Abstract
Purpose The purpose of our study was to examine the anatomy of the distal ulna and identify an interval that would be amenable to plating and would not cause impingement during wrist rotation nor irritation to the extensor carpi ulnaris (ECU) tendon.
Methods Six cadaveric forearms were dissected and the arc of the articular surface of the distal ulna was measured. The distal ulna was divided up as a clock face, with the ulnar styloid being assigned the 12 o'clock position, and the location of the ECU was identified accordingly. The distance from the ulnar styloid to where the dorsal sensory ulnar nerve crosses from volar to dorsal was also measured. Based on these measurements a safe zone was defined.
Results A safe zone was identified between the 12 and 2 o'clock position on the right wrist, and between the 10 and 12 o'clock on the left wrist. The dorsal sensory branch of the ulnar nerve crossed from volar to dorsal position at a variable location near the ulnar styloid. Two commercially available plates were utilized and could be placed in our designated interval and did not cause impingement when the forearm was rotated fully.
Conclusion Our study demonstrates a location for plating of the distal ulna that avoids impingement during forearm rotation and that is outside of the footprint of the ECU subsheath.
Clinical Relevance Plating of the distal ulna may be necessary with distal ulna fracture, and although plate placement may be dictated by the fracture pattern, it is important to understand the implications of plate placement. Although the ideal plate may not be possible because of comminution, the patient can be educated in regards to potential for tendon irritation, loss of motion, or need for hardware removal.
Keywords: distal ulna fracture, distal radius fracture, plating, safe zone, fixation, dorsal sensory branch of ulnar nerve
Fractures of the distal ulna usually occur in association with distal radius fractures.1 Injuries to the distal ulna can lead to derangement of the distal radioulnar joint (DRUJ), subsequently resulting in pain from incongruity or ulnocarpal impaction, limitation of forearm rotation due to scarring, and weakness secondary to instability of the joint under load.2 3 Unstable and displaced fractures require open reduction and surgical stabilization, usually with a mini-fragment plate to avoid derangement of the load-bearing surface.4
The anatomy of the distal ulna poses a challenge to surgeons. The distal ulna has been described to have 270 degrees of articular surface.5 Reconstruction of the articular surface is important for the articulation with the sigmoid notch of the radius to help prevent later DRUJ dysfunction. Surgeons must also be mindful of the soft tissue structures in the region, especially given the subcutaneous nature of the ulna. The extensor carpi ulnaris (ECU) tendon along with the dorsal sensory branch of the ulnar nerve (DSBUN) lie within close proximity in this area. The DSBUN has been described to emerge at the dorsomedial border of the FCU at a mean distance of 5 cm from the proximal edge of the pisiform and runs subcutaneously, crossing the ECU a fingerbreadth distal to the ulnar head.5 6
There are plates specifically made for periarticular distal ulna fractures and fractures of the ulnar head. The anatomy of the distal ulna with its styloid, unique articular surface, and various soft tissue components can make plating difficult. For example, a plate placed too far dorsally may cause irritation to the ECU tendon. In contrast, a plate placed volarly and distal could cause impingement if placed too radially. The purpose of this study, utilizing cadaver forearms, was to define a “safe zone” for plate placement on the distal ulna with minimal impact on forearm rotation and tendon irritation. We then tested two commercially available plates for the distal ulna to see whether they would fit in our defined safe zones and to verify that they would not cause impingement during forearm rotation (Fig. 1). Both plates are specifically desiged for the distal ulna and represent different options depending on the fracture pattern. One plate (2.0-mm LCP Distal Ulna Plate, Synthes, West Chester, PA, USA) is designed for fracture patterns involving the ulnar styloid. The pointed hooks are able to grip the ulnar styloid with locking fixation in the head to avoid penetration into the DRUJ. The plate is 46 mm long and 5 mm wide. The other plate used in this study (Acumed Distal Ulna Plate, Hillsboro, OR, USA) is designed more for fractures of the ulnar head and neck and is not designed to extend as distally as the other plate used in the study. The five-hole plate utilized for this study is 66 mm in length, 44 mm wide at the distal aspect, and 8 mm wide at the proximal aspect.
