Abstract
Background Intra-articular distal radius fractures can have many complications, including radiocarpal osteoarthritis and distal radioulnar joint (DRUJ) dysfunction leading to pain and restricted wrist function.
Case Description We describe the case of a 38-year-old patient who sustained a left distal radius intra-articular fracture, which was treated with volar plating. She developed pain from the radiocarpal joint as a result of intra-articular malunion and was listed for total wrist fusion. On the day of surgery this was converted to a Darrach procedure for minor DRUJ symptoms. This resulted in pain from the DRUJ as a result of instability, in addition to persisting radiocarpal arthritis pain. Due to her subsequent poor wrist function, she presented to the authors and underwent DRUJ arthroplasty with a proximally placed Scheker prosthesis to deal with her DRUJ symptoms and, later, a KinematX radiocarpal hemiarthroplasty for her radiocarpal symptoms. She remains happy with her outcome at 36-month follow-up.
Literature Review The complications of the Darrach procedure include painful radioulnar convergence and wrist instability. The Scheker prosthesis allows restoration of stability of the DRUJ with good outcomes and 100% 5-year survival in one series. Sparing the midcarpal joint, the KinematX hemiarthroplasty allows preservation of the dart thrower's motion arc, which is key in many complex wrist movements and functions.
Clinical Relevance This case highlights the negative consequences of distal ulna resection and shows both the Scheker and KinematX prostheses as viable, effective means to restore function to young, active patients with posttraumatic radiocarpal arthritis and/or instability.
Keywords: distal radius fracture, distal radioulnar joint (DRUJ), hemiarthroplasty
Distal radius fractures predominantly affect two adult population groups: elderly patients with fragility fractures and young adults following high-energy trauma. These injuries represent 20% of all adult fractures, of which up to 50% have an intraarticular component. The development of posttraumatic arthritis following intra-articular fractures is well known, resulting in pain and functional impairment. Malunion causing articular step-offs leading to changes in contact stresses may result in degenerative changes.1 For this reason the management principles of intra-articular fractures aim to achieve anatomic reduction and fixation to restore joint line congruity. One of the key focuses is the articular support of the carpal bones, with articular alignment and congruity thought to be most important in restoring pain-free wrist function.
The main compromised joint in distal radial fractures is the radiocarpal joint,2 but distal radioulnar joint (DRUJ) involvement is also frequently observed, particularly when the fracture involves the sigmoid notch. This can have damaging effects on upper limb function and increase the morbidity of the fracture. With patients in whom the DRUJ is involved or dysfunctional, restoration of normal anatomy is key, to enable free rotation to position the hand in space appropriately.
Darrach's procedure has been used successfully in the treatment of DRUJ symptoms, but it has had high incidences of pain due to radioulnar convergence and wrist instability, which can produce severe morbidity, particularly in young, active patients. Of the management options for the complications of Darrach's procedure, a constrained DRUJ prosthesis (Scheker; APTIS Medical, Glenview, KY, USA) has shown promising results in relieving patient symptoms.
The midcarpal joint, frequently spared in posttraumatic wrist arthritis, is key in many complex, integral wrist movements. Hemiarthroplasty of the radiocarpal joint with the KinematX prosthesis (Extremity Medical, Parsippany, NJ, USA), a treatment option for posttraumatic radiocarpal arthritis, can treat the dysfunctional joint while preserving the midcarpal joint and so preserving said wrist motion.
This report serves to highlight three main points:
Intra-articular distal radius fractures generally affect only the radiocarpal joint, so preservation of the midcarpal joint is key in maintaining fundamental wrist movements. The KinematX prosthesis has promising early results and may in the future be considered as a treatment option for these patients.
Darrach's procedure can have very debilitating effects, particularly in young patients, but can be managed well with the Scheker prosthesis.
The management of DRUJ alongside radiocarpal dysfunction can pose many difficulties, but preoperative planning can address this and prevent the compromise of either component of management.
Case Presentation
A 38-year-old, right-handed female office worker sustained an intra-articular distal radius fracture following a mountain biking accident in Colombia. Managed locally with volar plating, she later developed severe radiocarpal arthritis and mild DRUJ dysfunction, secondary to inadequate intra-articular reduction. Further surgery for symptom relief was unsuccessfully pursued with Darrach's procedure. Her development of DRUJ instability and reduced wrist function and grip strength led to her presentation to the supervising author ∼2 years after the initial injury.
