Abstract
Background Here we present a preliminary case series of unicompartmental isoelastic resurfacing prosthesis of the distal radius to treat comminuted articular fractures of osteoporotic elderly patients.
Materials and Methods Our study included 12 patients, mean age 76 years, who presented with comminuted osteoporotic distal radius fracture. Because of the severity of injury and poor bone quality; osteosynthesis was not deemed to be a good option.
Description of Technique The surgery was performed through a dorsal approach. The subchondral bone of the entire distal radial articular was excised and a unicompartmental prosthesis was applied.
Results At an average follow-up of 32 months, the pain was 2.8/10, Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) 37.4/100, grip strength in neutral 49.9%, in supination 59.0%, and in pronation 56.2% of the contralateral normal side. The wrist ranges of motion in flexion and extension were 56.1% and 79.3%, in supination and pronation 87.7% and 91.0% of the contralateral normal side. Two patients experienced a complex regional pain syndrome (CRPS) type II; these resolved spontaneously. One patient experienced distal radioulnar joint (DRUJ) stiffness, which improved after an ulna head resection. Finally, one patient required revision surgery after a secondary traumatic fracture. Radiographically; the average volar tilt was 9.8°; the average of radial inclination was 11.6°.
Conclusion The concept of a unicompartmental isoelastic resurfacing prosthesis offers a promising option for the treatment of comminuted, osteoporotic distal radius articular fractures of elderly patients.
Level of Evidence IV
Keywords: unicompartmental isoelastic resurfacing prosthesis, distal radius fracture, hemi-prosthesis, osteoporosis, elderly, wrist prosthesis
Displaced comminuted articular fractures of the distal radius in elderly patients with osteoporosis represent a treatment dilemma. Although volar locking plate fixation has often become the treatment of choice for patients without osteoporosis, volar locking plate fixation is not as successful in distal radius fractures with severe comminution and osteoporosis.1 2 As in the case of other osteoporotic joint fractures in the elderly such as the hip,3 shoulder,4 and elbow,5 sometimes a prosthesis is a necessary or attractive option. In select cases, a prosthesis can immediately reconstruct the articular surface and quickly restore autonomy to elderly patients.
Total wrist prostheses have not been proposed for the treatment of acute fractures of the distal radius, probably because they have often had loosening of the carpal component.6 7 8 To improve this problem, some authors have proposed to treat these fractures with Unicompartmental prosthesis of distal radius.9 10 11 12
Here we present a preliminary case series of bicompartmental isoelastic resurfacing prosthesis of distal radius. This prosthesis preserves bone stock, and primary fixation is provided by an intramedullary pin resting on the subchondral bone of the radial head.
Materials and Methods
Our retrospective study included 12 patients (all women) with a mean age of 76 years (range: 53–92 years; Table 1). One patient (case 10) underwent surgery for a failed volar plate fixation of a distal radius fracture: Eleven patients underwent primary surgery for a distal radius fracture with a Unicompartmental isoelastic resurfacing prosthesis (Prosthelast, Argomedical, Cham, Switzerland). The prosthesis is anatomically designed much like a surface replacement arthroplasty in that it seats against the scaphoid and lunate fossa. The prosthesis is fixed with an intramedullary pin using an attachment screw. The implant is provided in left and right hand configurations.
Table 1. Series of 12 patients treated by unicompatimental isoelastic resurfacing prosthesis of distal radius.
| Patient (N) |
Age | Sex (M/F) |
Dominant side (R/L) |
Operated side (R/L) |
Type of fracture (AO classification) |
|---|---|---|---|---|---|
| 1 | 76 | F | R | L | C2.3 (Primary) |
| 2 | 78 | F | L | L | C1.3 (Primary) |
| 3 | 74 | F | R | R | A3.3 (Primary) |
| 4 | 88 | F | R | L | A3.3 (Primary) |
| 5 | 53*1 | F | R | R | C2.2 (Primary) |
| 6 | 78 | F | R | L | C2.2 (Primary) |
| 7 | 74 | F | R | L | C3.1 (Primary) |
| 8 | 62*2 | F | L | L | C2.2 (Primary) |
| 9 | 82 | F | R | L | C2.1 (Primary) |
| 10 | 87 | F | R | R | C2.2 (Secondary) |
| 11 | 72 | F | R | L | C3.2 (Primary) |
| 12 | 92 | F | R | R | C3.2 (Primary) |
*1: Severe comminuted and die punch fracture
*2: Severe comminuted fracture
Abbreviations: F, female; L, left; M, male; R, right.
