Abstract
The conquest of pellagra is commonly associated with one name: Joseph Goldberger of the US Public Health Service, who in 1914 went south, concluded within 4 months that the cause was inadequate diet, spent the rest of his life researching the disease, and—before his death from cancer in 1929—found that brewer's yeast could prevent and treat it at nominal cost. It does Goldberger no discredit to emphasize that between 1907 and 1914 a patchwork coalition of asylum superintendents, practicing physicians, local health officials, and others established for the first time an English-language competence in pellagra, sifted through competing hypotheses, and narrowed the choices down to two: an insect-borne infection hypothesis, championed by the flamboyant European Louis Westerna Sambon, and the new “vitamine hypothesis,” proffered by Casimir Funk in early 1912 and articulated later that year by two members of the American Clinical and Climatological Association, Fleming Mant Sandwith and Rupert Blue. Those who resisted Goldberger's inconvenient truth that the root cause was southern poverty drew their arguments largely from the Thompson-McFadden Pellagra Commission, which traces back to Sambon's unfortunate influence on American researchers. Thousands died as a result.
INTRODUCTION
Medical students learn pellagra as “the disease of four D's”—dermatitis, diarrhea, dementia, and death—caused by deficiency of niacin (vitamin B3). Its protean manifestations reflect in part the requirement for nicotinamide in the coenzyme pair NAD+/NADH (Figure 1). During the early 20th century, pellagra claimed at its peak at least 7,000 lives each year in the 15 southern states. The root cause was monotonous diet due to poverty. The proximate cause may have been the early-20th-century invention of the Beall degerminator, which changed corn from a whole grain to a highly-refined carbohydrate upon which millions of Americans relied for most of their caloric intake.
Fig. 1.

The principal forms of niacin are nicotinic acid and nicotinamide. Both are usually derived from food, but the body can synthesize nicotinamide from tryptophan. Niacin is a component of (among other things) the coenzymes NAD+ and NADH, the numerous functions of which—including the synthesis of ATP, explain the protean manifestations of pellagra.
The conquest of pellagra is commonly associated with one name: Joseph Goldberger (Figure 2). In February 1914, Surgeon General Rupert Blue of the US Public Health Service made Goldberger his chief pellagra investigator. As the story is usually told, pellagra was widely considered an infectious disease and most people, including Goldberger himself, anticipated that he would find the causative germ. Goldberger went south and observed at orphanage after orphanage, asylum after asylum, that inmates' diets were monotonous and that staff members never got pellagra. By June 1914, Goldberger concluded that pellagra was caused by inadequate diet, and by late 1915 he had prevented and caused pellagra by dietary manipulation alone. Southern public health officials, politicians, and others rejected the dietary explanation especially because it indicted southern poverty. Goldberger devoted the rest of his life to pellagra and, before his death from cancer, found an inexpensive way to prevent and treat it: brewer's yeast. After Goldberger's ashes were scattered into the Potomac River on January 18, 1929, then−Surgeon General Hugh Cumming wrote that “the disease which has baffled the best medical talent of Europe for two centuries has yielded well within a decade to the researches of one American scientist” (1).
Fig. 2.

Joseph Goldberger (1874−1929) acknowledged those who helped him reach his conclusions about pellagra. Courtesy: National Library of Medicine.
Goldberger never told the story quite that way. It does him no discredit to note that between 1907 and 1914 a patchwork coalition of asylum superintendents, practicing physicians, local health officials, and others established for the first time an English-language competence in pellagra, sifted through competing hypotheses, and narrowed the choices down to two: an insect-borne infection hypothesis, championed by the flamboyant European Louis Westerna Sambon, and the new “vitamine hypothesis,” proffered by Casimir Funk in early 1912 and articulated later that year in the United States by two members of the American Clinical and Climatological Association, Fleming Mant Sandwith and Rupert Blue. Those who resisted Goldberger's inconvenient truth that the root cause was southern poverty sought scientific refuge in the Thompson-McFadden Pellagra Commission, which traces back to Sambon's unfortunate impact on American researchers.
THE AMERICAN RESPONSE TO PELLAGRA, 1907–1914
Although there had been rare case reports of pellagra in the United States before 1907, it was generally thought not to occur in this nation, as William Osler wrote in the sixth edition of his textbook (2). However, in April 1907, Dr George H. Searcy of Alabama reported epidemic pellagra at the Mt Vernon Hospital for the Colored Insane (3). Later that year, Dr James Woods Babcock (Figure 3) and his colleagues at the South Carolina State Hospital for the Insane in Columbia, unaware of Searcy's reports, made the same observation. Searcy and Babcock described a more aggressive disease than was usually observed in Europe (4). In June 1908, Babcock went to Italy and confirmed that pellagra in the United States was nonetheless the same disease familiar to Italians (5). On the way home he had an audience in London with the foremost authority on pellagra in the English-speaking world, Fleming Mant Sandwith (Figure 4) (6–9). Sandwith had expanded the known range of highly endemic pellagra to include Egypt and South Africa, and his suspicion that conditions were ripe for pellagra in parts of the United States had now been confirmed by Searcy and Babcock.
Fig. 3.
