Abstract
Preterm infants’ hospital discharge is often delayed due to their inability to feed by mouth safely and competently. No evidence-based supported guidelines are currently available for health professionals caring for these infants. Available interventions advocating benefits are not readily acknowledged for lack of rigorous documentation inasmuch as any improvements may ensue from infants’ normal maturation. Through research, a growing understanding of the development of nutritive sucking skills has emerged shedding light on how and why infants may encounter oral feeding difficulties due to the immaturity of specific physiologic functions. Unfortunately, this knowledge has yet to be translated to the clinical practice to improve the diagnoses of oral feeding problems through the development of relevant assessment tools and to enhance infants’ oral feeding skills through the development of efficacious preventive and therapeutic interventions. This review focuses on the maturation of the various physiologic functions implicated in the transport of a bolus from the oral cavity to the stomach. Although infant’s readiness to oral feeding is deemed attained when suck, swallow, and respiration are coordinated, we do not have a clear definition of what coordination implies. We have learned that each of these functions encompasses a number of elements that mature at different times and rates. Consequently, it would appear that the proper functioning of sucking, the swallow processing, and respiration need to occur at two levels: first, the elements within each function must reach an appropriate functional maturation that can work in synchrony with each other to generate an appropriate suck, swallow process, and respiration; and second the elements of all these distinct functions, in turn, must be able to do the same at an integrative level to ensure the safe and efficient transport of a bolus from the mouth to the stomach.
Keywords: oral feeding prematurity, preterm, term, feeding skills
The ability of infants to breast- or bottle-feed safely and competently is not routinely a concern for the majority of mothers. Unfortunately, 25 to 45% of normally developing infants/children and up to 80% of developmentally delayed infants/children, e.g., those born prematurely, do experience oral feeding difficulties [1]. Safe and competent oral feeding requires the proper integration of physical and neurophysiologic functions that may not necessarily be mature at the time oral feeding is introduced [2]. For preterm infants, such issues are generally identified during their hospitalization in neonatal intensive care units (NICUs) as attainment of independent oral feeding is a major criterion for hospital discharge [3]. For term and late preterm infants, this may not be recognized until they are home due to their short hospital stay or small initial volumes of feeding. At present, the determination of whether poor oral feeding may be due to immature oral feeding skills or other medical concerns has been challenged by the lack of appropriate tools for the objective assessment(s) of such skills. Additionally, the limited understanding of the causes leading to inadequate oral feeding performance has hampered the development of evidence-based efficacious interventions to assist these infants [4].
Infant oral feeding research is a relatively young field. Recognition of the health impact resulting from oral feed difficulties essentially arose over the last two decades following the increased survival of preterm infants, many of whom encounter difficulty transitioning from tube to oral feeding and experience delayed hospital discharge and reunification with their mother [5;6]. With the growing population of preterm infants, researchers have been offered the unique opportunity to study the development of oral feeding skills and gain a better understanding of the causes of the varied problems they encounter as they are weaned from tube to oral feeding. For the majority of term infants, oral feeding is not an issue; their ability to safely and competently feed by mouth is often accepted as a given. Unfortunately, as mentioned earlier, a substantial number of these infants do encounter similar problems [1]. Sadly, these infants are under-diagnosed as they are not patients per se, unless they are brought to the attention of healthcare providers. Therefore, if we understand the continued development of all the complex neurophysiologic and motor functions implicated in oral feeding as infants mature, we will allow for more accurate diagnoses while facilitating the development of optimal tools and interventions for their proper growth and development.
It is recognized that safe and efficient nutritive sucking does not relate solely to sucking, but rather to the synchronous activities of sucking, swallowing, breathing, and esophageal function. Together, all these functions within what may be called the ‘nutritive sucking pathway” are responsible for the swift and safe transport of a milk bolus from the oral cavity to the stomach [4]. Difficulty in oral feeding is not so much an illness as the result of infants’ continuously maturing physiologic functions [2;7-9]. With so “many moving parts in flux”, it is difficult at any one time to pinpoint the specific cause(s) preventing an infant’s safe and efficient oral feeding experience. To better understand the complex interactions of all the above constituents, a nutritive sucking pathway is proposed that encompasses two closely intertwined conduits with suck-pharyngeal swallow -respiration pertaining to safety and suck- pharyngeal swallow-esophageal activity pertaining to efficiency. The differentiation made between ‘swallow’ and ‘pharyngeal swallow’ in this context emphasizes the importance of the different phases of the swallowing process discussed below that are not routinely taken into consideration in clinical practice.