Clinical outcomes were assessed using the visual analogue scale (VAS) for pain and the Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) questionnaire for functionality. For the VAS, pain was measured from 0 (no pain) to 10 (most extreme pain imaginable). The QuickDASH functional score of upper limb was measured from 0 (no discomfort) to 100 (unusable upper limb). All measurements for wrist range of motion and strength were made by hand therapists independent from the surgeon. Range of motion of the wrist was reported as the percentage compared with the contralateral normal side. The grip strength in the neutral position was measured by using the Jamar (Arex, Palaiseau, France) dynamometer, pronosupination strength were also measured by using overhand dynamometer (Arex, Palaiseau, France). Radiographic parameters were assessed by the surgeons and include volar tilt and radial inclination with the use of measurement software. On lateral view, volar tilt was measured by the angle between the line drawn from the dorsal tip to the volar tip of the prosthesis and a line perpendicular to the shaft axis. On anteroposterior (AP) view, radial inclination was measured by the angle between the line drawn from the radial tip to the ulnar tip of the prosthesis and a line perpendicular to the shaft axis.
Surgical Technique
The surgical technique was the same for all patients (Video 1). All patients were operated on through a dorsal approach under regional anesthesia. In all cases a pneumatic tourniquet at the humeral level was used. Through the dorsal incision, the fourth extensor compartment was opened and the radiocarpal joint was exposed by using two triangular capsular flaps. The midcarpal joint was not exposed. The subchondral bone of the entire distal radial articular was excised. Metaphyseal bone stock was preserved. A 2.5-mm diameter Kirschner wire (K-wire) was introduced retrograde and inserted up the medullary canal to the subchondral bone of the radial head using fluoroscopy. A trial implant was applied to determine the optimal length (ulnar variance = 0) of K-wire. The trial was removed, and the definitive implant was fixed with the intramedullary pin using an attachment screw. The distal radioulnar joint (DRUJ) was preserved in eight cases. A resection of the head of the ulna was necessary in four cases at the same time of operation. Exam under fluoroscopy was performed at the wrist and elbow to confirm stability and motion. The wound was closed in layers. A forearm-based palmar wrist splint with 20° of extension was applied, and the tourniquet was released. No drain was used. At 2 weeks after the operation, the splint and stiches were removed and self-rehabilitation was begun.
Video 1
Surgical techniques (case 3).
Online content including video sequences viewable at: www.thieme-connect.com/products/ejournals/html/10.1055/s-0035-1556855.
Results
No intraoperative complications were noted, especially no fracture of the radial head. In one case (case 2) increased radiocarpal laxity was solved by careful repair of the dorsal capsule, sutured by 2–0 Vicryl (Ethicon, Issy-les-Moulineaux, France) passed through the holes of the prosthesis. This laxity resulted from an insufficient length of radius after reconstruction, compared to the contralateral normal side. The mean duration of surgery was 53 minutes, with a range of 22 to 98 minutes. The duration of the surgery gradually decreased with surgeon experience with the prosthesis and the operation. There were no immediate postoperative complications such as carpal tunnel syndrome, infection, or tendon rupture.
The average follow-up was 32 months with a range of 24–42 months.
