Since 1999,1 the Canadian Hypertension Education Program (CHEP) has released guidelines on the diagnosis and management of hypertension. The 2015 guidelines, released earlier this year,2 therefore represent the 17th annual synthesis of the evidence to date in this area. These guidelines, along with other knowledge translation activities by Hypertension Canada, have been credited as contributing factors for our nation’s improving rates of hypertension control, treatment and awareness—estimated at 64.6%, 79.0% and 82.5%, respectively.3 On all CHEP guidelines published to date, multidisciplinary expert panels including physicians, nurses and pharmacists have been involved in evidence synthesis and dissemination. Indeed, an expanding role for pharmacists has been identified as a strategy to further improve the detection and treatment of hypertension among Canadians, due to strong evidence of the beneficial effects of pharmacist interventions in this area.4-9
The Canadian Pharmacists Journal has regularly published versions of the CHEP guidelines specifically for pharmacists, with the most recent full set of guidelines published in 201110 and regular updates since.11,12 This article highlights the changes integrated into the current 2015 guidelines since the 2014 publication. Readers requiring a complete set of guidelines are encouraged to consult these earlier pharmacist-specific publications or the full CHEP guidelines in the Canadian Journal of Cardiology2 or at www.hypertension.ca.
Preference for the use of electronic (oscillometric) monitors over manual (auscultatory) measurement for in-office blood pressure assessment
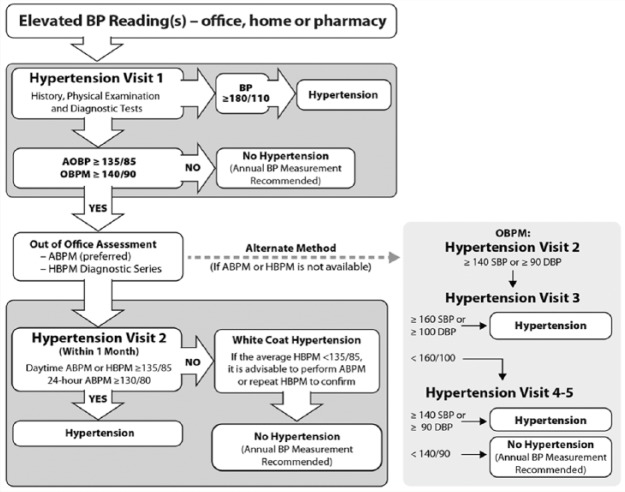
An overview of the criteria for hypertension diagnosis and follow-up is presented in Figure 1. Readers will recognize that the physician’s office, the patient’s home and the pharmacy are specifically indicated as sites for blood pressure (BP) assessment and that the new figure has some significant differences from previous guidelines, which are summarized below. Note also in the figure that office blood pressure measurement (OBPM) refers to either manual or electronic measurement with the clinician initiating each measurement, whereas automated office blood pressure (AOBP) refers to unattended electronic measurement where the clinician initiates a sequence of automated measurements and then leaves the room after verifying that the BP is being captured. Automated office devices record multiple readings (usually between 3 and 6) and calculate the mean systolic/diastolic BP, excluding the first reading.
Figure 1.
Criteria for the diagnosis of hypertension
ABPM, ambulatory blood pressure measurement; AOBP, automated office blood pressure (unattended); HBPM, home blood pressure measurement; OBPM, office blood pressure measurement (manual or automatic, attended). Originally published in the Canadian Journal of Cardiology.2 Used with permission.
A recent review highlighted a number of factors influencing the accuracy of manual office readings.13 While validated manual devices possess accuracy within the strict protocol of a validation study (also often described as “standardized” manual measurement), real-world practice introduces factors that may influence the results obtained, such as clinician and patient conversation during measurement, recording of only a single reading, insufficient patient rest prior to measurement, too-rapid cuff deflation and digit preference (the rounding of readings to final digits of 0 or 5). This review found that manual readings obtained in practice are on average 9/6 mmHg higher than those obtained within research studies under strict protocols. Because of the inaccuracies introduced into BP measurement when auscultation is used in everyday clinical practice and because educational programs teaching proper auscultatory technique have not had sustained impact, the use of electronic (oscillometric) upper arm office devices is preferred over manual (auscultatory) measurements. A new recommendation has been made in the 2015 guidelines to this effect (Table 1).
Table 1.