Her radiographs at presentation demonstrated evidence of Darrach's procedure and features of radiocarpal arthritis, associated with an intra-articular step of > 1 mm and visible callus at the fracture site (Fig. 1a). Magnetic resonance imaging (MRI) confirmed degenerative changes affecting radial and carpal surfaces of the radiocarpal joint. On examination of her wrist, there was dorsal prominence of the distal ulna with instability, with flexion/extension arc 40° (compared with the other side), radioulnar deviation 28°; the wrist was held in pronation but supination was limited to 20° by pain. Her preoperative Disabilities of the Arm, Shoulder and Hand (DASH) was 70.5 and Mayo Wrist Score 10. To improve wrist function, a DRUJ replacement and wrist hemiarthroplasty was performed (Fig. 1b). A proximally placed Scheker prosthesis was performed to allow insertion of the custom-made KinematX wrist hemiarthroplasty (following a total proximal row carpectomy).
Fig. 1.
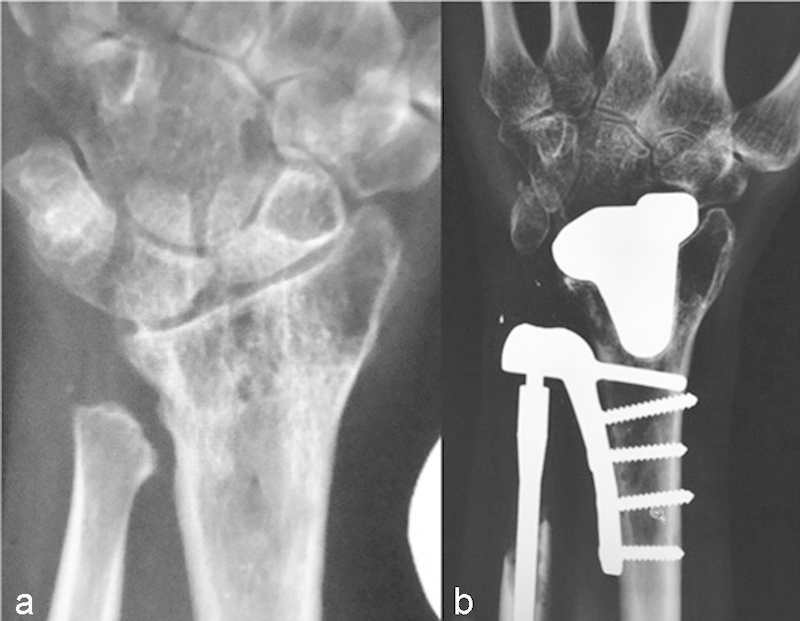
(a) Preoperative anteroposterior (AP) radiograph. (b) Postoperative radiograph showing both prostheses.
At 36-month follow-up, the patient reported satisfactory wrist function; with an improvement in her flexion/extension arc to 60°, radial/ulnar deviation 28°, pronation 90°, and supination 80°. Her postoperative DASH was 31.8 and her Mayo (excluding forearm rotation) only reached 55.
Discussion
Articular distal radius fractures can lead to severe symptoms, causing loss of pain-free wrist function. This commonly affects the radiocarpal joint and DRUJ (the latter to a lesser extent in this reported case), sparing the midcarpal joint, which is key in complex wrist movement, particularly the dart thrower's motion arc. Though shown to have good results in the treatment of severe DRUJ arthritis, distal ulnar resection can have severe complications relating to impaired wrist function, as in this case.
Arthroplasty
Treatment options for posttraumatic wrist arthritis range from total arthroplasty to arthrodesis and ablative surgery. Three Cochrane studies failed to identify one method management as superior, due to insufficient evidence. Total wrist arthroplasty was first reported by Swanson in 1973 using a silicone implant and is the mainstay in treatment of pancarpal arthritis, particularly in younger patients. Pancarpal arthritis, however, is more commonly found in inflammatory arthiritides of the wrist rather than in post-traumatic ones, whichtend to be focal, involving the radiocarpal joint. While total wrist replacement offers better functional outcome than arthrodesis, the failure rate of the distal component is high and may require revision surgery.