Fig. 1.

Plates designed specifically for fractures of the distal ulna. From left, distal ulna hook plate (Synthes) and left and right distal ulna locking plate (Acumed).
Methods
The forearms of six fresh frozen cadavers were exposed through the interval between the flexor carpi ulnaris (FCU) and extensor carpi ulnaris (ECU) tendons. The location of the DSBUN was identified with relation to the ulnar styloid (Fig. 2). The distance from the styloid from where the nerve went from the volar to dorsal aspect of the wrist was measured from the tip of the ulnar styloid. The wrist was disarticulated to visualize the DRUJ at its distal surface. The ulnar styloid was designated as the twelve o'clock position and the ECU tendon was mapped on the “clock face.” The margins of the nonarticular portions of the ulnar head were marked with Kirschner wires (K-wires; Fig. 3a–e). The perimeter between the two K wires was measured and the angle between the two K-wires was measured, after photographs were taken, using ImageJ Software (National Institutes of Health, Bethesda, MD).
Fig. 2.
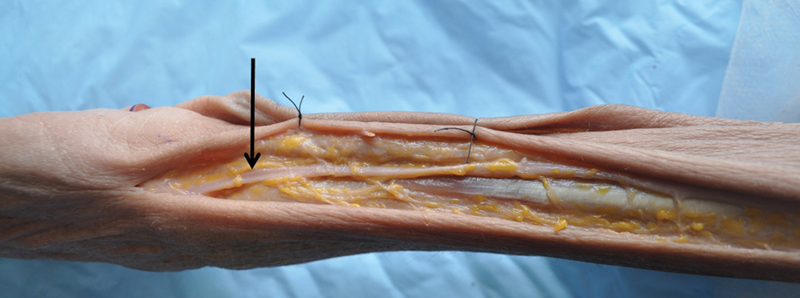
The DSBUN was observed to cross from volar to dorsal at the ulnar styloid as demonstrated here (arrow).
Fig. 3.
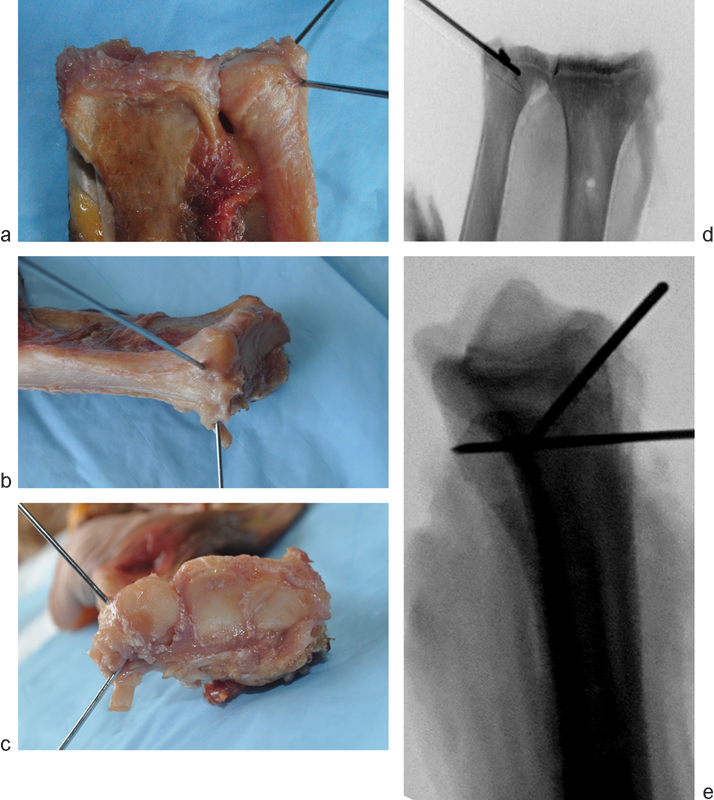
(a) Anteroposterior (AP), (b) lateral, and (c) axial view of the safe zone defined by placement of the K-wires (c). (d) AP and (e) lateral radiograph. The perimeter of the nonarticular portion was measured along with edges of the arc.
