Abstract
Background Chronic, dynamic bidirectional instability in the distal radioulnar joint (DRUJ) is diagnosed clinically, based on the patient's complaints and the finding of abnormal laxity in the vicinity of the distal ulna. In cases where malunion is ruled out or treated and there are no signs of osteoarthritis, stabilization of the DRUJ may offer relief. To this end, several different techniques have been investigated over the past 90 years.
Materials and Methods In this article we outline the procedure for a new technique using a tendon graft to reinforce the distal edge of the interosseous membrane.
Description of Technique A percutaneous technique is used to harvest the palmaris longus tendon and to create a tunnel, just proximal to the sigmoid notch, through the ulna and radius in an oblique direction. By overdrilling the radial cortex, the knotted tendon can be pulled through the radius and ulna and the knot blocked at the second radial cortex, creating a strong connection between the radius and ulna at the site of the distal oblique bundle (DOB). The tendon is fixed in the ulna with a small interference screw in full supination, preventing subluxation of the ulna out of the sigmoid notch during rotation.
Results Fourteen patients were treated with this novel technique between 2011 and October 2013. The QuickDASH score at 25 months postoperatively (range 16–38 months) showed an improvement of 32 points. Similarly, an improvement of 33 points (67–34 months) was found on the PRWHE. Only one recurrence of chronic, dynamic bidirectional instability in the DRUJ was observed.
Conclusion This simple percutaneous tenodesis technique between radius and ulna at the position of the distal edge of the interosseous membrane shows promise in terms of both restoring stability and relieving complaints related to chronic subluxation in the DRUJ.
Keywords: distal radioulnar joint, distal oblique bundle, instability, posttraumatic wrist disorder
Instability of the distal radioulnar joint (DRUJ) can be highly disabling. Complaints include persistent discomfort on the ulnar side of the wrist, a painful click during rotation, and sharp pain during loaded (forceful) supination (e.g., lifting an object). This complex of symptoms suggests palmar subluxation of the ulnar head relative to the radius, due to instability of the DRUJ. In cases where the triangular fibrocartilage complex (TFCC) is ruptured and the extrinsic stabilizers are insufficient, the relation between distal radius and ulna becomes floppy and both palmar and dorsal subluxation can occur (bidirectional instability). Although the complaints were well described by Darrach in 1932 in his comments on the paper of Eliason, describing one of the first stabilization techniques, nowadays quite a considerable number of orthopedic trauma surgeons remain unaware of this diagnosis.1
In the absence of malunion of the distal radius with misalignment in the DRUJ, this dynamic instability can be attributed to inadequate stabilization by the soft tissues. While the diameter of the (more or less flat) sigmoid notch is larger than that of the distal ulna, as required for translation in two directions during rotation, soft tissue stabilization is needed to create a mobile, self-centering joint.2
Joint-stabilizing soft tissues can be divided into intrinsic and extrinsic stabilizers. The intrinsic stabilizing structure (the TFCC) is considered the primary stabilizer, although there is no hard evidence for this assumption.3 Moreover, the TFCC seems not absolutely essential for DRUJ stability. Gofton et al reported on a stable DRUJ due to intact extrinsic stabilizers even after complete division of the TFCC.4 It is known that the TFCC can be damaged after sustaining a fracture of the distal radius, based on initial fracture displacement. Mohanti et al showed that46% of patients with a displaced distal radius fracture were diagnosed by arthrography with a rupture of the TFCC.5 However, it is not clear how many of these patients sustained a central defect only, with stability unaffected. Richards et al arthroscopically identified radial-side ruptures of the TFCC in 39% of distal radius fractures, creating residual laxity in the DRUJ.6 Such a high proportion of TFCC injuries in patients with a distal radius fracture is not in line with clinical experience, as clinically significant instability is not seen in these large numbers. Since a considerable number of these patients do have a TFCC tear, there is a discrepancy between the laxity observed by surgeons during wrist surgery and patients' complaints in the long term. Given that pain-free functionality of the wrist seems to be possible in the absence of an intrinsic stabilizer such as the TFCC, extrinsic stabilizers may be more important than previously thought. Okada's recent study links the absence of a thickened portion in the distal interosseous membrane, known as the distal oblique bundle (DOB), to complaints of instability in the DRUJ.7 Since this DOB is not universal, its presence may explain why not all patients with a ruptured TFCC complain of instability.8
Therefore, we aimed to develop an effective treatment for patients with symptomatic posttraumatic, bidirectional dynamic instability of the DRUJ using a simple tenodesis technique that mimics a DOB. Since our center is a tertiary referral center for DRUJ injuries, a large number of patients with this fairly uncommon injury were presented to us over the last few years. This is the first study to describe the results of this procedure.
