Abstract
Cholangiocytes are the epithelial cells that line the bile ducts. Along the biliary tree, two different kinds of cholangiocytes exist: small and large cholangiocytes. Each type has important differences in their biological role in physiologic and pathologic conditions. In response to injury, cholangiocytes become reactive and acquire a neuroendocrine-like phenotype with the secretion of a number of peptides. These molecules act in an autocrine/paracrine fashion to modulate cholangiocyte biology and determine the evolution of biliary damage. The failure of such mechanisms is believed to influence the progression of cholangiopathies, a group of diseases that selectively target biliary cells. Therefore, the understanding of mechanisms regulating cholangiocyte response to injury is expected to foster the development of new therapeutic options to treat biliary diseases. In this review, we discuss the most recent findings in the mechanisms driving cholangiocyte adaptation to damage, with particular emphasis on molecular pathways that are susceptible of therapeutic intervention. Morphogenic pathways (Hippo, Notch, Hedgehog), which have been recently shown to regulate biliary ontogenesis and response to injury, are also reviewed as well as the results of ongoing clinical trials evaluating new drugs for the treatment of cholangiopathies.
Keywords: Biliary Epithelium, Primary Biliary Cirrhosis, Primary Sclerosing Cholangitis
Abbreviations used in this paper: BA, biliary atresia; BDL, bile duct ligation; cAMP, adenosine 3′,5′-cyclic monophosphate; CFTR, cystic fibrosis transmembrane conductance regulator; FSH, follicle-stimulating hormone; FXR, farnesoid X receptor; GnRH, gonadotropin-releasing hormone; Hes, Hairy/Enhancer of split homolog; Hh, Hedgehog; HNF, hepatocyte nuclear factors; IL, interleukin; IP3, d-myo-inositol 1,4,5-triphosphate; LATS1/2, large tumor suppressor homolog 1/2; miR, microRNA; MT, melatonin; NGF, nerve growth factor; NICD, Notch intracellular domain; OCA, obeticholic acid; PBC, primary biliary cirrhosis; PBP, peribiliary plexus; PKA, protein kinase A; PSC, primary sclerosing cholangitis; RBP-Jκ, recombination signal binding protein immunoglobulin Jκ; Sox-9, sex-determining region Y-box 9; SR, secretin receptor; TGF, transforming growth factor; TGR5, G protein-coupled bile acid receptor; VEGF, vascular endothelial growth factor; UDCA, ursodeoxycholic acid; YAP, Yes-associated protein
Summary.
Important pathophysiological changes occur in cholangiocytes in response to injury. These will be addressed in the review, with particular emphasis on neuroendocrine factors and morphogenic signaling pathways activated in reactive cholangiocytes.
The liver, the largest gland in the body, is endowed with critical metabolic functions that involve digestion of food and clearance of toxic substances. At the level of the bile canaliculus, hepatocytes secrete bile, which is then carried to the duodenum through a complex network of bile ducts lined by cholangiocytes.1, 2, 3
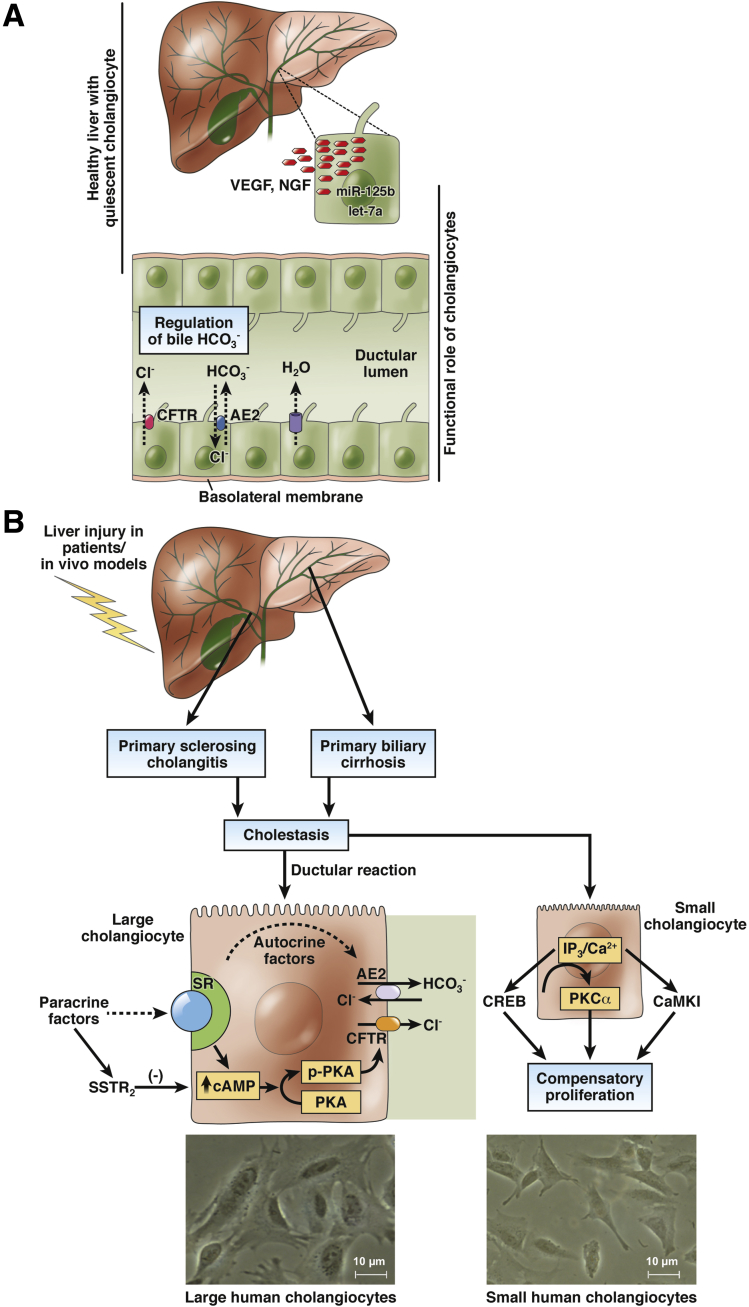
Under physiologic conditions, cholangiocytes actively contribute to the final composition and volume of bile secretion by basal and hormone-regulated events.4 In normal conditions, one of the most important and well-studied functions of cholangiocytes is secretin-induced release of bicarbonate into bile. The binding of secretin to the secretin receptor (SR) on the basolateral membrane of cholangiocytes leads to the formation of adenosine 3′,5′-cyclic monophosphate (cAMP), protein kinase A (PKA)-dependent phosphorylation of cystic fibrosis transmembrane conductance regulator (CFTR), and the subsequent extrusion of Cl− in the lumen of bile ducts. Driven by the Cl− gradient across the plasma membrane, the activation of the apical Cl−/HCO3− anion exchanger 2 (AE2) culminates in the net excretion of bicarbonate in bile,5 with passive influx of water (Figure 1). As a result, cholangiocytes participate to up to 40% of the so-called bile salt–independent bile flow.6
Figure 1.
Overview of cholangiocyte role in biliary functions. (A) Intrahepatic bile ducts are lined by both large and small cholangiocytes. Under physiologic conditions, cholangiocytes (large cholangiocytes preferentially) modify ductal bile by a sequence of secretory and absorptive processes mediated by membrane exchangers. This modification mainly leads to the formation of bicarbonate rich bile. Cholangiocytes also secrete vascular endothelial growth factor (VEGF) and nerve growth factor (NGF), which are regulated by microRNA 125b and let-7a, respectively. (B) The formation of bicarbonate rich bile is enhanced by stimulation with secretin and adenosine 3′,5′-cyclic monophosphate (cAMP), which increase in response to liver insult. The liver behaves as a neuroendocrine compartment in response to injury and starts to respond to hormones and peptides in an autocrine as well as paracrine manner. Liver injury is subsequently followed by large cholangiocyte proliferation under the influence of these factors (neurotransmitters, gastrointestinal peptides, steroids). The large, but not the small, bile ducts express secretin receptor (SR) and somatostatin receptor 2 (SSTR2) and respond to secretin and somatostatin. Biliary hyperplasia results in cholestasis, which further results in human biliary disorders such as primary sclerosing cholangitis (PSC) and primary biliary cirrhosis (PBC). Occasionally, in response to specific events injury or drug administration, small cholangiocytes proliferate by a d-myo-inositol 1,4,5-triphosphate (IP3)-mediated signaling pathway, often to compensate for the lack of large cholangiocyte proliferation and thus maintain the biliary mass. Bottom: Isolation of small (right), approximately 9-μm diameter, and large (left), approximately 13-μm diameter, cholangiocytes from human SV-40 transformed cholangiocytes (H69 cells). Small and large human cholangiocytes were purified by counterflow elutriation followed by immunoaffinity purification. Original magnification: ×800.
Cholangiocytes are the specific target of a heterogeneous group of human diseases, termed cholangiopathies, that have deep consequences on the biology of these cells.7 In the present review, we discuss the differences in the structure and function of cholangiocytes and underline the main findings in biliary pathophysiology of the last 10 years. The clinical implications of ongoing research are also specifically addressed.