The two commercially available plates designed specifically for the distal ulna plates were then applied to specimens using the defined parameters of the designated safe zones to see whether they could be accommodated (Figs. 4a–e, 5a–e). Fluoroscopy was used to verify plate position within the safe zone in this area.
Fig. 4.
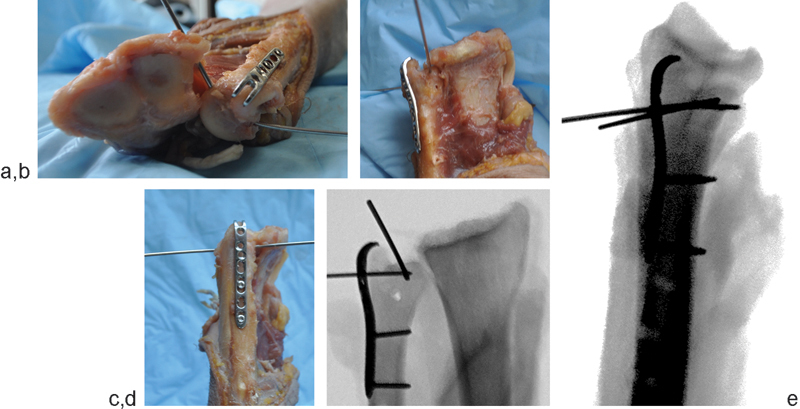
(a) AP, (b), lateral, and (c) axial views of the applied distal ulna hook plate with the safe zone designated with K-wires. (d) AP and (e) lateral radiographs.
Fig. 5.
(a) AP, (b) lateral, and, (c) axial views of the applied distal ulna locking plate with the safe designated with K-wires. (d) AP and (e) lateral radiographs
Results
Our results are summarized in Table 1. The average perimeter of the safe zone was 21.5 mm (SD = 3.3 mm), and the average arc measured 116° (SD = 6.8°). The DSBUN was seen to cross from volar to dorsal at the ulnar styloid in four out of six specimens; in one specimen the nerve crossed 38 mm proximal to the ulnar styloid and 15 mm distal to the ulnar styloid in the last. In the right forearms, the ECU tendon was found to occupy the one o'clock position in four out of six of the forearms and the two o'clock position in the other two. This would correspond to ten and eleven o'clock positions on a left wrist, respectively.
Table 1. A summary of measurements of each sample.
| Sample | Safe zone length (mm) | Degrees of safe zone | Location of DSBUN | Location of ECU tendon (clock face position) |
|---|---|---|---|---|
| 1 | 19 | 110 | 15 mm distal to ulnar styloid | One |
| 2 | 23 | 114 | At ulnar styloid | One |
| 4 | 24 | 121 | 38 mm proximal to ulnar styoid | One |
| 4 | 19 | 109 | At ulnar styloid | One |
| 5 | 17 | 116 | At ulnar styloid | Two |
| 6 | 25 | 127 | At ulnar styloid | Two |
Both plates could be placed within the defined safe zone. The distal ulna hook plate (Synthes) could be placed outside of the footprint of the ECU tendon. The distal ulna locking plate (Acumed) was designed to be placed volarly. The plate needs to be placed proximal to the sigmoid notch to prevent impingement with DRUJ rotation. The locking screws are directed distally to help control the ulnar head fragment. Representative samples that were used for plating within the defined safe zone are demonstated in Figs. 4a–e and 5a–e.
