Abstract
Background
Preventing preterm birth and subsequent adverse neonatal sequelae is among the greatest clinical challenges of our time. Recent studies suggest a role for Candida spp. in preterm birth and fetal injury, as a result of their colonization of either the vagina and/or the amniotic cavity. We hypothesised that intraamniotic C. albicans would cause a vigorous, acute fetal inflammatory response.
Methods
Sheep carrying singleton pregnancies received single intraamniotic (IA) injections of either saline (control) or 107 CFU C. albicans 1 or 2 d prior to surgical delivery and euthanasia at 124 ± 2 d gestation.
Results
Colonization of the amniotic cavity by C. albicans resulted in a modest inflammatory response at 1 d and florid inflammation at 2 d, characterised by fetal thrombocytopenia, lymphopenia and significant increases of inflammatory cytokines/chemokines in the fetal membranes skin, lung and the amniotic fluid.
Conclusion
Acute colonization of the amniotic cavity by C. albicans causes severe intrauterine inflammation and fetal injury. C. albicans is a potent fetal pathogen which can contribute to adverse pregnancy outcomes.
Introduction
Preterm birth remains a leading cause of neonatal mortality and morbidity worldwide. Although the causes of preterm birth are multi-factorial, infection of the amniotic cavity and subsequent intrauterine inflammation are both strongly associated with preterm delivery and adverse neonatal outcomes (including respiratory, gastrointestinal and neurological injuries), most notably in deliveries occurring at ≤ 32 weeks completed gestation 1–3. Culture and molecular-based analyses have identified bacterial genera including Ureaplasma, Fusobacterium, Streptococcus, Bacteroides and Gardnerella spp. as the microorganisms most commonly isolated from preterm deliveries 1,4,5. Recent studies suggest that many of the intrauterine infections associated with preterm labour are polymicrobial in nature 5,6.
Historically, the role of Candida spp. in preterm birth and neonatal injury has been somewhat unclear. However, recent molecular data suggest that Candida albicans may colonise the amniotic cavity more frequently than initially suggested by culture-based analyses, and cases of congenital candidiasis have been reported in the literature 7–12. Rode and colleagues have suggested a possible association between serial amniocenteses and candida chorioamnionitis 13. More recently, Bean et al. published the resolution of two cases of intraamniotic Candida albicans infection with maternal and intraamniotic fluconazole. Key conclusions of this case report were that intraamniotic Candida albicans infection has devastating implications for the fetus and that prompt diagnosis and treatment of infection is essential for pregnancy wellbeing 14.
Candida spp., (most commonly C. albicans) are believed to asymptomatically colonise the vagina of 20% of healthy women (more frequently during pregnancy), and invasive candidiasis can be a primary cause of death and neurological injury in extremely low birth-weight infants (<1000 g) 5,15–17. Although a causal association for bacterial infection in early preterm labour is well established, the role of Candida spp. in uterine infection and preterm delivery is more controversial 5,16. A large multi-centre study of pregnancy outcomes and Candida spp. colonization in 13,914 women concluded that colonization with Candida spp. was not associated with low birth weight or preterm delivery 18. In direct contrast, a retrospective study of 38,151 infants, identified a 34–64% reduction in preterm birth in a subset (8.1%) born to mothers that received Clotrimazole (anti-Candida spp.) treatment during pregnancy 19. In addition, more recent smaller intervention studies reported either a significant reduction or a trend to reduction in preterm birth in groups receiving treatment for asymptomatic vaginal candidiasis 16,20. Of particular interest is research suggesting an apparent association between indwelling contraceptives and cervical cerclage with Candida spp. infection of the amniotic cavity 5.
We have previously utilised pregnant sheep to investigate the effects of E.coli lipopolysaccharides (LPS)21, antenatal corticosteroids 22, interleukin (IL)-1 23 and live Ureaplasma spp. 24 on the fetal lung 25, gut26 and skin27 and modulation of the fetal immune system 28. In light of emerging clinical data, animal studies are now needed to clarify the impact of acute intraamniotic C. albicans infection. To that end, we tested the pathogenicity of acute intrauterine C. albicans infection in a sheep model of human pregnancy. We hypothesised that intraamniotic C. albicans would cause a vigorous, acute fetal inflammatory response.
Materials and Methods
Animals
All procedures involving animals were performed at The University of Western Australia (Perth, Western Australia) following review and approval by the animal care and use committees of The University of Western Australia and Cincinnati Children’s Hospital (Cincinnati, OH.). Twenty nine date-mated Australian merino ewes with singleton pregnancies were randomised to receive either: i) a single ultrasound-guided intraamniotic injection of 2 mL saline (n=13); or ii) a single ultrasound-guided intraamniotic injection of 107 CFU C. albicans (Western Australian clinical isolate) in 2 mL saline with delivery after 1 d (1 d Candida group; n=8) or 2 d (2 d Candida group; n=8). Successful placement of intraamniotic injections were confirmed with electrolyte (Cl−) analysis of amniotic fluid using a Siemens Rapidlab 1265 Analyser (Siemens, Munich, Germany). No fetal losses occurred in the 1 d Candida, 2 d Candida or Saline control groups.
Fetuses were surgically delivered at 124 ± 2 d GA, and euthanized with intravenous pentobarbitone (100 mg/kg). Fetal lung fluid and tissues for protein and mRNA expression analyses were collected at autopsy and snap frozen in liquid nitrogen. To eliminate a potential sampling bias, fetal skin was selectively collected from the fetal groins. A minimum of five, randomly selected animals were analysed from each group. Fetal lung tissues for histological analysis were inflation fixed in 10% neutral buffered formalin for 24 h before paraffin embedding. Fetal skin tissues for histological analysis were cryopreserved in OCT.
