Abstract
Background
Postpartum depression (PPD) is a maternal mental health problem that affects women from all regions of the world. Unfortunately, even in developed countries, half of the cases go undetected and, consequently, untreated. Individuals from low and middle income countries trend toward underutilization of mental health services, partly due to the limited number of available psychological resources. The primary aims of this pilot randomized controlled trial were to adapt to the Internet the Mothers and Babies Course/Curso Mamás y Bebés, a prevention of PPD intervention, to describe the characteristics of the pregnant women who engaged in the intervention site, and to obtain preliminary data on the efficacy of the Internet intervention to reduce the risk of PPD.
Methods
Pregnant women, 18 years or older who were interested in using the site for themselves were recruited and randomly assigned to a fully-automated self-help Internet intervention or to an information-only control condition. Randomized participants were invited to complete monthly depression assessments up to six months postpartum. To examine the prevention effects of the Internet intervention, pregnant women who did not meet current criteria for a major depressive episode, who engaged with the study website, and who provided depression data during the postpartum follow-up period were included in the study analyses.
Results
Participants were 111 predominantly Spanish-speaking (82.9%) and Latino/Hispanic (71.3%) pregnant women residing in 23 countries worldwide. The effect of the prevention intervention condition failed to reach significance at the a priori alpha-level. However, the observed coefficient trended in the hypothesized direction (b = −0.514, χ2 (1) = 3.43, p = .061; HR = 0.598). The benefits of receiving the e-MB Internet intervention was greater for pregnant women reporting high (vs. low) levels of prenatal depression symptoms (b = −0.605, χ2 (1) = 5.20, p =.023).
Conclusions
This study provides preliminary evidence that Internet interventions are a promising method toward expanding the reach of psychological resources to perinatal women at-risk for PPD.
Keywords: Postpartum depression, Spanish-speaking, women, prevention, Internet intervention, global mental health
1. Introduction
Major depression is a chronic and debilitating mental health problem that affects up to 16% of individuals worldwide during their lifetime (World Federation for Mental Health, 2012). It is the leading cause of disability among women (Ferrari et al., 2013) and, compared to men, women are at higher risk of experiencing major depression during their lifetime (14.0% vs. 7.3%; Steel et al., 2014). An estimated 10-15% of women experience depression during the year following childbirth, with rates as high as 20% in low- and middle-income countries (O’Hara & Swain, 1996). The rate of postpartum depression (PPD) among women in Spanish-speaking countries is elevated, ranging from 17 to 35% (Bonilla-Sepúlveda, 2010; Jadresic, Nguyen, & Halbreich, 2007; Melo, Cecatti, Pacagnella, Leite, Vulcani, & Makuch, 2012; Tannou, Gigante, Fuchs, & Busnello, 2008)). For example, self-reported PPD was up to 20% at 6 months postpartum in a sample of Mexican women (Lara, Navarrete, Nieto, Barba Martín, Navarro, & Lara-Tapia, 2014). In Spain, the prevalence of PPD among the general population ranges between 10-13% but is higher among Latin American immigrant women living in Spain (17%; Garcia-Esteve et al., 2014). In the U.S., postpartum Latinas a are at an increased risk for PPD due to immigration, higher rates of life and economic stressors, and interpersonal conflict (Diaz, Cooper, Muñoz, & Le, 2007) with rates among pregnant and postpartum Latinas ranging between 16-56% (Chaudron et al., 2005; Lara, Le, Letechipia, & Hochhausen, 2009; Zayas, Jankowski, & McKee, 2003).
The negative impact of depression on the well-being of the mother and her ability to care for a newborn child underscores the importance of identifying and treating prenatal and postpartum depression. Unfortunately, however, women often do not receive the level of care needed to address psychological issues during the perinatal (i.e., pregnancy to one year postpartum) period; approximately 50% of cases go undetected and, consequently, untreated (World Federation for Mental Health, 2012). Reduced budgetary allocations and the limited number of trained professionals are likely contributors to this global mental health disparity (World Health Organization, 2009). Thus, the need for widely accessible, low-cost, and innovative psychological resources, specifically focused on perinatal mood and affective symptoms, is needed by women from all around the world.
Prevention interventions are effective at lowering the incidence of depression (van Zoonen et al., 2014; Muñoz, Beardslee, & Leykin, 2012) and are effective at reducing the risk of PPD among non-depressed pregnant and postpartum women (Dennis & Dowswell, 2013). The applied theoretical framework of the interventions have varied but most use a cognitive behavioral therapy (CBT; e.g., Muñoz et al., 2007) or interpersonal psychotherapy (IPT; e.g., Zlotnick, Miller, Pearlstein, Howard, & Sweeney, 2006) approaches in addition to psychoeducational (e.g., Lara, Navarro, & Navarrete, 2010) and debriefing approaches (e.g., Priest, Henderson, Evans, & Hagan, 2003). These interventions have been delivered in traditional face-to-face individual and group format, over the telephone, and by home visitation by professionals, peers, and trained community members (Dennis & Dowswell, 2013). A limited number of investigations, however, have used innovative methods, such as technology-based tools, to reach perinatal women.
Internet interventions for reducing depressive symptoms among postpartum women are being developed and tested (Danaher et al., 2013; O’Mahen et al., 2013). The MomMoodBusters/MumMoodBusters (Danaher et al., 2013) was effective at reducing depression symptoms from pre- to post-intervention and up to 6-months in a sample of U.S. and Australian postpartum women. Postpartum women randomized to an 11-session behavioral activation program enhanced by the NetMums website reported postpartum depression symptoms below the Edinburgh Postnatal Depression Scale (EPDS) score when compared to those in the control condition (43.8% vs. 63%, respectively; O’Mahen et al., 2013). These Internet intervention treatment studies offer initial evidence that online interventions can be useful to postpartum women who are already struggling with depression. The design, methodology, and outcome of these trials suggest promising future replication and potential dissemination beyond the communities in which they were tested.
The studies described actively recruited postpartum women already experiencing depression. The ability to address the problem of perinatal mood and affective disorders prior to the onset of symptoms among high risk populations is of significant importance. To date, fewer Internet interventions have focused their attention on the prevention of PPD. Haga, Drozd, Brendryen, and Slinning (2013) described a feasibility and acceptance pilot study of an automated, unguided Internet intervention (Mamma Mia) to prevent PPD and to enhance well-being among perinatal women. Of the 103 pregnant and postpartum women recruited, 81 engaged with the 44-session intervention. Pregnant participants completed an average of 7 sessions and postpartum participants an average of 12 sessions. Together, participants rated the intervention to be of high quality (65%), appropriate breadth and depth (67-78%), user-friendly (M=4.2, SD=1.3, range=1-7), and credible (M=5.8, SD=0.09, range=1-7). A protocol for an online prevention RCT using the MoodGYM Internet intervention was described by Jones and colleagues (2013) recruited and randomize 175 non-depressed postpartum women to either the 5-week MoodGYM intervention or to a health-themed control condition. MoodGYM is a well-documented effective Internet intervention for depression prevention and treatment (Christensen, Griffiths, & Jorm, 2004; Griffiths, Farrer, & Christensen, 2010). The outcomes of the prevention trial by Jones and colleagues will shed light on how effective it is among postpartum women.