Summary of updates to the 2015 Canadian Hypertension Education Program (CHEP) guidelines
| CHEP 2014 | CHEP 2015 |
|---|---|
| Accurate measurement of BP | |
| Automated OBPM can be used in the assessment of office BP (Grade D). | Measurement using electronic (oscillometric) upper arm devices is preferred over auscultation (Grade C) [New Recommendation]. |
| Criteria for diagnosis of hypertension and recommendations for follow-up | |
|
|
| Global vascular protection therapy for adults with hypertension without compelling indications for specific agents | |
|
|
ABPM, ambulatory blood pressure monitoring; AOBP, automated office blood pressure; BP, blood pressure; CKD, chronic kidney disease; DBP, diastolic blood pressure; HBPM, home blood pressure monitoring; OBPM, office BP measurement; SBP, systolic blood pressure.
Bold text represents changes to the 2015 guidelines from the 2014 guidelines.
Looking at automated devices, a study of the BpTRU automated office monitor among 481 patients found that the BpTRU resulted in measurements that were 10.8/3.1 mmHg lower than manual readings, on average.14 This indicates that AOBP eliminates much of the error associated with manual measurement. Automated device readings were also found to be better correlated to awake ambulatory BP than manual readings, and preliminary data suggest that automated office BP measurements are as well correlated with target organ damage (left ventricular mass index) as ambulatory BP monitoring and better correlated than manual readings.15 Minimizing those factors listed above, reducing the “white-coat” effect and maximizing workflow efficiency (because the clinician can attend to other tasks while measurements are being taken) are the key benefits of automated devices for in-office use.
Pharmacists are reminded that even when an automated device is used, a minimum of 3 measurements should be taken, with the first measurement discarded and the remainder averaged. Readers requiring guidance on various devices available and their validation status can consult the listings of the dabl Educational Trust (www.dableducational.org/sphygmomanometers.html) or the British Hypertension Society (www.bhsoc.org/bp-monitors/bp-monitors/).
Out-of-office measurement (24-hour ambulatory blood pressure or home blood pressure) should be performed to confirm the initial diagnosis in any individual suspected of having hypertension
As noted in Figure 1, out-of-office BP measurement through the use of 24-hour ambulatory blood pressure monitoring (ABPM) or home blood pressure monitoring (HBPM) is recommended to verify the diagnosis of hypertension after an initial finding of elevated BP in-office and prior to a second in-office reading. This represents a significant change from previous guidelines. Previously, hypertension could be diagnosed using multiple readings averaged over serial office visits or through use of out-of-office measurement. Additional in-office visits to confirm a diagnosis of hypertension are now only advised in those scenarios where ambulatory or home monitoring is unavailable, and the CHEP guidelines stress that this is not the preferred way of ruling in the diagnosis. Of the 2 options for out-of-office measurement, ambulatory monitoring is preferred over home monitoring because it provides more readings overall as well as information on nocturnal BP.
A study of 38 patients with hypertension compared different modes of BP measurement to measures of target organ damage including microalbuminuria, left ventricular hypertrophy, left ventricular mass and retinal damage.16 Each patient completed 3 averaged manual clinic readings, 3 home measurements over each of 2 days within the same week and 24-hour ABPM. Systolic BP readings obtained via ABPM and HBPM were both significantly lower than those obtained in clinic. The study found no correlation between clinic measurements and albumin excretion or left ventricular mass, whereas HBPM correlated significantly with both of these parameters. ABPM also correlated significantly with both left ventricular mass and albumin excretion, to an even greater extent than HBPM. Therefore, ABPM is noted by CHEP as the preferred method for out-of-office measurement. ABPM monitoring also represents an excellent opportunity for pharmacists to provide this service to their patients, since many clinics do not have access to these devices.
In addition to their greater predictive value for target organ damage, out-of-office measurements also assist with the identification of both white-coat and masked hypertension. Recall that white-coat hypertension is the presence of elevated BP in office while normotensive outside of the office, while masked hypertension is the presence of elevated BP out of office but normotensive BP in-office. The potential consequences of treating patients with white-coat hypertension range from the cost of unnecessary drug therapy to adverse effects secondary to treatment. Although masked hypertension is less common than white-coat hypertension, the 10-year incidence of cardiovascular mortality and stroke from masked hypertension was found to be similar to that from sustained hypertension, whereas patients with white-coat hypertension were found to have similar risks to the normotensive population.17 Therefore, the ability of out-of-office measurements to detect masked hypertension is also highly valuable. Risk factors identified in the literature for both white-coat and masked hypertension are presented in Table 2.18-21 The potential for misdiagnosis of both conditions through the sole use of office measurements therefore warrants the use of out-of-office verification whenever hypertension is suspected.
Table 2.