Discussion
The anatomy of the distal ulna provides a unique challenge for fixation because of the limited area available. Much of the distal ulna is covered with articular cartilage, and the footprint of the ECU tendon is a potential area for tendon irritation. Certain fracture patterns, such as those with large ulnar styloid fragments with extension into the ulnar head, may be more amenable to plate fixation. Typically, the distal ulna is approached in the internervous plane between the ECU and FCU tendons. We attempted to define a safe zone using this surgical approach, where a plate may be applied outside of the articular surface and away from the ECU tendon sheath to avoid tendon irritation. Our data suggest that the safe zone for plate placement on the distal ulna is approximately between the 10 and 12 o'clock positions on the right wrist or between the 12 and 2 o'clock positions on the left wrist (Fig. 6a–g). This would avoid impingement with the distal radius and avoid interfering with the ECU sheath. If plating of the distal ulna is required, the plate should be less than 20 mm wide and placed immediately volar to the ECU tendon.
Fig. 6.
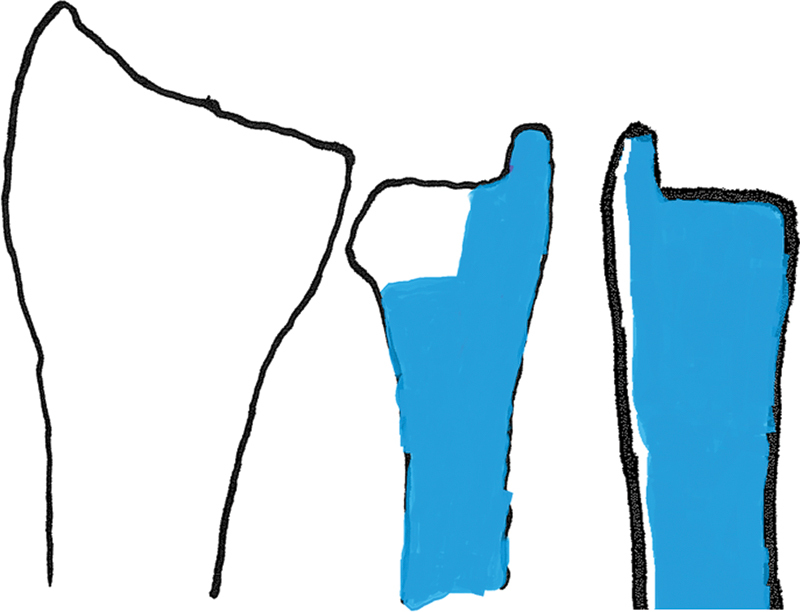
AP and lateral depictions of the safe zone for plating of the distal ulna. The safe zone has been shaded in blue.
This purpose of this study was to identify anatomic considerations when plating the distal ulna. When utilizing the hook plate, care must be taken to keep the plate out of the footprint of the ECU tendon subsheath. The plate is very narrow, which makes this quite possible. However, because of this the narrow profile, the plate has limited use for fracture patterns where more comminution is present. The other plate used in this study is meant to be placed more volarly. The distal locking screws are meant to help control the distal head fragments. If the plate is placed too distally, the plate will impinge and impede motion of the DRUJ. Care must be taken to ensure that the plate is left proximal to the sigmoid notch of the distal radius. Because of this limitation, it is difficult for the plate to control very distal fragments, especially those involving the ulnar styloid.
Our study does not provide absolute specifications for plate placement but guidelines utilizing the ulnar styloid as a reference. Also, our study demonstrated that there can be quite some variability in position of the DSBUN, indicating that dissection is needed when approaching the distal ulna through the ECU/FCU interval. The anatomic study by Botte and colleagues demonstrated that the DSBUN emerged 5 cm from the proximal edge of the pisiform, with 1.8 cm standard deviation, which is consistent with our findings that variability does exist when it emerges and course dorsally.6 This is especially important to consider during the surgical approach. A recent study by Das De and colleagues examined soft tissue complications of dorsal versus volar plating for ulnar shortening osteotomies.7 They found a higher incidence of painful hardware requiring removal of implants in the volar group. The region where dorsal plating occurred was more proximal than the region that was examined in this study, which involves more of the ECU tendon. Patients should be counseled about the complication of painful hardware and possible need for removal when volar plating of the ulna is needed to treat distal ulna fractures.
