay between injury and surgery was 2 days (range 1–3 days). The average operating time was 66 minutes (range 55–85 minutes). The patients were discharged at an average of 5 days (range 2–8 days). No explantation of this prosthesis occurred at the time of follow-up (implant survival: 100%).
The clinical results are summarized in Table 1.
Table 1. Clinical data.
| Study patients | 8 |
| Average age (years) | 80 |
| Gender: M/F | 0/8 |
| Fracture side: Left/Right | 3/5 |
| Dominant side: Left/Right | 3/5 |
| Average follow-up (months) | 25 |
| Motion (degrees): | |
| Flexion | 46 (SD, 4.18) |
| Extension | 44 (SD, 4.18) |
| Pronation | 85 (SD, 7.58) |
| Supination | 75 (SD, 5) |
| Radial | 20 (SD, 5) |
| Ulnar | 25 (SD, 6) |
| Grip | 92 (SD, 9.84) |
| Herzberg score (%) | 78,6% |
| DASH score (/100) | 18 (SD, 6.22) |
| VAS | 2 (SD, 1.5) |
Abbreviations: DASH, disabilities of the arm, shoulder and hand ; F, female ; M, male ; SD, standard deviation; VAS, visual analog scale.
The patients were able to come back home and return to activities of daily living (ADLs) on average in 3 weeks (range 0.5–5 weeks).
No patients were disappointed with this surgery according to a patient satisfaction form (Fig. 4).
Fig. 4.

(a–g) Displaced distal radius fractures: Example radiological of the hemiarthroplasty and clinical results at 12 months: Flexion-extension (left wrist).
Only one case of periprosthetic calcification was demonstrated on X-ray. There were no cases of implant loosening, infection, complex regional pain syndrome (CRPS), or dislocation.
Discussion
Treatment of complex distal radius fractures in elderly patients remains controversial.11 12 Despite numerous plate designs, an anatomical reduction is often unobtainable in elderly patients with complex articular fractures.13 14 An advantage to the use of a hemiarthroplasty is the rapid return to autonomous function and ADLs, which was typically 3 weeks. Roux obtained similar clinical results to ours in six patients who were treated with a hemiarthroplasty8 (Table 2). However, our functional results are slightly better with a QuickDASH at 18 versus 27 for Roux.8 His cases, however, included patients with acute trauma as well as tumors and distal radius malunions: four comminuted and osteoporotic fractures in elderly patients, one malunion in an elderly patient, and one pathological fracture of epiphyseal destructive tumor in a young man.
Table 2. Results of two Sophia Biotech hemiarthroplasty series.
| Series | Our series | Roux 2008 |
|---|---|---|
| Mean age (years) | 80 | 73 |
| Follow-up (months) | 25 | 27 |
| Mean flexion-extension (°) | 89 | 90 |
| Mean pro-supination (°) | 160 | 110 |
| Grip (kg f) | 18 (90%) | 16 (80%) |
| DASH score | 18.2 | 27.2 |
| Complications | 1 periprosthetic calcification | 1 CRPS |
Abreviations: CRPS, complex regional pain syndrome; DASH, disabilities of the arm, shoulder and hand; F, female; M, male.
We utterly agree with Roux on the fact that despite encouraging results, the low follow-up of this technique and the limited number of cases lead us to be cautious and use this procedure only in the indications described previously.
Footnotes
Conflict of Interest None
References
- 1.Rozental T D, Makhni E C, Day C S, Bouxsein M L. Improving evaluation and treatment for osteoporosis following distal radial fractures. A prospective randomized intervention. J Bone Joint Surg Am. 2008;90(5):953–961. doi: 10.2106/JBJS.G.01121. [DOI] [PubMed] [Google Scholar]
- 2.Glickel S Z, Catalano L W, Raia F J, Barron O A, Grabow R, Chia B. Long-term outcomes of closed reduction and percutaneous pinning for the treatment of distal radius fractures. J Hand Surg Am. 2008;33(10):1700–1705. doi: 10.1016/j.jhsa.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Zenke Y, Sakai A, Oshige T, Moritani S, Nakamura T. The effect of an associated ulnar styloid fracture on the outcome after fixation of a fracture of the distal radius. J Bone Joint Surg Br. 2009;91(1):102–107. doi: 10.1302/0301-620X.91B1.21026. [DOI] [PubMed] [Google Scholar]
- 4.Richard M J, Katolik L I, Hanel D P, Wartinbee D A, Ruch D S. Distraction plating for the treatment of highly comminuted distal radius fractures in elderly patients. J Hand Surg Am. 2012;37(5):948–956. doi: 10.1016/j.jhsa.2012.02.034. [DOI] [PubMed] [Google Scholar]
- 5.Saffar P Mazodier F Werther J R Fractures in the elderly patient: is it necessary to operate on patients over 75 years old? [in French] Rev Chir Orthop Repar Appar Mot 200187130–132. [Google Scholar]
- 6.Chen N C, Jupiter J B. Management of distal radial fractures. J Bone Joint Surg Am. 2007;89(9):2051–2062. doi: 10.2106/JBJS.G.00020. [DOI] [PubMed] [Google Scholar]
- 7.Charissoux J-L Mabit C Fourastier J et al. Comminuted intra-articular fractures of the distal humerus in elderly patients [in French] Rev Chir Orthop Repar Appar Mot 200894(4, Suppl):S36–S62. [DOI] [PubMed] [Google Scholar]
- 8.Roux J L. Replacement and resurfacing prosthesis of the distal radius: a new therapeutic concept [in French] Chir Main. 2009;28(1):10–17. doi: 10.1016/j.main.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 9.Herzberg G, Dumontier C. Symposium: fresh fractures of the distal radius in the adult [in French] Rev Chir Orthop Repar Appar Mot. 2000;86 01:1585–1588. [Google Scholar]
- 10.Dubert T, Voche P, Dumontier C, Dinh A. The DASH questionnaire. French adaptation of an international evaluation tool [in French] Chir Main. 2001;20(4):294–302. doi: 10.1016/s1297-3203(01)00049-x. [DOI] [PubMed] [Google Scholar]
- 11.Gehrmann S V, Windolf J, Kaufmann R A. Distal radius fracture management in elderly patients: a literature review. J Hand Surg Am. 2008;33(3):421–429. doi: 10.1016/j.jhsa.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 12.Schneppendahl J, Windolf J, Kaufmann R A. Distal radius fractures: current concepts. J Hand Surg Am. 2012;37(8):1718–1725. doi: 10.1016/j.jhsa.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 13.Hanel D P, Lu T S, Weil W M. Bridge plating of distal radius fractures: the Harborview method. Clin Orthop Relat Res. 2006;445(445):91–99. doi: 10.1097/01.blo.0000205885.58458.f9. [DOI] [PubMed] [Google Scholar]
- 14.Ginn T A Ruch D S Yang C C Hanel D P Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. Surgical technique J Bone Joint Surg Am 200688(Suppl 1 Pt 1):29–36. [DOI] [PubMed] [Google Scholar]