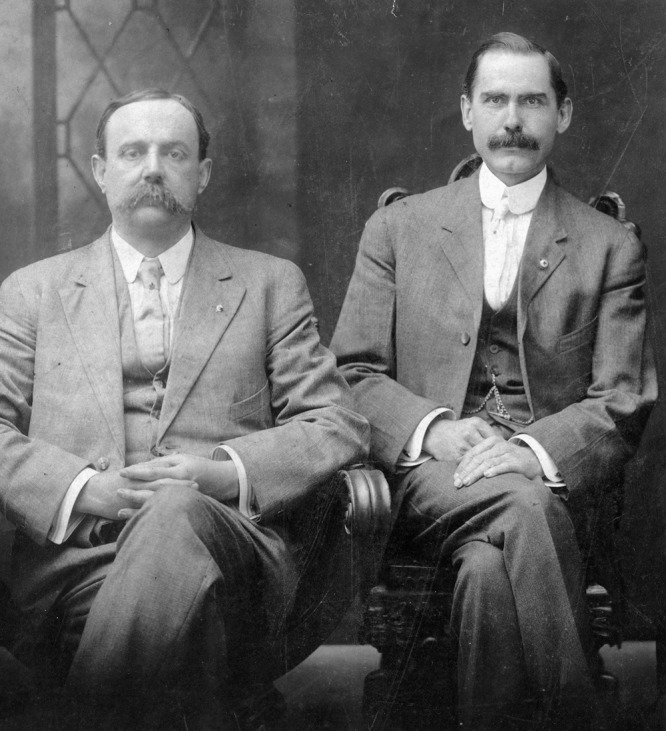
James Woods Babcock (1856−1922) (left), with Robert Wilson Jr. (1867−1946). Babcock, who was superintendent of the South Carolina State Hospital for the Insane, spearheaded the early American response to pellagra. Wilson, who later served as vice president of the American Clinical and Climatological Association, was chairman of the South Carolina State Board of Health. Courtesy: South Caroliniana Library, University of South Carolina, Columbia, S.C.
Fig. 4.

Fleming Mant Sandwith (1853−1918) was elected a corresponding member of ACCA in 1904, and was the only authority on pellagra in the English-speaking world in 1907 when American physicians began to recognize the disease. Courtesy: National Portrait Gallery, London.
Southern physicians soon realized they had a major problem. They began to see numerous patients with stereotypical pellagra (Figure 5), especially in asylums, orphanages, textile workers, and the rural poor. What was the cause? How should it be treated, or, better, prevented? Speculations abounded, but nearly everyone recognized that pellagra usually occurred in the setting of monotonous diet and that treatment included a diet rich in milk, meat, and vegetables.
Fig. 5.
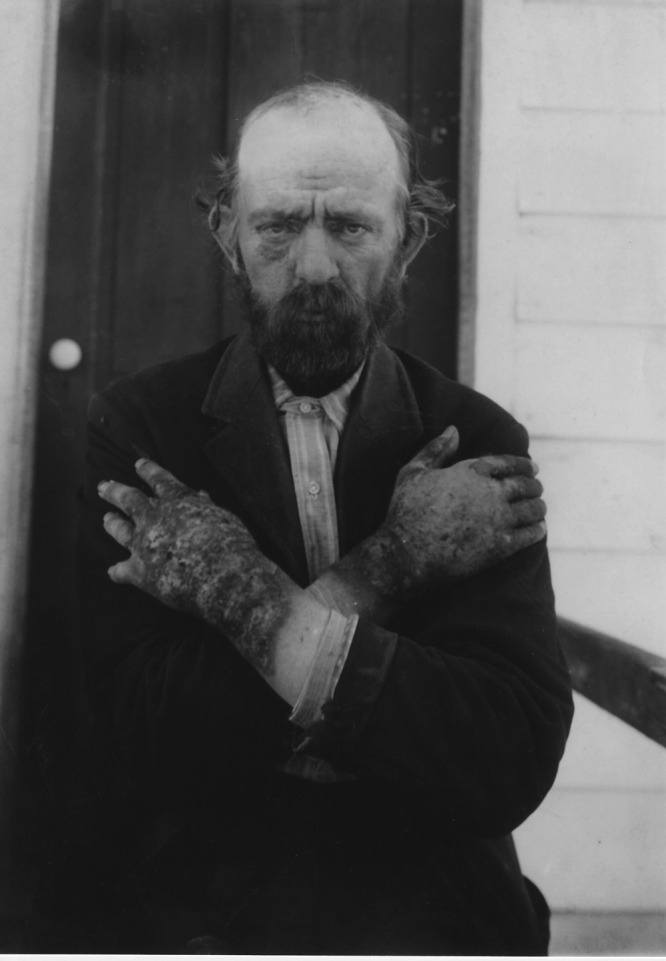
This photograph, taken by Dr. Joseph Jenkins Watson of Columbia, SC, is perhaps the most frequently reproduced illustration of pellagra in English-language accounts. “Pellagrins,” wrote Harvey E. McConnell of Chester, SC, “almost always have a frown of their foreheads” and the “erythematous eruption of the hands … the most constant and diagnostic sign … needs to be seen only once to be recognized, and if you ever shake hands with one of these patients, you never forget the sensation.” Courtesy: Waring Historical Library, Medical University of South Carolina, Charleston, SC.
Europeans, beginning with the Spaniard Gaspar Casál who between 1720 and 1735 described a disease known to Asturian peasants as mal de la rosa or “disease of the red rash,” had correlated pellagra with poverty and prescribed better diet. In 1810, an Italian, Giovanni Battista Marzari, proposed that corn lacked something necessary for health—that pellagra might be a deficiency disease. These and other observations anticipated Goldberger's breakthrough. What went wrong?
Late-19th-century enthusiasm for the germ theory fueled a chase for infectious etiologies, as it did for other diseases of then-unknown origin. Two variants of the germ theory ultimately required enormous expenditures of time and money to disprove. The Italian Cesare Lombroso, who is best remembered as “the father of modern criminology” because his work in forensic psychiatry shifted focus from the crime to the criminal, championed the idea that pellagra was caused by a toxin in spoiled corn. He claimed a specific fungus, Sporisorium maidis, caused corn to make a pellagra-causing toxin which he named pellagrozeïn. Louis Sambon (Figure 6) formulated an insect-borne infection hypothesis. The argument will be made here that Sambon's intricate speculation more than anything else sidetracked Americans' scientific assault on pellagra and led to thousands of deaths that might have been prevented.