Development of the sucking function
Irrespective of whether sucking is nutritive or non-nutritive, i.e., involving milk transport or not, mature sucking comprises 2 components, suction and expression [10;11]. Suction corresponds to the negative intraoral pressure generated with closure of the nasal passages by the soft palate, lips tightening around breast or bottle nipple, and the lowering of the lower jaw [12]. With no air penetration into an increased volume of the oral cavity, milk is drawn into the mouth, an action similar to that of drinking from a straw. Expression corresponds to the compression or stripping of the breast or bottle nipple by the tongue against the hard palate to eject milk into the mouth, an action similar to milking a cow by hand [13].
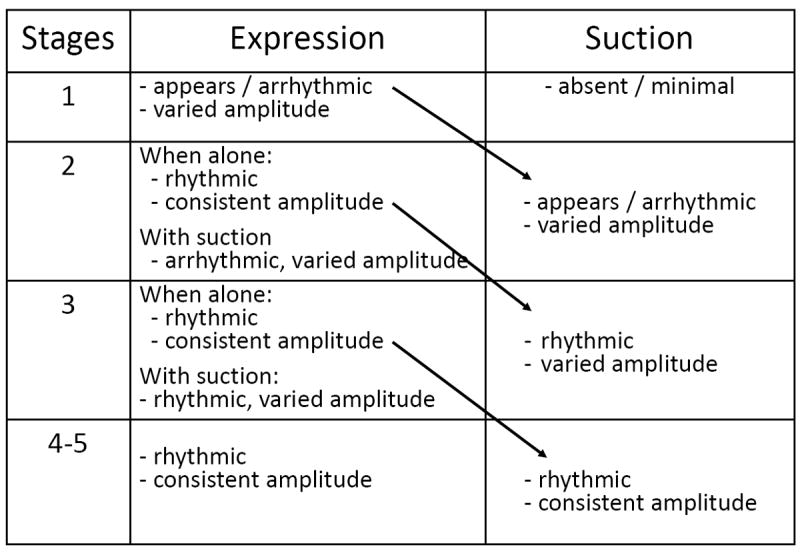
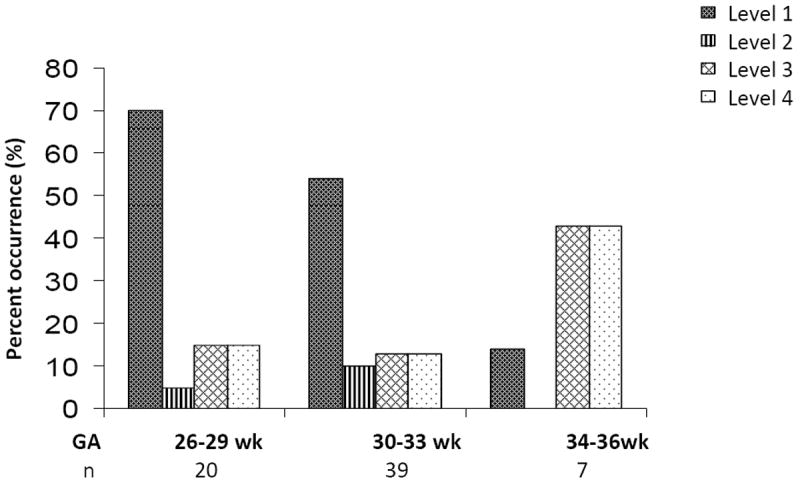
With the unique opportunity to monitor over time the maturational stages of nutritive sucking patterns in preterm infants and using the nutritive sucking pattern of term infants as the ‘gold standard’, i.e., representative of a mature pattern, we developed a descriptive scale of the maturation of the suction and expression component of nutritive sucking (Fig.1) [14]. In brief, 5 levels of maturity were defined as infants matured; namely, in a sequential manner, the appearance of the expression component followed by that of suction, their respective rhythmicity followed by the mature pattern of alternating rhythmic suction/expression characteristic of term infants. Maturation of the suction component is delayed in relation to that of expression (Fig. 2). Recently, we developed an objective oral feeding skills (OFS) scale that allows differentiation between infants’ oral feeding skills and endurance [15]. As this scale does not require any special equipment, it can be readily used by any caregiver. Four levels are defined based on an infant’s rate of milk transfer over an entire feeding (ml/min) and their ‘proficiency’ defined as the percent volume taken during the first 5 minutes of a feeding/total volume to be taken. Rate of transfer is used as an indirect marker of fatigue or endurance as it reflects an infant’s overall performance as fatigue increases. Proficiency, on the other hand, is used as a direct marker for the ‘true’ skills of infants when fatigue is deemed minimal (Fig. 3). It is of interest to note that within infants of similar gestational age (GA), a broad variation in OFS skill levels can be observed (Fig. 4).
