Abstract
OBJECTIVE:
Functional constipation and fecal incontinence are common childhood gastrointestinal conditions. Both conditions may be associated with behavioral problems. Attention-deficit/hyperactivity disorder (ADHD) is the most common behavioral disorder of childhood, characterized by shortened attention span and hyperactivity. We hypothesize that a diagnosis of ADHD increases the risk for functional constipation and fecal incontinence.
METHODS:
A retrospective cohort study of children was performed by using the military health system database. Children of active-duty military personnel, aged 4 to 12 years, from October 2005 to September 2007, were included. ADHD, constipation, and fecal incontinence were identified by International Classification of Diseases, Ninth Revision, Clinical Modification diagnostic codes. Relative risks and adjusted incidence rate ratios (IRRs) were calculated. A subgroup analysis of subjects receiving medical therapy was performed.
RESULTS:
There were 742 939 children identified in the study, 32 773 (4.4%) of whom had ADHD. Children with ADHD had an increased prevalence of constipation (4.1% of children with ADHD vs 1.5% children without ADHD; P < .001) and fecal incontinence (0.9% of children with ADHD vs 0.15% of children without ADHD; P < .0001). Children with ADHD had more visits than those without ADHD for both constipation (IRR 3.39; 95% confidence interval 2.59–4.43) and fecal incontinence (IRR 7.74; 95% confidence interval 5.01–11.98). Children with ADHD receiving medicinal therapy did not differ significantly from children with ADHD not receiving medicinal therapy on rates of constipation visits (P = .57) or fecal incontinence visits (P = .32).
CONCLUSIONS:
Children with ADHD are significantly more likely to have constipation and fecal incontinence. Medical therapy for ADHD does not impact visit rates for defecation disorders.
Keywords: ADHD, constipation, encopresis, fecal incontinence
What’s Known on This Subject:
Several studies have shown that behavioral problems can be associated with defecation and voiding disorders, although few studies have looked directly at a link between a diagnosis of attention-deficit/hyperactivity disorder (ADHD) and constipation or fecal incontinence.
What This Study Adds:
We identified an increased risk for both constipation and fecal incontinence in children with ADHD. In patients with concomitant ADHD and defecation disorders, more aggressive medical and behavioral treatment of the constipation or fecal incontinence may be warranted.
Constipation is a common problem among children in the United States. It is estimated that 0.7% to 29.6% of children suffer from constipation.1 Constipation can be defined by difficulty or pain with passage, as well as consistency and frequency of bowel movements. In children, it also can be characterized by volitional stool retention.2 Functional constipation, or constipation not due to other anatomic, medical, or medication effects, is the most common form in childhood.3 Constipation is often associated with other symptoms, including abdominal pain, retentive fecal soiling, or painful defecation. Fecal incontinence is the involuntary passage of stool beyond the age at which one may reasonably expect a child to be toilet trained. This age is most often accepted as 4 years old.2 Constipation and fecal incontinence often coexist and their associated symptoms can be frustrating for patients, parents, and physicians. These conditions also lead to multiple doctors’ visits, excessive health care utilization costs, and may also detrimentally affect quality of life.4–6
Functional constipation in children is multifactorial, often developing from a combination of a diet insufficient in fiber and behavioral withholding of stool.7 Practitioners experienced in the treatment of constipation in children know that management of the behavioral aspects of constipation are as important as the medical and dietary aspects.8 Few studies have evaluated the relationship between pediatric constipation, fecal incontinence, and other behavioral, psychological, or emotional disorders. In 1966, Bellman9 reported that 75 boys with the diagnosis of fecal incontinence were more likely to demonstrate school disturbances. In 1984, Abrahamian and Lloyd-Still10 noted that 20% of children with chronic constipation had “significant psychological problems on the basis of behavior problems at home or at school.” Studies that have used the Child Behavior Checklist or other similar questionnaires to evaluate behavioral or other emotional problems have associated higher (more severe) behavioral scores with constipation, fecal incontinence, and voiding.11–13 Most recently in 2013, Peeters et al14 reported that a large number of children presenting with defecation disorders also fall into the autism spectrum disorder.