Morphology, Hepatic Vasculature, and Function of Cholangiocytes
The biliary epithelium is composed of intrahepatic and extrahepatic bile ducts lined by cholangiocytes.8 The human intrahepatic biliary epithelium is classified by size: hepatic ducts (>800 μm), segmental ducts (400–800 μm), area ducts (300–400 μm), septal bile ducts (100 μm), interlobular ducts (15–100 μm), and bile ductules (<15 μm).9, 10, 11 The intrahepatic biliary epithelium of rodents is formed by ducts of different sizes, small (<15 μm in diameter) and large (>15 μm).12, 13 The cholangiocytes lining small and large bile ducts have been morphologically and functionally categorized into small and large cholangiocytes, respectively.12, 13, 14, 15 With regards to cellular structure, the small cholangiocytes are cuboidal, but the larger cholangiocytes in larger bile ducts are more columnar in shape.9, 10, 11 Moreover, small cholangiocytes are poorly specialized and have a high nucleus/cytoplasm ratio whereas large cholangiocytes are supplied with plenty of organelles and a small nucleus/cytoplasm ratio.16 The large, but not the small, cholangiocytes have cilia, which act as chemo- and mechanosensors within the bile duct lumen.17
The expression of molecules involved in secretin-stimulated biliary secretion also differs along the biliary epithelium. SR, CFTR, and anion exchanger 2 (AE2) are only expressed by large cholangiocytes and are responsible for the majority of biliary fluid secretion through the activation of a cAMP-dependent pathway.12, 13 In small cholangiocytes, on the other hand, Ca2+-activated signaling pathways seem predominant. Indeed, the activation of purinergic receptors in small and large cholangiocytes induces Ca2+-dependent Cl− secretion via transmembrane member 16A (TMEM16A), providing an alternative route to the secretin-stimulated cAMP-dependent ductal fluid secretion.18, 19
Functionally, large cAMP-dependent cholangiocytes are more susceptible to damage whereas small cholangiocytes are more resistant to liver injury.12, 20, 21, 22 During damage of large cholangiocytes, small cholangiocytes replenish the biliary epithelium. Again, the amplification of Ca2+-dependent signaling pathways in small cholangiocytes is essential in driving the de novo acquisition of large cholangiocyte phenotypes (see Figure 1).20, 21
Cholangiocytes are normally quiescent in the liver, but they respond to injury or stress by enhanced proliferation.3, 23, 24 Compensatory responses to liver injury include biliary hyperplasia, ductular reaction, and ductopenia. Biliary hyperplasia (characterized by proliferation/loss of cholangiocytes as observed in cholestatic liver diseases such as primary sclerosing cholangitis) is associated with enhanced biliary secretion of HCO3− in bile, which may be a compensatory protective mechanism for the injured biliary epithelium.25 Ductopenia is evidenced by the damage of bile ducts in response to toxins or in certain diseases such as biliary atresia.15, 20, 21, 26, 27 The hepatic artery is the main blood supplier of the biliary epithelium within the peribiliary vascular plexus (PBP). The PBP secretes a number of angiogenic factors such as vascular endothelial growth factor (VEGF) that have been shown to regulate biliary proliferation in experimental models of cholestasis.28, 29, 30, 31
Changes of the Biliary Epithelium in Pathologic Conditions
Pathophysiology of Biliary Response to Injury
Cholestatic liver diseases represent a heterogeneous group of diseases characterized by an impairment of bile formation or bile flow that can arise at the hepatocellular or cholangiocellular level.32 Emblematic diseases in this group are primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC).33 The current various animal models allow a better insight into the signaling pathways involved in the development of cholestasis. Such studies may provide potential treatment strategies to restore impaired secretory functions of hepatocytes and cholangiocytes, or to modulate the response of these cells to liver injury. Specific types of liver injury activate the proliferation of particular cholangiocyte subpopulations (ie, large/small).15, 20, 21 In most instances, biliary proliferation contributes to the major part of the ductular reaction. However, new ductules may also originate from activated progenitor cells or from cells that have entered from the circulation and differentiate into liver cells.23, 34, 35
Cholangiocyte response to injury is an articulated event, which retains a “double face” in pathophysiologic terms. After an initial insult, cholangiocytes become activated and start to proliferate. This modification is functional to compensate for the anatomic loss of biliary cells and also to sustain their secretory activities.36 In most instances, however, biliary proliferation eventually subsides, and apoptotic mechanisms become prevalent with the development of ductopenia.7 Along with proliferation, cholangiocyte response to injury is characterized by the so-called neuroendocrine-like transdifferentiation, which plays an essential role not only in sustaining biliary proliferation itself but also in immune responses, hepatic inflammation, and development of liver fibrosis.4, 23 To this extent, a number of neuroendocrine factors are synthesized de novo by reactive cholangiocyte and have been shown to modulate biliary damage by autocrine/paracrine mechanisms (Table 1).23
Table 1.
Summarizing the Main Neuroendocrine Factors Involved in Cholangiocyte Response to Injury
| Molecule | Functions | Reference |
|---|---|---|
| Secretin | Stimulates the proliferation of both normal and BDL large cholangiocytes | 38 |
| Produced by cholangiocytes and S cells, induces the up-regulation of VEGF and NGF via down-regulation of microRNA 125b and let7a | 37, 39 | |
| VEGF | As a component of PDX-1-induced neuroendocrine-like transdifferentiation of cholangiocytes, stimulates biliary proliferation via an autocrine mechanism | 29, 43 |
| Sustains cholangiocyte proliferation and PBP reactive expansion after BDL | 28 | |
| Stimulates biliary cystogenesis in cholangiocytes of the polycystic kidney rat model | 40 | |
| Participates to arterial vasculogenesis during human liver embryogenesis | 44 | |
| FSH | Stimulates cholangiocyte proliferation | 45 |
| Histamine | Stimulates small cholangiocyte proliferation via the activation of the histamine receptor H1 | 22, 47 |
| Stimulates large cholangiocyte proliferation via the activation of the histamine receptor H2 | 47 | |
| Reduces cholangiocyte proliferation via the activation of the histamine receptor H3 | 57 | |
| Increases the growth of cholangiocarcinoma cells and the synthesis of VEGF | 59 | |
| Estrogens | Stimulate cholangiocyte proliferation and prevent apoptosis in BDL rats | 49, 50 |
| NGF | Stimulates cholangiocyte proliferation (additive effect in combination with estrogens) | 48 |
| Serotonin | Inhibits cholangiocyte proliferation and secretory activities | 52, 53 |
| Melatonin | Produced by both pineal gland and cholangiocytes, inhibits biliary proliferation and secretory functions of BDL rats | 24, 54, 55 |
| Down-regulates VEGF synthesis by cholangiocytes | 56 |
BDL, bile duct ligation; FSH, follicle-stimulating hormone; NGF, nerve growth factor; PBP, peribiliary plexus; PDX-1, pancreatic and duodenal homeobox 1; VEGF, vascular endothelial growth factor.
In an elegant morphologic study, Gaudio et al31 provided strong evidence for the autocrine/paracrine role of VEGF in the regulation of biliary damage. After cholestasis induced by bile duct ligation (BDL), the PBP undergoes extensive proliferation to support the increased nutritional and functional needs of the proliferating biliary epithelium. However, the proliferation of the PBP only occurs after cholangiocytes support the autocrine role of the biliary system by secreting angiogenic factors in the regulation of biliary function.31 To demonstrate the important role of angiogenic factors in sustaining biliary growth, we have shown that secretin stimulates biliary proliferation by microRNA 125b and let7a-dependent up-regulation of VEGF-A and nerve growth factor (NGF), respectively.37 Knockout of the SR (which is only expressed by large cholangiocytes) decreases biliary hyperplasia in cholestatic mice by down-regulation of cAMP signaling.38
Other studies have demonstrated the proproliferative effect of VEGF-A and VEGF-C, which increase biliary growth of normal rats by interaction with VEGF receptors 2 and 3, respectively. The same study also showed that the in vivo administration of neutralizing antibodies for VEGF-A/C decreased BDL-induced biliary hyperplasia.29 The paracrine effect of VEGFs on biliary functions was also demonstrated in experiments where the ligation of the hepatic artery resulted in disappearance of the PBP (the source of angiogenic factors such as VEGFs), significant reduction of biliary growth (accompanied by enhanced apoptosis), and reduced secretion of VEGF and bicarbonate by cholangiocytes.28 Another study has shown that inhibition of VEGF expression in cholangiocytes by overexpression of microRNA-125b (miR-125b) and knockdown of histidine decarboxylase (the enzyme that regulates histamine synthesis) decreased BDL-induced biliary hyperplasia.39
Consistent with the role of VEGF on biliary functions, Ren et al40 have shown that VEGF plays an important role in the infection-induced increase of biliary cystogenesis in cholangiocytes of the polycystic kidney rat model. Prolonged feeding of taurocholic acid to BDL rats prevents biliary damage induced by hepatic artery ligation or caffeic acid by overexpression of VEGF-A.41, 42 Also, cholangiocyte neuroendocrine-like transdifferentiation, driven by the de novo expression of pancreatic duodenal homeobox-1, has been associated with enhanced biliary VEGF expression.43 Another study has shown that cholangiocytes generate a VEGF gradient that is key during arterial vasculogenesis, whereas angiopoietin-1 signaling from hepatoblasts participates in the remodeling of the hepatic artery to sustain the nutritional demands of the proliferating biliary epithelium.44
Biliary hyperplasia is also promoted by a number of growth factors such as NGF, follicle-stimulating hormone (FSH), gonadotropin-releasing hormone (GnRH), estrogens, and the biogenic amine histamine by the interaction with their specific receptors.22, 45, 46, 47 For example, we have shown that 1) intrahepatic bile ducts secrete NGF and express NGF receptors, and 2) NGF stimulates (in combination with estrogens) biliary proliferation by activating the ERK pathway as well as the phosphatidylinositol 3-kinase pathway.48 The decrease in intrahepatic bile duct mass (concomitant with reduced expression of estrogen receptor α and β and enhanced biliary apoptosis) supports the role of endogenous estrogens in sustaining the enhanced proliferative and secretory activities of cholangiocytes during cholestasis, which may be important during ductopenic states.49 Also supporting this concept, another study has shown that estrogens maintain biliary mass and reduce apoptosis after biliodigestive anastomosis in cholestatic BDL rats.50 A recent study has also shown that cholangiocytes express FSH and its receptor and also secrete FSH. In vivo, FSH increases biliary mass, whereas administration of antide (a GnRH antagonist blocking FSH secretion) and anti-FSH antibody to BDL rats decreases cAMP-dependent cholangiocyte proliferation and biliary mass.