Fig. 6.
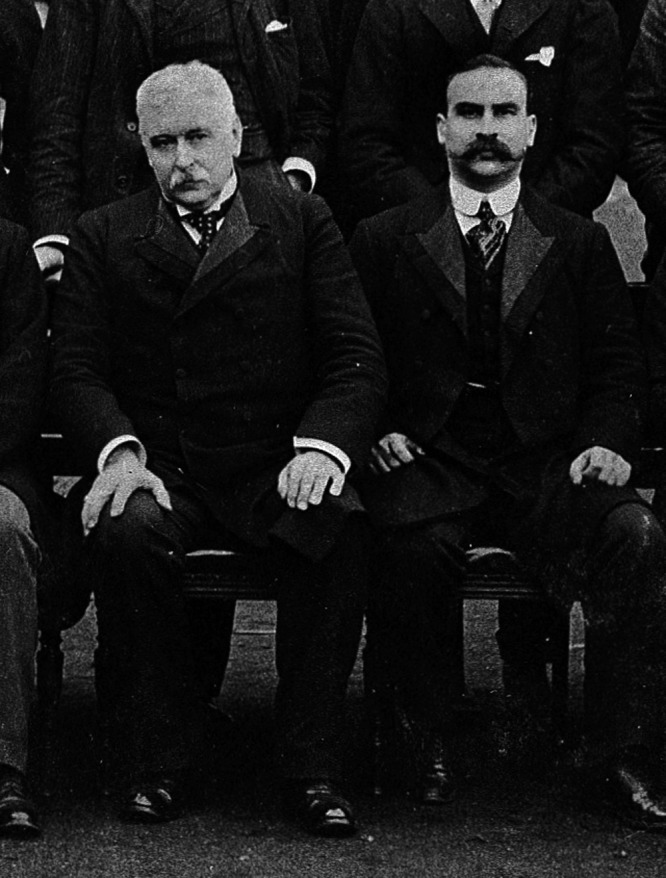
Sir Patrick Manson (1844−1922) and Louis Westerna Sambon (1865−1931) at the London School of Tropical Medicine in 1902. Note Sambon's upright posture, direct gaze, and clenched fists—features that are also present in other group photographs containing Sambon. Courtesy: London School of Hygiene and Tropical Medicine.
Sambon, born Luigi Westerna Sambon in Milan, was as extroverted and self-asserting as Fleming Sandwith was introverted and self-effacing. He was a “romantic and colorful figure” with an “electric temperament” who came across as “grandiloquent in style,” “assured in judgment and pugnacious in tone,” and nearly always “exuberant.” He could charm an audience not only as a scientist but also as a cordon bleu cook, an accomplished amateur archaeologist, a naturalist, a mountaineer, a linguist, and a connoisseur of the arts (10,11). As a lecturer, he
“was brilliant and entertaining and his histrionic performances were always a great draw. He strutted and gesticulated on the stage, using the arts and actions of a great actor. It did not matter if his facts were drawn on a too generous scale from the realms of mythology or were based on his fertile imagination. It was sensational; it was stimulating, and invariably invoked applause” (12).
Sambon began his career as a gynecologist in Rome, became interested in infectious diseases (13), moved to London, and courted controversy at the Royal Geographical Society by proposing that parts of Africa were “the white man's grave” not because of the climate but because of parasites, notably the trypanosomes that cause sleeping sickness (14). Sir Patrick Manson, the “father of tropical medicine,” had become almost obsessed with finding parasitic causes of diseases of then-unknown origin (15) and therefore welcomed the colorful and supremely self-confident Sambon into the London School of Tropical Medicine. Many admired Sambon's powers of inductive reasoning. An editorialist wrote: “Apart from Manson perhaps no one working at tropical medicine has given us so many new ideas as Dr. Louis Sambon” (16).
In 1902, Manson and Sambon opposed the idea that beriberi was caused by monotonous diet, favoring an infectious etiology instead (17). In 1905, Sambon speculated that pellagra was a vector-borne infectious disease (18). Basing his argument on the seasonal and geographic distribution of pellagra in northern Italy, where pellagra seemed to occur mainly in people living near fast-flowing streams, he reasoned that pellagra was caused by a specific infectious agent (probably a protozoan parasite and possibly a trypanosome) transmitted by a specific insect (probably a fly of the genus Simulium, which includes buffalo gnats, sand flies, and black flies).
When Americans encountered epidemic pellagra in 1907, there were two major sets of hypotheses: the Zeist hypotheses (based on the idea that Indian corn [Zea mays] had a definite causal relationship to pellagra), and the anti-Zeist hypotheses (based on the idea that Indian corn had nothing to do with it). Foremost among the Zeist hypotheses was Lombroso's spoiled-corn hypothesis. Foremost among the anti-Zeist hypotheses was Sambon's thesis that pellagra was an infectious disease transmitted by the Simulium flies.
On October 29, 1908, the first conference on pellagra ever held in an English-speaking country took place at the South Carolina State Hospital for the Insane, organized by Babcock. The proceedings were published in the state medical journal and as a separate booklet (19), making this the first monograph on pellagra in English. Seventy-two physicians and approximately 200 laypersons attended. Babcock concluded that pellagra in the American Southeast resembled the Italian and Egyptian forms of the disease, but with important differences: the overwhelming preponderance of females, the high death rate early in the disease, and the presence of rash in areas normally covered by clothing, such as the inner thighs and the skin around the genitalia and anus (which like “Sandwith's bald tongue” may have been due to coexistent riboflavin deficiency). He echoed the Europeans' therapeutic advice: “As a rule, the patient should not be allowed any food derived from Indian corn…. A generous dietary should be given, including fresh meats and vegetables” (20). Among the attendees was Claude Lavinder of the US Public Health and Marine Hospital Service (Figure 7), who wrote the surgeon general that the regents of the Columbia asylum had passed a resolution requesting help “from the Public Health and Marine Hospital Service, or some similar scientific body”(21). Thus began the journey of the US Public Health Service (as it was renamed in 1912) toward the eventual conquest of pellagra.