Figure 1.

A five-stage descriptive scale of the development of VLBW infants’ nutritive sucking defined by the sequential presence/absence of the suction and expression components of sucking and their respective rhythmicity. At the earlier stages (1 to 3), infants readily shift from using either pattern (A) or (B).
Figure 2.
Temporal appearance of characteristics of the Expression and Suction components of nutritive sucking as per stages described in Figure 1
Figure 3.
Percent distribution of OFS levels by GA strata at introduction of oral feeding (reproduced by permission Karger Publishers)
Figure 4.
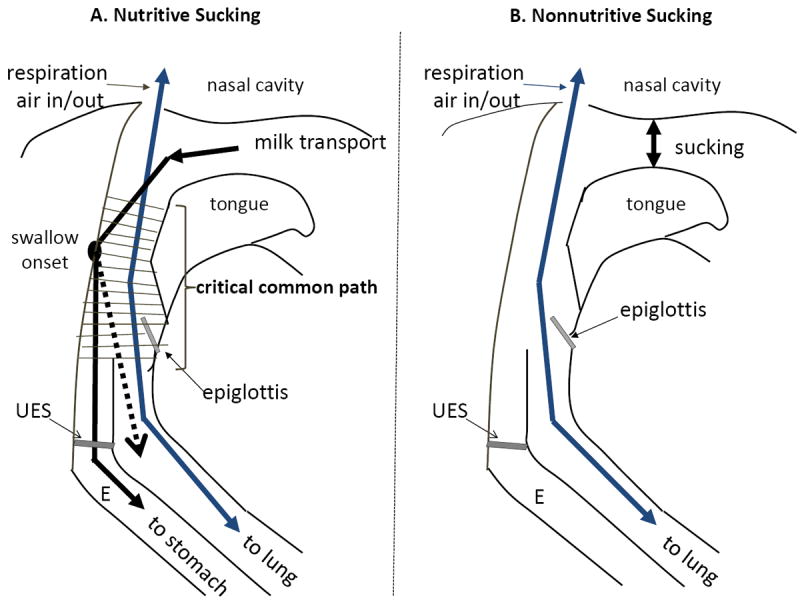
Schematic of sucking, pharyngeal swallow and respiratory airflow during nutritive (A) and nonnutritive (B) sucking
Nutritive sucking implies the ingestion of liquid and in a mature term infant occurs at a frequency of 1 cycle or suck per second. Nonnutritive sucking with no liquid ingestion, e.g., sucking on a pacifier, occurs at 2 cycles or sucks per second [11]. Such differing sucking rates likely result from the fact that during nutritive sucking, as the passage of the milk bolus and air follow a common pharyngeal path, the proper synchrony of suck-swallow and swallow-respiration is critical for safety in order to prevent concurrent milk entry into the trachea and esophagus [7](Fig.5A). As swallows are minimally involved during nonnutritive sucking, the pharyngeal phase of swallowing is not activated allowing sucking and respiration to essentially function independently from one another at a more rapid pace (Fig.5B).
