Abstract
Between 2.2% and 17% of all strokes have symptom onset during hospitalization in a patient originally admitted for another diagnosis or procedure. These in-hospital strokes represent a unique population with different risk factors, more mimics, and substantially worsened outcomes compared to community-onset strokes. The fact that these strokes manifest during the acute care hospitalization, in patients with higher rates of thrombolytic contraindications, creates distinct challenges for treatment. However, the best evidence suggests benefit to treating appropriately selected in-hospital ischemic strokes with thrombolysis. Evidence points toward a “quality gap” for in-hospital stroke with longer in-hospital delays to evaluation and treatment, lower rates of evaluation for etiology, and decreased adherence to consensus quality process measures of care. This quality gap for in-hospital stroke represents a focused opportunity for quality improvement.
Keywords: stroke, quality, neurohospitalist, stroke and cerebrovascular disease, safety
Introduction
In-hospital stroke is defined as acute infarction of central nervous system tissue that occurs during hospitalization in a patient originally admitted for another diagnosis or procedure. Between 2% and 17% of all patients with stroke in published series had onset of symptoms during hospitalization.1–10 In-hospital strokes complicate between 0.04% and 0.06% of all admissions.10,11 The proportion of reported in-hospital events tends to be lower in large stroke registries than in single hospital studies. In-hospital transient ischemic attacks (TIAs) and subtle infarctions may be unrecognized, or underreported, in complicated ill inpatients.
The societal burden of in-hospital stroke is substantial. The 30-day cost of care for an in-hospital stroke of average severity can be estimated at US$17 500.5,12 With an estimate of 35 000 to 75 000 in-hospital strokes in the United States each year, the lifetime direct and indirect costs for these in-hospital strokes would be approximately 4.9 billion to 10.5 billion dollars.12,13 Given that the comorbidity of in-hospital strokes is higher than in community strokes, these are likely conservative estimates.
Mechanisms
In-hospital stroke can be considered either a complication of the illness and comorbidity, which led to hospitalization, or an iatrogenic consequence of therapeutic interventions and withdrawal of protective therapy during hospitalization. Mechanism can be direct complication of vessel manipulation, brain ischemia from systemic hypoperfusion, or a thromboembolic event due to stasis and hypercoagulability induced by comorbid illness or surgery.7 Underlying risk may be magnified by withdrawal of antithrombotic or anticoagulant therapy due to bleeding, inability to take oral medications, or invasive procedures. Hospitalized patients may experience any combination of these factors, and this may help explain the higher risk of strokes for patients hospitalized compared to those in the community.11
Iatrogenic complications of procedures can cause accidental ligation of arteries during surgery, arterial dissection, or disruption of plaque and subsequent clot as a result of intrinsic or extrinsic vessel manipulation. In-hospital strokes may occur after embolization of thrombus from endocarditis, after cardioversion for arrhythmia, or as a consequence of stasis from atrial fibrillation, cardiomyopathy, or myocardial infarction with wall motion hypokinesis. One percent of all admissions for myocardial infarction will be complicated by in-hospital stroke.14
Perioperative and periprocedural stroke deserves special mention as between half and two-thirds of in-hospital strokes follow catheterization or surgery.5,7,15 Cardiac surgery patients appear to represent a particularly high-risk population, likely due to the combination of arrhythmias, hypotension, and the arterial manipulation required for evaluation and treatment. There may also be shared risk factors for unstable plaque in both coronary and cerebral vasculature beds.16 One potent risk of periprocedural stroke relates to withdrawal of antithrombotic therapy, which was noted in more than a quarter of all patients with in-hospital stroke.15
Six independent risk factors have been identified for nonprocedural in-hospital stroke.9 These include fever, leukocytosis, elevated diastolic blood pressure, unstable blood pressure, dehydration, and a past history of myocardial infarction. Some of these may reflect transient hypercoagulability, which attends illness leading to hospitalization. High rates of cancer have been reported in patients with in-hospital stroke presumably due to the hypercoagulable state that can accompany malignancy.6,15 Inflammatory states can promote plaque vulnerability and increase the risk of in situ thrombosis. Hospitalization is well recognized to be a period of increased risk of venous thromboembolism. In some cases, clots from the venous system can cross an intracardiac shunt and lead to in-hospital stroke. One study found that a higher percentage of in-hospital strokes had a right to left shunt compared to community-onset strokes, and paradoxical embolism was identified more commonly for in-hospital strokes.6