Candida albicans culture for intraamniotic injection
A single Western Australian clinical isolate of C. albicans was cultured on Difco Sabaraud-Dextrose agar (Becton Dickinson & Co., Franklin Lakes, NJ.) at 37°C for 48 h and single colonies were inoculated into sterile 1 × phosphate buffered saline (Sigma-Aldrich, St. Loius, MO.). C. albicans colony morphology was confirmed by growth on Brilliance Candida Agar (Oxoid). Inoculums were quantified using a plate dilution series as per standard microbiological methods and recorded as CFU/mL. Quantified inoculums (107 CFU in 2 mL 1 × phosphate buffered saline) were stored at −80°C prior to use.
Nucleic acid extraction
To develop a standard curve for quantitation of C. albicans in fetal tissues, total RNA was extracted from 250 μL of C. albicans (the same Western Australian clinical isolate used in vivo in this study) using the Versant Sample Preparation kit 1.0 (Siemens, Munich, Germany) on a Kingfisher automated extraction platform (Thermo Scientific, Rockford, IL.) as per manufacturer’s instructions. Total RNA was extracted from liquid nitrogen-homogenised fetal tissues using TRIzol as previously reported21. Extracted RNA was treated with Turbo-DNase (Life Technologies, Carlsbad, CA.) to remove any residual DNA and subsequently quantified on a Qubit fluorometer (Life Technologies) using a broad-range RNA quantitation kit. RNA yields from fetal tissues were normalised to 100 ng/μL.
Candida albicans detection/quantitation
RNA extracted from fetal lung, skin, chorioamnion and spleen was screened using a real-time PCR assay targeting the RNase P RNA gene of C. albicans 29. RNA-based reactions were performed using an EXPRESS One-Step SuperScript qRT-PCR Kit (Life Technologies) with 0.5 μM each primer, 0.2 μM probe, 400 ng template RNA and water to a final volume of 20 μL. To enable quantitation of C. albicans within each sample, a standard curve of pure C. albicans (study isolate) RNA was included in each assay at a final concentration of 40, 4 and 0.4 ng per 20 uL reaction. Reaction cycling conditions were as follows: 15 min reverse transcription at 50°C and an initial denaturation at 95°C for 20 s, followed by 40 cycles of 95°C for 3 s and 60°C for 30 s. All reactions were performed in 96 well plates on a ViiA7 real-time PCR thermocycler (Life Technologies). The presence of viable C. albicans in amniotic fluid samples was determined using a Sabaraud-Dextrose agar plate dilution series as described above. Three single colonies from positive plates were subsequently inoculated onto Candida Brilliance agar (Oxoid, Basingstoke, UK) for confirmation of isolate identification.
Relative quantification of mRNA expression
Ovine-specific PCR primers and hydrolysis probes for IL-1β, IL-6, IL-8, TNF-α, MCP-1 and MCP-2 (Life Technologies) were used to perform quantitative PCR reactions on RNA from fetal lung, skin, and chorioamnion tissue. Reactions were performed using an EXPRESS One-Step SuperScript qRT-PCR Kit (Life Technologies) with 400 ng template RNA in a total volume of 20 μL. Reaction cycling conditions were as described above. Cq values were normalised to 18s rRNA and expressed as fold changes relative to pooled control values. Reaction efficiencies were within limits proposed in the MIQE guidelines 30.
Enzyme-linked immunosorbent assays
Quantification of IL-1β and IL-8 protein concentrations in AF was performed as previously described 31. AF samples were diluted 1:5 in assay buffer. Quantification of IL-6 protein concentration in ovine AF was performed using an identical protocol with the following modifications: Plate wells were coated overnight at 4°C with 5 μg/mL capture antibody (MCA1659; ABD Serotech, Kidlington, UK). Recombinant sheep IL-6 protein standards (Protein Express, Cincinnati, OH.) and AF samples, diluted 1:2 in assay buffer, were incubated overnight at 4°C. The detection antibody (AHP424; ABD Serotech) was diluted 1:750 in assay buffer. All samples and standards were assayed in duplicate. Cortisol measurements were performed with a Cortisol EIA kit (Oxford Biomedical Research, Rochester Hills, MI.) on 1:10 diluted fetal arterial cord blood plasma according to the manufacturer’s instructions.
Haematology
Complete blood counts (CBC) and differential analyses were performed with an automated Coulter counter customised for sheep blood.
Histology
5 μm-thick sections from formalin fixed lung (right upper lobe) tissues embedded in paraffin blocks or 10 μm-thick sections from cryopreserved skin tissues embedded in OCT were stained with haematoxylin and eosin. For lung tissues, five random fields were scored for inflammatory cell infiltration and airway consolidation as follows: 0: Normal; 1: Airway inflammatory cells, no consolidation; 2: Airway inflammatory cells + microconsolidation focii (1–2/5 Low Power Field); 3: Airway inflammatory cells + microconsolidation focii (≥3/5 Low Power Field); and 4: Extensive airway inflammatory cells and consolidation. Immunohistochemical staining of fetal lung for CD3 (A0452, Dako, Glostrup, Denmark, working concentration 1:100) and C. albicans (B65411R, Meridian Life Science, Inc. Memphis, TN., working concentration 1:50) was performed as previously published32. CD3 counts in fetal lung were obtained by counting positively stained cells in five randomly selected, non-overlapping fields at 20 × objective magnification.