Patients and Methods
Between January 1, 2011, and October 31, 2013, all patients complaining of bidirectional DRUJ instability (a combination of palmar subluxation in supination and dorsal subluxation in pronation) referred to the department of Traumatology of the Maastricht University Medical Center were prospectively included in this observational study and treated using the DOB reinforcement technique described in subsequent paragraphs. In case of a simultaneous malunion of the radius (both dorsal tilt and radial shift), only patients with persistent instability after correction of the malunion were included. Functional outcomes were determined using the Disabilities of the Arm, Shoulder, and Hand (QuickDASH) score and the Patient-Rated Wrist/Hand Evaluation (PRWHE) prior to treatment and at follow-up.
Surgical Technique
As the intention is to mimic the DOB, the tendon should be facing in an oblique direction at the distal edge of the interosseous membrane and centered in the ulna, and the radius, with the forearm in a neutral position. To be sure the tension of the construct is enough to prevent palmar subluxation of the ulnar head, the tendon is tightened in supination.The surgical procedure is as follows. First, at least 10 cm (4 inches) of the tendon of the palmaris longus (or if this is absent, the flexor carpi radialis tendon) is harvested using a percutaneous technique and a tendon stripper of an appropriate size.
The tendon is knotted once (or in the case of a small tendon, twice) in the middle. At least 5 cm of tendon should be available on one side to pull through the radius and ulna. The knot is marked with a small radiopaque metal clip to signal its position in the radius after it is pulled through, using the image intensifier.
The arm is flexed at the elbow and the forearm positioned upwards. From a neutral position, the head of the ulna is squeezed to ensure that it is centered in the sigmoid notch. Using a small stab incision, the ulna is temporarily fixed to the radius ∼15 cm from the DRUJ with a 2-mm Kirschner wire (K-wire).
A small, straight incision is made on the ulnar side 3 cm from the ulnar styloid, where the tunnel should start. A small area of bare ulna bone can be created to facilitate drilling through the center of the ulna. A second 1-mm K-wire, part of a cannulated drill system (Arthrex Inc., Naples, FL, USA), is then drilled through both cortices of the ulna into the radius in the previously marked direction. The position of the wire should be correct in both anteroposterior (AP) and lateral direction, as this determines the position of the tendon at the end of the procedure (Fig. 1). To this end, a target device may be helpful.
Fig. 1.
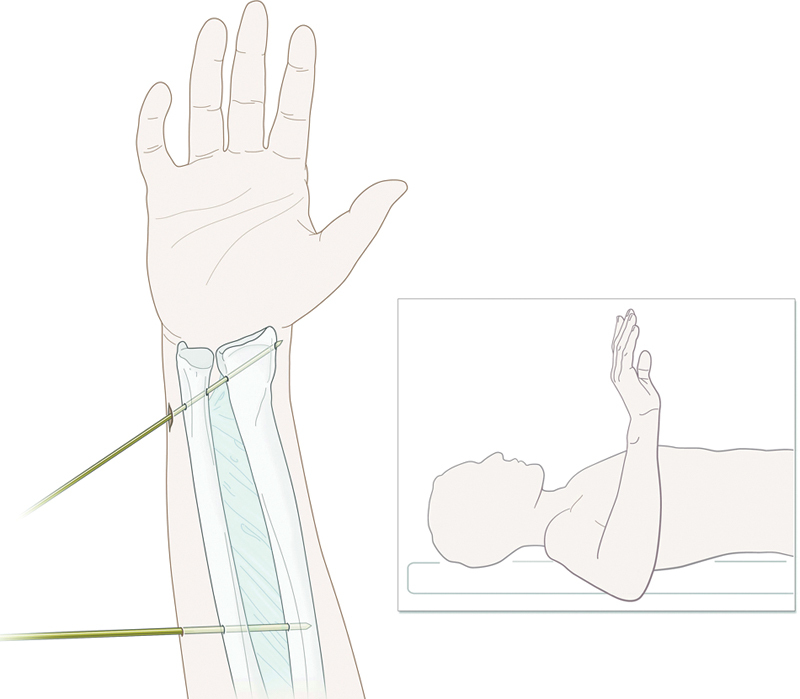
K-wire fixation between radius and ulna in neutral position. A 1-mm K-wire is drilled through the center of the radius and ulna in an oblique direction, just cranial of the sigmoid notch.