Characterizing In-Hospital Strokes
In the largest study of in-hospital strokes, the median age of patients was 73 years, and 53% occurred in women.3 In all, 49% were on antiplatelet therapy, and 17% were on anticoagulation before admission.3 The median National Institute for Health Stroke Severity (NIHSS) score was 9, which was more than twice the median severity for strokes from the community (9 vs 4; P < .0001).3 The most common services caring for patients who suffer in-hospital strokes are cardiology or cardiovascular surgery.10 Relatively few patients with in-hospital stroke have symptom onset on the neurology units where stroke expertise is highest.15 In 1 study for patients who experienced an in-hospital stroke, the admitting diagnosis was cardiovascular (24%), neurology/neurosurgery (15%), hematology/oncology (8%), orthopedic/trauma (7%), gastrointestinal (7%), and respiratory (5%).5 Half of periprocedural events occur in the first 24 hours of surgery or invasive procedure.10 Two-thirds of in-hospital strokes are witnessed at symptom onset, most commonly by a nurse.15,17
Across a variety of studies, cardiac risk factors are more frequently observed in patients with in-hospital stroke including atrial fibrillation, coronary artery disease, and congestive heart failure/cardiomyopathy.2,3,6,8,10 Conversely, atherosclerotic risk factors such as hypertension and tobacco use appear to be more common in community-onset strokes.3,6,8,10
Transient ischemic attacks appear to be less commonly reported as manifestation of in-hospital ischemia.5 In-hospital strokes have a greater severity in general, but the lower observed rates of TIA may also be influenced by impaired ability to recognize transient ischemic symptoms in complex ill inpatients with plausible alternative explanations for symptoms. Cardioembolic events are more commonly identified for in-hospital strokes and represent the etiology for approximately half of all in-hospital strokes (P < .001 for difference in stroke mechanism).10,15 Conversely, large artery mechanism strokes are half as common in the in-hospital setting (12% vs 24%), and small vessel lacunar occlusions are relatively rare (<5%).10,15
Prognosis
It makes intuitive sense that a patient who has suffered a stroke after requiring admission for another illness or surgery would face a higher hurdle to recovery than a patient who experienced a spontaneous stroke without other acute medical problems. In effect the patient has suffered 2 “hits” to health and function; the original cause of the hospitalization followed by the complication of in-hospital stroke. The confluence of higher stroke severity and greater burden of comorbid illness likely explains why the majority of the evidence points to worse prognosis for in-hospital strokes. Observational studies demonstrate that patients with in-hospital stroke have a longer length of stay (P < .0001), greater disability on the modified Rankin score (mRS; P < .001), and are half as likely to return directly home from the hospital (P < .0001).3,5 In all, 45% to 61% of patients with in-hospital stroke have moderate to severe disability on discharge compared to 25% to 36% of patients with community-onset stroke (P < .0001).5,8 In multivariate models, patients with in-hospital stroke were less likely to be able to ambulate independently at discharge (adjusted odds ratio [OR] 0.42, 95% confidence interval, CI [0.39-0.45]; P < .001) and less likely to be discharged home (OR 0.37, 95% CI [0.35-0.39]; P < .001).3 Long term studies of functional outcome for in-hospital stroke patients are lacking. Discharge functional outcomes cannot distinguish between potentially reversible functional limitations from the initial illness and chronic disability as a consequence of the in-hospital stroke deficits. In-hospital stroke portends a grave prognosis with a mortality rate 2 to 3× greater than community-onset strokes and absolute in-hospital mortality rates of 14% to 19% (P < .001).3,5,8,10,15
Acute Treatment
The fundamentals of acute treatment for in-hospital stroke are the same as for stroke with onset in the community. Treatment hinges on rapid evaluation to rule out stroke mimics, assess contraindications, and timely administration of thrombolysis and other acute therapeutic interventions. Intravenous (IV) thrombolytic treatment rates for in-hospital stroke range from 2.6% to 11%.2–5,10 Two significant differences appear in the literature relating to treatment delivery for this population. The first is that medical or surgical contraindications to IV thrombolysis are common for patients with in-hospital stroke. The second is that time to evaluation and treatment for in-hospital strokes have significant delays, exceeding quality benchmarks, and are prolonged compared to community-onset strokes.
Higher rates of medical contraindications to IV thrombolysis (68% vs 37%; P < .0001) were found in analysis of a Colorado statewide stroke database.2 Many patients with in-hospital stroke are on anticoagulation, have prior bleeding, or have undergone a recent invasive procedure. Physicians, and those responsible for in-hospital stroke response system design, should be aware of this higher likelihood of contraindication to IV thrombolysis.