Fig. 7.
Claude Hervey Lavinder (1872−1950), the first physician assigned to pellagra by the US Public Health and Marine Hospital Service. Courtesy: National Library of Medicine.
Lavinder was assigned to pellagra, arrived in Columbia in May 1909, and, with Babcock and the state health officer, Frederick Williams, determined that pellagra was widespread in South Carolina and elsewhere in the Southeast, especially in asylums (22). He set up a laboratory in Babcock's asylum and injected small animals with materials from pellagrins, with negative results. These were the first of numerous attempts to transmit pellagra from humans to animals by Lavinder and other Americans (including attempts to transmit pellagra from human to primates by at least five groups of investigators) with essentially negative results. These studies were enormously useful to Goldberger in reaching the conclusion that pellagra was not an infectious disease.
On November 3−4, 1909, the first national conference on pellagra took place at the South Carolina asylum, organized by Babcock and attended by 394 physicians and many laypersons. The 41 speakers represented 12 states, the US Public Health and Marine Hospital Service, the US Army, and six additional nations. Most speakers leaned toward the Zeist position that pellagra was somehow related to overreliance on corn, but a vocal minority represented the emerging anti-Zeists. The participants resolved to form a National Association for the Study of Pellagra and elected Babcock president. The editor of the Journal of the American Medical Association praised the “purely scientific, humanitarian spirit” with “no disposition … to seek personal gain or aggrandizement,” adding that “every delegate had come with a desire to learn more about this disease” (23). The proceedings were published as a 297-page book (24). When Goldberger first wrote on “The Etiology of Pellagra” in 1914, he drew his first three observations directly from these proceedings (25).
Physicians throughout the United States and especially in the Southeast took notice. Americans quickly surpassed Italians in the number of papers on pellagra catalogued in the Index Medicus. Between 1907 (the year Searcy reported epidemic pellagra at an Alabama asylum) and 1915 (the year Goldberger reported experiments confirming that good diet prevented pellagra), 409 Americans published 746 articles on the disease. Many of these were isolated case reports, but 118 of these 409 Americans wrote at least two papers and some were prolific. Four hard-cover monographs on pellagra, beginning with an English translation by Lavinder and Babcock of a French treatise, also appeared (26–29). American doctors who made even half-hearted attempts to stay abreast of new knowledge could now name the salient features of the disease, and the more diligent doctors could trace its history, recite competing hypotheses, and discuss treatment and prevention. The collaborative effort of so many American physicians in so many places focusing on a new disease was without precedent.
The United States lacked the institutions and infrastructures to tackle such a challenging new disease. The Hygienic Laboratory in Washington, DC, precursor to the National Institutes of Health, was a small institution, and the Centers for Disease Control and Prevention did not exist. Nevertheless, two of the groups and commissions that sprang up to examine pellagra were reasonably well funded. These were the Illinois Pellagra Commission and the Thompson-McFadden Pellagra Commission of the New York Post-Graduate Medical School. The Illinois Pellagra Commission convened in November 1909 and dissolved in November 1911 after issuing a 250-page report (30). The Thompson-McFadden Pellagra Commission convened in 1912 and remained active through 1917, issuing three reports amounting to 771 pages with 20 maps, 88 photographs, 205 figures, and 312 tables (31–33). Both commissions concluded that diet did not have a causative role. One senses the invisible guiding hand of Louis Sambon in the researchers' improbable conclusions, unsupported by solid data, that pellagra was in all likelihood an infectious disease.
The Thompson-McFadden Pellagra Commission, while well-intentioned, ultimately proved extremely counterproductive. Its origin traces to the influence of Sambon on Joseph F. Siler, one of the US Army's top infectious diseases researchers. Siler had accompanied Sambon on a trip to Italy to glean more evidence for the insect-vector hypothesis. Later, Siler no doubt told Ward J. MacNeal about Sambon's ideas while they both worked with the Illinois Pellagra Commission. This excited MacNeal especially since he had studied trypanosomes at the University of Michigan with Frederick Novy. MacNeal moved from the University of Illinois to the New York Post-Graduate Medical School, invited Siler to lecture on tropical diseases, and made sure his new boss, George N. Miller, attended. Miller obtained funding from philanthropists Robert Means Thompson and John Howard McFadden. The Thompson-McFadden Pellagra Commission set up field headquarters in Spartanburg County, SC, where pellagra was epidemic among textile workers. The field work was supervised by Siler (on loan from the US Army) and Philip E. Garrison (on loan from the US Navy). MacNeal stayed in New York to design the studies and analyze the data.
Their crucial mistake, in retrospect, was to use the methods of descriptive epidemiology—including dietary histories, which we now know to be notoriously unreliable—rather than the experimental method. They examined the habits and circumstances of 262 pellagrins in exquisite detail and concluded that diet was not the problem. They found a strong correlation between pellagra and outdoor privies, especially the “ordinary open-in-back surface” type privy used by 63% of the textile workers and their families. They failed to implicate Simulium flies and turned to the stable fly (which swarmed around privies), or perhaps the common house fly, as the likely vector.