Statistical analyses
All values are expressed as mean ± standard deviation (SD). All analyses were performed using IBM SPSS Statistics for Windows, software version 20.0 (IBM Corp. Armonk, NY.). Data were assessed for normality with Shapiro-Wilk tests and histograms. Parametric data were screened for outliers with Dixon’s Q-parameter and differences tested for significance with one-way ANOVA employing an α-value of 0.05. Multiple post-hoc comparisons were performed using Tukey’s test. Apparent differences in non-parametric data were tested for significance with Kruskal-Wallis one-way ANOVA employing an α-value of 0.05. Multiple post-hoc comparisons were performed using Rank Sum Tests with an α-value corrected for n multiple comparisons.
Results
Intrauterine infection with 107 CFU C. albicans resulted in florid intrauterine inflammation at 2 d post-infection. Limited histological changes in skin and lung, and relatively modest increases in cytokine/chemokine expression were detected in fetal tissues collected 1 d post-infection.
Detection of viable Candida albicans
Amniotic fluid from all 1 d and 2 d C. albicans exposed animals but none of the controls were positive for viable C. albicans growth (data not shown). qPCR analysis demonstrated increased C. albicans RNA in fetal lung (3.8 ± 3 ng), chorioamnion (78 ± 32 ng) and skin (50 ± 48 ng) taken from animals exposed to C. albicans for 2 d, relative to fetal lung (0.2 ng ± 0.1 ng), chorioamnion (14 ± 10 ng) and skin (6.0 ± 5.0 ng) exposed to C. albicans for 1 d (Figure 1a). The highest levels of C. albicans RNA were detected in chorioamnion tissue after a 2 d exposure (p < 0.010 vs. 2 d fetal lung). No C. albicans RNA was detected in the fetal spleen after either 1 d or 2 d C. albicans exposure or in any saline control animal.
Figure 1.
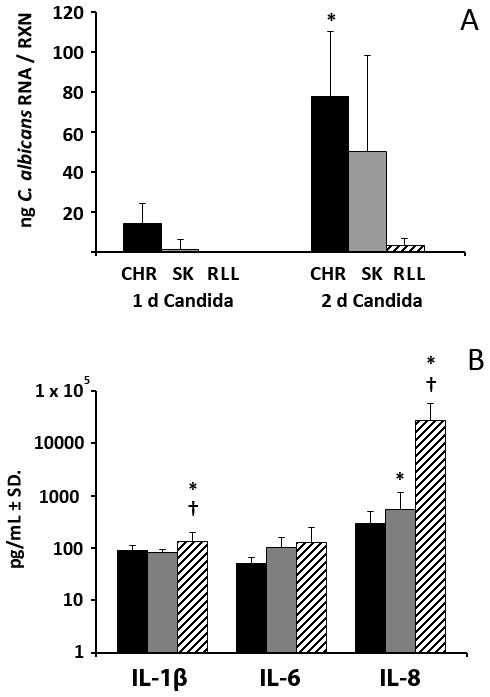
Panel A: C. albicans RNA in fetal tissues in 1 d and 2 d post-infection groups. (1 d Candida n=5; 2 d Candida n=5). CHR, chorioamnion; SK, skin; RLL, right lower lobe of lung. *, significant difference (p < 0.010) vs. RUL. Panel B: Concentration of IL-1β (Black bars, Control n=10; Grey bars, 1 d Candida n=8; Hatched bars, 2 d Candida n=8) and IL-8 (Black bars, Control n=6; Grey bars, 1 d Candida n=6; Hatched bars, 2 d Candida n=6), but not IL-6 (Black bars, Control n=6; Grey bars, 1 d Candida n=6; Hatched bars, 2 d Candida n=6;) is increased in AF in response to IAI with C. albicans. * p<0.05 vs. control; † p<0.05 vs. 1 d Candida albicans exposure.
Cytokine/chemokine protein concentration in fetal plasma, amniotic fluid and fetal lung fluid
No changes in IL-1β, IL-6 or IL-8 protein concentration were detected in fetal plasma from animals exposed to C. albicans for either 1 d or 2 d, relative to control (data not shown). Analysis of IL-1β, IL-6 and IL-8 protein concentrations in the AF demonstrated significant increases in the concentration of: i) IL-1β in 2 d C.albicans exposed animals relative to 1 d C. albicans exposed animals (p=0.001) and control (p=0.002); and ii) IL-8 in 2 d C. albicans exposed animals relative to 1 d C. albicans exposed animals (p=0.044) and control (p=0.046). No change in IL-6 concentration was detected (Figure 1b). Analysis of IL-1β, IL-6 and IL-8 protein concentration in fetal lung fluid demonstrated significant increases in the concentration of: i) IL-1β in 2 d C. albicans exposed animals relative to control (680 ± 900 pg/mL vs. 157 ± 10 pg/mL; p=0.048); and ii) IL-8 in 2 d C. albicans exposed animals, relative to control (20 ± 18.5 ng/mL vs. 1.4 ± 2.0 ng/mL p=0.002). No change in fetal lung fluid IL-6 concentration was detected (data not shown).
Elevated circulating fetal cortisol
Concentrations of cortisol in fetal arterial plasma demonstrated variable, but significant increases in concentration at 2 d post-infection relative to 1 d post-infection (p=0.007) and control (p=0.002) (Figure 2).