Patients with in-hospital stroke appropriate for IV thrombolytic treatment appear to get equal benefit compared to patients with community-onset stroke. A retrospective review of patients with in-hospital stroke receiving IV thrombolysis demonstrated equivalent rates of neurologic improvement compared to treated community-onset strokes.18 No statistical difference was seen between in-hospital and community-onset strokes with NIHSS decrease ≥8 points at 7 days (63% vs 52%; P = nonsignificant) and mRS ≤2 at 90 days (56% vs 55%; P = nonsignificant).18 Safety also appears similar. In a national registry, patients with in-hospital stroke who are treated with IV thrombolysis experience similar rates of intracranial hemorrhage (ICH; 4.5% vs 5.3%; P = .0988) and serious bleeding (1.6% vs 1.2%; P = .0871) but did have slightly higher rates of “other serious complications” (3.2% vs 2.5%; P = .0288) compared to community-onset strokes after IV thrombolysis.3
Although by definition the prehospital time that represents the majority of the interval between stroke onset and treatment for strokes in the community is absent, delays in hospital-based evaluation have been described for in-hospital strokes.18 A 2008 study out of Spain found in only 25% of in-hospital stroke cases was neurology consultation considered an emergency.19 A third of patients in a 2010 study were not evaluated by a neurologist within the thrombolytic window and delays in calling the neurologist precluded IV thrombolytic therapy in half of eligible patients.15 In the statewide Michigan Stroke Registry, only 3.1% of patients with in-hospital stroke received brain imaging within the benchmark 25 minutes from symptom recognition.5 In the American Heart Association/American Stroke Association national Get-With-The-Guidelines database, time to treatment for in-hospital strokes averaged 100 minutes, and only 1 in 5 patients with in-hospital stroke achieved the goal of 60 minutes from recognition of symptoms by hospital staff to treatment.3
For patients with contraindication to IV thrombolysis, endovascular therapy may be an option and growing evidence supports intra-arterial (IA) and mechanical thrombolysis. An analysis from 6 certified stroke centers enrolled in a National Stroke Association (NSA) Initiative for in-hospital stroke revealed 8.2% of patients with in-hospital stroke received IV thrombolysis alone, 10.3% received IA/mechanical thrombolysis alone, and 1% received both.20 Successful use of IA thrombolysis has been described after cardiac catheterization, immediately postpartum, postcesarian section, and in the early perioperative period including after cardiac surgery.21–25
In a series of 13 cardiac surgery patients treated with IA tissue plasminogen activator (tPA), 38% of treated patients had neurologic improvement although 2 patients required transfusion (1 with hemothorax and 1 with a small ICH).25 The largest series described 36 patients from a mixed postoperative population who had ischemic stroke were treated with IA thrombolysis.21 Of treated patients, 25% had surgical site bleeding, 25% had intracranial bleeding (6 of 9 asymptomatic), and 8% had fatal major bleeding.21 Two-thirds of the fatalities related to bleeding were in postcraniotomy patients and 2 of 3 craniotomy patients treated with IA tPA had fatal ICH. Good clinical outcome (mRS <2) was seen in 38% of patients.21 The authors concluded that IA thrombolysis in the postoperative setting has a reasonable safety profile, although surgical site bleeding should be expected in a quarter of patients, and neurosurgical patients represent a particularly high-risk group for adverse safety events.
Although there are a higher percentage of patients with contraindication to IV thrombolysis, the evidence supports equivalent benefit for those treated appropriately and no higher rates of hemorrhagic complications. For those with contraindication to IV thrombolysis, endovascular intervention may be considered, although neurosurgery patients may not be good candidates for IA thrombolysis. Evidence supports use of advanced endovascular interventions for patients with acute ischemic stroke. The Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands (Mr CLEAN) and Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times (ESCAPE) trials published in 2015 supported the use of such treatment for patients with proximal intracranial occlusion of the anterior circulation in improving function outcomes.26,27 The majority of the patients in these trials received IV thrombolysis before endovascular intervention. More research is needed on the benefits and safety of IA thrombolysis and/or mechanical endovascular intervention for in-hospital strokes who are not candidates for IV thrombolysis.
Quality of Care
Beyond speed of evaluation and thrombolytic treatment rates, the quality of care for in-hospital strokes demonstrates gaps both in comprehensive stroke evaluation and in adherence to consensus process measures of care (Table 1). Studies have demonstrated lower rates of imaging of cerebral vasculature for in-hospital strokes.5,10 There is also lower frequency of evaluation for underlying etiology and modifiable risk factors for in-hospital stroke and less implementation of secondary prevention measures. Although some measures, such as rehabilitation assessment, are higher for in-hospital stroke, others such as lipid assessment appear to be lower.2,3,5 The national Get With The Guidelines stroke database reported lower overall adherence to consensus process measures of quality care for in-hospital strokes for whom defect-free care was only 61% compared to 82% for community-onset strokes (P < .0001).3
Table 1.