The status of Internet interventions for perinatal women suggest that they are a viable means to reach pregnant women in need of mental health services during and after pregnancy and that they are effective at reducing symptoms among new mothers with moderate to severe symptoms of depression. Whether they are effective in preventing new episodes of PPD is still to be determined. The flexibility of the Internet to reach women makes this an attractive addition to traditional face-to-face approaches to mental health. In many parts of the world perinatal women are already frequent users of the Internet during and after pregnancy. Thus, these online tools are likely to be highly accessible and acceptable. However, there are limitations to the existing studies in terms of global maternal mental health disparities. For example, the studies described were conducted in developed countries where there is likely greater access to healthcare by a majority of the population. Second, they relied heavily on human monitoring by the research team or mental health providers. In much of the world, resources are scarce for the provision of mental health services and the need for such care far outweighs what local providers and community leaders can offer to those who are suffering or at risk for PPD. In some cases, the interventions were lengthy and reliant on participants who were capable of accessing more advanced technologies (e.g., streaming). Finally, none of the referenced interventions were available or examined among Spanish-speaking perinatal women, which is the second most commonly spoken language worldwide (Ethnologue, 2014).
The current study builds on a body of work using the Mothers and Babies Course/Curso Mamás y Bebés (MB; Muñoz et al., 2001). Two initial trials to examine the MB using a weekly group format demonstrated reductions in the incidence of PPD which were statistically significant (Le, Zmuda, Perry, & Muñoz, 2010; Muñoz, Le, Ippen, Diaz, Urizar, Soto, et al., 2007). The original pilot trial examined a twelve session group intervention plus four individual booster sessions among a sample of low-income pregnant women seeking prenatal care in a public sector medical clinic (N=41). Relative to a usual care condition, the MB demonstrated a non-significant lower incidence of major depressive episodes (MDE) at one year postpartum when compared to women in the usual control condition (14% vs. 25%, ns). The MB was adapted by Le and colleagues (Le et al., 2010) to eight weekly group sessions with three individual booster sessions. Among a sample of low-income, Spanish-speaking pregnant immigrant women (N=217), the non-significant cumulative incidence of postpartum depression was lower for women in the MB relative to those in the usual care condition (7.8% vs. 9.6%, ns) (Le, Perry, & Stuart, 2011). More recently, a four session home visitation program of the MB was compared to usual care home visitation services (N=78) among a predominantly African American sample of pregnant and postpartum women (Tandon, Leis, Mendelson, Perry, & Kemp, 2014). Incidence of PPD at the 6-month follow-up was favorable for the home visitation version of the MB when compared to those assigned to the usual care condition (14.6% vs. 32.4%, respectively, p=.07). Leis et al. (2014) conducted a pilot study (N=10) where the MB was integrated into a pediatric primary care clinic. The intervention was reduced to 6-weekly, 2-hour group sessions, a timely adaptation given the systemic shift in healthcare. Pre/post assessments among group completers (4 or more sessions) indicated that the MB was effective at reducing depression symptoms and increasing women’s ability to regulate emotional changes.
The current study focused on adapting the face-to-face MB to a digital format, so that it can be used beyond the usual geographical constraints of studies such as those mentioned above.
The initial goals of this pilot study were a) to adapt the MB intervention to an online platform (e-MB); b) to describe the characteristics of the English- and Spanish-speaking pregnant women who engaged the fully-automated Internet intervention; and c) to examine whether the e-MB was effective at reducing the incidence of PPD. To the best of our knowledge, this is the first fully-automated Internet intervention report that includes a global sample of Spanish- and English-speaking pregnant and postpartum women.
2. Methods
2.1. Recruitment
The study web address was registered with search engines directories and used Google Ads “sponsored links” to advertise participation to Internet users (Barrera, Kelman, & Muñoz, 2014). Eligible participants (N=5,071) were female, pregnant, 18 years or older, and interested in the study website for personal use. Participants who met these initial criteria and who provided a valid email address were presented with the informed consent form. Eligible participants who refused to consent were redirected to online resources for perinatal depression. Participants in this study were recruited during the first year of the trial (January to December, 2009).
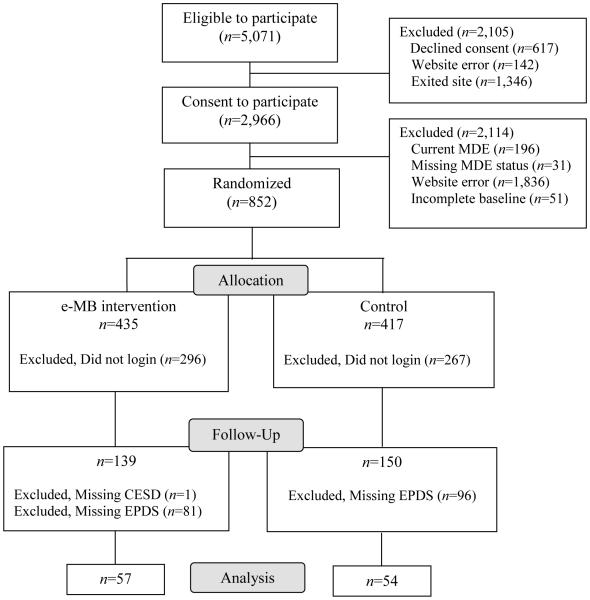
The study recruitment and enrollment flow are detailed in Figure 1. Of the 2,966 who eligible women who consented to participate and who met the prevention subsample criteria (eligibility criteria and not currently meeting DSM-IV diagnostic criteria for a MDE), 852 were randomized to the e-MB intervention or the information-only control condition. Of these, 563 (53.72%) did not log in to the website for their assigned condition and 178 (31.6%) failed to provide sufficient data to ascertain their postpartum depression status and, therefore, were excluded from the analyses. The selected subsample in this prevention analysis included pregnant women who did not meet diagnostic criteria for a current MDE at baseline, who logged in to the website of their assigned condition and who provided at least one postpartum depression score. The final sample meeting these criteria was comprised of 111 pregnant women, 57 who had been randomly assigned to the e-MB intervention and 54 to the information-only control condition. At randomization, there were no demographic or clinical differences across conditions, and the proportion of participants lost to follow-up did not differ across conditions (all ps > .05). However, regardless of condition assigned, women were more likely to log on to either condition’s site if they were older (M = 29.01 years, SD = 5.75 vs. M = 27.42 years, SD = 5.43; t (850) = 3.97, p < .01) and less depressed at the time of consent (CES-D, M = 23.16, SD = 12.70 vs. M = 25.72, SD = 13.80; t (833) = 2.69, p < .01). The majority of participants (n = 73; 65.77%) completed 2 or more postpartum follow-up assessments. There were no differences in the number of follow-up reports completed across conditions (χ2(6) = 7.42, p = .28).