Figure 2.
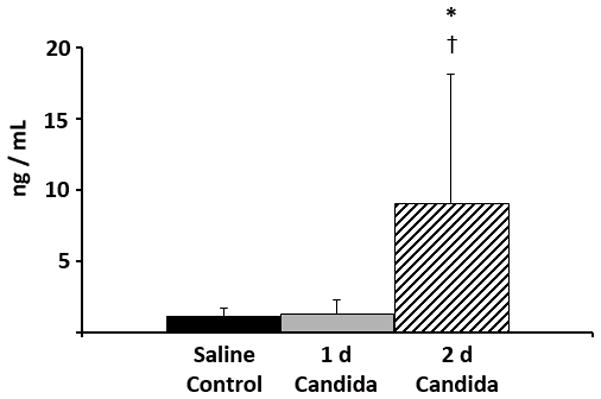
Concentration of fetal arterial plasma cortisol (Control n=13; 1 d Candida n=8; 2 d Candida n=8) is increased in response to 2 d C. albicans exposure, vs. control. * p<0.05 vs. control; † p<0.05 vs. 1 d C. albicans exposure.
Haematological analyses
Complete/differential fetal blood counts demonstrated marked thrombocytopenia and leukopenia after 2 d intrauterine C. albicans infection (Table 1); circulating platelets (p=0.026) and white blood cells (p=0.006) were significantly reduced relative to control. Lymphocytes at 2 d post-infection were significantly reduced relative to counts at 1 d post-infection (p=0.015) and an apparent reduction relative to control counts closely approached significance (p=0.08).
Table 1.
Group, birth-weight and differential blood count summary data for control (n=13), 1 d (n=8) and 2 d (n=8) Candida post-infection groups.
| n | Fetal Weight Kg | Platelet 109/L | Total WBC 1011/L | Monocytes 109/L | Lymphocytes 109/L | |
|---|---|---|---|---|---|---|
| Saline | 13 | 2.8 ± 0.3 | 616 ± 157 | 2.83 ± 1.3 | 0.1 ± 0.1 | 1.90 ± 1.0 |
| 1 d Candida | 8 | 3.1 ± 0.4 | 576 ± 63 | 3.50 ± 1.0 | 0.2 ± 0.01 | 2.30 ± 1.0 |
| 2 d Candida | 8 | 2.9 ± 0.2 | 437 ± 170* | 1.50 ± 1.1* | 0.2 ± 0.10 | 0.90 ± 0.80† |
p<0.05 vs. control;
p<0.05 vs. 1 d Candida post-infection group.
Elevated cytokine/chemokine mRNA expression in the fetal lung, skin and membranes
Analysis of cytokine/chemokine expression in the fetal lung, skin and membranes identified a pattern of significant mRNA up-regulation at 2 d post-C. albicans infection, relative to both control and 1 d post-C. albicans infection tissues. Significant increases in IL-1β (p=0.007), IL-6 (p=0.007), IL-8 (p=0.010), TNF-α (p=0.003) and MCP-1 (p=0.003) mRNA expression were identified in the fetal lung at 2 d post-infection, relative to control (Figure 3a). In the fetal skin, significant mRNA increases were observed in the expression of IL-6 at 2 d (p=0.004), TNF-α at 2 d (p=0.019), IL-8 at 1 d (p=0.000) and 2 d (p=0.000), and MCP-2 at 1 d (p=0.031) and 2 d (p=0.000) post-C. albicans infection, relative to control (Figure 3b). In fetal membranes, a significant increase was only observed in IL-8 mRNA expression (p=0.020) at 2 d post-C. albicans infection, relative to control (Figure 3c).
Figure 3.
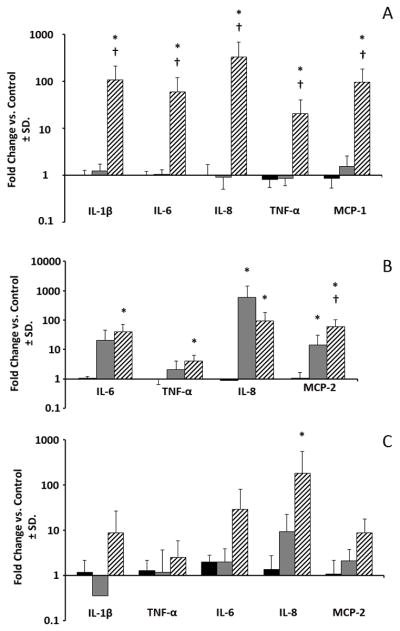
Panel A: Expression of cytokine/chemokine mRNA is increased in the fetal lung in response to 2 d C. albicans exposure. Black bars, Control n=13; Grey bars, 1 d Candida n=8; Hatched bars, 2 d Candida n=8. * p<0.05 vs. control; † p<0.05 vs. 1 d C. albicans exposure. Panel B: Expression of cytokine/chemokine mRNA is variably increased in the fetal skin in response to 1 d and 2 d C. albicans exposure. Black bars, control n=6; Grey bars, 1 d Candida n=5; Hatched bars, 2 d Candida n=6. * p<0.05 vs. control; † p<0.05 vs. 1 d C. albicans exposure. Panel C: Only IL-8 is significantly increased in the chorioamnion in response to 1 d and 2 d C. albicans exposure. Black bars, Control n=6; Grey bars, 1 d Candida n=6; Hatched bars, 2 d Candida n=5) * p<0.05 vs. control.