When the position of the wire is correct in both directions, the radial side of the cortex of the radius can be perforated. It should be noted that this may cause damage to the extensor pollicis brevis tendon, the abductor pollicis longus tendon, and the superficial radial nerve; therefore, a small incision should be made as soon as it is clear where the K-wire is expected. The wire should be made to protrude radially ∼5 cm, being careful not to damage any oft tissue.
A 2.7-mm cannulated drill (or 3.0-mm for thick tendons) is then used to create a tunnel through the ulna and radius over the K-wire, starting from the ulnar side. From the radial side, the tunnel is overdrilled up to 5 mm, using the cannulated drill bits available in 0.5-mm increments. The exact amount depends on the size of the knot, which has to pass the first cortex of the radius but not the second, to avoid the knot slipping out of the radius. At this point the use of the image intensifier is recommended (Fig. 2).
Fig. 2.
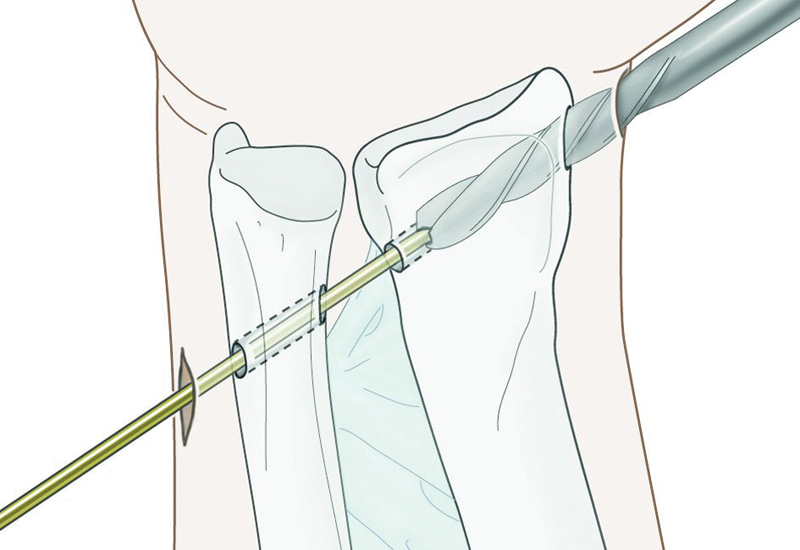
The ulna and radius are drilled with a 2.7-mm cannulated drill. Then, the radial cortex is overdrilled in retrograde fashion with a 5-mm cannulated drill up to the second radial cortex.
Next, a suture is attached to the slip of the tendon using Kessler stitches. The end of the tendon must be prevented from thickening, since it will need to pass through the tunnel in both the radius and ulna. A simple thread around the knot—a sort of “rescue wire”—makes it possible to withdraw the tendon in case of obstruction when passing through the radius. This thread remains on the outside at the radial side.
From the ulnar side, the thread of the tendon is grasped using a suture retriever. The tendon is then pulled through the radius and ulna with controlled force, with the knot lodging inside the radius near the second cortex (Fig. 3). The correct position of the radiopaque clip in the knot should be identified using the image intensifier (Fig. 4).
Fig. 3.