Modulation of biliary FSH expression may be a target for the management of cholestatic liver diseases.45 FSH as well as other growth factors including estrogens either directly or by synergizing NGF, insulin-like growth factor 1, FSH, and VEGF have been shown to regulate the proliferative and secretive activities of cystic epithelium of polycystic liver diseases in rodent models and human cell lines. Also, GnRH (secreted by the hypothalamus as well as cholangiocytes) has been shown to stimulate biliary proliferation by both paracrine/autocrine pathways.51 Disruption of the GnRH/GnRH-receptor cascade may be an important target for the management of cholangiopathies.
Conversely, a number of other molecules have been shown to reduce cholangiocyte proliferation. For example, the activation of serotonin 1A and 1B receptors inhibits biliary hyperplasia in cholestatic rats by enhanced IP3/Ca2+/protein kinase C signaling and subsequent inhibition of the cAMP/protein kinase A/Src/extracellular signal-regulated kinase 1/2 pathway. Cholangiocytes also secrete serotonin that reduces biliary proliferation during the course of cholestasis in an autocrine fashion.52 In addition, they express the neuronal isoform of neuronal tryptophan hydroxylase, synthesize serotonin, and use serotonin as an autocrine/paracrine signal to regulate biliary remodeling.53
Other studies have provided evidence for the growth-limiting function of the hormone melatonin (MT). In cholestatic BDL rats, MT both in vivo and in vitro decreased biliary hyperplasia by cAMP-dependent down-regulation of clock gene expression through the interaction with MT1 receptor subtype.24 Furthermore, when BDL rats were housed in prolonged darkness there was reduced biliary hyperplasia and fibrosis, which was accompanied by a significant increase in the serum levels of MT likely originating from the pineal gland.54 Hepatic inhibition of arylalkylamine N-acetyltransferase (the rate-limiting enzyme regulating MT synthesis) by Vivo-morpholino sequence of arylalkylamine N-acetyltransferase (which decreases MT hepatic secretion) increases biliary growth and the expression of angiogenic factors in cholestatic rats.55, 56
A number of elegant studies have also been performed to evaluate the role of histamine on cholangiocyte proliferation. It has been found in rodent models of cholestasis that histamine increases or inhibits biliary proliferation by interacting with either H1-H2 histamine receptors (stimulatory) or H3-H4 histamine receptors (inhibitory).22, 47, 57, 58 Stimulation of H3 histamine receptors by H3 histamine receptor agonist decreases BDL-induced cholangiocyte hyperplasia via inhibition of cAMP signaling, thus suggesting a possible beneficial effect of histamine in cholangiopathies. Histamine also interacts with the H1 histamine receptor and increases the proliferation of small cholangiocytes by activation of IP3/Ca2+/calmodulin-dependent kinase I/cAMP response element-binding protein–dependent signaling.58, 59 This differential response induced by histamine may be employed in variable conditions of liver diseases where either reduction in biliary hyperplasia or regeneration of liver would be desirable, depending on the injury.
It is evident from these studies that modulation of the different receptors could be of prime importance while managing the balance between biliary growth/loss in cholangiopathies or posttransplantation. In vivo, GABA induces the damage of cAMP-dependent large cholangiocytes concomitant with de novo proliferation of small cholangiocytes, which amplify their Ca2+-dependent signaling and acquire phenotypes of large cholangiocytes to repair the damaged biliary epithelium.20, 21
Emerging Morphogenic Pathways Regulating Biliary Pathophysiology
Hippo Signaling Pathway
The Hippo signaling pathway is an evolutionarily conserved pathway that regulates bile duct differentiation and homeostasis in the liver.60 The core Hippo signaling pathway is a kinase cascade.61 The apical membrane-associated four-point-one, ezrin, radixin, moesin (FERM) domain protein neurofibromin 2 (NF2) directly binds and recruits the nuclear Dbf2-related family kinase large tumor suppressor homolog 1/2 (LATS1/2) to the plasma membrane. Membrane recruitment, in turn, promotes LATS1/2 phosphorylation by the Ste-20 family protein kinase mammalian STE20-like protein kinase 1/2 (MST1/2), together with the adaptor protein Salvador homolog 1 (SAV1). In turn, LATS1/2, in a complex with small regulator protein Mps one binder homolog A (MOB1), phosphorylates Yes-associated protein (YAP), a transcription coactivator. Phosphorylation of YAP deactivates its transcription coactivator activity through sequestering YAP in cytoplasm.
YAP is highly expressed in cholangiocytes of both mouse and human livers, which suggests that YAP plays a role in cholangiocyte biology.62, 63 By use of genetically modified mouse models, Zhang et al64 found that transcriptional regulation activity of YAP was required for bile duct development. Liver-specific Yap deletion leads to postnatal bile duct paucity due to failure formation of primitive ductal structures around E18.5. Accordingly, increasing YAP activity through ablating upstream negative regulator Nf2 significantly increases the number of primitive ductal structures and results in bile duct hyperplasia.64 However, the YAP downstream targets involved in regulating bile duct development remain to be elucidated.
YAP is also important for determining biliary cell fate.62, 65 Compared with cholangiocytes, hepatocytes maintain a lower YAP activity. Increasing hepatocyte YAP activity through ectopic YAP expression or ablating upstream negative regulator Mst1/2 dedifferentiates periportal hepatocytes into ductal cells. Furthermore, Yimlamai et al62 demonstrated that YAP regulates hepatic cell fate determination directly through Notch signaling, another critical signaling pathway for bile duct development.
Notch Signaling Pathway
The Notch signaling pathway contains four transmembrane Notch receptors (Notch-1, -2, -3, -4) and two types of cell surface ligands, Serrate/Jagged (Jag-1, -2) or Delta-like (Dll-1, -3, -4).66 The activation of the Notch signaling requires a cell-cell interaction between the “transmitting” cell expressing Notch ligands and the “receiving” cell expressing Notch receptors. Upon ligand engagement, the Notch receptor is cleaved by the γ-secretase complex, leading to the cytoplasmic release of the Notch intracellular domain (NICD). NICD will then translocate into the nucleus where it binds to the recombination signal binding protein immunoglobulin Jκ (RBP-Jκ) to displace the RBP-Jκ-associated corepressors, thereby allowing the transcription of the Notch target genes. Among them, the Hairy/Enhancer of split homologs transcription factors (Hes and Hey), the family of the hepatocyte nuclear factors (HNF) and the sex-determining region Y-box 9 (Sox-9) are involved in biliary cell differentiation. Mouse models deficient in Notch receptor Notch-2,67, 68, 69 Notch ligands Jag-1,70, 71 Notch nuclear effector RBP-Jκ,72, 73 Notch transcription target Hes-1,74 Sox-9, and HNF1β75, 76 all show defects in intrahepatic bile duct tubulogenesis during fetal development and early postnatal life. Consistently, constitutive activation of the Notch-2 intracellular domain (NICD) in hepatoblasts during development leads to ectopic formation of tubular and cystic structures, resembling early malignant biliary lesions.77, 78 In agreement with their physiologic role in the commitment of the biliary lineage, Notch2, Jagged1, Hes1, Sox-9, and HNF1β are highly expressed in biliary cells.73, 74
Hedgehog Signaling
Both immature and mature cholangiocytes produce and respond to the Hedgehog (Hh) signaling ligands Sonic hedgehog (Shh) and Indian hedgehog (Ihh).79, 80, 81 Shh and Ihh ligands then bind to their transmembrane Hedgehog receptor Patched (Ptc), which relieves the suppression of Smoothened (Smo) and leads to activation of the Glioblastoma (Gli) family of transcription factors (Gli1, Gli2, Gli3).79 The important role of the Hedgehog pathway in cholangiocyte pathogenesis has been demonstrated with a cholestatic injury model.80, 82 Dramatic increases in hepatic expression of Hh ligands and up-regulation of Hh pathway activity occur after BDL in rodents. Moreover, mice with a genetic ablation of Ptc exhibit exacerbated ductular and fibrogenic responses. However, the physiologic role and the molecular mechanism of Hedgehog signaling during maintenance of bile duct homeostasis are not fully understood and remain to be further investigated.
Role of Cholangiocytes in the Development of Human Chronic Cholestatic Conditions
Primary Sclerosing Cholangitis
Signaling mechanisms fueling PSC development are being studied in several different animal models. Among the different rodent models, MDR2−/− mice have been particularly helpful for studying the development of fibrosis in PSC.83 MDR2−/− mice have a decreased concentration of phosphatidylcholine in bile, which is known to potentiate the toxicity of bile acids. Additionally, MDR2−/− mice demonstrate leakage of bile into portal tracts, caused by disrupted tight junctions of the biliary epithelium, which is responsible for causing inflammation and fibrosis.84
Fibrosis is regulated by the expression of several pro/antifibrotic genes. For example, tissue inhibitor of metalloproteinase-1 (TIMP-1) mRNA expression is increased, whereas matrix metalloprotease 13 (MMP-13) is suppressed in this model. Additionally, a number of proinflammatory molecules such as TNFα, interleukin-1β (IL-1β), IL-6, transforming growth factor-β (TGF-β1), and interferon-γ are overexpressed in MDR2−/− mice compared with controls. Mainly based on experiments on MDR2−/− mice,85 new possible treatment options for PSC are currently being evaluated in clinical trials.