Figure 5.

Tracings of nonnutritive and nutritive sucking monitored 3 min apart during same feeding sessions of an infant born at 331/7 weeks GA, introduced to oral feeding at 342/7 weeks PMA, and attaining 8 oral feedings per day at 361/7 weeks PMA
Maturity of nonnutritive sucking has been and still is used as a marker of readiness to oral feed [12;16]. This remain debatable as we have shown that mature nonnutritive sucking appears earlier than mature nutritive sucking [17] (Fig. 6). Consequently, one may advance that nonnutritive sucking is a good marker for sucking per se, but cannot be predictive of the coordination between suck, pharyngeal swallow, breathe, and esophageal function.
Our work has shown that mature nutritive sucking defined by the rhythmic alternation of suction/expression is not necessary for bottle feeding. Indeed, infants using expression only can complete a bottle feeding safely, albeit not as efficiently as counterparts using a rhythmic alternation of suction/expression [13]. However, it is uncertain that an infant using only the expression component can successfully breastfeed inasmuch as the maternal nipple is not as firm as a bottle nipple. It has been speculated that presence of the suction component would be necessary for infants to latch onto and retain the maternal nipple during breastfeeding. This is indirectly supported by the advantage offered by the use of the nipple shield that has a firm nipple when breastfeeding is introduced.
Development of the swallowing process
The normal swallowing process is commonly divided into an oral phase, beginning pharyngeal phase, pharyngeal phase, beginning esophageal phase, and esophageal phase [18]. Based on knowledge acquired from the development of oral feeding skills in preterm infants, we have learned that the components implicated within each of these phases may mature at different times and/or rates as described below. If we consider that nutritive sucking occurs at one suck per second, it is expected that there will be a bolus every second that will need to be sequentially cleared from the oral cavity, pharynx, and esophagus before the next bolus arrives. To emphasize the importance of how a delayed action at any or more of these steps may lead to oral feeding disruption, sites at which bolus transport may be challenged due to immature neurophysiologic and motor functions are: 1. the oral phase implicated in bolus formation [7;19;20]; 2. The beginning pharyngeal phase essential for the onset of the swallow reflex [21]; 3. the pharyngeal phase implicated in the swift and safe aboral peristaltic transport of the bolus towards the esophagus [22-24]; 4. the beginning of the esophageal phase essential for timely entry of the bolus through the upper esophageal sphincter (UES) into the esophageal body[25]; 5. the esophageal phase implicated in the swift aboral transport of the bolus towards the stomach [26-32]; and 6. the entry of the bolus through the lower esophageal sphincter (LES) into the stomach [30;33;34]. Additional discussion of normal and abnormal swallowing function is discussed by Dodrill in a subsequent chapter [35].
Briefly, with poor bolus formation, liquid draining into the pharynx may not trigger the swallow reflex. This, in turn, may lead to improper timing of the laryngeal elevation and epiglottic closure. Together with the potential of residual liquid lingering around the valleculae and pyriform sinuses, risks of penetration and/or aspiration into the larynx are increased if respiration is maintained [7]. UES maturation in preterm infants is characterized by an age-related increase in peak pharyngeal pressure just above the UES prior to a decrease in the time needed by the UES to fully relax to a nadir pressure. This suggests that in more premature infants, the UES is not fully relaxed when the propulsive forces of the bolus in the pharynx are their peak [25]. Esophageal motility comprises peristaltic and non-peristaltic waveforms. With maturation, an increase occurrence in propagating/aboral peristalsis is observed [36]
Development of the respiratory function
The proper integration of the respiratory function is germane to safe oral feeding. In general, as infants mature, so will their respiratory function. Infants early on breathe at a rate of 40-60 breaths per minute or 1.5 to 1 breath per second. Taking into account that the immature pharyngeal swallow may last from 0.35 to 0.75 second [37], the time left for safe air exchange may be threatened. In addition, during feeding, minute ventilation is decreased, exhalation is prolonged, and inhalation is shortened [38-40]. All together, these events further underscore the importance of the swift passage of a bolus through the common pharyngeal pathway for the sake of safety and proper oxygen/carbon dioxide exchange.