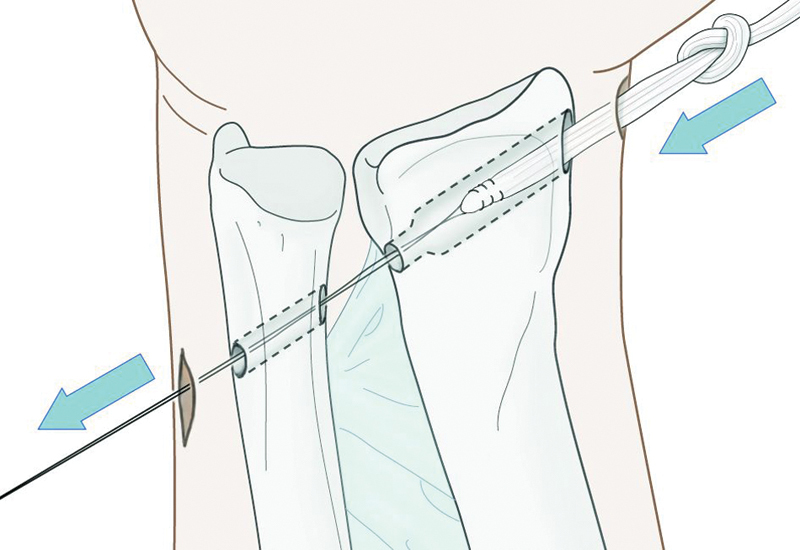
The palmaris tendon, with central knot, is pulled through the radius and ulna. The knot prevents the tendon from slipping out of the radius.
Fig. 4.

While the knot is being marked with a small vessel clip, its exact position can be checked using the image intensifier.
Next, the proximal K-wire is removed and the forearm rotated and brought into full supination. In this position, the tendon is tightened, and a 3 mm × 8 mm vented polyether ether ketone (PEEK) Tenodesis Screw with handled inserter (Bio-Tenodesis Screw System, Arthrex Inc., Naples, FL, USA) is inserted in the ulna (Fig. 5). This will secure the tendon in the ulna while also maintaining a certain tension in the system. The resulting decrease in distance between the radius and ulna in the sigmoid notch can be seen in the postoperative X-ray in Fig. 6.
Fig. 5.
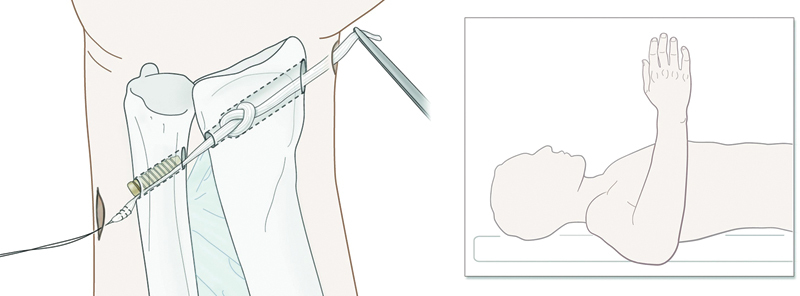
After removal of the radioulnar K-wire, the hand is rotated in full supination and the tendon fixed in the ulna using a 3 × 8 mm PEEK Tenodesis screw.
Fig. 6.

Note the decrease in radioulnar distance after fixation of the tendon transplant between radius and ulna.
An alternative fixation technique is to use a G2 Mitek anchor (DePuy Synthes, Inc., West Chester, PA, USA); however, the knot of the tendon on the ulnar side may cause the patient pain when the forearm is in working position.
If normal rotation is possible and the tendon is deemed to be in the correct position, the “rescue wire” can be removed and the protruding parts of the tendon cut on both sides, flush to the bone. The small stab incisions are then closed and the patient is given an above-elbow cast in full supination for 4 weeks. After removal of the cast, the patient starts to work on achieving full rotation.
In the case of concomitant malunion, the malunion is corrected first. Only when this does not increase stability is the tenodesis performed using the surgical procedure just described.
Results
Fourteen patients with complaints of bidirectional DRUJ instability were treated using the DOB reinforcement technique. Preoperatively, all patients had abnormal and painful laxity in the DRUJ in both dorsal and palmar directions, at least in neutral position, but to some extent also in maximum pron- and supination. Two out of 14 patients had a significant impairment of rotation of more than 30° (one in pronation only, one in both pronation and supination). All had chronic discomfort ulnarly and a sharp pain in loaded supination.