Alongside normal anatomical movements, the dart thrower's motion; the arc of radial extension to ulnar flexion, is thought to play a key role in most integral wrist movements separate to ulnar/radial deviation of the hand.2 Because this motion takes place almost exclusively at the mid-carpal joint, preservation of this joint is of great importance in maintaining complex functions, particularly in young, active patients. As said, this joint is frequently spared in posttraumatic wrist arthritis, so this motion need not be compromised.
Wrist hemiarthroplasty is a novel approach reported in two series in the literature3 4 with good intermediate results, which allows focal treatment of radiocarpal arthritis. The KinematX midcarpal hemiarthroplasty excises the radiocarpal joint by means of proximal row carpectomy, and the implant provides proximal carpal row replacement, thus preserving the midcarpal articulation, the anatomic center of rotation, and, consequently, the dart thrower's arc.
The benefits include abolished risk of nonunion and improved outcome scores, as seen in the case discussed. Additionally, the procedure is simple and performed within 1 hour. Poorer outcomes were experienced in patients with inflammatory arthritis.3
Hemiarthroplasty is indicated in patients with a preserved distal carpal row and posttraumatic radiocarpal arthritis, scapholunate advanced collapse (SLAC) wrist, scaphoid nonunion advanced collapse (SNAC) wrist, or Kienböck disease. In patients with diseased midcarpal joints, hemiarthroplasty may not be the treatment option to provide the best results. Alternative treatments for wrist arthritis in these cases include ablative surgery such as radial styloidectomy, partial scaphoidectomy, and proximal row carpectomy, although these have been shown to cause instability or lead to progressive degeneration.
Total arthrodesis is a reliable, simple procedure with durable results,5 particularly in cases of pancarpal arthritis. However, in isolated posttraumatic radiocarpal arthritis, the midcarpal joint is preserved, and there may be functional limitations in activities of daily living following unnecessary total arthrodesis.5 Partial arthrodesis provides an alternative in this scenario with procedures such as scaphoid excision, four-corner fusion, and radioscapholunate fusion, although there can be variable fusion rates, with nonunion reported to occur in 3–26%, which can then develop to midcarpal arthritis.3 One prerequisite for partial arthrodesis, however, is that articular surfaces must show minimal degeneration.
Distal Radius Osteotomy
Loss of radial length has found to be a strong predictor of poor wrist function due to the alteration in load bearing and carpal instability. This can also lead to ulna impaction, worsening the wrist instability. The correction of length and angulation of the distal radius allows restoration of normal anatomy. It also has the benefit of treating DRUJ instability, which can be one of the complications of intra-articular distal radius fractures (+/− an additional Adam's/Bower's procedure).
Extra-articular osteotomy was not indicated in this patient, as there was no significant malunion (either extra-articular or intra-articular) and the preoperative MRI demonstrated significant degenerative change on both articular surfaces of the radiocarpal joint.
Drawbacks of Distal Ulna Excision and Alternatives
Although having had good results in the treatment of distal radius fractures and post-traumatic arthritis, Darrach's procedure has had variable failure rates with 7–40%6 being reported in the literature. The main reported drawbacks include impingement causing pain and crepitus, loss of the ulna support of the carpus leading to instability, radioulnar convergence and reduced torque, generating weakness.6 Particularly for younger patients, DRUJ instability and pain can have devastating effects. Papatheodorou et al found, in a study of 20 patients, that an average of 2.2 additional procedures (up to 7) were necessary as an attempt to leave patients symptom free, with all patients still complaining of having problems with pain or wrist function at the end of the follow-up (mean 5 years).7
Management of Ulnar Resection
Treatment of distal ulna resection complications can be complex and can frequently result in reoperated, dissatisfied patients. Currently utilized treatments include stabilizing soft tissue procedures, further shortening of ulna, and ulna lengthening with prosthetics,8 but they have not yet produced reliable results.6
A promising potential salvage procedure is DRUJ arthroplasty, with the Scheker constrained prosthesis producing good results in 4 of 5 and 9/10 who remained revision free in the follow-up of 4 and 5 years.9 10 In the series of 20 patients by Scheker et al,11 the 5-year implant survival was found to be 5 years, with no further data yet gathered. Compared with other hemiarthroplasties, the Scheker implant replaces the ulna head, removing the prerequisite of an intact sigmoid notch and ligamentous support, increasing the number of potential candidates.