Risk factors for white-coat and masked hypertension
| White-coat hypertension18 | Masked hypertension19-21 |
|---|---|
| Female | Male |
| Older adults | Older adults |
| Nonsmokers | High-normal clinic blood pressure measurements |
| Patients with mild hypertension | Higher body mass index |
| Pregnant women | Smoking |
| Patients without evidence of target organ damage | Excess alcohol consumption |
| Diabetes | |
| Patients recently diagnosed with hypertension using a limited number of routine office blood pressure measurements | Peripheral arterial disease |
| Orthostatic hypotension | |
| Left ventricular hypertrophy |
Global cardiovascular risk management and vascular protection are key; therefore, advice and treatment for smoking cessation should be part of hypertension management
It is well known that elevated BP is rarely the only cardiovascular risk factor present among patients with hypertension—8 of 10 patients with diagnosed hypertension possess at least 1 other cardiovascular risk factor.22 Such risk factors can be clinical (e.g., diagnoses of diabetes, dyslipidemia, obesity) or lifestyle-based (e.g., smoking, excessive alcohol consumption, sodium intake, physical inactivity).
The 2015 guidelines have added 2 statements, related to asking patients about their smoking status regularly with advice to quit and the provision of both advice and pharmacotherapy to patients who smoke with the goal of cessation (Table 1). A Cochrane systematic review examined randomized controlled trials of smoking cessation advice from physicians, which assessed patients’ abstinence at least 6 months following the provision of the advice.23 Trials were included if they compared physician advice to stop smoking versus no advice or usual care, or compared differing levels of advice. Studies were excluded if they compared advice alone to advice plus nicotine replacement therapy (NRT) or if smoking cessation advice was provided in combination with multifactorial lifestyle advice such as dietary and exercise advice. The authors defined consultations of 20 minutes’ duration or less, with or without leaflet provision, and with up to 1 follow-up visit as “minimal intervention,” while consultations of greater than 20 minutes’ duration, with the use of additional materials other than a leaflet, or with more than 1 planned follow-up visit, were deemed “intensive.” Primary outcomes were smoking cessation or reduction in the number of cigarettes smoked at least 6 months following the provision of advice. Twenty-six trials of approximately 22,000 patients were included in the analysis of advice versus no advice or usual care. Meta-analysis found statistically significant increases in quit rates among the 17 studies evaluating minimal intervention versus control (relative risk 1.66, 95% CI 1.42-1.94) and even greater improvements among the 11 studies evaluating intensive intervention versus control (relative risk 1.86, 95% CI 1.60-2.15).
The recommendation that advice be provided in combination with pharmacotherapy is based, in part, on an overview of Cochrane systematic reviews of the effectiveness and safety of various pharmacotherapies for smoking cessation versus placebo.24 The primary effectiveness outcome was continuous and prolonged smoking cessation of at least 6 months’ duration, and the primary safety outcome examined was the incidence of serious adverse events associated with each treatment. Reviews were included if they compared NRT, bupropion or varenicline with each other or with placebo. Network meta-analyses were performed to compare benefits of each treatment with the others. Twelve reviews comprising 267 studies of over 100,000 participants were included. All 3 pharmacologic options demonstrated significant benefits over placebo, with bupropion and NRT showing equal efficacy (OR 0.99, 95% CI 0.86-1.13). Varenicline demonstrated superior efficacy to single forms of NRT where only 1 form of NRT is used (OR 1.57, 95% CI 1.29-1.91) but was not more effective than combination NRT where 2 or more NRT forms were used together (OR 1.06, 95% CI 0.75-1.48). Varenicline was also demonstrated to be superior to bupropion (OR 1.59, 95% CI 1.22-1.87). Meta-analyses of severe adverse events from bupropion and varenicline did not identify excess neuropsychiatric or cardiovascular event risks of either agent compared with placebo. The authors therefore concluded that all available options are effective for smoking cessation therapy, with combination NRT or varenicline being the most effective. Based on the current evidence, none of the available treatments appear to present a significant risk of severe adverse events that should mitigate their use in the general population. However, clinicians are reminded to consider an individual patient’s history of psychiatric illness when making patient-specific pharmacotherapy decisions.
As a result of evidence linking smoking status to elevated BP and major cardiovascular events,25-30 coupled with the evidence on the effectiveness and safety of smoking cessation interventions presented above, pharmacists are advised to regularly inquire about their hypertensive patients’ smoking status and encourage quitting with both advice and pharmacotherapy. Evidence on the pharmacist’s role in smoking cessation31 and expanding scopes of practice in various provinces allowing for pharmacist prescribing of smoking cessation therapies and, in some cases, remuneration for smoking cessation advice further support the role pharmacists can play in global cardiovascular risk reduction.