Representative Gaps in Quality Care Between In-hospital Strokes and Community-Onset Strokes.
| Quality Measure | In-Hospital Stroke | Community- Onset Stroke | P Value | Population | Comparison to Other Studiesa |
|---|---|---|---|---|---|
| Speed of treatment | |||||
| Time to brain imaging28 | 98 minutes | 29 minutes | <.0001 | Single center | Colorado State registry found nonsignificant trend toward longer time to brain imaging for in-hospital stroke (54 vs 43 minutes; P = .13).2 Michigan State registry found no difference in brain imaging within 25 minutes but for both groups the percentage evaluated within this time frame was low with high rates of missing data (3.1% vs 3.5%; P = .27).5 |
| IV tPA given for within the time goals3 | 31.6% | 73.4% | <.0001 | US National Stroke Registry | Michigan State registry and Colorado State registry studies did not attempt to compare treatment rates within time goals.2,5 |
| Evaluation for risk factors and etiology | |||||
| Cerebral vasculature investigated5 | 55.2% | 75.6% | <.01 | State of Michigan Stroke Registry | Results supported by a different single-center study, which found 13% incomplete evaluation of etiology for in-hospital strokes compared to 3% Community-onset strokes (P value not reported).10 |
| Lipids investigated3 | 71.5% | 86.3% | <.0001 | US National Stroke Registry | The Michigan State registry also demonstrated a significantly lower rate of lipid investigation for in-hospital strokes (23.6% vs 38.0%; P = .01).5 Overall performance on this metric was lower in the Michigan registry compared to the national registry, which may reflect a temporal trend toward improving quality adherence. However, the Colorado State registry found the same rate of use of lipid-lowering therapy between in-hospital and community-onset strokes (89.6% adherence in both groups; P = .87).2 |
| Complication prevention | |||||
| DVT prophylaxis3 | 88.8% | 92.2% | <.0001 | US National Stroke Registry | The Michigan State registry demonstrated a similar magnitude, nonsignificant, trend toward lower DVT prophylaxis for in-hospital strokes (55.2% vs 64.2%; P = .28).5 |
| Secondary prevention | |||||
| Early antithrombotics3 | 89.4% | 96.4% | <.0001 | US National Stroke Registry | The Colorado State registry did not demonstrate a difference in antithrombotic therapy by day 2 between in-hospital and community-onset strokes (100% vs 96.2%; P = 1.00).2 |
| Antithrombotics on discharge3 | 96.1% | 97.7% | <.0001 | US National Stroke Registry | While statistically significant due to a large sample size, the absolute difference is small and both the Colorado (97.7% vs 96.2%; P = .77) and Michigan State registries (88.0% vs 94.6%; P = .26) did not find a significant difference for antithrombotics on discharge.2,5 |
| Anticoagulants on discharge for afib/flutter3 | 90.6% | 93.8% | <.0001 | US National Stroke Registry | Michigan State registry found a similar magnitude of absolute difference for this metric but it was not significant (84.0% vs 86.6%; P = .82).5 The Colorado State registry found a higher rate of adherence also not meeting criteria for significance (100% vs 93.4%; P = 1.00).2 |
| Overall quality of care | |||||
| Defect-free care3 | 60.8% | 82.0% | <.0001 | US National Stroke Registry | This contrasts to the findings of the Colorado State registry which found higher rates of defect-free care for in-hospital strokes (52.8% vs 32.2%; P < .0001) driven by higher in-hospital stroke adherence rates of stroke education and assessment for rehabilitation.2 Metrics and methodology used to calculate defect-free care between the Colorado State registry and GWTG national registry differed. IV tPA metrics were not included in the calculation of defect-free care in the Colorado State registry. |
Abbreviations: afib, atrial fibrillation; DVT, deep vein thrombosis; GWTG, Get With The Guidelines; IV, intravenous; tPA, tissue plasminogen activator.
aDirect comparisons of performance on quality metrics between studies is problematic due to differences in power based on sample size, variation in definitions for quality metrics, and temporal trends toward improved adherence on individual quality metrics over time. Michigan Stroke Registry study included strokes from May 2002 to November 2002. The single-center trial included strokes from October 2005 to September 2007. Colorado Stroke Registry study included strokes from August 2005 and April 2009. National Stroke Registry study included strokes from January 2006 to April 2012.