Clinically, the average VAS score was 2.8/10. The average QuickDASH was 37.4/100. The grip strength in neutral was 49.9% of the opposite hand. Grip strength in supination and pronation were 59.0% and 56.2% compared with the opposite side respectively. The range of motion in flexion averaged 56.1% compared with the opposite wrist. The wrist extension averaged 79.3% compared with the opposite wrist. Supination and pronation averaged 87.7% and 91.0% respectively, compared with the contralateral normal side.
Results are shown in Table 2.
Table 2. Results of unicompatimental isoelastic resurfacing prosthesis of distal radius.
| Patient (N) |
Follow-up (months) |
QuickDASH (0–100) |
Pain (0–10) |
Grip strength (% contralateral) |
Range of motion (% contralateral) |
Radiological findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| G | S | P | F | E | S | P | Volar tilt (°) |
Radial inclination (°) |
Ulnar variance (mm) |
||||
| 1 | 34 | 72.73*1 | 5 | 50.0 | 10.0 | 44.4 | 62.5 | 100.0 | 100.0 | 100.0 | 15 | 12 | NA |
| 2 | 42 | 64.00*2 | 5 | 20.0 | 50.0 | 32.6 | 25.0 | 83.3 | 62.5 | 100.0 | 15 | 8 | 0 |
| 3 | 36 | 29.55 | 3 | 41.7 | 63.6 | 53.3 | 22.2 | 92.3 | 93.3 | 100.0 | 0 | 13 | 0 |
| 4 | 36 | 63.64 | 7*3 | 55.5 | 63.6 | 60.0 | 30.0 | 50.0 | 93.3 | 100.0 | -1 | 14 | NA |
| 5 | 35 | 54.55 | 4 | 28.6 | 14.3 | 22.7 | 23.5 | 62.5 | 113.3 | 93.8 | 0 | 11 | NA |
| 6 | 24 | 34.09 | 5 | 33.3 | 75.0 | 88.2 | 50.0 | 38.5 | 73.3 | 100.0 | 14 | 10 | –1 |
| 7 | 31 | 9.19 | 0 | 75.0 | 75.0 | 75.0 | 75.0 | 100.0 | 100.0 | 75.0 | 15 | 10 | 0 |
| 8 | 28 | 34.09 | 5 | 50.0 | 50.0 | 50.0 | 75.0 | 75.0 | 50.0 | 75.0 | 14 | 10 | +1 |
| 9 | 24 | 0.00 | 0 | 60.0 | 100.0 | 77.8 | 66.7 | 100.0 | 66.7 | 88.2 | 0 | 9 | 0 |
| 10 | 24 | 72.73*4 | 0 | 66.7 | — | — | 81.8 | 50.0 | 100.0 | 84.6 | 11 | 10 | NA |
| 11 | 40 | 13.64 | 0 | 58.3 | 87.5 | 53.8 | 62.0 | 100.0 | 100.0 | 75.0 | 15 | 12 | +1 |
| 12 | 24 | 0.00 | 0 | 60.0 | 60.0 | 60.0 | 100.0 | 100.0 | 100.0 | 100.0 | 20 | 10 | +2 |
Abbreviations: E, extension; F, Flexion; G, grasp; NA, non applicable; P, pronation; S, supination.
*1: High level of QuickDASH score was induced by bilateral radius fracture.
*2: High level of QuickDASH score was probably induced by CRPS type 2 after the operation.
*3: Residual pain and high level of QuickDASH score were induced by polyarthritis.
*4: High level of QuickDASH score was induced by progressive degenerative brain disease (probably Alzheimer disease).
Cases 7, 8, and 12: Latest consultation was performed by telephone interview.
Four postoperative complications were noted. Two patients initially exhibited stiffness and hypersensitivity, possibly suggestive of complex regional pain syndrome (CRPS) type II. However; both of these resolved spontaneously (cases 2 and 5). One patient had symptoms of pain and stiffness at the DRUJ. Her symptoms were improved by resection of ulna head (case 4). Finally, one patient tripped and fell 4 months after her operation. She experienced a secondary traumatic fracture of the distal radius and K-wire (case 1). Revision surgery was performed on the third day after the trauma. After removal of the fractured K-wire, a shorter K-wire was inserted and fixed to the radial prosthetic component. Augmented fixation was performed by filling with acrylic cement and fixed with a cerclage wiring at the distal metaphysis.