Figure 1. CONSORT Flow diagram from January to December 2009.
Note. MDE: Major depressive episode; Control: Information-only brochure; e-MB: Mothers and Babies Internet Course/Curso Internet Mamás y Bebés; CES-D: Center for Epidemiological Depression Scale; EPDS: Edinburgh Postnatal Depression Scale.
2.2. Participants
Participants in this study (N = 111) had a mean age of 30.19 years (SD = 5.57) and represented pregnant women from 23 countries worldwide. A majority resided in Chile, Spain, Argentina, Mexico, Colombia, and the United States. Most were Spanish-speaking (82.9%), of Latino/Hispanic ethnic identity (71.3%), and identified their racial background as Caucasian/European (53.2%) or Mestizo (31.8%). See Table 1 for detailed demographic information.
Table 1.
Demographic characteristics of pregnant women randomized to the e-MB and control conditions
| Total N=111 |
Control n=54 |
e-MB n=57 |
|
|---|---|---|---|
| Age, M (SD) | 30.19 (5.57) | 30.59 (4.99) | 29.81 (6.09) |
| Min, Max | 18, 43 | 19, 42 | 18, 43 |
| Spanish-speaking | 82.9% | 79.6% | 86.0% |
| Ethnicity a | |||
| Latina | 71.3% | 68.1% | 74.1% |
| Race | |||
| White/European descent | 53.2% | 60.9% | 45.9% |
| Mestizo b | 31.9% | 23.9% | 39.6% |
| African descent | 2.1% | 4.4% | 0% |
| Indigenous | 3.2% | 2.2% | 4.2% |
| Other | 9.6% | 8.7% | 10.4% |
| Marital status | |||
| Married | 56.8% | 61.1% | 52.6% |
| Education | |||
| 12 years or less | 13.4% | 4.4% | 21.2% |
| Some college | 76.3% | 84.4% | 69.2% |
| College or Professional degree | 10.3% | 11.1% | 9.6% |
| Full or Part Time Employment | 70.6% | 73.6% | 67.9% |
| Country of Residence | |||
| Chile | 18.9% | 14.8% | 22.8% |
| Spain | 16.2% | 24.1% | 8.8% |
| Argentina | 11.7% | 7.4% | 15.8% |
| Mexico | 10.8% | 13.0% | 8.8% |
| Colombia | 6.3% | 3.7% | 8.8% |
| United States | 5.4% | 7.4% | 3.5% |
| Peru | 4.5% | 1.9% | 7.0% |
| United Kingdom | 4.5% | 5.6% | 3.5% |
| Paraguay | 3.6% | 5.6% | 1.8% |
| Uruguay | 2.7% | 1.9% | 3.5% |
| Bolivia | 1.8% | 0.0% | 3.5% |
| Ireland | 1.8% | 1.9% | 1.8% |
| South Africa | 1.8% | 3.7% | 0.0% |
| Venezuela | 1.8% | 3.7% | 0.0% |
| Australia | 0.9% | 0.0% | 1.8% |
| Belgium | 0.9% | 1.9% | 0.0% |
| Bulgaria | 0.9% | 0.0% | 1.8% |
| Dominican Republic | 0.9% | 0.0% | 1.8% |
| Egypt | 0.9% | 1.9% | 0.0% |
| Ecuador | 0.9% | 1.9% | 0.0% |
| Guatemala | 0.9% | 0.0% | 1.8% |
| Nicaragua | 0.9% | 0.0% | 1.8% |
| Trinidad and Tobago | 0.9% | 0.0% | 1.8% |
Note. Control: Information-only brochure; e-MB: Mothers and Babies Internet Course/Curso Internet Mamás y Bebés.
Valid percent reported only to account for missing values.
Mestizo, person of mixed Spanish and Indigenous ancestry.
2.3. Procedures
Stratified randomization by MDE history (none, past, current) and depression symptom scale cut-off scores on the Center for Epidemiological Studies-Depression (CES-D; α = .77) above or below 16 were conducted in real time among consenting participants who clicked “submit” at the end of the baseline assessment. Randomized participants were notified of their assigned condition on the final page of the baseline assessment and were invited to complete monthly follow-up assessments during pregnancy and up to six months postpartum. Additional notification of assigned condition, links and unique passwords to access online materials, and follow-up assessment invitations were sent via automated email messages. All procedures and materials were approved by the University of California, San Francisco and Palo Alto University institutional review board committees.
2.4. Intervention
Mood management Internet intervention
The Mothers and Babies Course/Curso Mamás y Bebés (MB; Muñoz et al., 2001), is a prevention of PPD intervention originally designed and tested as a face-to-face, group intervention for culturally-diverse, low-income, perinatal women (Muñoz, Le, Ippen, Diaz, Urizar, Soto, et al., 2007). The guiding theoretical principles are based on a cognitive-behavioral framework and draws from the work of Lewinsohn and colleagues (Cuijpers, Muñoz, Clarke, & Lewinsohn, 2009; Lewinsohn et al., 1985). The goal of the course is to teach women how to actively participate in creating a healthy lifestyle for themselves and their newborn infants, and incorporates concepts from social learning theory (Bandura, 1977), reality management training (Muñoz, 1996), attachment theory (Bowlby, 1969), and socio-cultural issues relevant to culturally diverse populations. The original version of the face-to-face intervention is comprised of twelve 90-minute weekly group sessions plus four booster sessions during the first year postpartum.
In the current study, the study website was designed to recruit, screen, randomize, and conduct monthly follow-up assessments to all enrolled participants using a fully-automated self-help approach (i.e., no human assistance was provided). The Mothers and Babies Internet Course/Curso Intenet de Mamás y Bebés (e-MB) includes text/informational pages, short audio/video clips, images of infants and pregnant women, and worksheets for participants to enter personalized information in response to the lesson content. The first (AZB) and senior (RFM) authors adapted the content of the 8-session version of the MB (Le et al., 2011) using an iterative process whereby edits were made to accommodate the online platform and fidelity to the intervention constructs were confirmed. Usability testing of the e-MB was conducted in a sample of Spanish- and English-speaking pregnant and postpartum women from a public sector hospital who reported variable levels of technology experience (Barrera & Muñoz, 2009). Participant feedback centered on editing text and graphics for clarity, integrating interactive material and recommendations (e.g., tips), and reframing material to not exclude (by omission) women who may have additional health concerns following childbirth (e.g., cesarean). Edits were made in response to the feedback received from usability participants prior to launching the trial on the Internet.
Participants randomized to this condition were encouraged to review each of the eight lessons as many times as they wanted and to complete and print the worksheets for later review. Access to each lesson was unlocked in sequential order upon completing the preceding lesson. Number of logins, total time spent logged into the website, and last lesson viewed were recorded by the software program. No additional website data were available for analysis.