Tabibian et al86 isolated cholangiocytes from livers of PSC patients, cultured the intrahepatic cholangiocytes, and further confirmed their purity by immunofluorescence studies for cholangiocyte specific markers such as cytokeratin-19. They showed that PSC cholangiocytes expressed fewer tight junction proteins (ZO1, indicating impaired epithelial junctions) and were enlarged in size with robust filamentous structures throughout the cell body. Further, these cholangiocytes exhibited the characteristics of cellular senescence when compared with normal human cholangiocytes and H69. Next generation sequencing confirmed the elevated expression of proinflammatory cytokines and chemokines compared with controls. Thus, their study has provided targets that could potentially be used for devising treatment protocols for the management of PSC.86
As for many other diseases, genomewide association studies represent a promising approach not only for dissecting the pathophysiology of PSC but also for the identification of possible therapeutic targets. To date, a total of 16 genes have been associated with an increased risk of PSC.87 Among others, the single-nucleotide polymorphism located at chromosomal region 2q35 has attracted the interest of researchers. This particular single-nucleotide polymorphism is in close proximity to the G protein-coupled bile acid receptor (TGR5) gene and has been associated both with PSC and ulcerative colitis.88 TGR5 is the first G-protein coupled receptor for bile acids that has important roles in energy expenditure and basal metabolism.89 Interestingly, five mutations in the TGR5 gene have been shown to reduce or abolish the function of the protein.90 The activation of TGR5 in cholangiocytes is thought to stimulate bicarbonate secretion,91 possibly contributing to the protection of the biliary epithelium via the biliary bicarbonate umbrella.25
Primary Biliary Cirrhosis
PBC is an immune-mediated pathology of the biliary tree characterized by the generation of antimitochondrial antibodies directed against the pyruvate dehydrogenase complex (PDC-E2).92 Recent studies have shown that TLR9 and CD86 expression is enhanced in B cells of PBC patients.93, 94 Profiling studies for cytokines and chemokines have shown that these molecules are important in the pathogenesis of PBC.95 Further, there is often involvement of autoreactive CD4+ and CD8+ T cells in PBC. A number of animal models for PBC have been proposed. Despite the fact that none of them can perfectly recapitulate the complex interactions of the human disease, they have proved to be valuable tools to study PBC alterations and explore possible therapeutic targets. Briefly, the NOD.c3c4 mouse was the first animal model to develop PBC-like characteristics.96 The second mouse model, which is most frequently used for studying PBC, owing to the similarity of human PBC, is the one expressing the dominant negative form of TGF-β receptor II (dnTGF-βRII). This particular mouse model is characterized by higher serum level of TNFα, interferon-γ, and IL-6 when compared with control animals.97 Similarly, elevated serum cytokines, lymphocyte infiltration around portal tracts, and cholangiocyte injury are noted in a third rodent model of PBC, the IL-2Rα knockout mice model.98
In genetically susceptible individuals, environmental factors may trigger an immune-mediated injury of cholangiocytes. The immunologic events then occur in a step-by-step manner, starting from antigen presentation, T-cell differentiation, proliferation, and recruitment, and finally resulting in an effector-cell response and production of autoantibodies.99 In this context, a number of different signaling pathways have been implicated in this disease development or progression, and as such any of these steps could theoretically be targeted for treatment of PBC.
Because many pathophysiologic events of the human disease remain obscure and may differ from the animal models, caution should be implemented while evaluating the experimental effects of the manipulation of signaling pathways. Nonetheless, antibody-mediated therapy, targeted inhibition of cellular pathways relevant to immune regulation, and cell therapy methods directed toward reprogramming the immunomodulatory axis remain an intriguing opportunity to treat PBC patients.100, 101, 102
Biliary Atresia
Biliary atresia (BA) is a disease caused by obstructive cholangiopathy resulting from inflammation and fibrosis of extrahepatic bile ducts. Inflammatory reactions triggered by viral infection have been proposed as the possible cause of BA by several population studies as well as studies in murine models.103 Population studies have proved the presence of human papillomavirus, cytomegalovirus, and reovirus in the livers of BA patients.104, 105, 106 Evidence from studies in a rhesus-rotavirus infected murine model of BA as well as from fixed liver tissues from BA patients have shown that there are structural as well as pathologic changes in the extrahepatic cholangiocytes only. It was observed that primary cilia were selectively lost from the extrahepatic and not the intrahepatic cholangiocytes after rotavirus infection in experimental mice.107, 108 Jafri et al109 found that chemokine expression levels were also increased in cholangiocytes isolated from rotavirus-infected mice as well as in virus-infected cholangiocytes in culture. In their quantitative and qualitative assessments of several chemokines, they found that macrophage inflammatory protein-2 and monocyte chemotactic protein-1 were up-regulated after rotavirus infection when compared with normal in vivo and in vitro conditions.
Cholangiocyte proliferation and subsequent enlargement of extrahepatic bile ducts in BA have been linked to overexpression of IL-33 and activation of TH2 helper T cells. Li et al110 found that serum levels of IL-33 are elevated in BA patients and in the livers and bile ducts of experimental mice. Moreover, treatment of normal wild-type mice with IL-33 promoted cholangiocyte proliferation and cell growth that culminated in significantly enlarged extrahepatic bile ducts. They also found that bile ducts genetically primed to cholangiocarcinoma (by constitutive activation of the protein kinase B–Yap pathway) responded to administration of IL-33 via development of advanced tumors with intrahepatic metastases compared with controls. Such data suggest that activation of the IL-33 pathway may help biliary repair and that disruption of the same may halt carcinogenesis.110
Other studies have implicated the involvement of factors such as granzymes, which are secreted by hepatic natural killer and CD8 T cells and injure cholangiocytes in short-term culture. Consistent with in vitro data, it has been noted that in infants with BA there is increased hepatic mRNA expression of granzymes A and B.111 Thus, these studies offer multiple targets that could be manipulated to manage cholangiocyte proliferation accompanying liver conditions such as BA.
The role of microRNA in liver disease also has been increasingly recognized.112 For example, microRNA-21 (miR-21) was found to be up-regulated during the early stages of liver regeneration by targeting the Pellino-1 antibody.113 The Let-7 family members miR-127, miR-26a, miR-34a, and miR-23b were all found dysregulated during liver regeneration. Similarly, during treatment of mice with rhesus rotavirus, microRNA expression profiles were found altered in a time-dependent fashion in the extrahepatic bile ducts from the experimental animals. For instance, changes in expression pattern of miR-30b/c, miR-133a/b, miR-195, miR-200a, miR-365 have been proposed in the development of BA.114 Expansion on these reports could provide alternative treatment protocols for life-threatening conditions such as BA in small children.
Clinical Implications of Recent Advances in Biliary Research
Despite the enormous progress in recent years, the pathophysiology of cholangiopathies is far from being completely understood, which has severe consequences for the development of effective new treatments. Important signals come from clinical practice. To date, orthotopic liver transplantation remains the only curative treatment of cholestatic liver diseases, representing as much as 20% of the transplantation indications in adults.115 Moreover, symptoms such as fatigue and pruritus are often scarcely alleviated by the standard medical approaches.116, 117
Ursodeoxycholic acid (UDCA) remains the only approved drug for the treatment of fibrosing cholangiopathies. UDCA exerts its effects on multiple levels, from the protection of cholangiocytes against toxic bile acid to the stimulation of choleresis through posttranscriptional effects on hepatocellular and cholangiocyte transporters.118, 119
The administration of UDCA in a daily dose of 13–15 mg/kg has had well-established, favorable effects on the long-term survival of PBC patients.120, 121 Transplant-free survival in early-stage PBC patients treated with UDCA has been shown to be similar to healthy controls matched for age and gender.122, 123 However, not all PBC patients respond to UDCA administration. A good biochemical response was achieved only in 61% of PBC patients treated with UDCA, as defined by the Paris criteria which strongly correlate with transplant-free survival at 10 years.124
Although the administration of UDCA is universally recognized as the standard treatment for PBC, definitive evidence to recommend its use in PSC is still lacking. Moreover, the high daily doses of 28–30 mg/kg of UDCA in PSC patients have been associated with an increased risk of liver transplantation and development of esophageal varices.125 In fact, the latest available European guidelines do not propose any specific recommendation for UDCA use in PSC.126
Under these circumstances, the development of alternative therapies for cholestatic liver diseases is required, and intense research is ongoing. Promising results have recently emerged from the study of two bile acids derivatives: obeticholic acid and norursodeoxycholic acid.
Obeticholic acid (OCA), also known as INT-747, is a semisynthetic analogue of chenodeoxycholic acid that possesses a strong farnesoid X receptor (FXR) affinity.127 The role of FXR in bile acid homeostasis has clearly emerged in recent years. Endogenous bile acids bind to FXR, which in turn represses or induces the expression of various genes involved in their synthesis and secretion, such as cytochrome P450 7A1 (CYP7A1), bile salt export pump (BSEP), and sodium-taurocholate cotransporting polypeptide 115 (NTCP 115). Chenodeoxycholic acid is the most potent endogenous FXR ligand (with a 100-fold less affinity than OCA) whereas UDCA has no affinity. Interestingly, Fxr−/− mice have elevated serum bile acid levels, and the infusion of OCA in rats can stimulate bile flow and protect against lithocholic acid-induced liver damage.127, 128
Given these premises, the efficacy and safety of OCA has been recently tested in 165 PBC patients who failed to achieve a good biochemical response to UDCA alone. The results of the study demonstrated that the administration of 10, 25, or 50 mg of OCA significantly reduced levels of alkaline phosphatase, γ-glutamyltransferase, and alanine aminotransferase compared with placebo. However, a significant increase in pruritus was also registered; for all three OCA dosages the severity itching was worse compared with placebo, but the incidence of pruritus was higher only in the two higher-dosing groups.129 Phase 2 and phase 3 studies involving OCA are currently under way, with extremely promising preliminary results. Indeed, the administration of 5 or 10 mg of OCA has been shown to be superior to placebo in determining the improvement of biochemical parameters correlated with clinical outcome in patients with inadequate response to UDCA.130
Norursodeoxycholic acid (norUDCA) is a C23 homologue of UDCA with one fewer methylene group in the side chain of the molecule. The biology of norUDCA has peculiar characteristics; in fact, this bile acid derivative is usually not conjugated with taurine or glycine. It is secreted into the bile canaliculi and reabsorbed by cholangiocytes, and from there it returns to the liver. The resulting cholehepatic shunting leads to a bicarbonate rich-choleresis, which is thought to protect cholangiocytes against the toxicity of bile acids.131, 132 Fickert et al84 have tested the possible therapeutic effect of norUDCA in Mdr2−/− mice, a model for sclerosing cholangitis. They demonstrated that the administration of norUDCA ameliorated liver tests and liver histology in Mdr2−/− mice, in contrast with UDCA which had detrimental effects.85 A recent study of the same group confirmed that norUDCA improved liver injury in the selective BDL model in mice, where UDCA administration again was significantly more toxic than norUDCA.133 Based on these results, a phase 2 trial is currently recruiting patients to test the safety and efficacy of norUDCA in PSC patients.