Table 1 shows the patient demographics and preoperative findings of physical examination and magnetic resonance imaging (MRI) and/or computed tomography (CT). Mean age was 34.4 years (range 17–58), and 72% of the patients were female.
Table 1. Patient demographics and preoperative findings of physical examination and MRI and/or CT imaging.
| Patient | Trauma mechanism | Type of injury | Injury-therapy interval | Preop MRI findings | Preop CT findings | Pronation/supination pre-op | DRUJ malalignment? |
|---|---|---|---|---|---|---|---|
| ♀ 23y | Instability after fall in snow | # distal radius 10 years earlier | 6 months | TFC rupture | Flat sigmoid notch | No impairment | No |
| ♂ 19y | Fall from bike | # distal radius and # scaphoid (waist) | 28 months | TFC attached to avulsed styloid | Flat sigmoid notch | No impairment | No |
| ♂ 32y | Fall from chair | Malunited distal radius # with DRUJ instability | 16 months | No MRI performed | Normal sigmoid notch | 80/60 | Yes |
| ♀ 27y | Direct blow on ulna (assault) | Ulna fracture treated with plate | 21 months | TFC rupture | No CT performed | No impairment | No |
| ♀ 30y | Simple fall | # distal radius | 11 months | TFC rupture | Volar osteophyte ulna | 80/45 | No |
| ♂ 26y | Fall from jet ski | Open Galeazzi fracture | 23 months | No MRI performed | Normal sigmoid notch | No impairment | No (after correction of Galeazzi fracture) |
| ♀ 45y | Fall on ice | # distal radius with congenital bowing of the radius | 10 months | No MRI performed | No CT performed | No impairment | No |
| ♀ 25y | Minor trauma | No fracture | 4 months | No MRI performed | No CT performed | No impairment | No |
| ♂ 58y | Stumble | #distal radius with ulnar styloid # | 42 months | TFC rupture | Normal sigmoid notch | No impairment | No |
| ♀17y | Fall from scooter | # distal radius with # base ulnar styloid | 11 months | TFC rupture | No CT performed | No impairment | No |
| ♀50y | Simple fall | # distal radius with fleck fracture ulnar styloid | 12 months | TFC rupture | No CT performed | 50/50 | Yes |
| ♀18y | Fall from stairs | Ulnar pain, no fracture | 5 months | No MRI performed | Flat sigmoid notch | No impairment | No |
| ♀ 55y | Simple fall | # distal radius | 15 months | No MRI performed | Normal sigmoid notch | 80/60 | Yes |
| ♀ 57y | Simple fall | # distal radius | 48 months | TFC rupture | Normal sigmoid notch | No impairment | No |
Table 2 shows the outcomes after surgery.
Table 2. Description of the outcome of the DOB reinforcement technique in the first 14 patients.
| Patient | Type of injury | Pronation/supination postop |
Surgical procedure | Follow-up | QuickDASH preop/follow-up | PRWHE preop/follow-up | Recurrent instability | Remarks |
|---|---|---|---|---|---|---|---|---|
| ♀ 23y | # distal radius 10 years earlier | No impairment | DOBR | 38 months | 71/48 | 56/54 | No | Ulnar irritation due to knot (Mitekanchor technique) |
| ♂ 19y | # distal radius and # scaphoid (waist) | 50/65 | DOBR | 34 months | 63/16 | 86/21 | No | Constrained ulna prosthesis after 6 months due to progressive osteoarthritis |
| ♂ 32y | Malunited distal radius # with DRUJ instability | No impairment | DOBR after reconstruction of radius | 33 months | 55/25 | 62/44 | No | Plate removal after healing of osteotomy |
| ♀ 27y | Ulna fracture treated with plate | No impairment | DOBR | 32 months | 84/68 | 93/56 | No | Borderline patient, fibromyalgia |
| ♀ 30y | # distal radius | 80/60 | DOBR | 31 months | 59/25 | 40/20 | No | Initial Adams/Berger procedure |
| ♂ 26y | Open Galeazzi fracture | No impairment | DOBR | 27 months | 39/18 | 70/48 | No | Radial shaft plate removed |
| ♀ 45y | # distal radius with congenital bowing of the radius | No impairment | DOBR | 26 months | 55/30 | 72/25 | No | Hyperlaxity syndrome, fixed with FiberWire |
| ♀ 25y | No fracture | No impairment | DOBR | 25 months | 68/9 | 64/0 | No | |
| ♂ 58y | #distal radius with ulnar styloid # | No impairment | DOBR | 21 months | 77/52 | 72/52 | No | Initial styloid fixation |
| ♀17y | # distal radius with # base ulnar styloid | No impairment | DOBR | 21 months | 46/2 | 59/16 | No | |
| ♀50y | # distal radius with fleck fracture ulnar styloid | No impairment | DOBR after reconstruction radius | 16 months |
63/16 | 85/22 | No | |
| ♀18y | Ulnar pain, no fracture | No impairment | DOBR | 16 months | 61/2 | 76/11 | No | |
| ♀ 55y | # distal radius | No impairment | DOBR after reconstruction of radius | 16 months | 34/34 | 40/23 | No | 30° lack of supination of EPL rupture due to plate radius |
| ♀ 57y | # distal radius | No impairment | DOBR | 20 months |
89/69 | 66/79 | Yes | Initial Adams/Berger procedure |
Abbreviation: DOBR, distal oblique bundle reinforcement.