Information-only control. Materials for this condition included an electronic version of a PPD information brochure developed by MedEd (Wisner, Logsdon, & Shanahan, 2008). The four-page brochure was accessible via a hyperlink sent to each participant in this condition. The brochure contained symptom descriptions and prevalence rates on perinatal depression, a section debunking PPD myths, and resources on how to seek support in the event of escalating symptoms. This condition was unlocked upon first log in and was available for one-time use only; printing and downloading the brochure was encouraged for later review.
2.5. Measures
Participant characteristics obtained included age, ethnicity, race, country of residence, education level, employment, marital status, and prior use of the Internet for health information. Pregnancy history assessed for gestation (weeks), expected delivery date, number of previous pregnancies, and prior pregnancy difficulties.
Center for Epidemiologic Studies-Depression Scale (CES-D; Radloff, 1977). The CES-D is a 20-item self-report instrument that assesses for the presence of depressive symptoms during the past week. Scores range from 0 to 60 with a score of 16 or greater indicating significant depressive symptoms (Weissman et al., 1977). Continuous scores were used as the basis to determine prenatal depression symptom severity at the baseline assessment. Based on vulnerability levels for future PPD as described by Le, Muñoz, Soto, Delucchi, and Ghosh Ippen (2004), depression symptom vulnerability was designated based on the baseline CES-D score as high (≥24), medium (16-23), or low (<16).
Edinburgh Postnatal Depression Scale (EPDS; Cox, Holden, & Sagovsky, 1987). The EPDS is a 10-item measure designed to screen for postnatal depression, which accounts for overlapping symptoms between depression and perinatal physical changes. The maximum score is 30; a cut-off score of 10 or greater denoted an “event” of postpartum depression given previous recommendations by the original authors (Cox Chapman, Murray, & Jones, 1996) and evidence that a cut-off score of 10 or 11 is a valid indicator of PPD among Spanish-speaking women (Garcia-Esteve, Ascaso, Ojuel, & Navarro, 2003). The EPDS was administered at each postpartum monthly follow-up assessment; a score of 10 or greater was coded as an “event” (vs. a “non-event” which a EPDS score ≤ 9).
Major Depressive Episode Screener – Current/ Lifetime version (Muñoz, 1998). The MDE Screener is a self-report tool that inquires about the nine MDE symptoms specified in the DSM-IV (APA, 2001). It assesses for the presence of five or more MDE symptoms experienced within a 2-week or longer period of time during their lifetime or during the past two weeks for the current version. In order to meet severity criteria for a MDE, symptoms must also interfere with daily activities “a lot” (Criterion C). Good psychometric properties have been demonstrated with diagnostic screeners (Muñoz, McQuaid, González, Dimas, & Rosales, 1999) and clinical interviews with Spanish-speakers (Vázquez, Muñoz, Blanco, & López, 2008). The MDE Screener was included at the baseline assessment to assess for current diagnostic status and at 3- and 6-months postpartum to assess for incidence of PPD during the follow-up period. Few participants, however, provided data on their MDE status at 3- (n=26) and 6-months (n=26) postpartum. Thus, only the baseline MDE Screener was included in the data analysis.
Acceptability of intervention materials. At the end of the information-only brochure condition and of each lesson in the e-MB, participants were invited to provide feedback on the materials viewed. Participants rated how useful (e.g., How useful were the skills and information presented in this lesson?) and understandable (e.g., How easy or difficult was it to understand the presented skills and information?) the materials were using a 1 (not at all) to 5 (very) scale, and indicated whether they thought the materials were helpful (e.g., Did the skills and information help you think of things you can do to improve your mood or how you are feeling?).
2.7. Statistical Analysis
Descriptive and chi-square analyses were conducted to examine group differences using SPSS for Windows 20.0. A survival analysis framework was implemented where the “event” observations was defined as an EPDS score ≥10 (denoting PPD) during the follow-up assessment period and “non-event” observations were defined as EPDS scores ≤ 9 (denoting negative screening for PPD). Time scores (i.e., length of time to event) for each observation were based on the number of days from the date of birth of the baby to the last follow-up EPDS completed. The Cox models utilized this same information to estimate a hazard function that is conditional on the e-MB intervention, as well as prenatal depression scores (last CES-D completed). The semi-parametric Cox approach (Cox, 1972) was selected since time can be modeled as a continuous variable, which improves power in designs with varying follow-up intervals. Cox models were specified using the PHREG procedure in SAS 9.4 (SAS Institute, 2011), and the proportional hazards assumption was evaluated using the ASSESS PH option with resampling, which revealed that the assumption of proportional risk was likely satisfied (all p’s > .09). In the first step, we estimated a main-effects only model in which the Cox hazard function was regressed on each participants’ most recent prenatal CES-D score (mean centered) and assigned condition (information-only control = 0; e-MB intervention = +1). We also examined a follow-up model incorporating the Condition×pre-CESD interaction, which allowed us to evaluate the extent to which the effect of e-MB intervention varied as a function of prenatal depression.
3. Results
3.1. Group Comparisons
The baseline depression and pregnancy characteristics of analyzed participants are summarized in Table 2. No cross-condition differences were observed for pregnancy status or general sadness during pregnancy (all ps >.30). Additionally, participants in the information-only and e-MB conditions did not statistically differ in baseline MDE or depressive symptoms, history of treatment seeking for depression, and prior use of the Internet to access information regarding depression (all ps >.26). Participants assigned to the information-only control condition spent significantly less time (M = 5.30 minutes, SD = 2.995) logged-in to their respective site, compared to those in the e-MB (M = 40.47 minutes, SD = 52.72), t (56.4) = 5.03, p < .01). This discrepancy is due (at least in part) to the fact that participants in the control condition were allowed only a single login, whereas participants in the e-MB were not limited in the number of login occasions. Follow-up analyses revealed that 33 of the 57 participants (57.9%) in the e-MB condition logged-on to the study website once, 9 (15.5%) recorded two logins, and the remaining 15 participants (26.3%) logged-on three or more times. Group differences revealed that a greater proportion of participants who logged in two or more times used the Internet for gathering depression information prior to pregnancy (41.7% vs. 15%; χ2 (1) = 5.04, p =.025) and endorsed a higher rates of past MDE (33.3% vs. 12.1%; %; χ2 (1) = 3.76, p =.052).
Table 2.