Conclusions
The 2015 Canadian Hypertension Education Program guidelines present 3 key changes of relevance to pharmacists:
Preference for electronic BP monitors
The central role of out-of-office (ambulatory) BP measurement prior to a second in-office visit to confirm the diagnosis of hypertension
A focus on global cardiovascular risk reduction among patients with hypertension, with a particular emphasis on smoking cessation
Key messages from the 2015 guidelines are also highlighted in Table 3. Readers are encouraged to consult the full guidelines at the Canadian Journal of Cardiology,2 or at www.hypertension.ca, where they will also find additional professional and patient resources on hypertension. Education for pharmacists on hypertension assessment and management can be found on the Hypertension Canada webpage in the form of documents, video presentations and the new 15-hour Professional Education Program, developed in partnership with the Société Québécoise d’Hypertension Artérielle and at the annual Canadian Hypertension Congress. ■
Table 3.
Canadian Hypertension Education Program (CHEP) 2015 key messages
| • All Canadian adults should have their BP assessed at all appropriate clinical visits. Electronic (oscillometric) measurement methods are preferred to manual measurement. |
| • Out-of-office measurement (24-hour ABPM or HBPM) should be performed to confirm the initial diagnosis in any individual suspected of having hypertension. |
| • Optimum management of hypertension requires assessment of overall cardiovascular risk. |
| • Treat to target (<140/90 mmHg or <130/80 mmHg in patients with diabetes. In the very elderly—defined as age >80 years—initiate treatment if systolic BP is >160 mmHg to a target of <150 mmHg). |
| • Health behaviour modification is effective in preventing hypertension, treating hypertension and reducing cardiovascular risk. |
| • Combinations of both health behaviour changes and drugs are generally necessary to achieve target blood pressures. |
| • Focus on adherence. |
| • Be active in hypertension continuing professional development. |
| • Have your patients sign up at www.hypertension.ca to access the latest hypertension resources. |
ABPM, ambulatory blood pressure monitoring; BP, blood pressure; HBPM, home blood pressure monitoring.
Footnotes
Author Contributions:S. Houle, R. Padwal and L. Poirier drafted the manuscript. All authors reviewed, edited and approved the final version of the manuscript.
Declaration of Conflicting Interests:The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding:The authors received no financial support for the research, authorship and/or publication of this article.
References
- 1. Campbell NR, Burgess E, Choi BCK, et al. Methods and an overview of the Canadian recommendations. CMAJ 1999;160(9 suppl):S1-S6. [PMC free article] [PubMed] [Google Scholar]
- 2. Daskalopoulou SS, Rabi DM, Zarnke KB, et al. The 2015 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention and treatment of hypertension. Can J Cardiol. 2015;31(5):549-68. [DOI] [PubMed] [Google Scholar]
- 3. McAlister FA, Wilkins K, Joffres M, et al. Changes in the rates of awareness, treatment and control of hypertension in Canada over the past two decades. CMAJ 2011;183(9):1007-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chisholm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Med Care 2010;48:923-33. [DOI] [PubMed] [Google Scholar]
- 5. Santschi V, Chiolero A, Burnand B, et al. Impact of pharmacist care in the management of cardiovascular disease risk factors: s systematic review and meta-analysis of randomized trials. Arch Intern Med 2011;171:1441-53. [DOI] [PubMed] [Google Scholar]
- 6. Santschi V, Chiolero A, Paradis G, et al. Pharmacist interventions to improve cardiovascular disease risk factors in diabetes: a systematic review and metaanalysis of randomized controlled trials. Diabetes Care 2012;35:2706-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Santschi V, Chiolero A, Colosimo AL, et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc 2014;3:e000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tsuyuki R, Houle S, Charrois T, et al. A randomized trial of the effect of pharmacist prescribing on improving blood pressure in the community: the Alberta clinical trial in optimizing hypertension (RxACTION). Can Pharm J (Ott) 2014;147:S18. [DOI] [PubMed] [Google Scholar]