A QuickDASH and a PRWHE were administered prior to surgery and at follow-up (mean follow-up 25 months, range 16–38).The QuickDASH showed an improvement of 32.1 points (mean preop 61.7–mean postop 29.6), the PRWHE 33.6 points (mean preop 67.2–mean postop 33.6). (see Table 2)
Since we performed a procedure to reinforce extrinsic stabilizers, no additional arthroscopies were done. All MRIs showed a distal rupture of the TFCC.
In all cases where a corrective osteotomy of the radius was performed prior to DOB reinforcement, no malalignment persisted and the normal relation between the sigmoid notch and the distal ulna was restored. No sigmoid notch osseous reconstructions were performed.
Postoperatively, 13 out of 14 patients were no longer experiencing the acute, sharp pain of subluxation. In one patient with ongoing osteoarthritis of the DRUJ, the DOB reinforcement was eventually replaced by a constrained distal ulna prosthesis. During placement of the prosthesis, the tendon was found to be still intact and firmly fixed to the bone. One patient sustained a fracture of the ulna shaft after several attempts to fix the ulna to the radius in neutral position. The fracture healed after 4 weeks of cast immobilization. One patient had some persistent numbness in the area of the dorsal branch of the radial nerve. Finally, in only one patient did the reconstruction fail outright. As an Adams/Berger procedure was also unsuccessful, placement of a distal prosthesis was indicated.
Discussion
Instability of the DRUJ is not new. The first description of how to fix the ulna to the radius to stabilize it was published by Lowman in 1930, using a fascia lata strip through the radius and around the ulna.1 Many variations on this technique have been described since. All make use of a hole through the radius1 9 and a loop around the distal shaft, fixing the ulna in place and allowing free rotation. Liebolt fixed the ulna to the radius, but not through the center of the distal oblique bundle (DOB).9 Given that 40% of people have a ligament between the radius and ulna as an extension of the distal part of the interosseous membrane, it seems only logical to mimic this configuration.7 Riggenbach's study on cadavers showed that a DOB reconstruction can restore stability to the DRUJ, using a technique as sound as that described by Adams.10 11 Further, the ultrasound study by Okada et al showed that the absence of a DOB was correlated with more clinical complaints of instability in a small group of patients.8
It therefore seems to make sense to use the DOB to promote stability in the DRUJ. The minimally invasive technique we describe appears to offer a suitable and simple means of preventing subluxation of the ulna out of the sigmoid notch during rotation. It is this subluxation—especially in loaded supination, where the ulna “wants” to escape from the notch in a palmar direction—that causes the characteristic complaints. The construct mainly prevents the palmar subluxation of the ulna and probably the less symptomatic dorsal subluxation of the ulnar head. So in cases where a slight dorsal tilt of the radius is present, the palmar subluxation is the main cause of complaints, which are resolved with this technique. Various tests have been described and validated to investigate clinical instability.12 Dynamic instability, however, is the key for surgery, and the validity of most tests in this area is debatable. We use our own modification, which we call the “free rotation test.” In this test, the forearm is in loaded position, the elbow on the table, and the ulna resting on the outstretched fingers of the investigator. When, in shaking position, the hand is rotated, the investigator feels a “clunk” when the ulna and radius separate in the DRUJ. The patient recognizes this as the characteristic acute pain experienced in daily life. Indeed, a total rotation block can occur in supination. By reinforcing one of the extrinsic stabilizers of the DRUJ, the importance of the TFCC is minimized. For that reason we do not extensively focus on TFCC injuries prior to surgery.