Greater hospital delays to thrombolytic treatment for ischemic events with onset in the hospital compared to in the community have been observed for both stroke and ST elevation myocardial infarction.3,29 This raises the interesting question, why would it take longer to respond to time critical ischemic emergencies in patients already hospitalized? There are a number of factors that could explain quality gaps for stroke (Table 2). Recognition of stroke onset represents the first challenge. Symptoms can be misinterpreted as a result of the systemic illness that caused the original hospitalization, side effects of medications, or attributed to a mimic of stroke. In some cases such as stroke during general anesthesia or in a sedated patient, early recognition can be extremely difficult or impossible. The majority of patients with in-hospital stroke are not initially cared for on a neurology/stroke unit or have a neurologist as the primary admitting attending. Providers caring for patients who experience in-hospital stroke may be less experienced in stroke diagnosis, unfamiliar with time thresholds for evaluation and treatment, or unaware of the consensus measures of care quality. The competing priorities created by the demands of the original reason for admission and complicating comorbid illnesses may distract from focus on stroke-specific quality indicators.
Table 2.
Factors Contributing to Quality Gaps.a
| Potential Contributor | Barriers | Potential Solutions |
|---|---|---|
| Increased difficulty in initially recognizing possible stroke symptoms |
|
|
| Delay between symptom onset and symptom recognition by hospital staff |
|
|
| Delay in initial evaluation of stroke |
|
|
| Poor adherence to consensus measures of stroke process care quality during hospitalization |
|
|
| Transitions of care quality metrics inconsistently |
|
|
aTable reflects author opinion. Magnitude of contribution of each barrier has not been systematically examined in isolation to determine the relative contribution to the quality gap. Solutions have not been tested in isolation to determine the effect on quality metrics or outcomes.
Systems-level factors may also contribute. Community-onset strokes have a point of entry into the system through the emergency department (ED), which may facilitate rapid evaluation through physical proximity to scanning facilities and a culture of urgency. Use of quality care bundles embedded into stroke admission order sets facilitates adherence to individual measures, and these bundles may not be as accessible for the patient with stroke after the point of admission. Recognizing these factors offers a number of potential points of intervention for quality improvement (QI)—educating hospital staff about signs and symptoms of stroke, creating acute inpatient stroke response systems, and developing stroke protocols that can be overlaid onto existing care for patients with stroke after the point of admission.
Quality Improvement
Creating an In-Hospital Stroke Response Team
An effective means of concentrating expertise and achieving expedited evaluation of patients with suspected in-hospital stroke is a response team for inpatient stroke alerts. Some hospitals use generalist rapid response teams who also respond to inpatient cardiopulmonary crisis with additional stroke training. Others use a dedicated stroke response team also responding to strokes in the ED. The common theme is rapidly bringing expertise in the initial evaluation for thrombolysis to the bedside of a patient anywhere within the hospital. Effectiveness of an in-hospital stroke response system is critically dependent on hospital staff being adequately educated on stroke signs and symptoms in order for the in-hospital stroke alert to be activated. Any staff member should be capable of directly triggering the alert, and a single alert number provides a simple mechanism to activate the response team. The inpatient stroke response team requires the authority to proceed with evaluation to avoid delays inherent in obtaining approval from additional parties who may not be present at the bedside.
Acute inpatient stroke teams have been demonstrated to reduce in-hospital delays.28,30–32 When a general medicine rapid response team is used for in-hospital stroke alerts, additional stroke-specific training for rapid response team members is necessary. If a dedicated neurology response team is utilized, expertise on the team in urgent response to the common cardiopulmonary and metabolic mimics of stroke symptoms is similarly prudent.