Attention-deficit/hyperactivity disorder (ADHD) is a problem in which children exhibit inattentiveness, overactivity, impulsivity, or difficulty focusing. ADHD is also the most commonly diagnosed behavioral disorder of childhood.15 No study has evaluated an association between the diagnosis of ADHD and defecation disorders, such as constipation and fecal incontinence. By using a large health care billing database, we sought to evaluate the association of a diagnosis of ADHD with constipation or fecal incontinence.
Methods
A retrospective cohort study was performed by using data from the TRICARE Management Activity military health system (MHS) database. The TRICARE Management Activity oversees health care delivery for US uniformed services members and their families in the United States and abroad. Uniformed services beneficiaries aged 4 to 12 years who were enrolled in the MHS during fiscal years 2006–2007 (October 1, 2005–September 30, 2007) were identified. Age was determined at the beginning of the study period. Dependent children of National Guard or Reserve military personnel were excluded because of the short length and higher variation of eligibility periods.
Children with ADHD were identified by 2 or more ADHD visits during the study period using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 314.00, 314.01, 314.1, 314.2, 314.8, or 314.9. Children were identified as those having visited a provider with a diagnosis of constipation (ICD-9-CM codes: 564.0, 564.00, 564.01, 564.02, or 564.09) and fecal incontinence (ICD-9-CM codes: 307.7 or 787.6). Each child, with and without ADHD, was classified as either having or not having had a constipation or fecal incontinence diagnosis during the study period. The total number of visits each child had by type of complaint was extracted. Constipation and fecal incontinence visit rates were calculated by using total numbers of visits and length of time enrolled in the MHS.
Prescription data were obtained also for patients with a diagnosis of ADHD and was used to identify children with ADHD as using or not using ADHD medication. Included medications were identified as primary treatment of ADHD by using the American Hospital Formulary Service therapeutic class codes for methylphenidates, amphetamines, and atomoxetine; clonidine and α-agonists were included as well. Additional demographic and socioeconomic variables collected were marital status of parents, military rank of the parent, and birth order of the child. Marital status and firstborn status were included specifically to adjust for health care utilization; in previous studies we have found that there is an association with an increased health care utilization/visit rate.16,17
Prevalence of constipation and fecal incontinence was calculated by using χ2 analyses. Unadjusted relative risks (RRs) along with 95% confidence intervals (CIs) were calculated for both constipation and fecal incontinence. The adjusted incidence rate ratio (IRR) of visits for constipation and fecal incontinence were calculated by random-effects Poisson regression modeling. The dependent variables were visit number for either constipation or fecal incontinence. The independent variables were a diagnosis of ADHD and the child’s age and gender, along with the additional demographic variables listed previously. P < .05 was considered statistically significant. Analyses were conducted by using Stata Intercooled 10 (Stata Corp, College Station, TX). The study was reviewed and approved by the responsible institutional review boards.
Results
There were 742 939 children aged 4 to 12 years identified as eligible to receive medical care in the MHS during the study period. Of these children, 32 773 (4.4%) met criteria for an ADHD diagnosis. Demographic data are summarized by ADHD status and medication use in Table 1. Children with ADHD were significantly older, more likely to be boys, and more likely to be the firstborn in their families. They also were more likely to have parents who were junior enlisted rank and married. Of children with ADHD, those who took medication were significantly older and more likely to be boys. Use of medication was not associated with their parent’s military rank, or marital status, or the child's birth order. There were 12 805 (1.7%) children who saw a provider for either constipation (11 851) or fecal incontinence (1331) during the study period. Table 2 reports demographics of children by constipation or fecal incontinence diagnosis. Children who had a diagnosis of constipation or fecal incontinence were significantly older and less likely to be the firstborn child in the family. They also were more likely to have parents who were married and of junior enlisted rank.