The technique described by Adams and Berger—using a tendon to create a new TFCC configuration—is suggested to be an anatomic solution for instability.11 Our technique, which mimics the normal DOB structure, in fact does the same. DOB reinforcement is reserved for patients with clinical symptoms of instability, laxity in the DRUJ (which is greater than on the unaffected side and bidirectional due to a complete tear of TFCC), and no malunion or arthritis in the joint.
Provided that patients are selected carefully, this simple percutaneous technique seems to be a promising means of treating chronic instability in this important joint. It offers a good alternative to more invasive procedures and an elegant means of preserving the surrounding soft tissue, especially those tissues that support the residual stability of the joint. Further investigation would be worthwhile, particularly in the form of randomized prospective studies and comparative studies including other stabilizing procedures.
Footnotes
Conflict of Interest None
References
- 1.Eliason E L. An operation for recurrent inferior radioulnar dislocation. Ann Surg. 1932;96(1):27–35. doi: 10.1097/00000658-193207000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Szabo R M. Distal radioulnar joint instability. J Bone Joint Surg Am. 2006;88(4):884–894. doi: 10.2106/00004623-200604000-00027. [DOI] [PubMed] [Google Scholar]
- 3.Zimmerman R M, Jupiter J B. Instability of the distal radioulnar joint. J Hand Surg Eur Vol. 2014;39(7):727–738. doi: 10.1177/1753193414527052. [DOI] [PubMed] [Google Scholar]
- 4.Gofton W T, Gordon K D, Dunning C E, Johnson J A, King G J. Soft-tissue stabilizers of the distal radioulnar joint: an in vitro kinematic study. J Hand Surg Am. 2004;29(3):423–431. doi: 10.1016/j.jhsa.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 5.Mohanti R C, Kar N. Study of triangular fibrocartilage of the wrist joint in Colles' fracture. Injury. 1980;11(4):321–324. doi: 10.1016/0020-1383(80)90105-9. [DOI] [PubMed] [Google Scholar]
- 6.Richards R S, Bennett J D, Roth J H, Milne K Jr. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am. 1997;22(5):772–776. doi: 10.1016/S0363-5023(97)80068-8. [DOI] [PubMed] [Google Scholar]
- 7.Okada K, Moritomo H, Miyake J. et al. Morphological evaluation of the distal interosseous membrane using ultrasound. Eur J Orthop Surg Traumatol. 2014;24(7):1095–1100. doi: 10.1007/s00590-013-1388-6. [DOI] [PubMed] [Google Scholar]
- 8.Noda K, Goto A, Murase T, Sugamoto K, Yoshikawa H, Moritomo H. Interosseous membrane of the forearm: an anatomical study of ligament attachment locations. J Hand Surg Am. 2009;34(3):415–422. doi: 10.1016/j.jhsa.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 9.Green D P, ed. Operative Hand Surgery, 3rd ed New York, NY: Churchill Livingstone; 19931003 [Google Scholar]
- 10.Riggenbach M D, Conrad B P, Wright T W, Dell P C. Distal oblique bundle reconstruction and distal radioulnar joint instability. J Wrist Surg. 2013;2(4):330–336. doi: 10.1055/s-0033-1358546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adams B D, Berger R A. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg Am. 2002;27(2):243–251. doi: 10.1053/jhsu.2002.31731. [DOI] [PubMed] [Google Scholar]
- 12.Wijffels M, Brink P, Schipper I. Clinical and non-clinical aspects of distal radioulnar joint instability. Open Orthop J. 2012;6:204–210. doi: 10.2174/1874325001206010204. [DOI] [PMC free article] [PubMed] [Google Scholar]