Baseline depression, pregnancy, and Internet behaviors history of pregnant women randomized to the e-MB and control conditions
| Total N = 111 |
Control n=54 |
e-MB n=57 |
Sig. Test | |
|---|---|---|---|---|
| Pregnancy | ||||
|
| ||||
| Weeks pregnant a, M (SD) | 19.98 (10.36) | 19.42 (10.42) | 20.51 (10.37) | t (109) = −0.55, p = .58 |
| First pregnancy | 53.2% | 48.2% | 57.9% | χ2 (1) = 1.06, p = .30 |
| Sadness during pregnancy | 68.5% | 68.5% | 68.4% | χ2 (1) = 0.00, p = .99 |
|
| ||||
| Depression | ||||
|
| ||||
| Prior MDE history | 17.1% | 13.0% | 21.1% | χ2 (1) = 1.28, p = .26 |
| Final prenatal depression symptoms | ||||
| CES-D score, M (SD) | 18.64 (11.18) | 17.72 (10.57) | 19.50 (11.76) | t (109) = −0.84, p = .41 |
| CES-D ≥ 16 | 51.4% | 51.9% | 50.9% | χ2 (1) = 0.01, p = .92 |
| Past treatment seeking for depression (when not pregnant) |
59.5% | 61.1% | 57.9% | χ2 (1) = 0.12, p = .73 |
| Access Internet for depression | ||||
| When not pregnant | 25.2% | 24.1% | 26.3% | χ2 (1) = 0.07, p = .79 |
| During pregnancy | 36.0% | 33.3% | 38.6% | χ2 (1) = 0.33, p = .56 |
|
| ||||
| Access of Study Materials | ||||
|
| ||||
| Time spent logged-in | 23.36 (41.61) | 5.30 (2.99) | 40.47 (52.72) | t (56.4) = 5.03, p < .01 |
Note. All N = 111. CES-D: Center for Epidemiological Depression Scale; Control: Information-only brochure; e-MB: Mothers and Babies Internet Course/Curso Internet Mamás y Bebés; MDE: Major depressive episode.
Valid percent reported only to account for missing values.
There were no significant group differences between conditions in how participants rated the acceptability of the materials included in each condition (all ps >.08). In the e-MB intervention, 28/57 rated the lessons materials. Of these, 88.9% indicated that the lessons were helpful for managing mood changes, while the content was rated as easy to understand (M = 4.12, SD = 1.02) and highly useful (M = 4.20, SD = 1.10). Similar ratings were reported for those who rated the information-only condition brochure (35/54), such that 85.7% thought it was helpful, and understanding and usefulness of the content were also rated favorably (M = 4.43, SD = 1.01 and M = 4.06, SD = 0.838, respectively).
3.2. Impact of the e-MB intervention
A significant effect for prenatal CES-D emerged (b = 0.066, χ2 (1) = 30.786, p < .01; HR = 1.069 [95% CI: 1.045, 1.095]), suggesting that each unit increase in CES-D prior to birth was associated with an 8.9% increase in reporting an EPDS score greater than 10. Although the effect of treatment condition failed to reach significance at the a priori alpha-level, the observed coefficient trended in the hypothesized direction (b = −0.514, χ2 (1) = 3.453, p = .061; HR = 0.598 [95% CI: 0.339, 1.022]) with participants receiving the e-MB intervention potentially exhibiting a lower risk of PPD. Furthermore, the average time to event (EPDS score ≥10), was later for participants randomized to the e-MB intervention relative to those in the information-only control condition, but these findings did not reach statistical significance (M = 67.9 vs. 42.45 days, respectively; t (40) = 1.64, p = .11). Model parameters and fit statistics are provided in Table 3.
Table 3.
Time-to-event (Cox) analysis predicting postpartum depression
| Predictor/Fit | Coeff. | X 2 | p-value | Hazard Ratio |
HR 95% CIs | ||
|---|---|---|---|---|---|---|---|
| LCL | UCL | ||||||
| Model A | Condition | −0.514 | 3.453 | .061 | 0.598 | 0.339 | 1.022 |
| Pre-CESD | 0.066 | 33.786 | <.001 | 1.069 | 1.045 | 1.095 | |
|
|
|||||||
| Model Fit Statistics |
−2LL = 471.314 | AIC = 475.314 | SBC = 479.569 | ||||
|
| |||||||
| Model B | Condition | −0.413 | 2.318 | .128 | 0.790 | 0.393 | 1.671 |
| Pre-CESD | 0.100 | 21.477 | <.001 | 1.124 | 1.094 | 1.217 | |
| Cond×Pre-CESD | −0.048 | 3.590 | .058 | -- | -- | -- | |
|
|
|||||||
| Model Fit Statistics |
−2LL = 467.675 | AIC = 473.675 | SBC = 480.056 | ||||
Note. Condition was dummy coded: Information-only = 0; Mothers and Babies Internet Course/Curso Internet Mamás y Bebés (e-MB) = +1; Pre-CESD was centered around the sample mean. Hazard Ratio (HR) CIs were generated from a Markov Chain (Gibbs sampler; 2000 burnin; 10000 iterations) using the bayes option in PROC PHREG.
To examine whether the e-MB intervention was more effective among women reporting higher levels of prenatal depression, the Condition×Pre-CESD interaction was examined in a follow-up analysis. A decrease in fit indices (i.e., AIC, SBC), along with a significant change in model likelihood (Δ −2LL = 6.61, p < .01) c, suggested that the Wald χ2 test for the Condition×Pre-CESD interaction (b = −0.048 [95% CI: −0.098, 0.001], χ2 (1) = 3.59, p = .058) and the model Likelihood-Ratio test (Δ −2LL = 3.639, p = .056) d fell just short of rounding to the a priori α-level, the direction of the interaction suggests that the benefits of receiving the e-MB intervention (vs. information-only control) was greater for women reporting higher levels of prenatal CES-D.
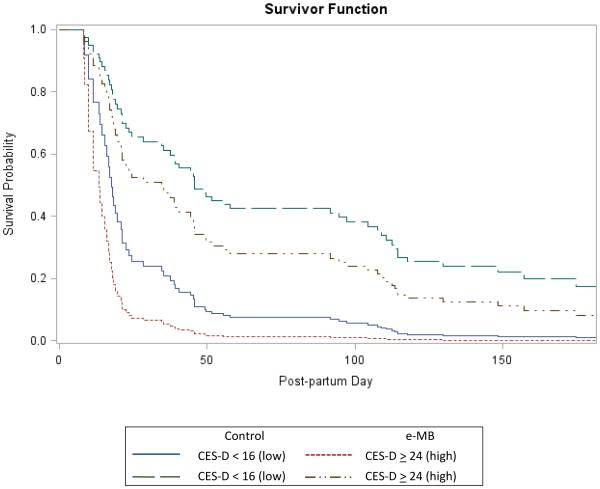
A simple-slopes approach (Aiken & West, 1991) was used to illustrate the interaction effect by estimating the conditional treatment effect at low (CES-D < 16) and high (CES-D ≥ 24) vulnerability levels of prenatal depression. Follow-up analysis revealed that the simple effect of Condition was significant among women reporting high levels of prenatal depressive symptoms (b = −0.605, χ2 (1) = 5.201, p = .023; HR = 0.546, [95% CI: 0.324, 0.936]) and the estimated hazard ratio was consistent with the predicted prevention effect (i.e., 45.4% lower risk) among women reporting high levels of prenatal CES-D. In contrast, no group differences were observed among women reporting low levels on the CES-D (b = −0.221, χ2 (1) = 0.503, p = .478; HR = 0.802 [95% CI: 0.436, 1.456]).