The conceptual breakthrough came in early 1912 when Casimir Funk, a young Polish-born chemist working in London, proposed that beriberi, scurvy, rickets, and pellagra were all deficiency diseases. “Deficiency diseases,” he wrote, “break out in countries where a certain unvarying diet is partaken for long periods. When this food happens to be deficient in a substance which is necessary for the metabolism, we have the real conditions for the outbreak of this type of disease.” Beriberi and scurvy had already been shown to respond to adding something back to the diet, even though the “something” had not yet been identified: “It is now known that all these diseases, with the exception of pellagra, can be prevented and cured by the addition of certain preventive substances; the deficiency substances, which are of the nature of organic bases, we will call ‘vitamines.’” Funk acknowledged that he was not the first to apply this concept to pellagra:
“The idea that pellagra is due to some deficiency in the diet was expressed by several authors, but at the present time there is no positive evidence in favour of this theory, as against any other theory…. A glance at all the existing theories suggests that an investigation of this disease on the lines … [used for] beri-beri might yield valuable results…. Research on this subject, which in the past has been very one-sided, is rendered more difficult by the impossibility of producing experimental pellagra in animals, and also by the lack of knowledge on the prevention of the disease by means of change of diet” (34).
A vignette told by Funk's biographer strongly suggests that Louis Sambon heard Funk present his hypothesis and dismissed it: “A lecturer at the School for Tropical Diseases maintained that pellagra was transmitted by some kind of fly and was particularly prevalent in localities near swift streams! Casimir's rebuttal was received with scant attention” (35). Almost certainly the “lecturer” was the highly-opinionated Sambon, who wanted to hear Funk's hypothesis no more than he wanted the opinions of Italian physicians, most of who did not think pellagra was an infectious disease.
On October 3−4, 1912, the second of three triennial meetings of the National Association for the Study in Pellagra took place at the South Carolina State Hospital for the Insane, again organized by Babcock. The 67 papers came from 19 states, the Thompson-McFadden Pellagra Commission, the US Public Health Service, the US Department of Agriculture, and eight additional nations. Opinion on causation remained sharply divided. Lombroso's spoiled-corn hypothesis was down but not yet out, but the conference was by no means a coronation of the germ theory or, more specifically, of Sambon's version of it. Funk's vitamin-deficiency hypothesis was introduced at a “Symposium on Pellagra” that began at 8:30 PM on the conference's long and sometimes tedious first day. Poor timing blunted its impact.
Surgeon General Rupert Blue (Figure 8) was the first to mention in public Funk's hypothesis on American soil. He outlined four “well-defined” theories of etiology: infection, intoxication, auto-intoxication, and food “deficiency.” He intended to focus on the first (and specifically on Sambon's hypothesis) and fourth (and specifically on Funk's hypothesis) because these seemed the most promising. He, like others, found Sambon's hypothesis intriguing but lacking data. Blue continued:
“A second promising line of investigation as regards the causation of the disease is to be found in the deficiency theory as advanced by Casimir Funk. He states that ‘it is beyond any doubt that pellagra has some close association with maize diet.’ Pellagra is thus placed in the same category with scurvy and beriberi. It is only in the case of an exclusive or one-sided diet of corn: and, if the corn is spoiled, it is all the more deficient in nutritive values” (36).
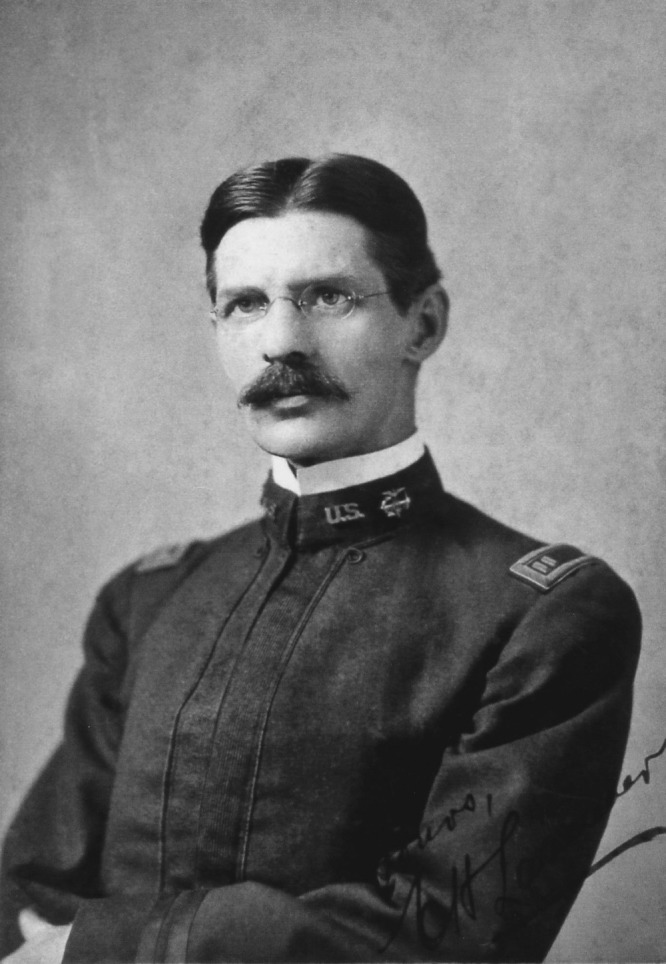
Fig. 8.

Surgeon General Rupert Blue (1868−1948) of the US Public Health Service, who was elected to ACCA in 1914, mentioned Casimir Funk's “vitamine hypothesis” during the 1912 conference of the National Association for the Study of Pellagra. Courtesy: National Library of Medicine.
Blue had little more to say about Funk's hypothesis, but the next speaker, Fleming Sandwith, said a lot in his compact paper, “Can Pellagra Be a Disease due to Deficiency of Nutrition?” (37).