Coordination of suck, pharyngeal swallow, respiratory, and esophageal functions
Although proper maturation of the above functions would enhance oral feeding performance, it is their coordinated activities that ultimately will lead to a safe and efficient feeding and ultimately define the term “readiness to oral feed”. In an earlier study, we speculated that the oral feeding difficulties encountered by preterm infants resulted from the different temporal development of the musculatures implicated in sucking, swallowing, and respiration and their coordinated activities [2]. Coordination between any of these motor functions, e.g., sucking-swallowing or swallowing-respiration, may result not only from the peripheral immaturity of the respective musculatures implicated in these functions, but also, just as importantly, from the incoordination between their respective neurophysiologic counterparts at the level of the central nervous system. At present, although little is known regarding the maturation of the neurological sites, it is well acknowledged that these motor functions being rhythmic in nature, e.g., nutritive and nonnutritive sucking averaging 1 and 2 sucks/sec, respectively, are controlled and regulated by central pattern generators (CPGs).
A. Development of the coordination of suck-pharyngeal swallow
In earlier studies, we examined the maturation of the interactions between suck-pharyngeal swallow and pharyngeal swallow-respiration. When introduced to bottle feeding, VLBW infants born between 26 and 29 weeks GA already demonstrated a steady 1:1 suck:pharyngeal swallow ratio similar to that of their term counterparts during their first 3 weeks of life, albeit the number suck-swallow per minute was significantly slower, i.e., 48±14:45±14 vs. 59±12:55±15, respectively (p<0.001; mean±SD). This observation supports the notion that the interaction between sucking and pharyngeal swallow were mature when oral feeding was introduced [7].
B. Development of the coordination of pharyngeal swallow-respiration
When pharyngeal swallow-respiration was monitored, these preterm infants preferentially swallowed during deglutition apnea and inhalation, two unsafe respiratory phases that increased risks of oxygen desaturation and penetration/aspiration into the lungs, respectively [7;41]. Term counterparts during their first two weeks of life demonstrated similar preference towards deglutition apnea only. However, by the third week on, they preferentially swallowed at safer respiratory phases, i.e., before the start of inhalation or exhalation at a time when risk of penetration/aspiration would be reduced as air in- and out-flow was minimal [7].
C. Development of the coordination of pharyngeal swallow-esophageal function
This area of research has not been as consistently studied in infants as the interactions of pharyngeal swallow and respiration. Studies conducted on esophageal maturation in infants have primarily monitored esophageal functions, i.e., UES, esophageal motility, LES activities when infants were tube fed, immediately following a feeding, when small volumes were delivered in the pharynx to initiate a pharyngeal swallow, and/or at different levels of the esophagus using micromanometric water perfusion techniques [20;27;36]. Although swallow and esophageal activities may be well described, by the nature of the methodologies used, these studies do not take into account the impact that sucking and respiration would normally play. To the author’s knowledge, no study has yet been conducted on pharyngeal swallowing, respiration, and esophageal function during oral feeding.
Summary/Conclusion
This article offers a summary of our current understanding of the development of infant oral feeding skills. The current care provided to infants with oral feeding difficulties, be they born prematurely or at term, lack evidence-based support. Any observed improvement cannot rule out the prime effect of maturation alone. Gaining a better understanding of the development of infants’ oral feeding skills will not only assist in identifying the potential causes at play, but also facilitate the development of evidence-based tools and interventions that can enhance the development of these skills.
From the research presented, ‘readiness to oral feed’ may be better defined by the term “coordination of sucking, swallow processing, and respiration” than “coordination of suck, swallow, and respiration”, as caregivers will be reminded of the negative impact that immature esophageal function can cause. Indeed, the swallowing process does not only encompass the pharyngeal phase of swallowing, but also its oral and esophageal phases. As we now know that many components within each of these levels mature at different times and rates, unsafe and inefficient oral feeding may be caused at any or all levels of the nutritive sucking pathway. Such occurrences may be a reason why infants of similar GA and at similar PMA demonstrate such wide variance in the maturation levels of their skills.