Figure 2 provides a plot of the estimated conditional survival functions generated using the PHREG procedure. Consistent with the simple slope analysis presented above, the survival function was similar for the information-only control and e-MB conditions when participants reported low prenatal depression vulnerability (Pre-CESD < 16). However, the protective benefits of the e-MB intervention are clearly illustrated by the divergent survival functions for participants reporting higher prenatal depression vulnerability (Pre-CESD ≥ 24). That is, participants allocated to the e-MB intervention exhibited a notably higher probability of remaining below the clinical threshold for depression (EPDS≤9) during the postpartum.
Figure 2. Number of days to postpartum EPDS ≥ 10 by assigned condition and prenatal depression vulnerability.
Note. CES-D: Center for Epidemiological Depression Scale; Control: Information-only brochure; e-MB: Mothers and Babies Internet Course/Curso Internet Mamás y Bebés; EPDS: Edinburgh Postnatal Depression Scale.
4. Discussion
This pilot study attempted to go beyond earlier prevention trials by examining a fully automated self-help Internet intervention designed to prevent PPD in a global sample of English and Spanish speaking women. Results are consistent with previous reports of the increased risk for PPD among women with elevated depression symptoms during pregnancy. Unfortunately, we failed to demonstrate a significant reduction in PPD incidence as a function of the e-MB intervention. However, we did find a significant reduction in PPD risk for women with the greatest severity of prenatal depression symptoms if they were assigned and engaged in the e-MB compared to women in the information-only condition. These preliminary findings support the continuing development and testing of the Mothers and Babies Course/Curso de Mamás y Bebés as a prevention intervention with the potential of reducing PPD among high-risk ethnically diverse pregnant women (see Le, Perry, Mendelson, Tandon, & Muñoz, 2015). More importantly, the findings have meaningful implications on the mother and the quality of care she is able to provide her newborn baby during her first year postpartum, which is critical for the development of the child and his/her relationship with the mother (Field, 2010). Few studies have focused on global communities of perinatal women, despite the emphasis and recognition that perinatal depression is a global maternal mental health problem (Rahman, Surkan, Cayetano, Rwagatare, & Dickson, 2013). Although a small percentage of the sample included endorsed a past MDE and women with a current MDE were excluded, the elevated levels of depression symptoms at study entry offers significant insight into the global need for ongoing screening of depression during and after childbirth, as well as designing and testing widely accessible resources for perinatal women at risk for or coping with depression.
In contrast to published Internet intervention studies targeting perinatal women, the primary method of recruitment in this study targeted a global community of Internet users with the goal of recruiting pregnant women interested in reducing their risk for PPD. As such, our recruitment methods cast an extremely wide net that likely resulted in attracting women who were simply browsing the Internet and, possibly, less committed to engaging in a structured online program during a time of major role transitions. In contrast to previous studies which targeted communities of perinatal women (e.g., use of the NetMums website; O’Mahen et al., 2013), this study perhaps did not attract optimal participants, that is, non-depressed pregnant women interested in learning about and reducing their risk for PPD (Barrera, Kelman, & Muñoz, 2014). The integration of “human support” or guided procedures into Internet interventions can improve participants’ experience and engagement in Internet interventions being tested. There are benefits to integrating human interactions into Internet interventions, but these are not always practical or possible when resources are limited. Further, the linear design of the intervention may have discouraged participants from continuing to view later material if earlier lessons were of minimal interest, met their desired needs for information, or appeared to require a greater time commitment than they could provide. Thus, future fully-automated Internet interventions for global communities of perinatal women can enhance the engagement and access to the intervention by integrating low-cost, flexible, and simple procedures to increase access and engagement with the intervention (e.g., email or text messaging reminders).
Findings from this study need to be considered within the context of its limitations. High attrition and low engagement were methodological concerns in this study. Low adherence and engagement are significant issues commonly discussed within the context of Internet interventions (Eysenbach, 2005) and are problematic even among highly motivated individuals. The rate of engagement with the intervention site in this study (1/8 sessions or 12.5%) was consistent with the average number of sessions completed by pregnant participants in the Haga et al. (2013) prevention study (7/44 sessions or 15.9%). Regardless, postpartum women are busy. Responding to online requests may not be a top priority, especially if they are coping with affective changes. Future Internet interventions designed for women need to consider the lives of new mothers, especially those suffering from PPD, when deciding how and when and which technology-based tools to use. The statistical approach was based on a completer analysis rather than an intent-to-treat analytical approach, which is the gold standard approach for RCTs. Thus, these results need to be interpreted as preliminary. This study did not exclude participants who accessed outside psychological services while enrolled in the study, an important methodological variable when assessing for the effectiveness of an intervention. Additionally, the modest sample size combined with considerable geographic diversity did not allow for the examination of treatment efficacy as a function of nationality and the associated cultural-demographic factors. Future studies are currently underway to examine the impact of cultural factors. Finally, the information-only condition was limited to one login, thus creating a ceiling effect for those assigned to this condition.
This study contributes to efforts to make depression prevention a global priority (Cuijpers, Beekman, & Reynolds, 2012). Despite the noted limitations, access to an evidence-based intervention to lower the risk of PPD was available to a large number of pregnant women worldwide. Recruitment results from this study demonstrate that women from all around the world are interested in using online resources to learn skills to manage psychosocial and emotional changes during and after childbirth. Pregnant and postpartum women in this study were screened for depression, educated about PPD, and informed about online resources to support perinatal women. From a public health perspective, there is a need to address maternal mental health worldwide and technology-based resources can serve as a tool to help pregnant women and new mothers cope with perinatal mood changes. This study is one of the first to examine the applicability of Internet interventions for Spanish-speaking pregnant women and for women from regions of the world where access to technology may have previously been limited but is currently growing at an increased rate (e.g., Latin America). This study is another step toward our long-term goal of improving the lives of new mothers by providing them the opportunity to learn mood management skills so they are better prepared to nurture and care for their newborn children.
Acknowledgements
This study was funded by a National Institute of Mental Health grant awarded to the first author (Barrera, P.I.; F32MH077371) and by a Robert Wood Johnson Health Disparities Seed Grant (Adler, P.I.; 053567; Recipient: Barrera). Additional funding was provided by intramural grants from the University of California Committee on Latino Research to the UCSF/SFGH Latino Mental Health Research Program (Muñoz, P.I.) and from SFGH Department of Psychiatry while under the direction of Robert Okin, M.D. to the UCSF Internet World Health Research Center (Muñoz, Director). We acknowledge and appreciate the generosity of Google, Inc., for awarding an AdWords grant to our team (Muñoz, P.I.) and the ongoing support of the Brin Wojcicki Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Latino and Hispanic are used interchangeable to reflect individuals who identify with an ethnic background that is from a Latin American country or Spain.
Abbreviations
- CES-D
- Center for Epidemiological Depression Scale
- EPDS
- Edinburgh Postnatal Depression Scale
- e-MB
- Mothers and Babies Internet Course/Curso Internet Mamás y Bebés
- MDE
- major depressive episode
- PPD
- postpartum depression
The change in model likelihood (−2LL) across Models A and B (i.e., Δ −2LL = (−2LLModel A) − (−2LLModel B) is a test-statistic distributed χ2 (1).
