Abstract
Spinal ependymoma commonly presents as an intramedullary tumor. We present a rare case of multicentric intradural extramedullary spinal ependymoma. A 59 years old female presented to us with spastic quadriparesis for 10 months. Magnetic resonance imaging of the spinal cord showed discretely located enhancing tumor masses from at C1-C2, C6-C7, and D4 to L3 level. Subtotal resection of the symptomatic tumor at C6-C7 and D7-D9 was done. The patient underwent radiotherapy with 50.4 Gy. At follow-up of 11 months, patient is doing well. The relevant literature is reviewed.
Keywords: Ependymoma, intradural extramedullary, multicentric
INTRODUCTION
Ependymomas are the most common intramedullary tumors in adults. They account for 60% of all intramedullary tumors. Most commonly they arise from cells lining of the central canal within the spinal cord and present as intramedullary tumor.[1] Intradural extramedullary (IDEM) ependymomas subtype are extremely rare.[1,2,3,4] Multiple IDEM ependymomas are even rarer. Only 4 such cases have been reported until.[2,3,4] We herewith present a fifth case of holocord dissemination of extramedullary ependymoma.
CASE REPORT
A 59-year-old woman complained of pain in neck over the past 6 years. About 10 months before, she came to us; she noted pain in her back which was radiating down the lower limbs to the little toes. As a result, she has to stop after walking a little while. She also started experiencing fear of fall when walking. On examination, her triceps were weak, especially on left. Flexors at the hips and quadriceps were weak. All deep reflexes were exaggerated. Magnetic resonance imaging (MRI) scan of spine showed lobulated, conglomerate and discrete IDEM tumors from D4 to L3 vertebral bodies. They were hypointense on T1W and hyperintense on T2W [Figure 1a-c]. A similar lesion was also seen in the posterior thecal sac at C6-C7 level. Smaller discrete lesions were seen in the rest of spine. The tumors showed homogenous contrast enhancement [Figure 1d and e]. Small IDEM was seen around the cervicomedullary region at C1-C2. MRI of the brain showed no tumor in cerebrum or cerebellum.
Figure 1.
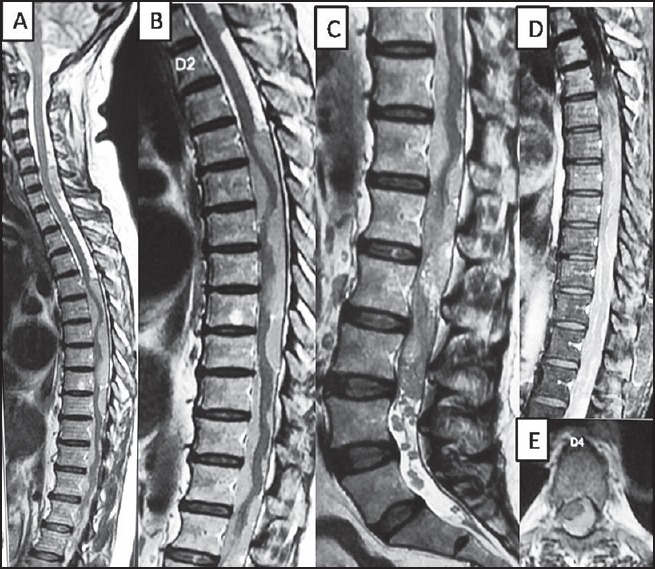
(a-c) are T2 weighted sagittal magnetic resonance imaging of spine showing multiple intradural extramedullary tumors in dorso-lumbar region. The tumor is T2 hypointense. (d and e) are T1 weighted postcontrast sagittal and axial images respectively showing areas of the tumor enhancement
On the basis of MRI image, we suspected lymphoma, and hence we decided to excise the cervical tumor for histology. C5-C7 laminectomy was done. On opening the dura, two separate pale brown, mildly vascular and fleshy tumors were seen deep to the arachnoid, one above the other. The tumors were excised. They were seen to be adherent to the spinal cord but did not expand it. Frozen section showed an ependymoma. We went on to do D7-D9 laminectomy. The visible spinal cord was covered by the tumors. They were not continuous but consisted of separate tumors one above the other as in the neck. We removed two more tumors and as in the neck, found them adherent to the spinal cord without expanding it. Postoperatively, the patient showed some improvement in her lower limbs and she could walk without fear of fall. Histopathological examination showed pseudorosettes with fibrillary processes from radially arranged tumor cells. The nuclei were oval, vesicular and hyperchromatic with small nucleoli. No mitotic activity or necrosis was seen. The above finding was suggestive of suggestive of low-grade ependymoma [Figure 2a and b].
Figure 2.
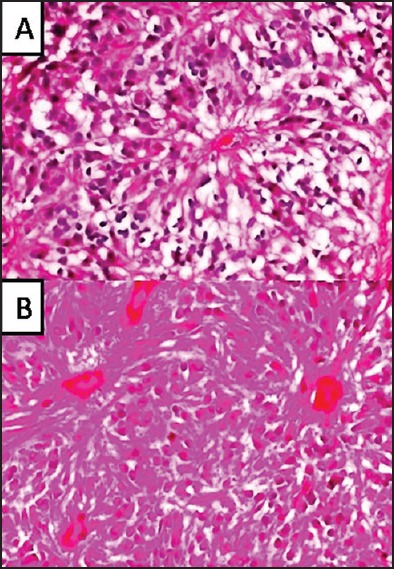
(a ×10 and b ×40) Hematoxylin and Eosin (H and E) stained images showing radially arranged ependymal cells with fibrillary processes. Pseudorosettes are seen with no mitotic activity
Six weeks after the operation, she was treated by radiotherapy with 28 fractions of 1.8 Gy-the total dose being 50.4 Gy. At follow-up of 11 months, patient is doing well.