Histological analysis of the fetal lung and skin
Seven of eight fetal lung samples from the 2 d Candida group assessed for inflammation and consolidation were graded 2 (n=4) or 3 (n=3) (Figure 4a), consistent with robust inflammation of the fetal lung. A marked increase in C. albicans staining intensity and distribution was apparent in lung tissues taken from 2 d C. albicans-exposed animals, relative to 1 d C. albicans-exposed and saline control animals (Figure 4a insert). CD3-positive cells were significantly increased (33.0 ± 8.0 vs. 12.0 ± 4.0 cells/low power field, p=0.006) in the fetal lung of animals exposed to C. albicans for 2 d, relative to control (Figure 4b). Haemotoxylin and eosin staining of transverse fetal skin sections demonstrated numerous foci of basophilic infiltration of the stratum corneum at 2 d post-infection (Figure 5a). Immunofluorescent analysis of IL-8 expression in the fetal skin demonstrated distinct increases in signal intensity and distribution in 1 d and 2 d C. albicans exposed tissues, relative to control (Figure 5b).
Figure 4.

Infiltration and consolidation of the fetal lung in response to 2 d C. albicans exposure (Control n=13; 1 d Candida n=8; 2 d Candida n=8). Panel A: Control; Panel B: 1 d C. albicans exposure; and Panel C: 2 d C. albicans exposure. Inserts: Immunofluorescent staining for cell nuclei (DAPI; blue) and C. albicans (Alexa 594; red). All scale bars represent 50 μm. Panel D: Analysis of Infiltration of fetal lung by CD3-positive cells in response to colonization with C. albicans. (Control n=6; 1 d Candida n=5; 2 d Candida n=5) * p<0.05 vs. control. HPV, high power view.
Figure 5.
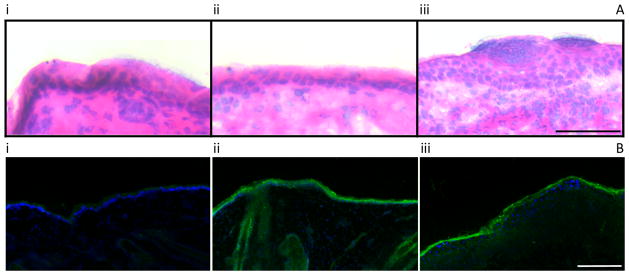
Panel A: Infiltration of the fetal skin in response to C. albicans exposure. (Control n=5; 1 d Candida n=5; 2 d Candida n=5). i: Control; ii: 1 d C. albicans exposure; and iii: 2 d C. albicans exposure. Scale bar represents 50 μm. Panel B: Relative to control, immunofluorescent staining for IL-8 (Alexa 488; green) is increased in the fetal dermis and epidermis after 1 d and 2 d C. albicans exposure. i: Control n=5 ii: 1 d Candida n=5; iii: 2 d Candida n=5. Cell nuclei are stained blue with DAPI. Scale bar represents 200 μm.
Discussion
Comparatively little animal data are available to describe the inflammatory response to acute C. albicans colonization of the amniotic cavity 33–35. We present novel data demonstrating: i) the colonization of the amniotic environment by C. albicans following intra-amniotic infection; and ii) that intrauterine infection with C.albicans rapidly progresses to an active infection involving multiple fetal surfaces yielding florid intrauterine inflammation and depletion of circulating fetal immunocytes and platelets. These findings add weight to recent clinical reports concluding that the prompt diagnosis and treatment of intraamniotic C. albicans infection is critical to pregnancy wellbeing 14.
Infection of the amniotic cavity with C. albicans was characterised by a quasi-latent period of at least 1 d post-infection. Although significant increases in IL-6, IL-8 and MCP-2 mRNA transcript expression were identified in the fetal skin and IL-8 protein concentration in the AF at 1 d post-infection, no changes were identified in lung or chorioamnion mRNA expression, fetal arterial plasma cortisol levels or fetal white blood cell counts. At 2 d post-infection, significant increases in mRNA expression were detected in the fetal skin and lung, with a limited (IL-8 only) response detected in the chorioamnion.
Cytokine/chemokine mRNA expression in the fetal skin and lung, and cytokine protein concentrations in the fetal lung fluid correlated with increased C. albicans RNA levels at 2 d. Interestingly, the vigorous inflammatory response identified in the fetal lung in the 2d post-infection group was disproportionate to the comparatively low level of C. albicans RNA detected. Conversely, the inflammatory response detected in the chorioamnion was comparatively mild (given the high levels of C. albicans RNA isolated from this tissue) at both 1 d and 2 d. These data suggest a differential sensitivity between tissues (lung, skin and chorioamnion) to inflammatory stimulation by C. albicans. Surprisingly, no C. albicans RNA was detected in the fetal spleen in either the 1 d or 2 d post-infection groups. Although we did not extensively culture from aseptically harvested fetal organs, these molecular data indicate that C. albicans does not gain access to the fetal circulation by 2 d despite significant colonization of the fetal lung and skin. This observation also suggests that the systemic changes (alterations in leukocyte counts and fetal arterial plasma) identified in this study are due to inflammatory signalling derived from amniotic fluid-exposed skin/amnion and lung. Using chronically instrumented preterm lambs, we have previously demonstrated the importance of the fetal lung to acute systemic inflammation32. Those findings are supported by data in the present study, which also suggest that fetal lung inflammation is a key mediator of a systemic fetal response. Additionally, our data also suggest that inflammation of the fetal skin/chorioamnion, in the absence of fetal lung inflammation, is sufficient to increase cytokine (IL-8) concentrations in the AF. Although not investigated in the present study, it would be of great interest to assess the inflammatory and structural changes deriving from colonization of the fourth AF-exposed fetal surface, the gastro-intestinal tract, by C. albicans.