TABLE 1.
Demographic Characteristics of Children With and Without ADHD
| Children Without Diagnosed ADHD | Children With Diagnosed ADHD | Children With ADHD Not on Medication | Children With ADHD on Medication | |
|---|---|---|---|---|
| n | 710 166 | 32 773 | 6408 | 26 365 |
| Age, y, median (IQR) | 7 (5–9) * | 8 (6–9) * | 8 (6–9)* | 8 (6–10)* |
| % Male | 50.1* | 73.7* | 71.2* | 74.3* |
| % Junior enlisted military parent | 2.86* | 4.55* | 4.7 | 4.5 |
| % Married parents | 83.5* | 85.1* | 85.3 | 85.1 |
| % Firstborn | 39.3* | 42.2* | 43.3 | 42.2 |
Comparisons made between patients with and without ADHD and those with and without ADHD on medication were performed by using either the χ2 test for categorical variables or Wilcoxon rank-sum test for continuous variables. *P < .001. IQR, interquartile range.
TABLE 2.
Demographic Characteristics of Children With Constipation or Fecal Incontinence
| Children Without Constipation/Fecal Incontinence | Children With Constipation/Fecal Incontinence | |
|---|---|---|
| n | 730 134 | 12 805 |
| Age, y, median (IQR) | 7 (5–9) | 7 (5–9) |
| % Male | 51.3 | 51.2 |
| % Junior enlisted military parent | 2.9* | 3.5* |
| % Married parents | 83.5* | 87.5* |
| % Firstborn | 39.4* | 43.1* |
Comparisons made between patients with and without constipation or fecal incontinence were performed by using either χ2 test for categorical variables or Wilcoxon rank-sum test for continuous variables. *P < .001. IQR, interquartile range.
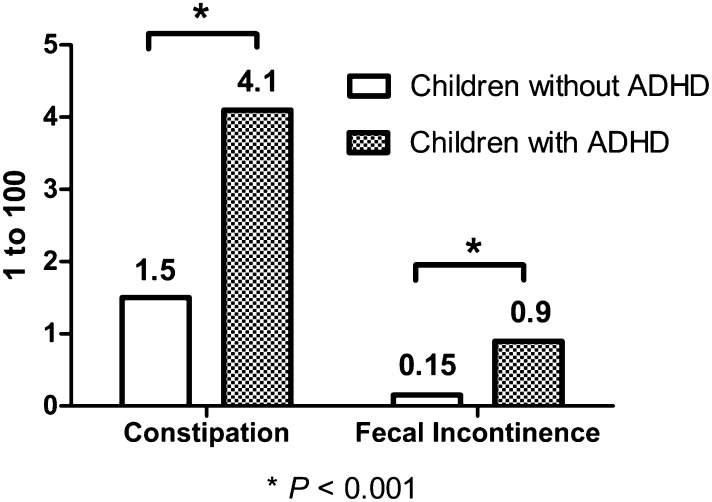
Children with ADHD had an increased prevalence of constipation, with 1356 (4.1%) of them seeing providers for constipation as compared with 10 495 (1.5%) children without ADHD (RR 2.88; 95% CI 2.72–3.05; P < .001) (Fig 1). Children with ADHD also had 84 visits for constipation per 1000 person-years, whereas children without ADHD had 30 visits per 1000 person-years in crude rate analysis (IRR 2.78; 95% CI 2.70–2.88; P < .001). Results of unadjusted and adjusted Poisson regression for the effect on visit rate constipation are presented in Table 3. In adjusted regression analysis accounting for the effects of age and gender, parent rank, parental marital status, and birth order, ADHD was associated with a higher rate of constipation visits (IRR 2.96; 95% CI 2.60–3.38; P < .001).
FIGURE 1.
Prevalence of constipation and fecal incontinence by ADHD status.
TABLE 3.