In this case, preoperative planning allowed the dual pathology of radiocarpal arthritis and DRUJ instability secondary to ulna resection to be managed well. The more proximal placement of the Scheker implant left sufficient space for a custom KinematX hemiarthroplasty to be placed without impingement and compromise of either of the implants, evidenced by the clinical and functional outcome results seen in this patient in her 36-month follow-up.
Conclusion
Management of DRUJ dysfunction alongside radiocarpal arthritis creates a difficult scenario, without a recognized method of restoring satisfactory wrist function in young patients. Appropriate preoperative planning, however, can allow a combination of prostheses to be implanted and provide the patient with adequate wrist function to enable the patient to return to work and activities of daily living. Longer-term follow-up of the KinematX prosthesis is needed to confirm its benefits and suitability for young, high-demand, active patients. The prosthetic load in a young patient may be an issue for the future; the most likely mode of failure is likely to be articular degeneration on the capitate surface due to the presence of the hemiarthroplasty, and this could be addressed by conversion to total wrist arthroplasty or total wrist fusion (which the patient wanted to avoid), which is feasible around the Scheker implant. Long-term wear in the Scheker implant may be addressed by replacement of the polyethylene ball.
Footnotes
Conflict of Interest None
References
- 1.Lutz M, Arora R, Krappinger D, Wambacher M, Rieger M, Pechlaner S. Arthritis predicting factors in distal intraarticular radius fractures. Arch Orthop Trauma Surg. 2011;131(8):1121–1126. doi: 10.1007/s00402-010-1211-3. [DOI] [PubMed] [Google Scholar]
- 2.Moritomo H, Apergis E P, Garcia-Elias M, Werner F W, Wolfe S W. International Federation of Societies for Surgery of the Hand 2013 Committee's report on wrist dart-throwing motion. J Hand Surg Am. 2014;39(7):1433–1439. doi: 10.1016/j.jhsa.2014.02.035. [DOI] [PubMed] [Google Scholar]
- 3.Vance M C, Packer G, Tan D, Crisco J J, Wolfe S W. Midcarpal hemiarthroplasty for wrist arthritis: rationale and early results. J Wrist Surg. 2012;1(1):61–68. doi: 10.1055/s-0032-1323644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Culp R W, Bachoura A, Gelman S E, Jacoby S M. Proximal row carpectomy combined with wrist hemiarthroplasty. J Wrist Surg. 2012;1(1):39–46. doi: 10.1055/s-0032-1323643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Field J, Herbert T J, Prosser R. Total wrist fusion. A functional assessment. J Hand Surg [Br] 1996;21(4):429–433. doi: 10.1016/s0266-7681(96)80039-8. [DOI] [PubMed] [Google Scholar]
- 6.Papatheodorou L K, Rubright J H, Kokkalis Z T, Sotereanos D G. Resection interposition arthroplasty for failed distal ulna resections. J Wrist Surg. 2013;2(1):13–18. doi: 10.1055/s-0032-1333062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bieber E J, Linscheid R L, Dobyns J H, Beckenbaugh R D. Failed distal ulna resections. J Hand Surg Am. 1988;13(2):193–200. doi: 10.1016/s0363-5023(88)80047-9. [DOI] [PubMed] [Google Scholar]
- 8.van Schoonhoven J, Mühldorfer-Fodor M, Fernandez D L, Herbert T J. Salvage of failed resection arthroplasties of the distal radioulnar joint using an ulnar head prosthesis: long-term results. J Hand Surg Am. 2012;37(7):1372–1380. doi: 10.1016/j.jhsa.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 9.Martínez Villén G, García Martínez B, Aso Vizán A. Total distal radioulnar joint prosthesis as salvage surgery in multioperated patients. Chir Main. 2014;33(6):390–395. doi: 10.1016/j.main.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Kakar S, Fox T, Wagner E, Berger R. Linked distal radioulnar joint arthroplasty: an analysis of the APTIS prosthesis. J Hand Surg Eur Vol. 2014;39(7):739–744. doi: 10.1177/1753193414523189. [DOI] [PubMed] [Google Scholar]
- 11.Scheker L R. Implant arthroplasty for the distal radioulnar joint. J Hand Surg Am. 2008;33(9):1639–1644. doi: 10.1016/j.jhsa.2008.08.014. [DOI] [PubMed] [Google Scholar]