With a better understanding of the maturational process of these physiologic functions, management of infant oral feeding issues can improve. Indeed, our expectations of what infants can achieve would be tailored around the functional maturity levels of our individual patients rather than be based on their GA and/or PMA.
Key messages.
Management of infant oral feeding lacks evidence-based support
-
Understanding the development of infant nutritive sucking skills, i.e., sucking, swallow processing, and respiration will:
-
■
improve the diagnoses of oral feeding difficulties
-
■
assist in the development of evidence-based assessment tools
-
■
assist in the development of preventive and therapeutic interventions to enhance infant skills, safety, and efficiency during oral feeding
-
■
assist in developing evidence-based supported guidelines
-
■
Acknowledgments
This work was supported by funding from the National Institutes of Health (R01 HD 28140; HD 044469; MO 1RR000188). The author had responsibility for all parts of the manuscript. The contents of this publication are solely the responsibility of the author and do not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- CPG
Central pattern generator
- GA
Gestational age (weeks)
- LES
Lower esophageal sphincter
- NICU
Neonatal intensive care unit
- PMA
Postmenstrual age (weeks)
- SLESR
Swallow-induced lower esophageal sphincter relaxation
- TLESR
Transient lower esophageal sphincter relaxation
- UES
Upper esophageal sphincter
- VLBW
Very low birth weight
Footnotes
Financial Conflict of Interest
The author does not have any financial conflict of interest
Reference List
- 1.Byant-Waugh R, Markham L, Kreipe RE, Walsh BT. Feeding and eating disorders in childhood. Int J Eat Disord. 2010;43:98–111. doi: 10.1002/eat.20795. [DOI] [PubMed] [Google Scholar]
- 2.Amaizu N, Shulman R, Schanler R, Lau C. Maturation of oral feeding skills in preterm infants. Acta Paediatr. 2008;97:61–67. doi: 10.1111/j.1651-2227.2007.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.AAP Policy Statement: Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119–1126. doi: 10.1542/peds.2008-2174. [DOI] [PubMed] [Google Scholar]
- 4.Lau C. Interventions to improve oral feeding performance of preterm infants. Perspectives on Swallowing and Swallowing Disorders (Dysphagia) 2014;23:23–45. [Google Scholar]
- 5.Lau C, Hurst N. Oral feeding in infants. Curr Probl Pediatr. 1999;29:105–124. doi: 10.1016/s0045-9380(99)80052-8. [DOI] [PubMed] [Google Scholar]
- 6.Eichenwald EC, Blackwell M, Lloyd JS, Tran T, Wilker RE, Richardson DK. Inter-neonatal intensive care unit variation in discharge timing: influence of apnea and feeding management. Pediatrics. 2001;108:928–933. doi: 10.1542/peds.108.4.928. [DOI] [PubMed] [Google Scholar]
- 7.Lau C, Smith EO, Schanler RJ. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr. 2003;92:721–727. [PubMed] [Google Scholar]
- 8.Kelly BN, Huckabee ML, Jones RD, Frampton CM. The early impact of feeding on infant breathing-swallowing coordination. Respir Physiol Neurobiol. 2007;156:147–153. doi: 10.1016/j.resp.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 9.Kelly BN, Huckabee ML, Jones RD, Frampton CM. The first year of human life: coordinating respiration and nutritive swallowing. Dysphagia. 2007;22:37–43. doi: 10.1007/s00455-006-9038-3. [DOI] [PubMed] [Google Scholar]
- 10.Sameroff AJ. The components of sucking in the human newborn. J Exp Child Psychol. 1968;6:607–623. doi: 10.1016/0022-0965(68)90106-9. [DOI] [PubMed] [Google Scholar]