Unadjusted and Adjusted IRRs for Constipation Provider Visits
| Unadjusted IRR | Adjusted IRR | |
|---|---|---|
| ADHD | 2.79 (2.52–3.08) | 3.39 (2.59–4.43) |
| Boys versus girls | 0.94 (0.89–0.99) | 0.77 (0.68–0.90) |
| Age | 0.82 (0.81–0.83) | 0.73 (0.69–0.77) |
| Junior enlisted versus higher military rank | 2.04 (1.79–2.33) | 0.83 (0.69–1.01) |
| Firstborn child | 1.24 (1.17–1.32) | 1.31 (1.15–1.49) |
| Married parents | 1.71 (1.54–1.89) | 1.88 (1.41–2.49) |
Unadjusted and adjusted IRRs were calculated by using random-effects Poisson regression modeling. The adjusted model included all variables listed in the table. Firstborn child and married status of parents were included in the model to adjust for increased health care use seen in these groups.
Children with ADHD also had an increased prevalence of fecal incontinence, with 292 (0.9%) seeing providers for fecal incontinence, as compared with 1035 (0.15%) children who did not have ADHD (RR 6.19; 95% CI 5.44–7.05; P < .001). Children with ADHD had 28 visits for fecal incontinence per 1000 person-years and children without ADHD had 4 visits per 1000 person-years in crude rate analysis (IRR 6.96; 95% CI 6.55–7.40; P < .001). Results of unadjusted and adjusted Poisson regression for the effect on visit rate for fecal incontinence are presented in Table 4. In adjusted regression analysis accounting for the effects of parental rank, marital status, child age, gender, and birth order, ADHD was associated with a higher rate of fecal incontinence visits (IRR 6.52; 95% CI 4.90–8.67; P < .001).
TABLE 4.
Unadjusted and Adjusted IRRs for Fecal Incontinence Provider Visits
| Unadjusted IRR | Adjusted IRR | |
|---|---|---|
| ADHD | 6.96 (5.59–8.67) | 7.74 (5.01–11.98) |
| Boys versus Girls | 2.06 (1.70–2.51) | 1.56 (1.07–2.28) |
| Age | 0.87 (0.85–0.90) | 0.76 (0.68–0.85) |
| Junior enlisted versus higher military rank | 1.57 (1.09–2.26) | 0.77 (0.45–1.28) |
| Firstborn child | 1.18 (0.99–1.41) | 1.30 (0.93–1.81) |
| Married parents | 1.64 (1.23–2.17) | 2.14 (1.14–4.01) |
Unadjusted and adjusted IRRs were calculated by using random-effects Poisson regression modeling. The adjusted model included all variables listed in the table. Firstborn child and married status of parents were included in the model to adjust for increased health care use seen in these groups.
Of the 32 773 children with ADHD, 26 365 (80.4%) were prescribed a medication for treatment of ADHD. The rate of constipation was the same in children with ADHD prescribed medications (1099; 4.2%) compared with children not prescribed medication (259; 4.1%), with an RR of 1.02 (95% CI 0.90–1.17; P = .72). Children with ADHD on medication also did not differ significantly from children with ADHD not on medication in the rate of constipation visits (84 vs 80 per 1000 person-years; IRR 1.06; 95% CI 0.867–1.3; P = .565). The rate of fecal incontinence also was the same in children with ADHD prescribed medication (247; 0.9%) compared with children not prescribed medication (47; 0.7%), with an RR of 1.28 (95% CI 0.90–1.75; P = .12). Children with ADHD prescribed medication had significantly fewer visits for fecal incontinence compared with children with ADHD who were not taking medication (26 vs 36 per 1000 person-years; IRR 0.75; 95% CI 0.66–0.85; P < .001). In multivariate Poisson regression modeling, however, the effect of medication treatment of ADHD on the rate of visits for fecal incontinence was not found to be significantly related to medication use (IRR 0.56; 95% CI 0.24–1.31; P = .321).