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th. Author; Washington, DC: 2001. Text Revision. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park: 1991. [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Barrera AZ, Kelman AR, Muñoz RF. Keywords to recruit Spanish- and English-speaking participants: Evidence from an online postpartum depression randomized controlled trial. Journal of Medical Internet Research. 2014;16(1):e6. doi: 10.2196/jmir.2999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrera AZ, Muñoz RF. Using participant feedback to guide the Web-adaptation of a postpartum depression prevention intervention. In D. Tandon (Chair), Using qualitative data to inform the development of preventive interventions for postpartum Depression. Symposium conducted at the Society for Prevention Research Annual Meeting; Washington, D.C. 2009. [Google Scholar]
- Bonilla-Sepúlveda ÓA. Depresión y factores asociados en mujeres adolescentes embarazadas y no embarazadas en Medellín (Colombia) 2009: Estudio de corte transversal. Revista Colombiana de Obstetricia y Ginecología. 2010;61(3):207–213. [Google Scholar]
- Bowlby J. Attachment and Loss. Basic Books; New York: 1969. Vol. 1: Attachment. [Google Scholar]
- Chaudron LH, Kitzman HJ, Peifer KL, Morrow S, Perez LM, Newman MC. Prevalence of maternal depressive symptoms in low income Hispanic women. The Journal of Clinical Psychiatry. 2005;66(4):418–423. doi: 10.4088/jcp.v66n0402. [DOI] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: Randomised controlled trial. BMJ. 2004;328:265–269. doi: 10.1136/bmj.37945.566632.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Cox JL, Chapman G, Murray D, Jones P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. Journal of Affective Disorders. 1996;39(3):185–189. doi: 10.1016/0165-0327(96)00008-0. [DOI] [PubMed] [Google Scholar]
- Cox DR. Regression models and life tables. Journal of the Royal Statistical Society. 1972;34:187–220. Series B. [Google Scholar]
- Cuijpers P, Beekman ATF, Reynolds CF., III Preventing Depression - A Global Priority. JAMA. 2012;307(10):1033–1034. doi: 10.1001/jama.2012.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Muñoz RF, Clarke GN, Lewinsohn PM. Psychoeducational treatment and prevention of depression: The “coping with depression” course thirty years later. Clinical Psychology Review. 2009;29:449–58. doi: 10.1016/j.cpr.2009.04.005. [DOI] [PubMed] [Google Scholar]
- Danaher BG, Milgrom J, Seeley JR, Stuart S, Schembri C, Tyler MS, Lewinshon PM. Web-Based Intervention for Postpartum Depression: Formative Research and Design of the MomMoodBooster Program. JMIR Research Protocol. 2012;1(2):e18. doi: 10.2196/resprot.2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database of Systematic Reviews. 2013:CD001134. doi: 10.1002/14651858.CD001134.pub3. Issue 2. No. DOI: 10.1002/14651858.CD001134.pub3. [DOI] [PubMed] [Google Scholar]
- Diaz MA, Cooper BA, Muñoz RF, Le HN. Interpersonal factors and perinatal depressive symptomatology in a low-income Latina sample. Cultural Diversity and Ethnic Minority Psychology. 2007;13(4):328–336. doi: 10.1037/1099-9809.13.4.328. [DOI] [PubMed] [Google Scholar]
- Ethnologue Languages of the world: Statistical summaries. 2014 Retrieved July 22, 2014, from http://www.ethnologue.com/statistics/size.
- Eysenbach G, Powell J, Englesakis M, Rizo C, Stern A. Health related virtual communities and electronic support groups: Systematic review of the effects of online peer to peer interactions. BMJ (Clinical Research Ed.) 2004;328:1166. doi: 10.1136/bmj.328.7449.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJL, Whiteford HA. Burden of depressive disorders by country, sex, age, and year: Findings from Global Burden of Disease Study 2010. PLOS Medicine. 2013;10(11):e1001547. doi: 10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T. Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behavior and Development. 2010;18(1):1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Esteve LL, Ascaso C, Ojuel J, Navarro P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. Journal of Affective Disorders. 2003;75(1):71–76. doi: 10.1016/s0165-0327(02)00020-4. [DOI] [PubMed] [Google Scholar]
- Garcia-Esteve L, Giménez AT, García PN, García PN, Terrén CA, Gelabert E. Maternity, migration, and mental health: Comparison between Spanish and Latina immigrant mothers in postpartum depression and health behaviors. In: Lara-Cinisomo S, Wisner KL, editors. Perinatal Depression among Spanish-Speaking and Latin American Women: A Global Perspective on Detection and Treatment. Springer; New York: 2014. pp. 15–37. [Google Scholar]
- Griffiths KM, Farrer L, Christensen H. The efficacy of internet interventions for depression and anxiety disorders: A review of randomised controlled trials. Medical Journal of Australia. 2010;192(11):S4–S11. doi: 10.5694/j.1326-5377.2010.tb03685.x. [DOI] [PubMed] [Google Scholar]
- Haga SM, Drozd F, Brendryen H, Slinning K. Mamma Mia: A feasibility study of a web-based intervention to reduce the risk of postpartum depression and enhance subjective well-being. JMIR Research Protocol. 2013;2(2):e29. doi: 10.2196/resprot.2659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BA, Griffiths KM, Christensen H, Ellwood D, Bennett K, Bennett A. Online cognitive behaviour training for the prevention of postnatal depression in at-risk mothers: A randomised controlled trial protocol. BMC Psychiatry. 2013;13:265. doi: 10.1186/1471-244X-13-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadresic E, Nguyen DN, Halbreich U. What does Chilean research tell us about postpartum depression (PPD)? Journal of Affective Disorders. 2007;102:237–243. doi: 10.1016/j.jad.2006.09.032. [DOI] [PubMed] [Google Scholar]
- Lara MA, Le HN, Letechipia G, Hochhausen L. Prenatal depression in Latinas in the U.S. and Mexico. Maternal Child Health. 2009;13:567–576. doi: 10.1007/s10995-008-0379-4. [DOI] [PubMed] [Google Scholar]
- Lara MA, Navarro C, Navarrete L. Outcome results of a psycho-educational intervention in pregnancy to prevent PPD: A randomized control trial. Journal of Affective Disorders. 2010;122:109–117. doi: 10.1016/j.jad.2009.06.024. [DOI] [PubMed] [Google Scholar]
- Lara MA, Navarrete L, Nieto L, Barba Martín JP, Navarro JL, Lara-Tapia H. Prevalence and incidence of perinatal depression and depressive symptoms among Mexican women. Journal of Affective Disorders . 2014;23(175C):18–24. doi: 10.1016/j.jad.2014.12.035. [DOI] [PubMed] [Google Scholar]
- Le H, Muñoz RF, Soto JA, Delucchi KL, Ghosh-Ippen C. Identifying risk for onset of major depressive episodes in low-income Latinas during pregnancy and postpartum. Hispanic Journal of Behavioral Sciences. 2004;26(4):463–482. [Google Scholar]
- Le H, Perry DF, Mendelson T, Tandon SD, Muñoz RF. Preventing perinatal depression in high risk women: Moving the Mothers and Babies Course from clinical trials to community implementation. Maternal and Child Health Journal. 2015 doi: 10.1007/s10995-015-1729-7. Advanced online publication. doi:10.1007/s10995-015-1729-7. [DOI] [PubMed] [Google Scholar]
- Le H, Perry DF, Stuart EA. Randomized controlled trial of a preventive intervention for perinatal depression in high-risk Latinas. Journal of Consulting and Clinical Psychology. 2011;79(2):135–141. doi: 10.1037/a0022492. [DOI] [PubMed] [Google Scholar]
- Le H, Zmuda J, Perry DF, Muñoz RF. Transforming an evidence-based intervention to prevent perinatal depression for low-income Latina immigrants. American Journal of Orthopsychiatry. 2010;80(1):34–45. doi: 10.1111/j.1939-0025.2010.01005.x. [DOI] [PubMed] [Google Scholar]
- Leis JA, Solomon BS, Wasserman KE, Carter TN, Mendelson T, Perry DF, Tandon SD. Preventing postpartum depression in a pediatric primary care clinic: A pilot study. Clinical Pediatrics. 2015;54(5):487–490. doi: 10.1177/0009922814536775. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hoberman H, Teri L, Hautzinger M, Reiss S, Bootzin R. Theoretical issues in behavior therapy. Academic Press; New York: 1985. [Google Scholar]
- Melo EF, Jr., Cecatti JG, Pacagnella RC, Leite DF, Vulcani DE, Makuch M. The prevalence of perinatal depression and its associated factors in two different settings in Brazil. Journal of Affective Disorders. 2012;136:1204–1208. doi: 10.1016/j.jad.2011.11.023. [DOI] [PubMed] [Google Scholar]
- Muñoz RF. Healthy Management of Reality. 1996 Retrieved on February 10, 2006, from http://www.medschool.ucsf.edu/latino/manuals.aspx.