- 11.Wolff PH. The serial organization of sucking in the young infant. Pediatrics. 1968;42:943–956. [PubMed] [Google Scholar]
- 12.Wolf LS, Glass RP. Feeding and swallowing disorders in infancy: Assessment and management. Tucson: Therapy Skills Builders; 1992. [Google Scholar]
- 13.Lau C, Sheena HR, Shulman RJ, Schanler RJ. Oral feeding in low birth weight infants. J Pediatr. 1997;130:561–569. doi: 10.1016/s0022-3476(97)70240-3. [DOI] [PubMed] [Google Scholar]
- 14.Lau C, Alagugurusamy R, Schanler RJ, Smith EO, Shulman RJ. Characterization of the developmental stages of sucking in preterm infants during bottle feeding. Acta Paediatr. 2000;89:846–852. [PubMed] [Google Scholar]
- 15.Lau C, Smith EO. A Novel Approach to Assess Oral Feeding Skills of Preterm Infants. Neonatology. 2011;100:64–70. doi: 10.1159/000321987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kish MZ. Improving preterm infant outcomes: implementing an evidence-based oral feeding advancement protocol in the neonatal intensive care unit. Adv Neonatal Care. 2014;14:346–353. doi: 10.1097/ANC.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 17.Lau C, Kusnierczyk I. Quantitative evaluation of infant’s nonnutritive and nutritive sucking. Dysphagia. 2001;16:58–67. doi: 10.1007/s004550000043. [DOI] [PubMed] [Google Scholar]
- 18.Arvedson JC, Lefton-Greif MA. A profession manual with caregiver guidelines. San Antonio: Communication Skill Builders; 1998. Pediatric videofluoroscopic swallow studies. [Google Scholar]
- 19.Buchholz DW, Bosma JF, Donner MW. Adaptation, compensation, and decompensation of the pharyngeal swallow. Gastrointest Radiol. 1985;10:235–239. doi: 10.1007/BF01893106. [DOI] [PubMed] [Google Scholar]
- 20.Omari T, Snel A, Barnett C, Davidson G, Haslam R, Dent J. Measurement of upper esophageal sphincter tone and relaxation during swallowing in premature infants. Am J Physiol. 1999;277:G862–G866. doi: 10.1152/ajpgi.1999.277.4.G862. [DOI] [PubMed] [Google Scholar]
- 21.Selley WG, Ellis RE, Flack FC, Brooks WA. Coordination of sucking, swallowing and breathing in the newborn: its relationship to infant feeding and normal development. Br J Disord Commun. 1990;25:311–327. doi: 10.3109/13682829009011980. [DOI] [PubMed] [Google Scholar]
- 22.Arvedson JC, Lefton-Greif MA. A professional manual with caregiver guidelines. San Antonio, TX: Communication Skill Builders; 1998. Pediatric videofluoroscopic swallow studies. [Google Scholar]
- 23.Arvedson J, Rogers B, Buck G, Smart P, Msall M. Silent aspiration prominent in children with dysphagia. Int J Pediatr Otorhinolaryngol. 1994;28:173–181. doi: 10.1016/0165-5876(94)90009-4. [DOI] [PubMed] [Google Scholar]
- 24.Noll L, Rommel N, Davidson GP, Omari TI. Pharyngeal flow interval: a novel impedance-based parameter correlating with aspiration. Neurogastroenterol Motil. 2011;23:551–e206. doi: 10.1111/j.1365-2982.2010.01634.x. [DOI] [PubMed] [Google Scholar]
- 25.Rommel N, van WM, Boets B, Hebbard G, Haslam R, Davidson G, Omari T. Development of pharyngoesophageal physiology during swallowing in the preterm infant. Neurogastroenterol Motil. 2011;23:e401–e408. doi: 10.1111/j.1365-2982.2011.01763.x. [DOI] [PubMed] [Google Scholar]