DISCUSSION
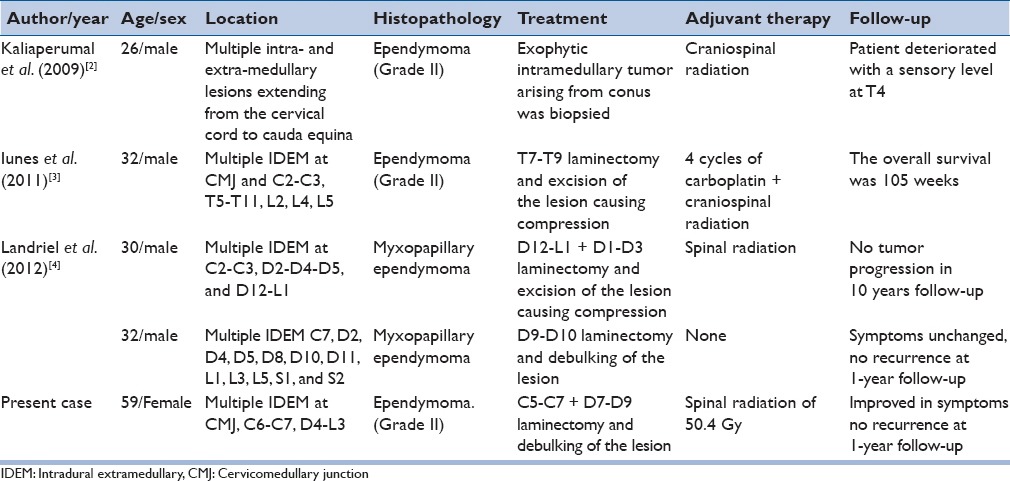
Ependymomas are the most common intramedullary tumors in adults. They account for 60% of all intramedullary tumors. The IDEM location of ependymoma is exceptional.[1] Though 20 cases of purely IDEM ependymomas have been reported in the literature, in most of these cases, single lesion was found.[1,2,3,4] Our case had multiple lesions scattered throughout the spinal axis. Only 4 such cases have been described in the literature [Table 1]. Our case is the fifth case of primary ependymomatosis of the intradural space.
Table 1.
Reported cases of multiple primary IDEM ependymoma
In a first report of IDEM ependymoma in 1951, Cooper et al. lead down criteria for IDEM gliomas. So in glial tumors presenting as IDEM lesions:
There is a lack of an apparent infiltration into the central nervous system.
There is an absence of a primary neoplastic process within the brain or spinal cord.
The tumors show encapsulation, are located along the neuraxis and are frequently association with congenital anomalies.[5] These criteria are
fulfilled here.
Ependymomas usually arise from the ependymal cells lining the ventricles and central canal of the spinal cord. However, IDEM ependymomas may arise from heterotopic ependymal cell rests were left in the IDEM space when the neural tube closed.[1]
As with typical intradural ependymomas, IDEM ependymomas occur irrespective of age but are most common in the third to fifth decades of life. The multiple IDEM ependymomas occur in second to third decade.[2,3,4] The overall prevalence of the majority of intradural ependymomas among males and females is equal, but, in multiple IDEM ependymomas are common in males [Table 1]. Our case was 59 years old male. Most spinal IDEM ependymomas affect the thoracic spine in contrast to intramedullary ependymomas, mainly located at the cervical spinal cord and the conus medullaris.[1] Our case was scattered throughout the spinal axis.
Neither the presenting symptoms nor the imaging features of IDEM ependymomas are different from other common IDEM tumors like schwannoma or meningioma. Therefore, mostly they are mistaken for schwannoma or meningioma and diagnosis is delayed.[1]
Though radical excision is recommended for ependymomas in general and near total resection is advisable for single IDEM ependymoma, it seems to be unrealistic and risky in cases of multiple IDEM ependymomas. In all the reported cases, decompression of the lesion causing mass effect was carried out followed by radiation in 2 cases and chemo-radiation in a single case.[1,2,3,4] Though role of radiation in such cases is controversial, biopsy of the symptomatic lesion followed by radiation seems to be the most rational option of this rare entity.
CONCLUSION
Multiple spinal IDEM ependymomas are very rare. They should be considered in the differential diagnosis of multiple IDEM tumors. A biopsy of the most symptomatic lesion followed by radiotherapy perhaps represents to be the most preferable option.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Son DW, Song GS, Han IH, Choi BK. Primary extramedullary ependymoma of the cervical spine: Case report and review of the literature. J Korean Neurosurg Soc. 2011;50:57–9. doi: 10.3340/jkns.2011.50.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaliaperumal C, Suttner N, Herron B, Choudhari KA. Rare case of primary spinal ependymomatosis occurring in a 26-year-old man: A case report. J Med Case Rep. 2009;3:72. doi: 10.1186/1752-1947-3-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iunes EA, Stávale JN, de Cássia Caldas Pessoa R, Ansai R, Onishi FJ, de Paiva Neto MA, et al. Multifocal intradural extramedullary ependymoma. Case report. J Neurosurg Spine. 2011;14:65–70. doi: 10.3171/2010.9.SPINE09963. [DOI] [PubMed] [Google Scholar]
- 4.Landriel F, Ajler P, Tedesco N, Bendersky D, Vecchi E. Multicentric extramedullary myxopapillary ependymomas: Two case reports and literature review. Surg Neurol Int. 2012;3:102. doi: 10.4103/2152-7806.100859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper IS, Craig WM, Kernohan JW. Tumors of the spinal cord; primary extramedullary gliomas. Surg Gynecol Obstet. 1951;92:183–90. [PubMed] [Google Scholar]