Discussion
In our population -based study, we demonstrate an association of ADHD with a diagnosis of constipation and fecal incontinence. We also show that children with ADHD visit a medical provider for constipation or fecal incontinence at an increased rate. Medical therapy for ADHD does not appear to have any positive or negative impact on the visit rate for constipation; however, there is a suggestion that medical therapy for ADHD may decrease the rate of provider visits for fecal incontinence. Although several studies, previously discussed, have used the Child Behavior Checklist or other behavioral questionnaires to evaluate an association between hyperactivity and constipation or fecal incontinence,11,13 our study is the first to have evaluated specifically the association of an ADHD diagnosis with constipation or fecal incontinence, as well as its association with any medical treatment of ADHD.
This association between behavior problems such as ADHD and defecation disorders could have several potential explanations. There is evidence that a unified neurobiological disorder may play a role in this relationship.18 Furthermore, this association also could be explained by an altered communication between the central nervous system and the enteric nervous system. This may result in delayed gastrointestinal motility or altered perception of intestinal distention, including signaling of rectal distention.
A study by Becker et al13 tested emotional responses to certain pictorial and acoustic stimuli in children with defecation disorders and controls. Becker et al13 showed that those with fecal incontinence and constipation had higher event evoked potentials when compared with controls, suggesting a relationship between central nervous system processing of emotions and the enteric nervous system. Another case report describes a pediatric patient who was placed on sertraline, a selective serotonin reuptake inhibitor, who then demonstrated marked improvement of fecal incontinence.19 This latter report provides additional support for an altered peripheral or enteric nervous system as a possible link for ADHD and fecal incontinence. The known association of ADHD with urinary voiding dysfunction provides reinforcement for a unified neurobiological disorder.12 Additionally, ADHD and defecation disorders may be linked as neurodevelopmental disorders because they both decrease in prevalence with age.20,21
Another possibility is that ADHD, as a behavioral disorder, leads to defecation disorders. Children with ADHD may not respond as promptly to physical cues of either defecation or urination, and have difficulty interrupting current more desirable tasks. Children with ADHD may be unable to focus on defecatory urges long enough to carry out normal evacuation. The risk of fecal incontinence is higher than constipation alone in children with ADHD, which could support behavioral and voluntary withholding of stool as an etiology. It is also possible that children with ADHD may have less motivation regarding toilet training. The results seen in this study suggest that medication used to treat ADHD does not have a significant impact on number of visits to a provider for constipation but may impact visits for fecal incontinence.
Although less likely, Johnston and Wright18 suggest the possibility that fecal incontinence may lead to the misbehaviors diagnosed as ADHD because of negative responses to soiling or a child’s shame. This would suggest that treatment of fecal soiling would lead to resolution of ADHD and there is little current evidence to support this hypothesis.
Nutritional status also may potentially influence constipation/fecal incontinence in those with ADHD. There are studies that have suggested that children with ADHD have lower levels of zinc and copper,22 as well as a decreased intake of Vitamin C.23 It is possible that dietary intake in children with ADHD may be an unidentified confounder for constipation and fecal incontinence.
Our findings have several implications for clinical practice. Educating parents and providers about this association can lead to better screening and treatment of constipation and fecal incontinence in individuals with ADHD. In patients who repeatedly present or require specialist referral for medical management for constipation and fecal incontinence, screening for ADHD may be helpful. In patients with concomitant ADHD and defecation disorders, more aggressive medical treatment of the constipation or fecal incontinence may be warranted, as evidenced by the much higher visit rate, which suggests a persistence of symptoms in these patients. In addition to medical management, more specific and aggressive behavioral approaches to management of defecation disorders in patients with ADHD could be considered. It is possible that typical reinforcement programs, focusing on toilet-sitting regimens, dietary changes, and medication compliance, may be more difficult for children with ADHD. In cases of more severe behavioral difficulties along with defecation disorders, earlier referral to a pediatric mental health specialist may be helpful for the child as well as the parents.