False alarms are the natural consequence of needing to rapidly respond to potential strokes given the considerable overlap between stroke symptoms and that of the many stroke mimics. In-hospital stroke alerts, possibly as a result of the complexity of illness in hospital inpatients, have a higher rate of alarms for nonstroke diagnoses. In an analysis of 6 stroke centers, approximately half of all alerts were for stroke mimics with wide variation in the false alarm rates between hospitals ranging from 28% to 67%.20 The 5 most commonly identified etiologies of inpatient stroke alerts for nonstroke diagnoses include seizure, systemic hypoperfusion, delirium, medication effect, and metabolic disturbance.20
Optimizing Response Speed
For hospitals with a gap in response time between ED and inpatient settings, explicit QI initiatives have been demonstrated to reduce in-hospital delays in evaluation. A hospital with a response time for stroke alerts on the ward more than twice that of the ED was able to reduce median response time from 69 to 29.5 minutes through application of LEAN QI principles (P < .0001).33 Efforts to reduce time to evaluation and treatment are multipronged and will include a multidisciplinary team of motivated stakeholders. An in-hospital stroke QI initiative will typically start by developing a process map of response for suspected in-hospital strokes. Interviews with individuals who touch the response process such as frontline nursing, stroke response team members, neurologists, radiology, and pharmacy staff elucidates the current state and supplement direct observation of process-in-action during stroke alerts. The NSA’s in-hospital stroke QI initiative developed a number of tools for institutions working to optimize response time available through the NSA In-Hospital Stroke Resource Center.34 It is useful to track multiple intervals within the overall process from symptom recognition to thrombolysis administration and the NSA developed a sample tool for this purpose for use by stroke programs.34 Examples might include time from symptom recognition to arrival of stroke response team, to computed tomography scan, to laboratory results, and to thrombolytic treatment. One would then focus on unreliable steps or reliably slow steps to target for improvement. The LEAN principles are applied to reengineer workflow for efficiency. Actions that were performed in a serial fashion but are not interdependent can be reorganized to occur in parallel and improve speed of evaluation and response. Inconsistent adherence to steps within the process can be addressed by clearly delineating roles and responsibilities and standardizing response steps. An example might be creating pocket cards carried by the stroke response team and provided to the patient’s nurse on arrival that outline exactly which steps need to occur, in what order, and by whom (Figure 1). Communication steps should be made explicit—who is contacted, when, and how. In the redesign of the process, several cycles of “mock stroke codes” provides the opportunity to incorporate iterative improvements in the process before the changes are implemented on a system level. The NSA developed instructions on how to use such a simulated stroke alert for training and design purposes.34 Education through in-service or Grand Rounds events provides the role of educating staff on signs and symptoms of stroke and the new improved response system. Real-time feedback after each in-hospital stroke alert with analysis of system performance to and from participants provides the chance to reinforce education but also creates a forum for input back to the stroke program from frontline providers to facilitate further refinement and improvements. A template for this feedback is available through the NSA In-Hospital Stroke Resource Center.34 A regular stream of data on median response times, typically on a monthly basis, is critical to support the stroke program’s ability to assess impact of rapid change events. Simple run charts or more complex control charts are methods to visually display improvement, need for further action, or stability of performance.
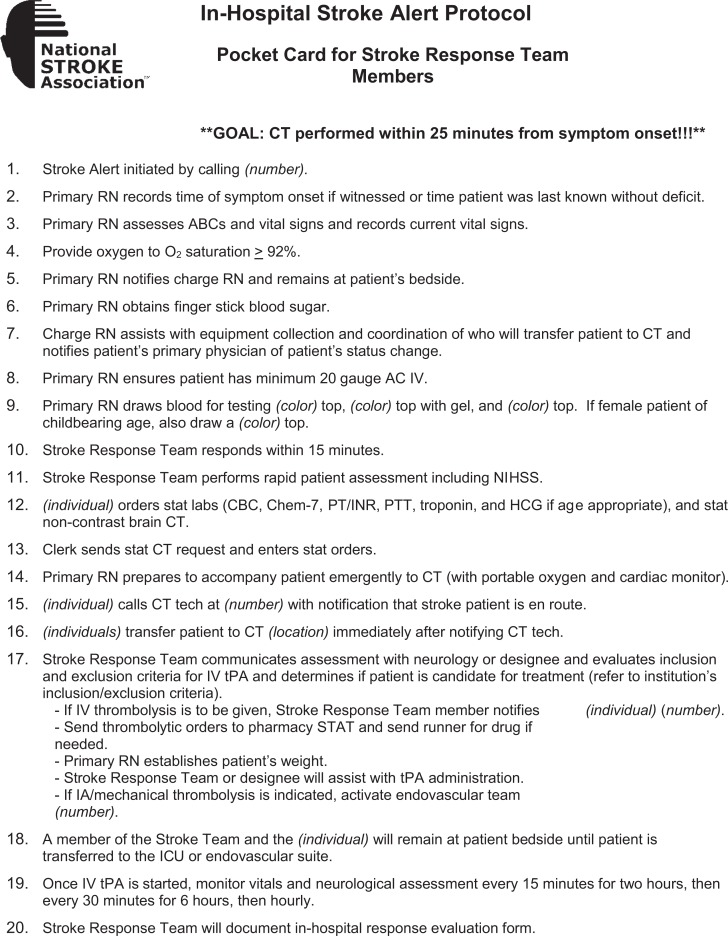
Figure 1.
In-hospital stroke alert protocol card.
Note. Designed to be individualized to meet the needs and resources of the individual hospital. Depending on delays identified, the order of the protocol may be modified.