Monoclonal antibodies have also attracted the interest of researches as a possible therapeutic tool to treat cholangiopathies. Given the encouraging results obtained with anti-CD20 antibodies in the dnTGF-βRII mouse model,134 the monoclonal antibody rituximab has been tested in a phase 1 trial in six PBC patients who have an incomplete response to UDCA. Rituximab treatment proved to be safe in PBC patients and transiently reduced serum levels of total IgG, IgM, and IgA and antimitochondrial antibodies.135 Based on the results of recent genomewide association studies showing a genetic association between variants of the IL-2 and IL-23 pathways and PBC,136, 137 a phase 2 clinical trial is currently under way to evaluate the safety and efficacy of ustekinumab, an anti-p40 monoclonal antibody.
The safety and efficacy of two different monoclonal antibodies (BTT1023 and simtuzumab) are being investigated in PSC patients. This study is currently in phase 2 clinical trials. BTT1023 is a human monoclonal antibody targeting the vascular adhesion protein-1 (VAP-1), a molecule that has been shown to stimulate the recruitment of effector lymphocytes to the liver through the up-regulation of the endothelial cell adhesion molecule MadCAM-1.138, 139 Simtuzumab is directed against the lysyl oxidase-like protein 2 (LOXL2), an enzyme that favors the cross-linking of collagen and elastin fibers.140 The results of these studies will hopefully lay the basis for possible new and effective treatments for biliary diseases.
Conclusion and Future Perspectives
Our knowledge of the mechanisms regulating biliary cell responses to injury has grown enormously in the last few decades.141 Studies from recent years have clarified that cholangiocytes are not the passive targets of biliary diseases. Indeed, reactive cholangiocytes undergo a series of profound modifications and acquire a neuroendocrine-like phenotype that allows cells to regulate the complex molecular interactions that occur in the diseased liver.4, 23 As discussed in our review, a number of molecular pathways have been shown to deeply influence the cholangiocyte response to injury. Moreover, animal models have proved an invaluable tool for dissecting the pathophysiologic changes that occur in the biliary tree in response to injury, providing important clues on the complex interactions occurring in vivo. As a result of these continuous efforts, new potential treatments for PBC and PSC have been developed and are currently being investigated in clinical trial with promising results. However, the etiology of many cholangiopathies is still obscure, and much work remains to be done to translate the large amount of data that have been collected on disease pathogenesis into effective medical treatments that can influence the natural history of biliary diseases.
Acknowledgments
The authors thank Tami Annable for editing assistance. This material is the result of work supported by resources at the Central Texas Veterans Health Care System. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Footnotes
Conflicts of interest The authors disclose no conflicts.
Funding This study was funded, in whole or in part, by the National Institutes of Health, grants DK054811 and DK076898 (to G.A. and F.M.) and by a Veterans Affairs Merit Review Grant 1I01BX001724 (to F.M. and G.A.), Veterans Affairs Research Career Award (to G.A.), the Dr. Nicholas C. Hightower Centennial Chair of Gastroenterology from Scott & White (to G.A.), and Scott & White Research Grants Program Project 90190 (to F.M.).
References
- 1.Nathanson M.H., Boyer J.L. Mechanisms and regulation of bile secretion. Hepatology. 1991;14:551–566. [PubMed] [Google Scholar]
- 2.Cardinale V., Wang Y., Carpino G. The biliary tree—a reservoir of multipotent stem cells. Nat Rev Gastroenterol Hepatol. 2012;9:231–240. doi: 10.1038/nrgastro.2012.23. [DOI] [PubMed] [Google Scholar]
- 3.Alpini G., Lenzi R., Sarkozi L. Biliary physiology in rats with bile ductular cell hyperplasia. Evidence for a secretory function of proliferated bile ductules. J Clin Invest. 1988;81:569–578. doi: 10.1172/JCI113355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Franchitto A., Onori P., Renzi A. Recent advances on the mechanisms regulating cholangiocyte proliferation and the significance of the neuroendocrine regulation of cholangiocyte pathophysiology. Ann Transl Med. 2013;1:27. doi: 10.3978/j.issn.2305-5839.2012.10.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Afroze S., Meng F., Jensen K. The physiological roles of secretin and its receptor. Ann Transl Med. 2013;1:29. doi: 10.3978/j.issn.2305-5839.2012.12.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trauner M., Boyer J.L. Bile salt transporters: molecular characterization, function, and regulation. Physiol Rev. 2003;83:633–671. doi: 10.1152/physrev.00027.2002. [DOI] [PubMed] [Google Scholar]
- 7.Lazaridis K.N., Strazzabosco M., Larusso N.F. The cholangiopathies: disorders of biliary epithelia. Gastroenterology. 2004;127:1565–1577. doi: 10.1053/j.gastro.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Alpini G., Prall R.T., LaRusso N.F. The pathobiology of biliary epithelia. In: Arias I.M., Boyer J.L., Chisari F.V., editors. The liver: biology and pathobiology. 4th ed. Lippincott Williams & Wilkins; Philadelphia: 2001. pp. 421–435. [Google Scholar]
- 9.Schaffner F., Popper H. Electron microscopic studies of normal and proliferated bile ductules. Am J Pathol. 1961;38:393–410. [PMC free article] [PubMed] [Google Scholar]
- 10.Ludwig J. New concepts in biliary cirrhosis. Semin Liver Dis. 1987;7:293–301. doi: 10.1055/s-2008-1040584. [DOI] [PubMed] [Google Scholar]
- 11.Sasaki H., Schaffner F., Popper H. Bile ductules in cholestasis: morphologic evidence for secretion and absorption in man. Lab Invest. 1967;16:84–95. [PubMed] [Google Scholar]
- 12.Alpini G., Roberts S., Kuntz S.M. Morphological, molecular, and functional heterogeneity of cholangiocytes from normal rat liver. Gastroenterology. 1996;110:1636–1643. doi: 10.1053/gast.1996.v110.pm8613073. [DOI] [PubMed] [Google Scholar]
- 13.Glaser S., Gaudio E., Rao A. Morphological and functional heterogeneity of the mouse intrahepatic biliary epithelium. Lab Invest. 2009;89:456–469. doi: 10.1038/labinvest.2009.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alpini G., Glaser S., Robertson W. Large but not small intrahepatic bile ducts are involved in secretin-regulated ductal bile secretion. Am J Physiol Gastrointest Liver Physiol. 1997;272:G1064–G1074. doi: 10.1152/ajpgi.1997.272.5.G1064. [DOI] [PubMed] [Google Scholar]
- 15.LeSage G., Glaser S., Marucci L. Acute carbon tetrachloride feeding induces damage of large but not small cholangiocytes from BDL rat liver. Am J Physiol. 1999;276:G1289–G1301. doi: 10.1152/ajpgi.1999.276.5.G1289. [DOI] [PubMed] [Google Scholar]
- 16.Benedetti A., Bassotti C., Rapino K. A morphometric study of the epithelium lining the rat intrahepatic biliary tree. J Hepatol. 1996;24:335–342. doi: 10.1016/s0168-8278(96)80014-6. [DOI] [PubMed] [Google Scholar]
- 17.Masyuk A.I., Masyuk T.V., LaRusso N.F. Cholangiocyte primary cilia in liver health and disease. Dev Dyn. 2008;237:2007–2012. doi: 10.1002/dvdy.21530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Woo K., Sathe M., Kresge C. Adenosine triphosphate release and purinergic (P2) receptor-mediated secretion in small and large mouse cholangiocytes. Hepatology. 2010;52:1819–1828. doi: 10.1002/hep.23883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dutta A.K., Khimji A.K., Kresge C. Identification and functional characterization of TMEM16A, a Ca2+-activated Cl− channel activated by extracellular nucleotides, in biliary epithelium. J Biol Chem. 2011;286:766–776. doi: 10.1074/jbc.M110.164970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mancinelli R., Franchitto A., Gaudio E. After damage of large bile ducts by gamma-aminobutyric acid, small ducts replenish the biliary tree by amplification of calcium-dependent signaling and de novo acquisition of large cholangiocyte phenotypes. Am J Pathol. 2010;176:1790–1800. doi: 10.2353/ajpath.2010.090677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mancinelli R., Franchitto A., Glaser S. GABA induces the differentiation of small into large cholangiocytes by activation of Ca2+/CaMK I-dependent adenylyl cyclase 8. Hepatology. 2013;58:251–263. doi: 10.1002/hep.26308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Francis H., Glaser S., DeMorrow S. Small mouse cholangiocytes proliferate in response to H1 histamine receptor stimulation by activation of the IP3/CaMK I/CREB pathway. Am J Physiol Cell Physiol. 2008;295:C499–C513. doi: 10.1152/ajpcell.00369.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alvaro D., Mancino M.G., Glaser S. Proliferating cholangiocytes: a neuroendocrine compartment in the diseased liver. Gastroenterology. 2007;132:415–431. doi: 10.1053/j.gastro.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 24.Renzi A., Glaser S., DeMorrow S. Melatonin inhibits cholangiocyte hyperplasia in cholestatic rats by interaction with MT1 but not MT2 melatonin receptors. Am J Physiol Gastrointest Liver Physiol. 2011;301:G634–G643. doi: 10.1152/ajpgi.00206.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beuers U., Hohenester S., de Buy Wenniger L.J. The biliary HCO3− umbrella: a unifying hypothesis on pathogenetic and therapeutic aspects of fibrosing cholangiopathies. Hepatology. 2010;52:1489–1496. doi: 10.1002/hep.23810. [DOI] [PubMed] [Google Scholar]