Our study has several limitations. As a retrospective study using billing data, we are dependent on ICD-9-CM coding. This can allow for misclassification of patient diagnoses. We could not interpret how a child was diagnosed with ADHD, constipation, fecal incontinence, or verify whether the fecal incontinence was retentive. We attempted to limit false diagnoses for ADHD by a definition that required 2 separate diagnoses at 2 different visits. Our evaluation for the effect of medication on defecation disorders was based on visit numbers. It is possible that there is actually a clinical improvement or worsening of defecation disorders with medical treatment of ADHD, which did not translate to the number of clinic visits. We also considered medication status to be a dichotomous variable, and the shortened time frame did not account for the constipation visit rate in periods before and after the initiation of ADHD medication. TRICARE is a universal health care system without copays, which could encourage parents to use health care visits at higher rates than other insurance options, and our reported visit rates may not be comparable to other populations. We did attempt to control for factors that could affect health care utilization, such as firstborn and marital status of the parents. Additionally, because our population was principally military members, there could be a selection bias due to different toilet-training regimens or discipline within the home found only in military culture.
A major strength of this study is the use of a very large health care database. The MHS is demographically and socioeconomically diverse and represents a geographically dispersed population of children. Although universal coverage is mentioned as a limitation previously, this could also be considered a strength; without any access to care bias our study was able to identify children with constipation or fecal incontinence who economically might otherwise not be able to visit a provider.
Conclusions
Having a diagnosis of ADHD increases a child’s likelihood of having constipation and fecal incontinence. Medical treatment of ADHD does not significantly increase or decrease visit rate for defecation disorders. Further studies regarding the effect of medical treatment of ADHD and clinical changes in outcomes for defection disorder should be performed.
Glossary
- ADHD
attention-deficit/hyperactivity disorder
- CI
confidence interval
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- IRR
incidence rate ratio
- MHS
military health system
- RR
relative risk
Footnotes
Dr McKeown interpreted analysis results, and drafted and edited the manuscript; Dr Hisle-Gorman conceptualized and designed the study, performed analysis and interpretation of the data, and revised the final manuscript; Ms Eide designed the data collection instruments, collected and organized the data, and revised the final manuscript; Dr Gorman conceptualized and designed the study, submitted institutional review board protocol, and edited the manuscript; Dr Nylund conceptualized and designed the study, directed data analysis, and edited the manuscript; and all authors approved the final manuscript.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the US Air Force, US Navy, Department of Defense, or the US government. Title 17 U.S.C. 105 provides that “copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. 101 defines a US government work as “a work prepared by a military service member or employee of the United States government as part of that person's official duties.” This work was prepared as part of our official duties.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Mugie SM, Benninga MA, Di Lorenzo C. Epidemiology of constipation in children and adults: a systematic review. Best Pract Res Clin Gastroenterol. 2011;25(1):3–18 [DOI] [PubMed] [Google Scholar]
- 2.Rasquin A, Di Lorenzo C, Forbes D, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130(5):1527–1537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Di Lorenzo C. Pediatric anorectal disorders. Gastroenterol Clin North Am. 2001;30(1):269–287, ix [DOI] [PubMed] [Google Scholar]