At final radiographic follow-up, the average of volar tilt was 9.8° with a range of –1° to 20°, the average of radial inclination was 11.6° with a range of 8–14°.
As far as other radiographic observations at final follow-up, there were no perforations or fractures of the radial head. There was no subluxation observed at the radiocarpal joint. In three cases (cases 8, 11, and 12), an osteolytic border appeared around the radial implant. There were no clinical symptoms in these cases. We observed progressive bone remodeling (Figs. 1a–c, 2a, b) around the prosthesis and the DRUJ in eight cases (cases 2, 3, 6, 7, 9, 10, 11, and 12). In four cases; there was radiographic evidence of bony reaction between the scaphoid and the radial edge of prosthesis (cases 1, 2, 6, and 12), and in two cases there was radiographic evidence of bony reaction in the lunate and the ulnar edge of the prosthesis (cases 3 and 5; Fig. 2a, b). In one of the cases of bony reaction in the scaphoid, the patient did appear to have symptoms of impingement with the prosthesis. Revision surgery was performed at 16 months after the first operation (case 2) with resection of the first carpal row without revision of the prosthesis. None of the other patients underwent revision surgery. No significant difference was finally noticed when the ulnar head was kept or removed.
Fig. 1.

Unicompartmental prosthesis was applied for a failed volar plate fixation of a distal radius fracture in 87-year-old patient (case 10). (a) Radiograph showed the secondary displacement of volar locking plate with severe joint destruction in a very osteoporotic bone. There is also typical radius shortening. (b) One month after the second operation for Prosthelast insertion, the ulna head resection was performed to correct ulnar variance. (c) 19 months after the operation, there was good congruency between the distal end of the ulna and the prosthesis. There was also radiographic evidence of bony remodeling around the prosthesis and some bone defect radially.
Fig. 2.
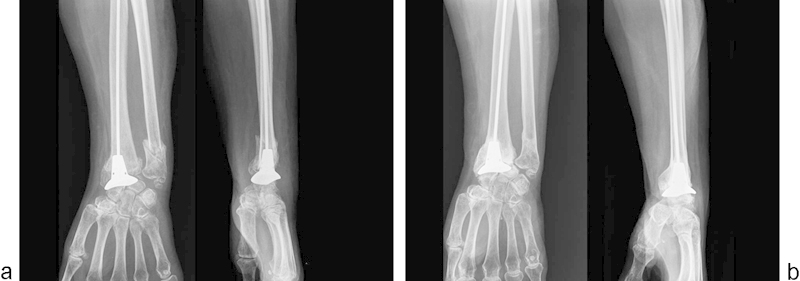
A case of bony reaction between the lunate and the prosthesis with a good clinical result (case 3). (a) Two months after the operation, there was inadequate coverage of lunate by the prosthesis, because the implant was too small and slightly malrotated. (b) 36 months after the operation, there was bony reaction between the lunate and the prosthesis. However, there was also radiographic evidence of bony remodeling around the prosthesis.
Discussion
Comminuted fractures of the distal radius in patients with osteoporosis remain a difficult clinical problem. The use of volar locking plates, external fixators, or other techniques have shown high failure rate when used to treat such injuries.13 14 Prosthetic replacement may be an attractive option in certain cases where the reconstruction of the articular surface would be difficult or impossible.
Our case series of results contained three important technical points: decision of the optimal length of the intramedullary pin, sufficient repair of the dorsal capsule, and one size of radial component.
Concerning the intramedullary pin, the most difficult point was to define and cut its ideal length. Too short an intramedullary pin would not gain support in the intramedullary canal, and the radial component could migrate proximally with risk of ulnocarpal impingement. Too long an intramedullary pin could risk lack of metaphyseal support of the prosthesis or cause radiocarpal impingement. The assumption was that the ideal length of the intramedullary pin would restore an anatomical distal radioulnar variance (average 0.375 mm in our series).