- 9. Pojskic N, Jackson M, Malek A, Cimino S. Impact of community pharmacist interventions in hypertension management on patient outcomes: a randomized controlled trial. Can Pharm J (Ott) 2014;147:S17. [Google Scholar]
- 10. Houle SKD, Tsuyuki RT, Campbell NRC. The Canadian Hypertension Education Program (CHEP) 2011 Guidelines for Pharmacists. Can Pharm J (Ott) 2011;144:295-304. [Google Scholar]
- 11. Houle SKD, Padwal R, Tsuyuki RT. The 2012-2013 Canadian Hypertension Education Program (CHEP) guidelines for pharmacists: an update. Can Pharm J (Ott) 2013;146:146-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Houle SKD, Padwal R, Poirier L, Tsuyuki RT. The 2014 Canadian Hypertension Education Program (CHEP) guidelines for pharmacists: an update. Can Pharm J (Ott) 2014;147:203-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Myers MG, Kaczorowski J, Dawes M, Godwin M. Automated office blood pressure measurement in primary care. Can Fam Phys 2014;60:127-32. [PMC free article] [PubMed] [Google Scholar]
- 14. Beckett L, Godwin M. The BpTRU automatic blood pressure monitor compared to 24 hour ambulatory blood pressure monitoring in the assessment of blood pressure in patients with hypertension. BMC Cardiovasc Disord 2005;5:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Andreadis EA, Agaliotis GD, Angelopoulos ET, et al. Automated office blood pressure and 24-h ambulatory measurements are equally associated with left ventricular mass index. Am J Hypertens 2011;24:661-6. [DOI] [PubMed] [Google Scholar]
- 16. Mule G, Caimi G, Cottone S, et al. Value of home blood pressures as predictor of target organ damage in mild arterial hypertension. J Cardiovasc Risk 2002;9:123-9. [DOI] [PubMed] [Google Scholar]
- 17. Ohkubo T, Kikuya M, Metoki H, et al. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring: 10-year follow-up from the Ohasama Study. J Am Coll Cardiol 2005;46:508-15. [DOI] [PubMed] [Google Scholar]
- 18. Franklin SS, Thijs L, Hansen TW, et al. White-coat hypertension: new insights from recent studies. Hypertension 2013;62:982-7. [DOI] [PubMed] [Google Scholar]
- 19. Hanninen MR, Niiranen TJ, Puukka PJ, et al. Determinants of masked hypertension in the general population: the Finn-Home study. J Hypertens 2011;29:1880-8. [DOI] [PubMed] [Google Scholar]
- 20. Andalib A, Akhtari S, Rigal R, et al. Determinants of masked hypertension in hypertensive patients treated in a primary care setting. Intern Med J 2012;42:260-6. [DOI] [PubMed] [Google Scholar]
- 21. Barochiner J, Cuffaro PE, Aparicio LS, et al. Predictors of masked hypertension among treated hypertensive patients: an interesting association with orthostatic hypertension. Am J Hypertens 2013;26:872-8. [DOI] [PubMed] [Google Scholar]
- 22. McAlister FA, Robitaille C, Gillespie C, et al. The impact of cardiovascular risk-factor profiles on blood pressure control rates in adults from Canada and the United States. Can J Cardiol 2013;29:598-605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stead LF, Buitrago D, Preciado N, et al. Physician advice for smoking cessation. Cochrane Database System Rev 2013,(5):CD000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database System Rev 2013;(5):CD009329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jee SH, Suh I, Kim IS, Appel LJ. Smoking and atherosclerotic cardiovascular disease in men with low levels of serum cholesterol: the Korea Medical Insurance Corporation Study. JAMA 1999;282:2149-55. [DOI] [PubMed] [Google Scholar]
- 26. Njolstad I, Arnesen E, Lund-Larsen PG. Smoking, serum lipids, blood pressure and sex differences in myocardial infarction: a 12-year follow-up of the Finnmark Study. Circulation 1996;93:450-6. [DOI] [PubMed] [Google Scholar]
- 27. Prescott E, Hippe M, Schnohr P, et al. Smoking and risk of myocardial infarction in women and men: longitudinal population study. BMJ 1998;316:1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937-52. [DOI] [PubMed] [Google Scholar]
- 29. Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet 2011;378:1297-305. [DOI] [PubMed] [Google Scholar]
- 30. Qiao Q, Tervahauta M, Nissinen A, Tuomilehto J. Mortality from all causes and from coronary heart disease related to smoking and changes in smoking during a 35-year follow-up of middle-aged Finnish men. Eur Heart J 2000; 21:1621-6. [DOI] [PubMed] [Google Scholar]
- 31. Saba M, Diep J, Saini B, Dhippayom T. Meta-analysis of the effectiveness of smoking cessation interventions in community pharmacy. J Clin Pharm Ther 2014;39:240-7. [DOI] [PubMed] [Google Scholar]