Directions for Future Research
Research is needed on means to reduce the incidence of in-hospital stroke, particularly in high-risk patients undergoing surgery. Ongoing trials on antithrombotic bridging management during hospitalization will inform practitioners on risk-benefit of this mechanism to reduce perioperative strokes. Although early recognition of symptoms is important to minimize ischemic time, the appropriate frequency of monitoring for new neurologic deficits in high-risk patients has not been established. Given high rates of delirium, metabolic disturbances, and medication effects in the hospital, optimized criteria for in-hospital stroke alerts that would maximize identification of ischemic strokes while minimizing inappropriate activation of the stroke team would be an area of important future research.
Conclusions
Evidence demonstrates that risk factors, mimics, and etiology of ischemia for in-hospital stroke are different than for those in the community. More concerning is the evidence that factors such as response times, adherence to quality processes of care, and treatment rates demonstrates a quality gap for in-hospital strokes. Outcomes for in-hospital stroke are uniformly observed to be worse than strokes in the community. To some extent this is an expected phenomenon given the 2-hit nature of a stroke after hospitalization for another acute illness. However, there is potential for explicit QI efforts to help narrow the divide.
Acknowledgments
The authors acknowledge The National Stroke Association and the American Heart Association/American Stroke Association for supporting in-hospital stroke quality improvement research.
Footnotes
Declaration of Conflicting Interests: The author declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Cumbler is the Course Director for the National Stroke Association’s In-hospital Stroke Quality Improvement initiative. He has collaborated with the American Heart Association/American Stroke Association on in-hospital stroke research using the Get-With-The-Guidelines-Stroke database. Dr Cumbler has spoken for COPIC insurance on the topic of in-hospital stroke.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Aly N, McDonald K, Leathley M, Sharma A, Watkins C. Retrospective case note review of acute and inpatient stroke outcomes. BMJ. 2000;320(7248):1511–1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cumbler EC, Murphy P, Jones WJ, Wald HL, Kutner JS, Smith DB. Quality of care for in-hospital stroke: analysis of a state-wide registry. Stroke. 2011;42(1):207–210. [DOI] [PubMed] [Google Scholar]
- 3. Cumbler E, Wald H, Bhatt DL, et al. Quality of care and outcomes for in-hospital ischemic stroke: findings from the national Get With The Guidelines-stroke. Stroke. 2014;45(1):231–238. [DOI] [PubMed] [Google Scholar]
- 4. Dulli D, Samaniego EA. Inpatient and community ischemic strokes in a community hospital. Neuroepidemiology. 2007;28(2):86–92. [DOI] [PubMed] [Google Scholar]
- 5. Farooq MU, Reeves MJ, Gargano J, Wehner S, Hickenbottom S, Majid A; for the Paul Coverdale National Acute Stroke Registry Michigan Prototype Investigators. In-hospital stroke in a statewide stroke registry. Cerebrovasc Dis. 2008;25(1-2):12–20. [DOI] [PubMed] [Google Scholar]
- 6. Iguchi Y, Kimura K, Kobayashi K, et al. In-hospital onset ischemic stroke may be associated with atrial fibrillation and right-to-left shunt. J Neurol Sci. 2007;254(1-2):39–43. [DOI] [PubMed] [Google Scholar]
- 7. Kelley RE, Kovacs AG. Mechanism of in-hospital cerebral ischemia. Stroke. 1986;17(3):430–433. [DOI] [PubMed] [Google Scholar]
- 8. Kimura K, Minematsu K, Yamaguchi T. Characteristics of in-hospital onset ischemic stroke. Eur Neurol. 2006;55(3):155–159. [DOI] [PubMed] [Google Scholar]
- 9. Nadav L, Gur AY, Korczyn AD, Bornstein MN. Stroke in hospitalized patients: are there special risk factors? Cerebrovasc Dis. 2002;13(2):127–131. [DOI] [PubMed] [Google Scholar]
- 10. Park JH, Cho HJ, Kim DW, et al. Comparison of the characteristics for in-hospital and out-of-hospital ischaemic strokes. Eur J Neur. 2009;16(5):582–588. [DOI] [PubMed] [Google Scholar]