- 26.Jadcherla SR. Upstream effect of esophageal distention: effect on airway. Curr Gastroenterol Rep. 2006;8:190–194. doi: 10.1007/s11894-006-0074-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rasch S, Sangild PT, Gregersen H, Schmidt M, Omari T, Lau C. The preterm piglet - a model in the study of oesophageal development in preterm neonates. Acta Paediatr. 2010;99:201–208. doi: 10.1111/j.1651-2227.2009.01564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singendonk MM, Kritas S, Cock C, Ferris LF, McCall L, Rommel N, van Wijk MP, Benninga MA, Moore D, Omari TI. Pressure-Flow Characteristics of Normal and Disordered Esophageal Motor Patterns. J Pediatr. 2015 doi: 10.1016/j.jpeds.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 29.Singendonk MM, Rommel N, Omari TI, Benninga MA, van Wijk MP. Upper gastrointestinal motility: prenatal development and problems in infancy. Nat Rev Gastroenterol Hepatol. 2014 doi: 10.1038/nrgastro.2014.75. [DOI] [PubMed] [Google Scholar]
- 30.Omari T. Lower esophageal sphincter function in the neonate. NeoReviews. 2006;7:e13–e18. [Google Scholar]
- 31.Loots C, van Herwaarden MY, Benninga MA, VanderZee DC, van Wijk MP, Omari TI. Gastroesophageal reflux, esophageal function, gastric emptying, and the relationship to dysphagia before and after antireflux surgery in children. J Pediatr. 2013;162:566–573. doi: 10.1016/j.jpeds.2012.08.045. [DOI] [PubMed] [Google Scholar]
- 32.Loots C, van WM, van der Pol R, Smits M, Benninga M, Omari T. Evaluation of esophageal motility using multichannel intraluminal impedance in healthy children and children with gastroesophageal reflux. J Pediatr Gastroenterol Nutr. 2011;52:784–785. doi: 10.1097/MPG.0b013e318214c6ef. comments. [DOI] [PubMed] [Google Scholar]
- 33.Pena EM, Parks VN, Peng J, Fernandez SA, Di LC, Shaker R, Jadcherla SR. Lower esophageal sphincter relaxation reflex kinetics: effects of peristaltic reflexes and maturation in human premature neonates. Am J Physiol Gastrointest Liver Physiol. 2010;299:G1386–G1395. doi: 10.1152/ajpgi.00289.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Wijk MP, Benninga MA, Davidson GP, Haslam R, Omari TI. Small volumes of feed can trigger transient lower esophageal sphincter relaxation and gastroesophageal reflux in the right lateral position in infants. J Pediatr. 2010;156:744–8. 748. doi: 10.1016/j.jpeds.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 35.Dodrill P. Normal and abnormal swallowing fucntion: evaluation and treatment. 2015 [Google Scholar]
- 36.Jadcherla SR. Esophageal motility in the human neonate. NeoReviews. 2006;2:e7–e11. [Google Scholar]
- 37.Koenig JS, Davies AM, Thach BT. Coordination of breathing, sucking, and swallowing during bottle feedings in human infants. J Appl Physiol. 1990;69:1623–1629. doi: 10.1152/jappl.1990.69.5.1623. [DOI] [PubMed] [Google Scholar]
- 38.Rosen CL, Glaze DG, Frost JD., Jr Hypoxemia associated with feeding in the preterm infant and full-term neonate. Am J Dis Child. 1984;138:623–628. doi: 10.1001/archpedi.1984.02140450005002. [DOI] [PubMed] [Google Scholar]
- 39.Mathew OP, Clark ML, Pronske ML, Luna-Solarzano HG, Peterson MD. Breathing pattern and ventilation during oral feeding in term newborn infants. J Pediatr. 1985;106:810–813. doi: 10.1016/s0022-3476(85)80363-2. [DOI] [PubMed] [Google Scholar]
- 40.Miller MJ, DiFiore JM. A comparison of swallowing during apnea and periodic breathing in premature infants. Pediatr Res. 1995;37:796–799. doi: 10.1203/00006450-199506000-00020. [DOI] [PubMed] [Google Scholar]
- 41.Fucile S, McFarland DH, Gisel EG, Lau C. Oral and nonoral sensorimotor interventions facilitate suck-swallow-respiration functions and their coordination in preterm infants. Early Hum Dev. 2012;88:345–350. doi: 10.1016/j.earlhumdev.2011.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