An additional technical point is the repair of the dorsal capsule. If the dorsal capsule is repaired too loosely, it may cause anterior instability of the carpus. If the capsule is repaired too tightly, it may limit wrist flexion postoperatively. Some of our patients did show limited wrist flexion at the last follow-up (cases 2, 3, 4, and 5). The ideal repair of the dorsal capsule probably provides an appropriate balance of wrist stability and mobility. In our experience, the ideal dorsal capsule repair consisted of two horizontal triangular capsular flaps. One is a radially based flap, and the other one is an ulnarly based flap. Each capsular flap is sutured with each other at the end of intervention (Video 1). There is no need to suture the dorsal capsule at the midcarpal joint level.
Finally, our series consisted of only one size of Prosthelast prostheses. This possibly was responsible for some impingement between the prosthesis and the scaphoid (cases 1, 2, 6, and 12) or between the prosthesis and the lunate (case 3, 5). We did not observe any problems on the dorsum of the wrist between the prosthesis and the extensor tendons.11 It would seem essential to put an implant in the most appropriate size for the patient's anatomy; a second size of implants (small) is now available. However, even with the use of a single-size component, the overall motion, strength, and QuickDASH scores of the patients in this series was favorable.
Interestingly, in this series, there were eight cases that showed radiographic evidence of bony remodeling around the prosthesis (cases 2, 3, 6, 7, 9, 10, 11, and 12). Possibly, micro-motion of the prosthesis allows or accelerates bone formation. It may be that this is evidence in favor of the concept of isoelasticity described by Butel.15 Based on his concept, the implant and the bone deformed as a single unit. For the lower extremity, the clinical results of isoelastic hip replacement were unsuccessful, and the prosthesis is no longer in use.12 For the upper extremity, however, the compressive stresses are small and the bending stresses and rotation are more important. The application of an isoelastic prosthetic might be more appropriate to the upper limb. To our knowledge, this phenomenon or type of prosthesis has not been described in the previous literature for the wrist.
In this series, there were no cases of proximal migration of the prosthesis, no cases of elbow pain, and no limitation of movement of the elbow or perforation of the radial head. The stability of the prosthesis is possibly explained by the block effect of the rectilinear pin into the intramedullary canal and the doubly curved radius. Therefore, the forces on the distal prosthesis are partially absorbed by the shaft of the radius.
Other authors have developed unicompartmental prosthetic radius implants for use in these situations.10 11 12 However, these other unicompartmental prostheses have had some limitations. One of the other prostheses necessitates a wide resection of the radial metaphysis.12 Such wide resection could lead to loss of bone stock and make salvage operations such as a secondary arthrodesis quite difficult. A second limitation of these other prostheses is that the fixation of the prosthesis is restricted to the radial metaphysis. Such a prosthesis has a risk of insufficient primary stabilization, particularly in cases of a longitudinal fracture line at the radial metaphysis.
We hypothesized that the ideal distal radius prosthesis for the treatment of the comminuted articular fracture in osteoporotic bone complies with the following conditions: (1) only the articular surface of the distal radius is replaced (thus avoiding loosening of the carpal component), (2) only the subchondral bone of the distal radius is resected (to preserve bone stock maximally), and (3) the use of intramedullary support would provide reliable primary stabilization of the prosthesis. The concept of an isoelastic prosthesis, developed in the field of lower limb surgery,15 16 could be applied to meet these conditions in the wrist.
In our series of 12 patients with a minimum follow up of 2 years, we have noted quite good functional results with this unicompartmental isoelastic resurfacing prosthesis in a very challenging patient population. Obviously, there is a learning curve in the use of this prosthesis, and having additional size options for the prosthesis may allow us to better reconstruct the anatomy. We will continue to follow these patients over a longer period. For the appropriately selected elderly patients with intraarticular distal radius fractures, the use of this prosthesis offers a single-operation treatment option that restores early function. In conclusion, a unicompartmental isoelastic resurfacing prosthesis is a potentially viable treatment option for comminuted articular fractures of the distal radius in elderly patients.