Babcock had written Sandwith on May 2, 1912, inviting him to submit a paper for the conference. Sandwith wrote back that he could not attend because he was overwhelmed with routine work, adding that he had “nothing fresh to say on the subject” (38). Sometime between May and October 1912 he learned of Funk's hypothesis and, as they were both in London, they possibly met. Sandwith through his submitted paper told the conference attendees that “some of my valued correspondents in the Southern States” had been impressed with the discovery that beriberi was caused by “too continuous use of polished rice” and that “now a young chemist, Dr Casimir Funk,” had closed in on the key substance in rice polishings. Sandwith mentioned Frederick Gowland Hopkins's demonstration that young mice needed tryptophan and suggested that “tryptophan might be directly utilized as the normal precursor of some specific ‘hormone,’ or other substance essential to the processes of the body.” Sandwith asked: “Is pellagra, too, a deficiency disease, waiting for a ‘Vitamine’ to be discovered?”(37).
Many and perhaps most attendees probably forgot about Sambon's short paper while listening (if they were still awake) to the windy paper that followed, submitted by Sambon and like Sandwith's read by a stand-in. Sambon expressed gratification that various American doctors had “already confirmed my topographic findings” suggesting that pellagra was transmitted by Simulium flies along the banks of fast-flowing streams (39).
Correspondence subsequent to the meeting indicates that Babcock grasped the significance of the vitamin-deficiency hypothesis, as did Carl Alsberg of the US Department of Agriculture (40,41). Alsberg suggested feeding experiments with extracts that might contain vitamins. Unfortunately, nobody seriously followed up on the idea. Babcock was not a researcher and Alsberg had just been promoted to chief of the Bureau of Chemistry of the US Department of Agriculture, a job that evolved under his leadership into the now-powerful position of director of the US Food and Drug Administration. However, Sandwith published the next year a paper entitled “Is pellagra a disease due to deficiency of nutrition?” He wrote, “The recent developments in connection with beri-beri have caused me to wonder anew whether we have not here to deal with another disease due to deficiency of nutrition. I therefore ventured to express this view in a paper I was asked to contribute to the Conference on pellagra held in Columbia, South Carolina, in October, 1912” (42). Sandwith's 1913 paper constitutes the strongest articulation of the vitamin-deficiency hypothesis for pellagra before Goldberger entered the fray.
They had not heard the last from Louis Sambon, who had been invited to be the featured speaker for the public announcement of the Thompson-McFadden Pellagra Commission's first progress report, scheduled for September 3, 1913, in Spartanburg, SC. Sambon sailed from England and, upon reaching New York, told reporters all about Simulium flies and fast-flowing streams, adding that “food had absolutely nothing to do with the spread of pellagra” (43). He dominated the 1-day meeting and, returning to New York, told reporters at the Hotel Astor that it had been agreed in Spartanburg that “pellagra was an infectious disease, the germ carried by an insect” (44). It was a classic example of science by consensus.
It was also a classic example of Sambon's misleading ebullience. Local newspapers, archival sources, and a comment made during a medical meeting 19 years later strongly suggest that Sambon's 1913 North American adventure seriously weakened his swaggering self-confidence in the insect-vector hypothesis (45–51). The Thompson-McFadden researchers had been unable to implicate any insect. After the Spartanburg meeting, Sambon, along with Siler and the entomologist Allan Jennings, went to Charleston to study pellagra in the neighboring barrier islands, where pellagra was endemic among African Americans. Again, they could not implicate Simulium flies. Sambon, Siler, and Jennings later went to the British West Indies; again, they found pellagra but no evidence for transmission by Simulium flies. After returning to London, Sambon, according to a letter his wife wrote to Joseph Siler, began to doubt his hypothesis and went to Italy for further investigations (51). Sambon apparently “gave up” on his hypothesis, but failed to convey any new doubts to the American researchers.
Meanwhile, the epidemic grew worse. Highly reliable statistics are unavailable, but, according to a paper published by Lavinder in 1912, at least 30,000 cases of pellagra had been reported in the US from all but nine states, with a case-fatality rate approaching 40 percent (52). Lavinder now based his pellagra investigations at the Marine Hospital in Savannah, GA, where he became bogged down in administration and patient care. He wrote Babcock that “I dream pellagra these days, but no inspiration comes to help me get a clue. The whole thing gets worse and worse,” and described his going back and forth among hypotheses as “mental gymnastics with a vengeance” (53).
In early 1914, Lavinder sought relief from pellagra work. He had helped sound the alarm, clarified the epidemic's extent, and shown that pellagra could not be transmitted from humans to rhesus monkeys or other animals, at least not easily (54). On February 7, 1914, Surgeon General Blue asked 39-year-old Joseph Goldberger to replace Lavinder, telling Goldberger that the work “could be placed in no better hand” (55). Goldberger received instructions to go to Savannah and Milledgeville, GA, and then to Spartanburg, SC, to “inspect the operation of the Service in respect to pellagra investigations at those points” (56).
JOSEPH GOLDBERGER GOES SOUTH
The rest of the story has been told many times. Goldberger published within 4 months that pellagra was not an infectious disease, but was caused instead by monotonous diet (25). His quick conclusion is often depicted as an “aha moment”—a sudden, brilliant flash or insight. Goldberger's first biographer wrote: “He had no previous experience with the disease, and knew nothing about it except that two centuries of investigation had been entirely unrewarded” (57). Others have written, for example, that “the US Public Health Service assigned Joseph Goldberger to study pellagra, presumably to find its infectious agent” (58), or that “Goldberger was expected, by the USPHS and himself, to find an infectious cause of pellagra” (59). Goldberger, to reiterate, never told the story this way, and these accounts overlook the extent to which he knew about pellagra, the extent to which Rupert Blue, who sent him south, almost surely favored a dietary explanation, and the extent to which competing hypotheses had been simplified by American students of the disease.
First, in June 1911, Goldberger and John F. Anderson, director of the Hygienic Laboratory in Washington, D.C., published their unsuccessful attempts to transmit pellagra from two patients to five rhesus monkeys (60). This paper seems to have been overlooked by all historians of pellagra, Goldberger's biographers, and even Goldberger's bibliographer (61), possibly because the Index Medicus incorrectly cited Anderson as sole author. Clearly, then, Goldberger had been thinking about pellagra for at least three years and had discussed it many times with Anderson and perhaps with other researchers.