- 26.Yamaguti D.C., Patricio F.R. Morphometrical and immunohistochemical study of intrahepatic bile ducts in biliary atresia. Eur J Gastroenterol Hepatol. 2011;23:759–765. doi: 10.1097/MEG.0b013e32832e9df0. [DOI] [PubMed] [Google Scholar]
- 27.Kumagi T., Guindi M., Fischer S.E. Baseline ductopenia and treatment response predict long-term histological progression in primary biliary cirrhosis. Am J Gastroenterol. 2010;105:2186–2194. doi: 10.1038/ajg.2010.216. [DOI] [PubMed] [Google Scholar]
- 28.Gaudio E., Barbaro B., Alvaro D. Administration of r-VEGF-A prevents hepatic artery ligation-induced bile duct damage in bile duct ligated rats. Am J Physiol Gastrointest Liver Physiol. 2006;291:G307–G317. doi: 10.1152/ajpgi.00507.2005. [DOI] [PubMed] [Google Scholar]
- 29.Gaudio E., Barbaro B., Alvaro D. Vascular endothelial growth factor stimulates rat cholangiocyte proliferation via an autocrine mechanism. Gastroenterology. 2006;130:1270–1282. doi: 10.1053/j.gastro.2005.12.034. [DOI] [PubMed] [Google Scholar]
- 30.Glaser S., Gaudio E., Alpini G. Vascular factors, angiogenesis and biliary tract disease. Curr Opin Gastroenterol. 2010;26:246–250. doi: 10.1097/MOG.0b013e3283369d19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gaudio E., Onori P., Pannarale L. Hepatic microcirculation and peribiliary plexus in experimental biliary cirrhosis: a morphological study. Gastroenterology. 1996;111:1118–1124. doi: 10.1016/s0016-5085(96)70081-1. [DOI] [PubMed] [Google Scholar]
- 32.Poupon R. Liver alkaline phosphatase: a missing link between choleresis and biliary inflammation. Hepatology. 2015;61:2080–2090. doi: 10.1002/hep.27715. [DOI] [PubMed] [Google Scholar]
- 33.Padda M.S., Sanchez M., Akhtar A.J. Drug-induced cholestasis. Hepatology. 2011;53:1377–1387. doi: 10.1002/hep.24229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Azmaiparashvili E., Berishvili E., Kakabadze Z. Ductular reaction at the early terms of common bile duct ligation in the rats. Acta Biol Hung. 2012;63:321–332. doi: 10.1556/ABiol.63.2012.3.2. [DOI] [PubMed] [Google Scholar]
- 35.Cardinale V., Wang Y., Carpino G. Multipotent stem/progenitor cells in human biliary tree give rise to hepatocytes, cholangiocytes, and pancreatic islets. Hepatology. 2011;54:2159–2172. doi: 10.1002/hep.24590. [DOI] [PubMed] [Google Scholar]
- 36.Lesage G., Glaser S.S., Gubba S. Regrowth of the rat biliary tree after 70% partial hepatectomy is coupled to increased secretin-induced ductal secretion. Gastroenterology. 1996;111:1633–1644. doi: 10.1016/s0016-5085(96)70027-6. [DOI] [PubMed] [Google Scholar]
- 37.Glaser S., Meng F., Han Y. Secretin stimulates biliary cell proliferation by regulating expression of microRNA 125b and microRNA let7a in mice. Gastroenterology. 2014;146:1795–1808.e12. doi: 10.1053/j.gastro.2014.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Glaser S., Lam I.P., Franchitto A. Knockout of secretin receptor reduces large cholangiocyte hyperplasia in mice with extrahepatic cholestasis induced by bile duct ligation. Hepatology. 2010;52:204–214. doi: 10.1002/hep.23657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meng F., Onori P., Hargrove L. Regulation of the histamine/VEGF axis by miR-125b during cholestatic liver injury in mice. Am J Pathol. 2014;184:662–673. doi: 10.1016/j.ajpath.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 40.Ren X.S., Sato Y., Harada K. Biliary infection may exacerbate biliary cystogenesis through the induction of VEGF in cholangiocytes of the polycystic kidney (PCK) rat. Am J Pathol. 2011;179:2845–2854. doi: 10.1016/j.ajpath.2011.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Glaser S., Onori P., Gaudio E. Taurocholic acid prevents biliary damage induced by hepatic artery ligation in cholestatic rats. Dig Liver Dis. 2010;42:709–717. doi: 10.1016/j.dld.2010.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mancinelli R., Onori P., Gaudio E. Taurocholate feeding to bile duct ligated rats prevents caffeic acid-induced bile duct damage by changes in cholangiocyte VEGF expression. Exp Biol Med (Maywood) 2009;234:462–474. doi: 10.3181/0808-RM-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marzioni M., Saccomanno S., Candelaresi C. Pancreatic Duodenal Homeobox-1 de novo expression drives cholangiocyte neuroendocrine-like transdifferentiation. J Hepatol. 2010;53:663–670. doi: 10.1016/j.jhep.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 44.Fabris L., Cadamuro M., Libbrecht L. Epithelial expression of angiogenic growth factors modulate arterial vasculogenesis in human liver development. Hepatology. 2008;47:719–728. doi: 10.1002/hep.22015. [DOI] [PubMed] [Google Scholar]
- 45.Mancinelli R., Onori P., Gaudio E. Follicle-stimulating hormone increases cholangiocyte proliferation by an autocrine mechanism via cAMP-dependent phosphorylation of ERK1/2 and Elk-1. Am J Physiol Gastrointest Liver Physiol. 2009;297:G11–G26. doi: 10.1152/ajpgi.00025.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jensen K., Marzioni M., Munshi K. Autocrine regulation of biliary pathology by activated cholangiocytes. Am J Physiol Gastrointest Liver Physiol. 2012;302:G473–G483. doi: 10.1152/ajpgi.00482.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Francis H.L., DeMorrow S., Franchitto A. Histamine stimulates the proliferation of small and large cholangiocytes by activation of both IP3/Ca2+ and cAMP-dependent signaling mechanisms. Lab Invest. 2012;92:282–294. doi: 10.1038/labinvest.2011.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gigliozzi A., Alpini G., Baroni G.S. Nerve growth factor modulates the proliferative capacity of the intrahepatic biliary epithelium in experimental cholestasis. Gastroenterology. 2004;127:1198–1209. doi: 10.1053/j.gastro.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 49.Alvaro D., Alpini G., Onori P. Effect of ovariectomy on the proliferative capacity of intrahepatic rat cholangiocytes. Gastroenterology. 2002;123:336–344. doi: 10.1053/gast.2002.34169. [DOI] [PubMed] [Google Scholar]
- 50.Svegliati-Baroni G., Ghiselli R., Marzioni M. Estrogens maintain bile duct mass and reduce apoptosis after biliodigestive anastomosis in bile duct ligated rats. J Hepatol. 2006;44:1158–1166. doi: 10.1016/j.jhep.2005.10.032. [DOI] [PubMed] [Google Scholar]
- 51.Ray D., Han Y., Franchitto A. Gonadotropin-releasing hormone stimulates biliary proliferation by paracrine/autocrine mechanisms. Am J Pathol. 2015;185:1061–1072. doi: 10.1016/j.ajpath.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marzioni M., Glaser S., Francis H. Autocrine/paracrine regulation of the growth of the biliary tree by the neuroendocrine hormone serotonin. Gastroenterology. 2005;128:121–137. doi: 10.1053/j.gastro.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 53.Omenetti A., Yang L., Gainetdinov R.R. Paracrine modulation of cholangiocyte serotonin synthesis orchestrates biliary remodeling in adults. Am J Physiol Gastrointest Liver Physiol. 2011;300:G303–G315. doi: 10.1152/ajpgi.00368.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Han Y., Onori P., Meng F. Prolonged exposure of cholestatic rats to complete dark inhibits biliary hyperplasia and liver fibrosis. Am J Physiol Gastrointest Liver Physiol. 2014;307:G894–G904. doi: 10.1152/ajpgi.00288.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Renzi A., DeMorrow S., Onori P. Modulation of the biliary expression of arylalkylamine N-acetyltransferase alters the autocrine proliferative responses of cholangiocytes in rats. Hepatology. 2013;57:1130–1141. doi: 10.1002/hep.26105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Renzi A., Mancinelli R., Onori P. Inhibition of the liver expression of arylalkylamine N-acetyltransferase increases the expression of angiogenic factors in cholangiocytes. Hepatobiliary Surg Nutr. 2014;3:4–10. doi: 10.3978/j.issn.2304-3881.2014.01.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Francis H., Franchitto A., Ueno Y. H3 histamine receptor agonist inhibits biliary growth of BDL rats by downregulation of the cAMP-dependent PKA/ERK1/2/ELK-1 pathway. Lab Invest. 2007;87:473–487. doi: 10.1038/labinvest.3700533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Francis H., Meng F., Gaudio E. Histamine regulation of biliary proliferation. J Hepatol. 2012;56:1204–1206. doi: 10.1016/j.jhep.2011.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Francis H., DeMorrow S., Venter J. Inhibition of histidine decarboxylase ablates the autocrine tumorigenic effects of histamine in human cholangiocarcinoma. Gut. 2012;61:753–764. doi: 10.1136/gutjnl-2011-300007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yu F.X., Meng Z., Plouffe S.W. Hippo pathway regulation of gastrointestinal tissues. Annu Rev Physiol. 2015;77:201–227. doi: 10.1146/annurev-physiol-021014-071733. [DOI] [PubMed] [Google Scholar]