Our data also contrast with earlier LPS-based studies in this model, wherein intraamniotic injection of 10 mg LPS resulted in broad increases in mRNA expression in both the fetal lung and chorioamnion at 1 d post-injection36. The isolation of fetal inflammatory response to the skin at 1 d post C. albicans infection may derive from the complete exposure of the fetal skin to the AF and C. albicans’ preference this epithelial surface 37. It may also reflect a temporal difference in inflammatory response between skin and chorioamnion in the sheep . Interestingly, the magnitude and scope of inflammatory response elicited by 2 d infection with C. albicans was much greater than that identified in previous studies in fetal sheep involving E. coli lipopolysaccharides or Ureaplasma spp. over a similar time frame 27,38,39.
The marked increase in fetal cortisol identified in the 2 d post-infection group is consistent with a robust fetal inflammatory response 40 and is similar in relative size to that demonstrated by Challis and colleagues in chronically catheterised fetal sheep immediately prior to parturition41; chorioamnionitis and elevated levels of IL-1β and IL-6 have also been demonstrated to increase fetal cortisol production, inducing fetal lung maturation and reduced birth weight 40,42.
Thrombocytopenia is a salient feature of congenital and neonatal candidiasis 43,44; an especially striking feature of 2 d C. albicans infection in the present study was a marked reduction in fetal platelets. In contrast to our 2 d findings, however, congenital candidiasis is associated with a marked increase in total white blood cells 8,9,45. This difference may relate to species or gestation-dependent responses to C. albicans infection or be a function of the acute (2 d) nature of our experimental model.
Limitations of this study include the acute time frame over which the impact of C. albicans infection was assessed and that the infection was established by intraamniotic injection as opposed to ascending vaginal infection and penetration of the fetal membranes, the hypothesised route of the majority of intrauterine infection in humans 2. Further studies, potentially employing a low-titre inoculum and sub-chorionic infection to mimic ascending infection via a focal breach in the fetal membranes 46, are warranted to advance our understanding of the pathogenic role played by C. albicans in pregnancy.
Conclusions
An increasing number of clinical studies now suggest a role for Candida spp. in preterm birth and fetal injury. Our data support the recently published findings of Bean and colleagues 14 and further suggest a likely role for C. albicans in preterm birth and chorioamnionitis. Importantly, our data demonstrate that an untreated acute infection of the amniotic cavity with C. albicans can cause a devastating, florid fetal inflammatory response that is consistent with adverse neonatal outcomes. Additional animal and clinical studies are warranted to further assess the role of Candida spp. in preterm birth and fetal injury, the potential benefits of Candida spp. screening and the best means of administering prophylaxis and treatment in pregnancy.
Acknowledgments
STATEMENT OF FINANCIAL SUPPORT: This work was supported by NIH grant HD 57869 to SK and by grants from the Women and Infants Research Foundation (Western Australia) and the Financial Markets Foundation for Children (Australia) to MWK.
The authors wish to thank: Pietro Presicce and Manuel Alvarez Jr. for expert technical assistance; Icon Agriculture (Darkan, Western Australia) for their expertise in date-critical animal breeding and Siemens Australia for the generous donation of Rapidlab 1265 reagents and consumables.
Footnotes
Reprints will not be available.
CONFLICT OF INTEREST STATEMENT: None declared.
Findings were presented at the 65th Annual Meeting, Society for Gynaecologic Investigation, Orlando, FL, March 18–21, 2013 and the Pediatric Academic Societies Annual Meeting, Washington D.C., May 4–7, 2013.
References
- 1.Agrawal V, Hirsch E. Intrauterine infection and preterm labor. Seminars in Fetal and Neonatal Medicine. 2012;17:12–9. doi: 10.1016/j.siny.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Romero R, Espinoza J, Kusanovic JP, et al. The preterm parturition syndrome. BJOG: An International Journal of Obstetrics and Gynaecology. 2006;113:17–42. doi: 10.1111/j.1471-0528.2006.01120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bastek JA, Gomez LM, Elovitz MA. The role of inflammation and infection in preterm birth. Clinics in Perinatology. 2011;38:385–406. doi: 10.1016/j.clp.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 5.DiGiulio DB. Diversity of microbes in amniotic fluid. Seminars in Fetal and Neonatal Medicine. 2012;17:2–11. doi: 10.1016/j.siny.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Jones HE, Harris KA, Azizia M, et al. Differing prevalence and diversity of bacterial species in fetal membranes from very preterm and term labor. PLoS ONE. 2009;4:1–9. doi: 10.1371/journal.pone.0008205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DiGiulio DB, Romero R, Kusanovic JP, et al. Prevalence and Diversity of Microbes in the Amniotic Fluid, the Fetal Inflammatory Response, and Pregnancy Outcome in Women with Preterm Pre-Labor Rupture of Membranes. American Journal of Reproductive Immunology. 2010;64:38–57. doi: 10.1111/j.1600-0897.2010.00830.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Darmstadt GL, Dinulos JG, Miller Z. Congenital cutaneous candidiasis: Clinical presentation, pathogenesis, and management guidelines. Pediatrics. 2000;105:438–44. doi: 10.1542/peds.105.2.438. [DOI] [PubMed] [Google Scholar]