Second, to reiterate, Rupert Blue, who sent Goldberger south, almost surely favored dietary deficiency. In 1909, two years before he became surgeon general, Blue told members of the San Francisco Medical Society that although “the communicability of the disease has … received considerable attention … I do not believe that the evidence thus far presented warrants us in the belief that pellagra is contagious or infectious” (62). Blue had publically mentioned Funk's “vitamine hypothesis.” It is safe to assume that Blue and Goldberger discussed these ideas extensively.
Finally, although the competing hypotheses made up a crowded field, the smart money was betting on just two: the infection hypothesis and the dietary-deficiency hypothesis (Table 1). Goldberger was in a position familiar to all student test-takers: a multiple-choice question essentially narrowed down to two.
TABLE 1.
The Leading Hypotheses on Causation of Pellagra in February 1914
| Nutritional Deficiency Hypothesis | Infection Hypothesis | |
|---|---|---|
| Essence | Pellagra is caused by a monotonous diet deficient in one or more key nutrients. | Pellagra is caused by an unidentified infectious agent, possibly transmitted by an insect. |
| School of thought | Zeists (but open to the possibility that eating corn is not a prerequisite for pellagra) | Anti-Zeists (holding that pellagra has nothing to do with corn) |
| Historical context | Observations by Europeans, beginning with Gaspar Casál (1720−1735), that pellagra occurs almost exclusively in persons whose diet consists mainly of corn | Late 19th-century germ theory of disease, setting off a pursuit for infectious causes of most if not all diseases of then-unknown origin |
| Prime originator(s) | Giovanni Battista Marzari (1810) | Various Italians |
| Refinement | Pellagra is caused by vitamin deficiency (Casimir Funk, 1912) | Pellagra is transmitted by an insect, possibly a fly of the genus Simulium (Louis Sambon, 1905) |
| Chief proponents | Casimir Funk and Fleming Sandwith in Great Britain; in the United States, no clear champion although Rupert Blue, James W. Babcock, Carl Alsberg, Edward Vedder, and others mentioned the idea and many saw an analogy with beriberi | Sambon and Sir Patrick Manson in Great Britain; in the United States, members of the Thompson-McFadden Pellagra Commission (notably Joseph F. Siler and Ward J. MacNeal) and others attracted by Sambon's force of argument |
| Supporting data | Pellagra is uncommon among persons with access to a diet varied with meat, milk, and leafy vegetables. If caught early, pellagra responds to treatment that includes a varied diet. | In Italy, according to Sambon, pellagra occurs mainly along the banks of fast-flowing streams teeming with Simulium larvae. A few Americans confirm this observation. |
| Opposing data | Pellagra sometimes occurs in persons with access to a varied diet; it also occurs in persons who never eat corn. Studies by the Illinois Pellagra Commission and the Thompson-McFadden Pellagra Commission point away from dietary deficiency. | Pellagra in the United States often occurs in closed institutions and places remote from fast-flowing streams. No causative organism has been convincingly demonstrated despite claims made for numerous bacteria, fungi, and parasites. |
To assert that Goldberger did not choose the dietary-deficiency hypothesis during an “aha moment” by no means belittles his accomplishments. He designed and carried out the crucial experiments solidifying the case for diet beyond a reasonable doubt. He came close to identifying the essential dietary component. He made practical recommendations and, just before he died, identified in brewer's yeast a cost-effective therapeutic and preventative measure. Goldberger, a steady and careful researcher, turned a hypothesis (a reasonable idea) into a theory (an idea that accounts for the known facts to a reasonable degree of certainty).
On October 21−22, 1915, the third and final triennial conference of the National Association for the Study of Pellagra took place at the South Carolina State Hospital for the Insane, again organized by Babcock. During the conference the news broke that Goldberger had prevented pellagra by changing the diet, while keeping all other conditions the same, at two Mississippi orphanages and on two wards of the Milledgeville, Georgia, asylum (63). Ward MacNeal, spokesperson for the Thompson-McFadden Commission and American champion of the insect-vector hypothesis, emerged as Goldberger's leading scientific opponent. MacNeal was stung by criticisms levied by Goldberger and others that his methods of data analysis were seriously flawed. Joining MacNeal were southern health officials, led by South Carolina's bombastic and highly-opinionated James Adams Hayne, and southern politicians who resisted the inconvenient truth that the root cause was regional poverty. The consequences were tragic for thousands of Americans.
Goldberger's opponents had one valid point. Goldberger had shown that pellagra could be prevented by giving inmates of asylums and orphanages what he called “the diet of the well-to-do.” Goldberger and his co-authors asserted in their 1915 paper that society should “improve economic conditions, increase wages, reduce unemployment” and “make the other class of foods” (that is, other than carbohydrates) “cheap and readily accessible” (63). Therein lay the rub, or perhaps the Simulium fly, in the ointment. The scientific challenge was to find a cost-effective alternative to the “diet of the well-to-do.”
Reactions to Goldberger's inconvenient truth continue to fascinate social historians. One calls pellagra “an unappreciated reminder of Southern distinctiveness” (64). Another describes “an epidemic of pride,” an “irrational Southern response … specifically related to the cultural identity and values of the South at this time” (65). A third tells how the discovery of the precise cause of pellagra and the implementation of control measures were delayed by “the conception of the South as the regional Other by Northern interests, a reluctance to acknowledge widespread deprivations in the region by Southern leaders, compounded by inadequate scrutiny of the racial and gender dimensions of the disease” (66). All of this makes good reading, but the scientific dimensions of the opposition to Goldberger are of at least equal importance.