- Muñoz RF. Preventing major depression by promoting emotion regulation: A conceptual framework and some practical tools. International Journal of Mental Health Promotion, Inaugural Issue. 1998:23–40. [Google Scholar]
- Muñoz RF. Using evidence-based Internet interventions to reduce health disparities worldwide. Journal of Medical Internet Research. 2010;12:e60. doi: 10.2196/jmir.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz RF, Beardslee WR, Leykin Y. Major depression can be prevented. American Psychologist. 2012;67(4):285–295. doi: 10.1037/a0027666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz RF, Ghosh-Ippen C, Le HN, Lieberman AF, Diaz MA, La Plante L. The Mothers and Babies Course: A Reality Management Approach Participant Manual. 2001 Retrieved July 1, 2005, from http://www.medschool.ucsf.edu/latino/manuals.aspx. [Google Scholar]
- Muñoz RF, Le H, Ippen CG, Diaz MA, Urizar GG, Jr., Soto J, Lieberman AF. Prevention of postpartum depression in low-income women: Development of the Mamás y Bebés/ Mothers and Babies Course. Cognitive and Behavioral Practice. 2007;14(1):70–83. [Google Scholar]
- Muñoz RF, McQuaid JR, Gonzalez GM, Dimas J, Rosales VA. Depression screening in a women’s clinic: Using automated Spanish-and English-language voice recognition. Journal of Consulting and Clinical Psychology. 1999;67(4):502–510. doi: 10.1037//0022-006x.67.4.502. [DOI] [PubMed] [Google Scholar]
- O'Hara MW, Swain AM. Rates and risk of postpartum depression - A meta-analysis. International Review of Psychiatry. 1996;8(1):37–54. [Google Scholar]
- O’Mahen HA, Woodford J, McGinley J, Warren FC, Richards DA, Lynch TR, Taylor RS. Internet-based behavioral activation-Treatment for postnatal depression (Netmums): A randomized controlled trial. Journal of Affective Disorders. 2013;150:814–822. doi: 10.1016/j.jad.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Priest S, Henderson J, Evans S, Hagan R. Stress debriefing after childbirth: a randomized controlled trial. Medical Journal of Australia. 2003;178:542–5. doi: 10.5694/j.1326-5377.2003.tb05355.x. [DOI] [PubMed] [Google Scholar]
- Rahman A, Surkan PJ, Cayetano CE, Rwagatare P, Dickson KE. Grand challenges: Integrating maternal mental health into maternal and child health programmes. PLOS Medicine. 2013;10(5):e1001442. doi: 10.1371/journal.pmed.1001442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, Silove D. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. International Journal of Epidemiology. 2014;43(2):476–493. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon SD, Leis JA, Mendelson T, Perry DF, Kemp K. Six-month outcomes from a randomized controlled trial to prevent perinatal depression in low-income home visiting clients. Maternal and Child Health Journal. 2014;18(4):873–881. doi: 10.1007/s10995-013-1313-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tannous L, Gigante LP, Fuchs SC, Busnello ED. Postnatal depression in Southern Brazil: Prevalence and its demographic and socioeconomic determinants. BMC Psychiatry. 2008;8:1–8. doi: 10.1186/1471-244X-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Zoonen K, Buntrock C, Ebert DD, Smit F, Reynolds CF, III, Beekman ATF, Cuijpers P. Preventing the onset of major depressive disorder: A meta-analytic review of psychological interventions. International Journal of Epidemiology. 2014;43:318–329. doi: 10.1093/ije/dyt175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vázquez FL, Muñoz RF, Blanco V, López M. Validation of Muñoz’s Mood Screener in a nonclinical Spanish population. European Journal of Psychological Assessment. 2008;24:57–64. [Google Scholar]
- Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: A validation study. American Journal of Epidemiology. 1977;106(3):203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- Wisner KL, Logsdon MC, Shanahan BR. Web-based education for postpartum depression: Conceptual development and impact. Archives of Women's Mental Health. 2008;11(5-6):377–385. doi: 10.1007/s00737-008-0030-9. [DOI] [PubMed] [Google Scholar]
- World Federation for Mental Health Depression: A global crisis. 2012 Oct; Retrieved on October 17, 2013 from http://www.who.int/mental_health/management/depression/wfmh_paper_depression_wm hd_2012.pdf.
- World Health Organization Mental health systems in selected low- and middle-income countries: A WHO-AIMS cross-national analysis. 2009 Retrieved on October 17, 2013 from http://www.who.int/mental_health/publications/who_aims_cross_national_analysis/en/
- Zlotnick C, Miller IW, Pearlstein T, Howard M, Sweeney P. A preventive intervention for pregnant women on public assistance at risk for postpartum depression. The American Journal of Psychiatry. 2006;163:1443–1445. doi: 10.1176/appi.ajp.163.8.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayas LH, Jankowski K, McKee MD. Prenatal and postpartum depression among low-income Dominican and Puerto Rican women. Hispanic Journal of Behavioral Sciences. 2003;25:370–385. [Google Scholar]