- 11. Azzimondi G, Nonino F, Fiorani L, et al. Incidence of stroke among inpatients in a large Italian hospital. Stroke. 1994;25(9):1753–1754. [DOI] [PubMed] [Google Scholar]
- 12. Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115(5):e69–e171. [DOI] [PubMed] [Google Scholar]
- 13. Blacker DJ. In-hospital stroke. Lancet Neurol. 2003;2(12):741–746. [DOI] [PubMed] [Google Scholar]
- 14. Witt BJ, Ballman KV, Brown RD, Jr, Meverden RA, Jacobsen SJ, Roger VL. Incidence of stroke after myocardial infarction: a meta-analysis. Am J Med. 2006;119(4):354. e1–e9. [DOI] [PubMed] [Google Scholar]
- 15. Vera R, Lago A, Fuentes B, et al. In-hospital stroke: a multi-centre prospective registry. Eur J Neurol. 2011;18(1):170–176. [DOI] [PubMed] [Google Scholar]
- 16. Selim M. Perioperative stroke. N Engl J Med. 2007;356(7):706–713. [DOI] [PubMed] [Google Scholar]
- 17. Albers MJ, Brass LM, Perry A, Webb D, Dawson DV. Evaluation times for patients with in-hospital strokes. Stroke. 1993;24(12):1817–1822. [DOI] [PubMed] [Google Scholar]
- 18. Masjuan J, Simal P, Fuentes B, et al. In-hospital stroke treated with intravenous tissue plasminogen activator. Stroke. 2008;39(9):2614–2616. [DOI] [PubMed] [Google Scholar]
- 19. Alvaro LC, Timiraos J, Sadaba F. In-hospital stroke: clinical profile and expectations for treatment. Neurologia. 2008;23(1):4–9. [PubMed] [Google Scholar]
- 20. Cumbler E, Simpson J. Code stroke: multi-center experience with in-hospital stroke alerts. J Hosp Med. 2015;10(3):179–183. [DOI] [PubMed] [Google Scholar]
- 21. Chalela JA, Katzan I, Siebeskind DS, et al. Safety of intra-arterial thrombolysis in the postoperative period. Stroke. 2001;32(6):1365–1369. [DOI] [PubMed] [Google Scholar]
- 22. Fukuda I, Imazura T, Osaka M, Watanabe K, Megura K, Wada M. Thrombolytic therapy for delayed in-hospital stroke after cardiac surgery. Ann Thorac Surg. 2003;76(4):1293–1295. [DOI] [PubMed] [Google Scholar]
- 23. Khatri P, Taylor RA, Palumbo V, et al. The safety and efficacy of thrombolysis for strokes after cardiac catheterization. J Am Coll Cardiol. 2008;51(9):906–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mendez JC, Masjuan J, Garcia N, de Lecinana M. Successful intra-arterial thrombolysis for acute ischemic stroke in the immediate postpartum period: case report. Cardiovasc Intervent Radiol. 2008;31(1):193–195. [DOI] [PubMed] [Google Scholar]
- 25. Moazami N, Smedira NG, McCarthy PM, et al. Safety and efficacy of intraarterial thrombolysis for perioperative stroke after cardiac operation. Ann Thorac Surg. 2001;72(6):1933–1939. [DOI] [PubMed] [Google Scholar]
- 26. Berkhemer OA, Fransen PSS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11–20. [DOI] [PubMed] [Google Scholar]
- 27. Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–1030. [DOI] [PubMed] [Google Scholar]
- 28. Cumbler E, Anderson T, Neumann R, Jones WJ, Brega K. Stroke alert program improves recognition and evaluation time of in-hospital ischemic stroke. J Stroke Cerebrovasc Dis. 2009;19(6):494–496. [DOI] [PubMed] [Google Scholar]
- 29. Garberich RF, Traverse JH, Claussen MT, et al. ST-elevation myocardial infarction diagnosed after hospital admission. Circulation. 2014;129(11):1225–1232. [DOI] [PubMed] [Google Scholar]
- 30. Daly ML, Orto V, Wood C. ID, stat: rapid response to in-hospital stroke patients. Nurs Manage. 2009;40(11):34–38. [DOI] [PubMed] [Google Scholar]
- 31. McDaniel J. Code grey case studies. Crit Care Nurs Q. 2003;26(4):303–315. [DOI] [PubMed] [Google Scholar]
- 32. Nolan S, Naylor G, Burns M. Code gray—an organized approach to inpatient stroke. Crit Care Nurs Q. 2003;26(4):296–302. [DOI] [PubMed] [Google Scholar]
- 33. Cumbler E, Zaemisch R, Graves A, Brega K, Jones W. Improving stroke alert response time: applying quality improvement methodology to the inpatient neurologic emergency. J Hosp Med. 2012;7(2):137–141. [DOI] [PubMed] [Google Scholar]
- 34. National Stroke Association’s In-hospital Stroke Quality Improvement Initiative Tool Kit. Web site http://www.stroke.org/we-can-help/healthcare-professionals/improve-your-skills/pre-hospital-acute-stroke-programs/in-hospital-stroke/in-hospital-stroke-resources. Accessed May 20, 2015.