- 9.Gonçalves-Ferri WA, Sato DA, Ramalho FS, De Carvalho Panzeri Carlotti AP, Duarte G, Mussi-Pinhata MM. Congenital systemic candidiasis without skin lesions presenting as septic shock in a late preterm infant. Journal of Pediatric Infectious Diseases. 2012;7:131–4. [Google Scholar]
- 10.Tiraboschi ICN, Niveyro C, Mandarano AM, et al. Congenital candidiasis: Confirmation of mother-neonate transmission using molecular analysis techniques. Medical Mycology. 2010;48:177–81. doi: 10.3109/13693780902824962. [DOI] [PubMed] [Google Scholar]
- 11.Van Winter JT, Ney JA, Ogburn PL, Jr, Johnson RV. Preterm labor and congenital candidiasis: A case report. Journal of Reproductive Medicine for the Obstetrician and Gynecologist. 1994;39:987–90. [PubMed] [Google Scholar]
- 12.DiGiulio DB, Romero R, Amogan HP, et al. Microbial prevalence, diversity and abundance in amniotic fluid during preterm labor: A molecular and culture-based investigation. PLoS ONE. 2008:3. doi: 10.1371/journal.pone.0003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rode ME, Morgan MA, Ruchelli E, Forouzan I. Candida chorioamnipnitis after serial therapeutic amniocenteses: A possible association. Journal of Perinatology. 2000;20:335–7. doi: 10.1038/sj.jp.7200381. [DOI] [PubMed] [Google Scholar]
- 14.Bean LM, Jackson JR, Dobak WJ, Beiswenger TR, Thorp JA. Intra-amniotic fluconazole therapy for Candida albicans intra-amniotic infection. Obstetrics and Gynecology. 2013;121:452–4. doi: 10.1097/aog.0b013e31827566ca. [DOI] [PubMed] [Google Scholar]
- 15.Mendling W, Brasch J. Guideline vulvovaginal candidosis (2010) of the german society for gynecology and obstetrics, the working group for infections and infectimmunology in gynecology and obstetrics, the german society of dermatology, the board of german dermatologists and the german speaking mycological society. Mycoses. 2012;55:1–13. doi: 10.1111/j.1439-0507.2012.02185.x. [DOI] [PubMed] [Google Scholar]
- 16.Roberts CL, Rickard K, Kotsiou G, Morris JM. Treatment of asymptomatic vaginal candidiasis in pregnancy to prevent preterm birth: An open-label pilot randomized controlled trial. BMC Pregnancy and Childbirth. 2011:11. doi: 10.1186/1471-2393-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369:1961–71. doi: 10.1016/S0140-6736(07)60917-9. [DOI] [PubMed] [Google Scholar]
- 18.Cotch MF, Hillier SL, Gibbs RS, et al. Epidemiology and outcomes associated with moderate to heavy Candida colonization during pregnancy. American Journal of Obstetrics and Gynecology. 1998;178:374–80. doi: 10.1016/s0002-9378(98)80028-8. [DOI] [PubMed] [Google Scholar]
- 19.Czeizel AE, Fladung B, Vargha P. Preterm birth reduction after clotrimazole treatment during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2004;116:157–63. doi: 10.1016/j.ejogrb.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 20.Kiss H, Petricevic L, Husslein P. Prospective randomised controlled trial of an infection screening programme to reduce the rate of preterm delivery. British Medical Journal. 2004;329:371–4. doi: 10.1136/bmj.38169.519653.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Snyder CC, Wolfe KB, Gisslen T, et al. Modulation of lipopolysaccharide-induced chorioamnionitis by Ureaplasma parvum in sheep. American Journal of Obstetrics and Gynecology. 2013;208:399.e1–e8. doi: 10.1016/j.ajog.2013.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moss TJ, Nitsos I, Knox CL, et al. Ureaplasma colonization of amniotic fluid and efficacy of antenatal corticosteroids for preterm lung maturation in sheep. Am J Obstet Gynecol. 2009;200:96.e1–6. doi: 10.1016/j.ajog.2008.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kallapur SG, Nitsos I, Moss TJM, et al. IL-1 mediates pulmonary and systemic inflammatory responses to chorioamnionitis induced by lipopolysaccharide. American Journal of Respiratory and Critical Care Medicine. 2009;179:955–61. doi: 10.1164/rccm.200811-1728OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moss TJM, Knox CL, Kallapur SG, et al. Experimental amniotic fluid infection in sheep: Effects of Ureaplasma parvum serovars 3 and 6 on preterm or term fetal sheep. American Journal of Obstetrics and Gynecology. 2008;198:122.e1–e8. doi: 10.1016/j.ajog.2007.06.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moss TJ, Nitsos I, Ikegami M, Jobe AH, Newnham JP. Experimental intrauterine Ureaplasma infection in sheep. Am J Obstet Gynecol. 2005;192:1179–86. doi: 10.1016/j.ajog.2004.11.063. [DOI] [PubMed] [Google Scholar]
- 26.Wolfs TGAM, Kallapur SG, Knox CL, et al. Antenatal ureaplasma infection impairs development of the fetal ovine gut in an IL-1-dependent manner. Mucosal Immunology. 2013;6:547–56. doi: 10.1038/mi.2012.97. [DOI] [PubMed] [Google Scholar]