- 4.Liem O, Harman J, Benninga M, Kelleher K, Mousa H, Di Lorenzo C. Health utilization and cost impact of childhood constipation in the United States. J Pediatr. 2009;154(2):258–262 [DOI] [PubMed] [Google Scholar]
- 5.Wald A, Sigurdsson L. Quality of life in children and adults with constipation. Best Pract Res Clin Gastroenterol. 2011;25(1):19–27 [DOI] [PubMed] [Google Scholar]
- 6.Rajindrajith S, Devanarayana NM, Benninga MA. Review article: faecal incontinence in children: epidemiology, pathophysiology, clinical evaluation and management. Aliment Pharmacol Ther. 2013;37(1):37–48 [DOI] [PubMed] [Google Scholar]
- 7.Rajindrajith S, Devanarayana NM. Constipation in children: novel insight into epidemiology, pathophysiology and management. J Neurogastroenterol Motil. 2011;17(1):35–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Lorenzo C. Childhood constipation: finally some hard data about hard stools! J Pediatr. 2000;136(1):4–7 [DOI] [PubMed] [Google Scholar]
- 9.Bellman M. Studies on encopresis. Acta Paediatr Scand. 1966;(suppl 170):1. [PubMed] [Google Scholar]
- 10.Abrahamian FP, Lloyd-Still JD. Chronic constipation in childhood: a longitudinal study of 186 patients. J Pediatr Gastroenterol Nutr. 1984;3(3):460–467 [DOI] [PubMed] [Google Scholar]
- 11.Benninga MA, Voskuijl WP, Akkerhuis GW, Taminiau JA, Büller HA. Colonic transit times and behaviour profiles in children with defecation disorders. Arch Dis Child. 2004;89(1):13–16 [PMC free article] [PubMed] [Google Scholar]
- 12.Duel BP, Steinberg-Epstein R, Hill M, Lerner M. A survey of voiding dysfunction in children with attention deficit-hyperactivity disorder. J Urol. 2003;170(4 pt 2):1521–1523, discussion 1523–1524 [DOI] [PubMed] [Google Scholar]
- 13.Becker A, Rubly M, El Khatib D, Becker N, von Gontard A. Central nervous system processing of emotions in children with faecal incontinence. Acta Paediatr. 2011;100(12):e267–e274 [DOI] [PubMed] [Google Scholar]
- 14.Peeters B, Noens I, Philips EM, Kuppens S, Benninga MA. Autism spectrum disorders in children with functional defecation disorders. J Pediatr. 2013;163(3):873–878 [DOI] [PubMed] [Google Scholar]
- 15.Wolraich M, Brown L, Brown RT, et al. Subcommittee on Attention-Deficit/Hyperactivity Disorder. Steering Committee on Quality Improvement and Management . ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007–1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eide M, Gorman G, Hisle-Gorman E. Effects of parental military deployment on pediatric outpatient and well-child visit rates. Pediatrics. 2010;126(1):22–27 [DOI] [PubMed] [Google Scholar]
- 17.Mazen A, Nylund C, Eide M, Hisle-Gorman E, Gorman G. Abdominal pain and constipation outpatient visits during military deployments in children aged 3-8 years old. J Pediatr Gastroenterol Nutr. October 20–23, 2011;53(1):E-65 [Google Scholar]
- 18.Johnston BD, Wright JA. Attentional dysfunction in children with encopresis. J Dev Behav Pediatr. 1993;14(6):381–385 [PubMed] [Google Scholar]
- 19.Mendhekar DN, Gupta N. Use of sertraline in childhood retentive encopresis. Ann Pharmacother. 2010;44(2):395. [DOI] [PubMed] [Google Scholar]
- 20.Rowland AS, Lesesne CA, Abramowitz AJ. The epidemiology of attention-deficit/hyperactivity disorder (ADHD): a public health view. Ment Retard Dev Disabil Res Rev. 2002;8(3):162–170 [DOI] [PubMed] [Google Scholar]
- 21.Bongers ME, van Wijk MP, Reitsma JB, Benninga MA. Long-term prognosis for childhood constipation: clinical outcomes in adulthood. Pediatrics. 2010;126(1). Available at: www.pediatrics.org/cgi/content/full/126/1/e156 [DOI] [PubMed] [Google Scholar]
- 22.Kiddie JY, Weiss MD, Kitts DD, Levy-Milne R, Wasdell MB. Nutritional status of children with attention deficit hyperactivity disorder: a pilot study. Int J Pediatr. 2010;2010:767318 [DOI] [PMC free article] [PubMed]
- 23.Kim Y, Chang H. Correlation between attention deficit hyperactivity disorder and sugar consumption, quality of diet, and dietary behavior in school children. Nutr Res Pract. 2011;5(3):236–245 [DOI] [PMC free article] [PubMed] [Google Scholar]