Footnotes
Conflict of Interest Philippe Liverneaux has a conflict of interest with Newclip Technics, Integra, Argomedical, iiN Medical.
References
- 1.Ginn T A Ruch D S Yang C C Hanel D P Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. Surgical technique J Bone Joint Surg Am 200688(Suppl 1 Pt 1):29–36. [DOI] [PubMed] [Google Scholar]
- 2.Hanel D P, Lu T S, Weil W M. Bridge plating of distal radius fractures: the Harborview method. Clin Orthop Relat Res. 2006;445(445):91–99. doi: 10.1097/01.blo.0000205885.58458.f9. [DOI] [PubMed] [Google Scholar]
- 3.Kwok D C, Cruess R L. A retrospective study of Moore and Thompson hemiarthroplasty. A review of 599 surgical cases and an analysis of the technical complications. Clin Orthop Relat Res. 1982;(169):179–185. [PubMed] [Google Scholar]
- 4.Neer C S II, Horwitz B S. Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res. 1965;41(41):24–31. [PubMed] [Google Scholar]
- 5.Burkhart K J, Nijs S, Mattyasovszky S G. et al. Distal humerus hemiarthroplasty of the elbow for comminuted distal humeral fractures in the elderly patient. J Trauma. 2011;71(3):635–642. doi: 10.1097/TA.0b013e318216936e. [DOI] [PubMed] [Google Scholar]
- 6.Herzberg G. Prospective study of a new total wrist arthroplasty: short term results. Chir Main. 2011;30(1):20–25. doi: 10.1016/j.main.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 7.Adams B D. Total wrist arthroplasty. Tech Hand Up Extrem Surg. 2004;8(3):130–137. doi: 10.1097/01.bth.0000131199.39073.2a. [DOI] [PubMed] [Google Scholar]
- 8.Chantelot C. Wrist prostheses [in French] Chir Main. 2006;25(6):271–279. doi: 10.1016/j.main.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Roux J L, Micallef J P, Allieu Y. London, UK: Martin Dunitz; 2000. Biomechanical considerations for wrist arthroplasty; pp. 183–191. [Google Scholar]
- 10.Roux J L. Replacement and resurfacing prosthesis of the distal radius: a new therapeutic concept [in French] Chir Main. 2009;28(1):10–17. doi: 10.1016/j.main.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 11.Roux J L. Treatment of intra-articular fractures of the distal radius by prosthetic replacement and resurfacing [in French] Rev Chir Orthop Traumatol. 2011;97S:S46–S53. [Google Scholar]
- 12.Vergnenègre G, Mabit C, Charissoux J L, Arnaud J P, Marcheix P S. Treatment of comminuted distal radius fractures by resurfacing prosthesis in elderly patients. Chir Main. 2014;33(2):112–117. doi: 10.1016/j.main.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 13.Gehrmann S V, Windolf J, Kaufmann R A. Distal radius fracture management in elderly patients: a literature review. J Hand Surg Am. 2008;33(3):421–429. doi: 10.1016/j.jhsa.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 14.Schneppendahl J, Windolf J, Kaufmann R A. Distal radius fractures: current concepts. J Hand Surg Am. 2012;37(8):1718–1725. doi: 10.1016/j.jhsa.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Butel J, Robb J E. The isoelastic hip prosthesis followed for 5 years. Acta Orthop Scand. 1988;59(3):258–262. doi: 10.3109/17453678809149357. [DOI] [PubMed] [Google Scholar]
- 16.Kinnard P, Vanbellinghen M, d'Affnay P L. Butel's isolestic hip prosthesis. A limited prospective study [in French] Rev Chir Orthop Reparatrice Appar Mot. 1994;80:316–319. [PubMed] [Google Scholar]