- 61.Yin F., Yu J., Zheng Y. Spatial organization of Hippo signaling at the plasma membrane mediated by the tumor suppressor Merlin/NF2. Cell. 2013;154:1342–1355. doi: 10.1016/j.cell.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yimlamai D., Christodoulou C., Galli G.G. Hippo pathway activity influences liver cell fate. Cell. 2014;157:1324–1338. doi: 10.1016/j.cell.2014.03.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bai H., Gayyed M.F., Lam-Himlin D.M. Expression of Yes-associated protein modulates Survivin expression in primary liver malignancies. Hum Pathol. 2012;43:1376–1385. doi: 10.1016/j.humpath.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang N., Bai H., David K.K. The Merlin/NF2 tumor suppressor functions through the YAP oncoprotein to regulate tissue homeostasis in mammals. Dev Cell. 2010;19:27–38. doi: 10.1016/j.devcel.2010.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fitamant J., Kottakis F., Benhamouche S. YAP inhibition restores hepatocyte differentiation in advanced HCC, leading to tumor regression. Cell Rep. 2015 doi: 10.1016/j.celrep.2015.02.027. http://dx/doi.org/10.1016/j.celrep.2015.02.027 Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Morell C.M., Fiorotto R., Fabris L. Notch signalling beyond liver development: emerging concepts in liver repair and oncogenesis. Clin Res Hepatol Gastroenterol. 2013;37:447–454. doi: 10.1016/j.clinre.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 67.Geisler F., Nagl F., Mazur P.K. Liver-specific inactivation of Notch2, but not Notch1, compromises intrahepatic bile duct development in mice. Hepatology. 2008;48:607–616. doi: 10.1002/hep.22381. [DOI] [PubMed] [Google Scholar]
- 68.Fiorotto R., Raizner A., Morell C.M. Notch signaling regulates tubular morphogenesis during repair from biliary damage in mice. J Hepatol. 2013;59:124–130. doi: 10.1016/j.jhep.2013.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lozier J., McCright B., Gridley T. Notch signaling regulates bile duct morphogenesis in mice. PLoS One. 2008;3:e1851. doi: 10.1371/journal.pone.0001851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hofmann J.J., Zovein A.C., Koh H. Jagged1 in the portal vein mesenchyme regulates intrahepatic bile duct development: insights into Alagille syndrome. Development. 2010;137:4061–4072. doi: 10.1242/dev.052118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Loomes K.M., Russo P., Ryan M. Bile duct proliferation in liver-specific Jag1 conditional knockout mice: effects of gene dosage. Hepatology. 2007;45:323–330. doi: 10.1002/hep.21460. [DOI] [PubMed] [Google Scholar]
- 72.Sparks E.E., Huppert K.A., Brown M.A. Notch signaling regulates formation of the three-dimensional architecture of intrahepatic bile ducts in mice. Hepatology. 2010;51:1391–1400. doi: 10.1002/hep.23431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zong Y., Panikkar A., Xu J. Notch signaling controls liver development by regulating biliary differentiation. Development. 2009;136:1727–1739. doi: 10.1242/dev.029140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kodama Y., Hijikata M., Kageyama R. The role of notch signaling in the development of intrahepatic bile ducts. Gastroenterology. 2004;127:1775–1786. doi: 10.1053/j.gastro.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 75.Antoniou A., Raynaud P., Cordi S. Intrahepatic bile ducts develop according to a new mode of tubulogenesis regulated by the transcription factor SOX9. Gastroenterology. 2009;136:2325–2333. doi: 10.1053/j.gastro.2009.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Coffinier C., Gresh L., Fiette L. Bile system morphogenesis defects and liver dysfunction upon targeted deletion of HNF1β. Development. 2002;129:1829–1838. doi: 10.1242/dev.129.8.1829. [DOI] [PubMed] [Google Scholar]
- 77.Jeliazkova P., Jors S., Lee M. Canonical Notch2 signaling determines biliary cell fates of embryonic hepatoblasts and adult hepatocytes independent of Hes1. Hepatology. 2013;57:2469–2479. doi: 10.1002/hep.26254. [DOI] [PubMed] [Google Scholar]
- 78.Tchorz J.S., Kinter J., Muller M. Notch2 signaling promotes biliary epithelial cell fate specification and tubulogenesis during bile duct development in mice. Hepatology. 2009;50:871–879. doi: 10.1002/hep.23048. [DOI] [PubMed] [Google Scholar]
- 79.Omenetti A., Diehl A.M. Hedgehog signaling in cholangiocytes. Curr Opin Gastroenterol. 2011;27:268–275. doi: 10.1097/MOG.0b013e32834550b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Omenetti A., Yang L., Li Y.X. Hedgehog-mediated mesenchymal-epithelial interactions modulate hepatic response to bile duct ligation. Lab Invest. 2007;87:499–514. doi: 10.1038/labinvest.3700537. [DOI] [PubMed] [Google Scholar]
- 81.Omenetti A., Porrello A., Jung Y. Hedgehog signaling regulates epithelial-mesenchymal transition during biliary fibrosis in rodents and humans. J Clin Invest. 2008;118:3331–3342. doi: 10.1172/JCI35875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Omenetti A., Popov Y., Jung Y. The hedgehog pathway regulates remodelling responses to biliary obstruction in rats. Gut. 2008;57:1275–1282. doi: 10.1136/gut.2008.148619. [DOI] [PubMed] [Google Scholar]
- 83.Popov Y., Patsenker E., Fickert P. Mdr2 (Abcb4)−/− mice spontaneously develop severe biliary fibrosis via massive dysregulation of pro- and antifibrogenic genes. J Hepatol. 2005;43:1045–1054. doi: 10.1016/j.jhep.2005.06.025. [DOI] [PubMed] [Google Scholar]
- 84.Fickert P., Fuchsbichler A., Wagner M. Regurgitation of bile acids from leaky bile ducts causes sclerosing cholangitis in Mdr2 (Abcb4) knockout mice. Gastroenterology. 2004;127:261–274. doi: 10.1053/j.gastro.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 85.Fickert P., Wagner M., Marschall H.U. 24-norUrsodeoxycholic acid is superior to ursodeoxycholic acid in the treatment of sclerosing cholangitis in Mdr2 (Abcb4) knockout mice. Gastroenterology. 2006;130:465–481. doi: 10.1053/j.gastro.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 86.Tabibian J.H., Trussoni C.E., O’Hara S.P. Characterization of cultured cholangiocytes isolated from livers of patients with primary sclerosing cholangitis. Lab Invest. 2014;94:1126–1133. doi: 10.1038/labinvest.2014.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Folseraas T., Liaskou E., Anderson C.A. Genetics in PSC: what do the “risk genes” teach us? Clin Rev Allergy Immunol. 2015;48:154–164. doi: 10.1007/s12016-014-8417-z. [DOI] [PubMed] [Google Scholar]
- 88.Karlsen T.H., Franke A., Melum E. Genome-wide association analysis in primary sclerosing cholangitis. Gastroenterology. 2010;138:1102–1111. doi: 10.1053/j.gastro.2009.11.046. [DOI] [PubMed] [Google Scholar]
- 89.Duboc H., Tache Y., Hofmann A.F. The bile acid TGR5 membrane receptor: from basic research to clinical application. Dig Liver Dis. 2014;46:302–312. doi: 10.1016/j.dld.2013.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hov J.R., Keitel V., Laerdahl J.K. Mutational characterization of the bile acid receptor TGR5 in primary sclerosing cholangitis. PLoS One. 2010;5:e12403. doi: 10.1371/journal.pone.0012403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Keitel V., Haussinger D. TGR5 in the biliary tree. Dig Dis. 2011;29:45–47. doi: 10.1159/000324127. [DOI] [PubMed] [Google Scholar]
- 92.Dyson J.K., Hirschfield G.M., Adams D.H. Novel therapeutic targets in primary biliary cirrhosis. Nat Rev Gastroenterol Hepatol. 2015;12:147–158. doi: 10.1038/nrgastro.2015.12. [DOI] [PubMed] [Google Scholar]
- 93.Kikuchi K., Lian Z.X., Yang G.X. Bacterial CpG induces hyper-IgM production in CD27+ memory B cells in primary biliary cirrhosis. Gastroenterology. 2005;128:304–312. doi: 10.1053/j.gastro.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 94.Moritoki Y., Lian Z.X., Wulff H. AMA production in primary biliary cirrhosis is promoted by the TLR9 ligand CpG and suppressed by potassium channel blockers. Hepatology. 2007;45:314–322. doi: 10.1002/hep.21522. [DOI] [PubMed] [Google Scholar]
- 95.Manousou P., Kolios G., Drygiannakis I. CXCR3 axis in patients with primary biliary cirrhosis: a possible novel mechanism of the effect of ursodeoxycholic acid. Clin Exp Immunol. 2013;172:9–15. doi: 10.1111/cei.12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Irie J., Wu Y., Wicker L.S. NOD.c3c4 congenic mice develop autoimmune biliary disease that serologically and pathogenetically models human primary biliary cirrhosis. J Exp Med. 2006;203:1209–1219. doi: 10.1084/jem.20051911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Oertelt S., Lian Z.X., Cheng C.M. Anti-mitochondrial antibodies and primary biliary cirrhosis in TGF-β receptor II dominant-negative mice. J Immunol. 2006;177:1655–1660. doi: 10.4049/jimmunol.177.3.1655. [DOI] [PubMed] [Google Scholar]
- 98.Wakabayashi K., Lian Z.X., Moritoki Y. IL-2 receptor alpha−/− mice and the development of primary biliary cirrhosis. Hepatology. 2006;44:1240–1249. doi: 10.1002/hep.21385. [DOI] [PubMed] [Google Scholar]
- 99.Jones D.E. Pathogenesis of primary biliary cirrhosis. Gut. 2007;56:1615–1624. doi: 10.1136/gut.2007.122150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dhirapong A., Yang G.X., Nadler S. Therapeutic effect of cytotoxic T lymphocyte antigen 4/immunoglobulin on a murine model of primary biliary cirrhosis. Hepatology. 2013;57:708–715. doi: 10.1002/hep.26067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tanaka H., Zhang W., Yang G.X. Successful immunotherapy of autoimmune cholangitis by adoptive transfer of forkhead box protein 3+ regulatory T cells. Clin Exp Immunol. 2014;178:253–261. doi: 10.1111/cei.12415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Myers R.P., Swain M.G., Lee S.S. B-cell depletion with rituximab in patients with primary biliary cirrhosis refractory to ursodeoxycholic acid. Am J Gastroenterol. 2013;108:933–941. doi: 10.1038/ajg.2013.51. [DOI] [PubMed] [Google Scholar]