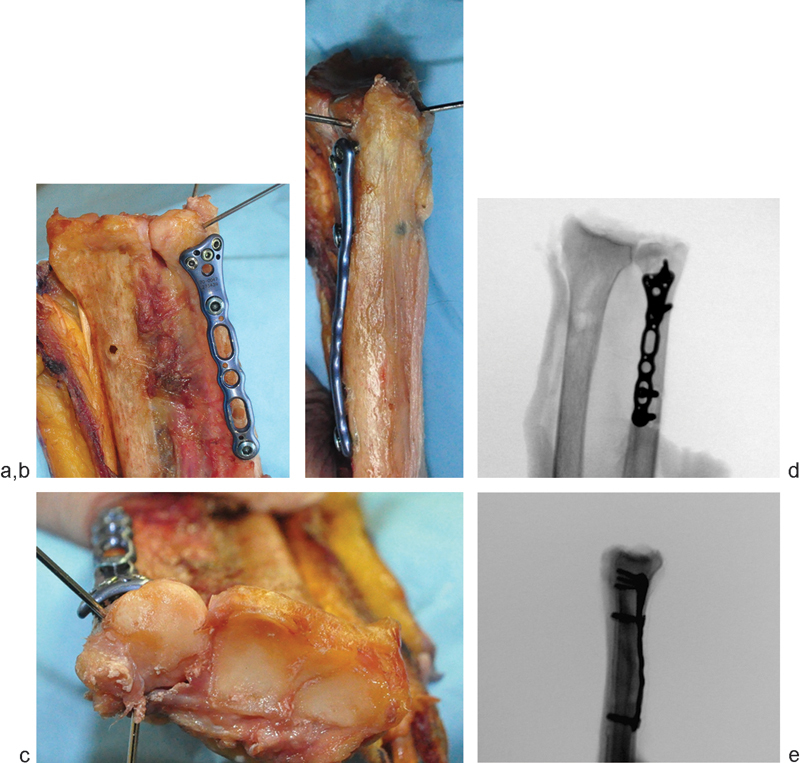
The ideal placement for plate fixation, given our findings, would be just volar tothe ulnar border of the wrist. However, this region is quite limited and may not be available given the comminution of a particular fracture pattern. For example, a 63-year-old man sustained a left open distal ulna fracture with bone loss from a dog bite (Fig. 7a, b). Initially, an attempt was made to use the smaller distal ulna hook plate, but, given the comminution of the fracture, the plate was not suitable for this injury. The distal ulna plate (Acumed) was used instead. Given the amount of bone loss, we had to place the plate quite distal and advised the patient that he may have pain with wrist rotation (Fig. 7c, d). He was asymptomatic from the plate and did not request for it be removed. Analysis of the CT scan demonstrated that our plate was mostly in the region of the defined safe zone, which likely explains his lack of impingement symptoms (Fig. 7e–g).
Fig. 7.