- 27.Kemp MW, Saito M, Kallapur SG, et al. Inflammation of the fetal ovine skin following in utero exposure to Ureaplasma parvum. Reproductive Sciences. 2011;18:1128–37. doi: 10.1177/1933719111408114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kallapur SG, Kramer BW, Knox CL, et al. Chronic fetal exposure to Ureaplasma parvum suppresses innate immune responses in sheep. J Immunol. 2011;187:2688–95. doi: 10.4049/jimmunol.1100779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Innings A, Ullberg M, Johansson A, et al. Multiplex real-time PCR targeting the RNase P RNA gene for detection and identification of Candida species in blood. J Clin Microbiol. 2007;45:874–80. doi: 10.1128/JCM.01556-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bustin SA, Benes V, Garson JA, et al. The MIQE guidelines: Minimum information for publication of quantitative real-time PCR experiments. Clinical Chemistry. 2009;55:611–22. doi: 10.1373/clinchem.2008.112797. [DOI] [PubMed] [Google Scholar]
- 31.Zhang L, Saito M, Jobe A, et al. Intra-amniotic administration of e coli lipopolysaccharides causes sustained inflammation of the fetal skin in sheep. Reproductive Sciences. 2012;19:1181–9. doi: 10.1177/1933719112446079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kemp MW, Kannan PS, Saito M, et al. Selective Exposure of the Fetal Lung and Skin/Amnion (but Not Gastro-Intestinal Tract) to LPS Elicits Acute Systemic Inflammation in Fetal Sheep. PLoS ONE. 2013:8. doi: 10.1371/journal.pone.0063355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carrara MA, Donatti L, Damke E, Svidizinski TIE, Consolaro MEL, Batista MR. A new model of vaginal infection by Candida albicans in rats. Mycopathologia. 2010;170:331–8. doi: 10.1007/s11046-010-9326-1. [DOI] [PubMed] [Google Scholar]
- 34.Clemons KV, Spearow JL, Parmar R, Espiritu M, Stevens DA. Genetic susceptibility of mice to Candida albicans vaginitis correlates with host estrogen sensitivity. Infection and Immunity. 2004;72:4878–80. doi: 10.1128/IAI.72.8.4878-4880.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fidel PL, Jr, Lynch ME, Sobel JD. Candida-specific cell-mediated immunity is demonstrable in mice with experimental vaginal candidiasis. Infection and Immunity. 1993;61:1990–5. doi: 10.1128/iai.61.5.1990-1995.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kramer BW, Moss TJ, Willet KE, et al. Dose and time response after intraamniotic endotoxin in preterm lambs. American Journal of Respiratory and Critical Care Medicine. 2001;164:982–8. doi: 10.1164/ajrccm.164.6.2103061. [DOI] [PubMed] [Google Scholar]
- 37.Zhu W, Filler SG. Interactions of Candida albicans with epithelial cells. Cellular Microbiology. 2010;12:273–82. doi: 10.1111/j.1462-5822.2009.01412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kallapur SG, Willet KE, Jobe AH, Ikegami M, Bachurski CJ. Intra-amniotic endotoxin: Chorioamnionitis precedes lung maturation in preterm lambs. American Journal of Physiology - Lung Cellular and Molecular Physiology. 2001;280:L527–L36. doi: 10.1152/ajplung.2001.280.3.L527. [DOI] [PubMed] [Google Scholar]
- 39.Kemp MW, Saito M, Nitsos I, Jobe AH, Kallapur SG, Newnham JP. Exposure to in utero lipopolysaccharide induces inflammation in the fetal ovine skin. Reproductive Sciences. 2011;18:88–98. doi: 10.1177/1933719110380470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Watterberg KL. Adrenocortical function and dysfunction in the fetus and neonate. Seminars in Neonatology. 2004;9:13–21. doi: 10.1016/j.siny.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 41.Challis JRG, Dilley SR, Robinson JS, Thorburn GD. Prostaglandins in the circulation of the fetal lamb. Prostaglandins. 1976;11:1041–52. doi: 10.1016/0090-6980(76)90011-3. [DOI] [PubMed] [Google Scholar]
- 42.Newnham JP, Moss TJM, Nitsos I, Sloboda DM. Antenatal corticosteroids: The good, the bad and the unknown. Current Opinion in Obstetrics and Gynecology. 2002;14:607–12. doi: 10.1097/00001703-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Benjamin DK, Jr, DeLong ER, Steinbach WJ, Cotton CM, Walsh TJ, Clark RH. Empirical therapy for neonatal candidemia in very low birth weight infants. Pediatrics. 2003;112:543–7. doi: 10.1542/peds.112.3.543. [DOI] [PubMed] [Google Scholar]
- 44.Dyke MP, Ott K. Severe thrombocytopenia in extremely low birthweight infants with systemic candidiasis. Journal of Paediatrics and Child Health. 1993;29:298–301. doi: 10.1111/j.1440-1754.1993.tb00516.x. [DOI] [PubMed] [Google Scholar]
- 45.Baud O, Boithias C, Lacaze-Masmonteil T, et al. Congenital disseminated candidiasis in very preterm infants. Infection maternofoetale disseminee a Candida albicans et grande prematurite. 1997;4:331–4. doi: 10.1016/s0929-693x(97)86449-4. [DOI] [PubMed] [Google Scholar]
- 46.Kim MJ, Romero R, Gervasi MT, et al. Widespread microbial invasion of the chorioamniotic membranes is a consequence and not a cause of intra-amniotic infection. Laboratory Investigation. 2009;89:924–36. doi: 10.1038/labinvest.2009.49. [DOI] [PMC free article] [PubMed] [Google Scholar]