- 103.Coots A., Donnelly B., Mohanty S.K. Rotavirus infection of human cholangiocytes parallels the murine model of biliary atresia. J Surg Res. 2012;177:275–281. doi: 10.1016/j.jss.2012.05.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tyler K.L., Sokol R.J., Oberhaus S.M. Detection of reovirus RNA in hepatobiliary tissues from patients with extrahepatic biliary atresia and choledochal cysts. Hepatology. 1998;27:1475–1482. doi: 10.1002/hep.510270603. [DOI] [PubMed] [Google Scholar]
- 105.Drut R., Drut R.M., Gomez M.A. Presence of human papillomavirus in extrahepatic biliary atresia. J Pediatr Gastroenterol Nutr. 1998;27:530–535. doi: 10.1097/00005176-199811000-00007. [DOI] [PubMed] [Google Scholar]
- 106.Fischler B., Woxenius S., Nemeth A. Immunoglobulin deposits in liver tissue from infants with biliary atresia and the correlation to cytomegalovirus infection. J Pediatr Surg. 2005;40:541–546. doi: 10.1016/j.jpedsurg.2004.11.035. [DOI] [PubMed] [Google Scholar]
- 107.Karjoo S., Hand N.J., Loarca L. Extrahepatic cholangiocyte cilia are abnormal in biliary atresia. J Pediatr Gastroenterol Nutr. 2013;57:96–101. doi: 10.1097/MPG.0b013e318296e525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Chu A.S., Russo P.A., Wells R.G. Cholangiocyte cilia are abnormal in syndromic and non-syndromic biliary atresia. Mod Pathol. 2012;25:751–757. doi: 10.1038/modpathol.2011.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jafri M., Donnelly B., Bondoc A. Cholangiocyte secretion of chemokines in experimental biliary atresia. J Pediatr Surg. 2009;44:500–507. doi: 10.1016/j.jpedsurg.2008.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Li J., Razumilava N., Gores G.J. Biliary repair and carcinogenesis are mediated by IL-33-dependent cholangiocyte proliferation. J Clin Invest. 2014;124:3241–3251. doi: 10.1172/JCI73742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shivakumar P., Mourya R., Bezerra J.A. Perforin and granzymes work in synergy to mediate cholangiocyte injury in experimental biliary atresia. J Hepatol. 2014;60:370–376. doi: 10.1016/j.jhep.2013.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Finch M.L., Marquardt J.U., Yeoh G.C. Regulation of microRNAs and their role in liver development, regeneration and disease. Int J Biochem Cell Biol. 2014;54:288–303. doi: 10.1016/j.biocel.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 113.Marquez R.T., Wendlandt E., Galle C.S. MicroRNA-21 is upregulated during the proliferative phase of liver regeneration, targets Pellino-1, and inhibits NF-κB signaling. Am J Physiol Gastrointest Liver Physiol. 2010;298:G535–G541. doi: 10.1152/ajpgi.00338.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bessho K., Shanmukhappa K., Sheridan R. Integrative genomics identifies candidate microRNAs for pathogenesis of experimental biliary atresia. BMC Syst Biol. 2013;7:104. doi: 10.1186/1752-0509-7-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Carrion A.F., Bhamidimarri K.R. Liver transplant for cholestatic liver diseases. Clin Liver Dis. 2013;17:345–359. doi: 10.1016/j.cld.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 116.Griffiths L., Jones D.E. Pathogenesis of primary biliary cirrhosis and its fatigue. Dig Dis. 2014;32:615–625. doi: 10.1159/000360515. [DOI] [PubMed] [Google Scholar]
- 117.Beuers U., Kremer A.E., Bolier R. Pruritus in cholestasis: facts and fiction. Hepatology. 2014;60:399–407. doi: 10.1002/hep.26909. [DOI] [PubMed] [Google Scholar]
- 118.Roma M.G., Toledo F.D., Boaglio A.C. Ursodeoxycholic acid in cholestasis: linking action mechanisms to therapeutic applications. Clin Sci (Lond) 2011;121:523–544. doi: 10.1042/CS20110184. [DOI] [PubMed] [Google Scholar]
- 119.Beuers U. Drug insight: Mechanisms and sites of action of ursodeoxycholic acid in cholestasis. Nat Clin Pract Gastroenterol Hepatol. 2006;3:318–328. doi: 10.1038/ncpgasthep0521. [DOI] [PubMed] [Google Scholar]
- 120.Poupon R.E., Lindor K.D., Cauch-Dudek K. Combined analysis of randomized controlled trials of ursodeoxycholic acid in primary biliary cirrhosis. Gastroenterology. 1997;113:884–890. doi: 10.1016/s0016-5085(97)70183-5. [DOI] [PubMed] [Google Scholar]
- 121.Lindor K.D., Therneau T.M., Jorgensen R.A. Effects of ursodeoxycholic acid on survival in patients with primary biliary cirrhosis. Gastroenterology. 1996;110:1515–1518. doi: 10.1053/gast.1996.v110.pm8613058. [DOI] [PubMed] [Google Scholar]
- 122.Corpechot C., Carrat F., Bahr A. The effect of ursodeoxycholic acid therapy on the natural course of primary biliary cirrhosis. Gastroenterology. 2005;128:297–303. doi: 10.1053/j.gastro.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 123.ter Borg P.C., Schalm S.W., Hansen B.E. Prognosis of ursodeoxycholic acid-treated patients with primary biliary cirrhosis. Results of a 10-yr cohort study involving 297 patients. Am J Gastroenterol. 2006;101:2044–2050. doi: 10.1111/j.1572-0241.2006.00699.x. [DOI] [PubMed] [Google Scholar]
- 124.Corpechot C., Abenavoli L., Rabahi N. Biochemical response to ursodeoxycholic acid and long-term prognosis in primary biliary cirrhosis. Hepatology. 2008;48:871–877. doi: 10.1002/hep.22428. [DOI] [PubMed] [Google Scholar]
- 125.Lindor K.D., Kowdley K.V., Luketic V.A. High-dose ursodeoxycholic acid for the treatment of primary sclerosing cholangitis. Hepatology. 2009;50:808–814. doi: 10.1002/hep.23082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.European Association for the Study of the Liver EASL Clinical practice guidelines: management of cholestatic liver diseases. J Hepatol. 2009;51:237–267. doi: 10.1016/j.jhep.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 127.Pellicciari R., Fiorucci S., Camaioni E. 6α-ethyl-chenodeoxycholic acid (6-ECDCA), a potent and selective FXR agonist endowed with anticholestatic activity. J Med Chem. 2002;45:3569–3572. doi: 10.1021/jm025529g. [DOI] [PubMed] [Google Scholar]
- 128.Sinal C.J., Tohkin M., Miyata M. Targeted disruption of the nuclear receptor FXR/BAR impairs bile acid and lipid homeostasis. Cell. 2000;102:731–744. doi: 10.1016/s0092-8674(00)00062-3. [DOI] [PubMed] [Google Scholar]
- 129.Hirschfield G.M., Mason A., Luketic V. Efficacy of obeticholic acid in patients with primary biliary cirrhosis and inadequate response to ursodeoxycholic acid. Gastroenterology. 2015;148:751–761.e8. doi: 10.1053/j.gastro.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 130.Nevens F., Andreone P., Mazzella G. O168 The first primary biliary cirrhosis (PBC) phase 3 trial in two decades—an international study of the FXR agonist obeticholic acid in PBC patients. J Hepatol. 2014;60(Suppl):S525–S526. [Google Scholar]
- 131.Cohen B.I., Hofmann A.F., Mosbach E.H. Differing effects of nor-ursodeoxycholic or ursodeoxycholic acid on hepatic histology and bile acid metabolism in the rabbit. Gastroenterology. 1986;91:189–197. doi: 10.1016/0016-5085(86)90457-9. [DOI] [PubMed] [Google Scholar]
- 132.Hohenester S., Wenniger L.M., Paulusma C.C. A biliary HCO3- umbrella constitutes a protective mechanism against bile acid-induced injury in human cholangiocytes. Hepatology. 2012;55:173–183. doi: 10.1002/hep.24691. [DOI] [PubMed] [Google Scholar]
- 133.Fickert P., Pollheimer M.J., Silbert D. Differential effects of norUDCA and UDCA in obstructive cholestasis in mice. J Hepatol. 2013;58:1201–1208. doi: 10.1016/j.jhep.2013.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Moritoki Y., Lian Z.X., Lindor K. B-cell depletion with anti-CD20 ameliorates autoimmune cholangitis but exacerbates colitis in transforming growth factor-beta receptor II dominant negative mice. Hepatology. 2009;50:1893–1903. doi: 10.1002/hep.23238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Tsuda M., Moritoki Y., Lian Z.X. Biochemical and immunologic effects of rituximab in patients with primary biliary cirrhosis and an incomplete response to ursodeoxycholic acid. Hepatology. 2012;55:512–521. doi: 10.1002/hep.24748. [DOI] [PubMed] [Google Scholar]
- 136.Lleo A., Gershwin M.E., Mantovani A. Towards common denominators in primary biliary cirrhosis: the role of IL-12. J Hepatol. 2012;56:731–733. doi: 10.1016/j.jhep.2011.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Hirschfield G.M., Liu X., Xu C. Primary biliary cirrhosis associated with HLA, IL12A, and IL12RB2 variants. N Engl J Med. 2009;360:2544–2555. doi: 10.1056/NEJMoa0810440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Eaton J.E., Talwalkar J.A., Lazaridis K.N. Pathogenesis of primary sclerosing cholangitis and advances in diagnosis and management. Gastroenterology. 2013;145:521–536. doi: 10.1053/j.gastro.2013.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Liaskou E., Karikoski M., Reynolds G.M. Regulation of mucosal addressin cell adhesion molecule 1 expression in human and mice by vascular adhesion protein 1 amine oxidase activity. Hepatology. 2011;53:661–672. doi: 10.1002/hep.24085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Moon H.J., Finney J., Ronnebaum T. Human lysyl oxidase-like 2. Bioorg Chem. 2014;57:231–241. doi: 10.1016/j.bioorg.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.O’Hara S.P., Tabibian J.H., Splinter P.L. The dynamic biliary epithelia: molecules, pathways, and disease. J Hepatol. 2013;58:575–582. doi: 10.1016/j.jhep.2012.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]