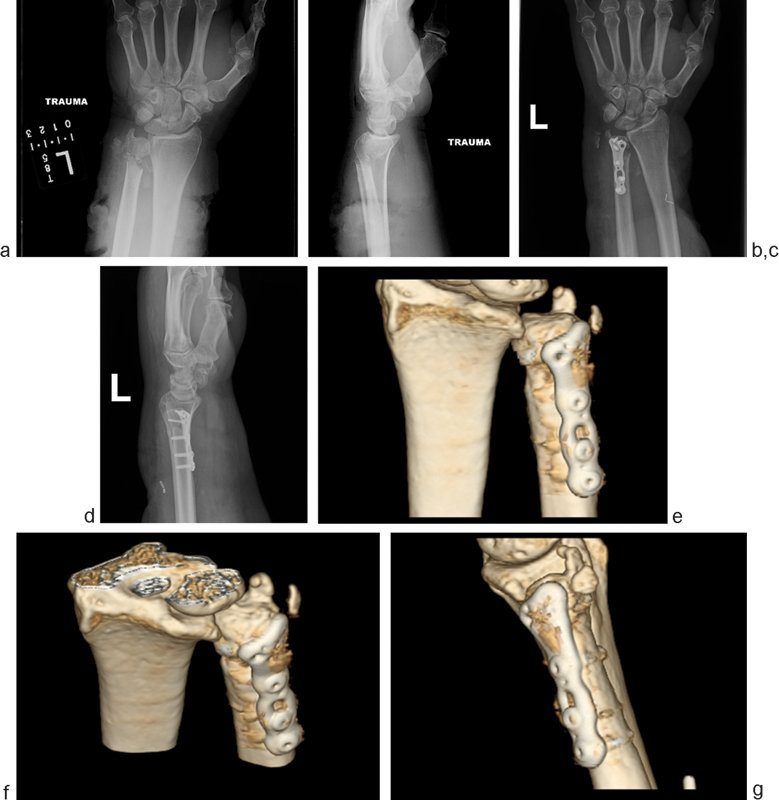
(a, b) AP and lateral X-ray images of the wrist of a 63-year-old man who sustained an open left distal ulna fracture with bone loss after a dog bite. (c, d) He underwent open reduction internal fixation using the distal ulna locking plate utilized in this study. (e–g) He went on to union as demonstrated by the 3-D computed tomography (CT) reconstruction.
Distal ulna injuries can be quite complex to manage. Certain injuries may necessitate the need to place hardware outside of the safe zone. In these situations, surgeons should make patients aware of the possible need for re-operation and hardware removal.
Acknowledgment
The authors would like to thank Synthes North America and Acumed for use of their distal ulna plates for this research project.
Footnotes
Conflict of Interest None
References
- 1.Biyani A, Simison A J, Klenerman L. Fractures of the distal radius and ulna. J Hand Surg [Br] 1995;20(3):357–364. doi: 10.1016/s0266-7681(05)80094-4. [DOI] [PubMed] [Google Scholar]
- 2.Geissler W B, Fernandez D L, Lamey D M. Distal radioulnar joint injuries associated with fractures of the distal radius. Clin Orthop Relat Res. 1996;(327):135–146. doi: 10.1097/00003086-199606000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Rozental T D, Bozentka D J, Katz M A, Steinberg D R, Beredjiklian P K. Evaluation of the sigmoid notch with computed tomography following intra-articular distal radius fracture. J Hand Surg Am. 2001;26(2):244–251. doi: 10.1053/jhsu.2001.22930. [DOI] [PubMed] [Google Scholar]
- 4.Faierman E, Jupiter J B. The management of acute fractures involving the distal radio-ulnar joint and distal ulna. Hand Clin. 1998;14(2):213–229. [PubMed] [Google Scholar]
- 5.Greenberg J A. Reconstruction of the distal ulna: instability, impaction, impingement, and arthrosis. J Hand Surg Am. 2009;34(2):351–356. doi: 10.1016/j.jhsa.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 6.Botte M J, Cohen M S, Lavernia C J, von Schroeder H P, Gellman H, Zinberg E M. The dorsal branch of the ulnar nerve: an anatomic study. J Hand Surg Am. 1990;15(4):603–607. doi: 10.1016/s0363-5023(09)90022-3. [DOI] [PubMed] [Google Scholar]
- 7.Das De S Johnsen P H Wolfe S W Soft tissue complications of dorsal versus volar plating for ulnar shortening osteotomy J Hand Surg Am 2015; In press [DOI] [PubMed] [Google Scholar]