Nicotinic acid and its crystalline structure had been known since 1873, nicotinamide had been synthesized in 1894, and in 1913 Casimir Funk published that one of the three substances he had isolated from the vitamin fraction of yeast “appears to be nicotinic acid” (67). In 1916 Atherton Seidell, a biochemist working at the National Hygienic Laboratory in Washington, DC, formulated a vitamin preparation using brewer's yeast and suggested it be tried in pellagra (68). Also in 1916, a North Carolina veterinarian suggested that “black tongue” in dogs might be a canine analogue for pellagra (69), and the following year two Yale University physiologists reported that a condition in dogs resembling human pellagra could be induced by faulty diet and cured with meat (70). But it was not until 1922 that Goldberger and his colleagues began to publish on canine black tongue (71) and it was not until 1925 that they published definitively on the treatment of canine black tongue and human pellagra with yeast (72,73). What took so long?
The answer seems clear: Goldberger had to disprove the conclusions of the Thompson-McFadden Pellagra Commission, which Goldberger's opponents recited “like a well-worn catechism of faith” (74). MacNeal never conceded. In 1917 he brought out the Thompson-McFadden Pellagra Commission's third and final report, a 454-page tome in which Goldberger is not even mentioned (33). One critic calls this report “the medical fraud of the century,” the centerpiece of the “Great Pellagra Cover-Up of 1916−33, which kept the medical benefit of Goldberger's work on pellagra from the entire nation for two decades” (75). As late as 1922, MacNeal published on “The Infectious Etiology of Pellagra” and in a thinly veiled reference to Goldberger asserted that “even public health officials make serious mistakes” (76). Goldberger had to disprove the Thompson-McFadden Pellagra Commission's conclusions from the Spartanburg County, SC, field studies, and he had to convince the public that pellagra was not infectious. To the first end Goldberger and his colleagues performed elaborate studies—classics for students of public health—that proved his intuitive conviction that the privies were merely surrogate markers of poverty. To the second end he subjected 16 volunteers including himself and his wife to materials from pellagrins. In perhaps his most famous experiment, performed at the South Carolina State Hospital for the Insane, Goldberger took skin scales, urine, and liquid feces from three pellagrins, added wheat flour, rolled the mixture into pill-sized pellets, and swallowed the pellets, feces and all (77). These and other studies enhanced Goldberger's legacy but delayed the demonstration that brewer's yeast was a cost-effective alternative to the “diet of the well-to-do.” Thousands died as a result.
And while the opponents to the inconvenient truth that poverty was the root cause of pellagra could thank Ward MacNeal, their ultimate benefactor was Louis Sambon. On August 30, 1931, Sambon collapsed and died in a Paris café. A colleague wrote in the British Medical Journal that “the world of medicine has lost one of its brightest ornaments” (78). More perceptively the Lancet observed that although his ideas were seldom confirmed he “obtained … considerable support for his views, of the correctness of which he always remained certain” (79). An historian of the London School of Tropical Medicine writes that Sambon's dashing around Europe and the United States claiming he had “proved” pellagra transmission by a Simulium fly seriously damaged his reputation. The same historian adds that Sambon “had all the failings of a minor prophet” (80).
In summary, the early response to pellagra constitutes an underappreciated story in the coming-of-age of American medical science. Never again would the response to a major epidemic fall upon such a ragtag group as the asylum superintendents, practicing physicians, and local health officials who organized conferences, published extensively, and sifted through hypotheses. Never again would the US government's response rely so heavily on a single person, as it did on Joseph Goldberger. And never again would American physicians and scientists be so duped by the likes of Louis Westerna Sambon.
Footnotes
Potential Conflicts of Interest: None disclosed.
DISCUSSION
Billings, Baton Rouge: So when you go into places in Appalachia today do you find that pellagra is still present?
Bryan, Columbia: It's rarely recognized and can be overlooked. I think all of us have probably overlooked the “V” or Casal's necklace in patients who were malnourished and suffering from alcoholism, for example. And rare cases are still seen and reported. We had one at our hospital about 8 or 9 years ago.
Dale, Seattle: Was there a story here of medical journals publishing or not publishing this work? What was the role of reviewers in terms of how the truth was seen in this period before World War I.
Bryan, Columbia: The question if I understand you correctly is, was there a role of adequate peer review? I can't answer that specifically; maybe someone could. But articles on pellagra are published in the Journal of the American Medical Association, for example, and other prestigious journals in addition to numerous state medical journals and so on and so forth. I doubt that the peer review process was what it is today. I have gone through the Index Medicus for the entire period and catalogued all of the articles. Interestingly, there were essentially no articles by what might be called the eastern medical establishment. There were no papers on pellagra as far as I can tell presented at the ACCA except for a case report around 1929, until the story breaks that nicotinamide and nicotinic acid are effective. Sociologists have had a field day with pellagra, and some would look at it as people in the north seeing the south as a regional “other” and neglecting this disease. It does call into question the extent to which a disease of this magnitude was overlooked by the medical establishment. But on the other hand, the American research apparatus that we are now so familiar with and accustomed to and bask in — particularly a forum such as this and as exemplified by the previous speaker — was simply nonexistent. The National Hygienic Laboratory in Washington, DC, our predecessor of today's NIH, had done studies in pellagra. The paper to which I alluded by Goldberger was co-authored with John Anderson, the director of Hygienic Laboratory. They were the first to attempt pellagra studies in primates; to transfer pellagra from humans to monkeys. That paper is often overlooked. There were studies — and they were good studies — done by researchers in Chicago and so on and so forth; studies in the Journal of Infectious Diseases, for example.
Schuster, New York: You describe really a problem of a concealed variable which continues to plague observational epidemiological studies. I wonder what the timing is between the work you describe here and the appreciation for the design of proper observational epidemiological studies and the concept of a concealed variable. Do those two intersect? Was this important in the epidemiologist coming to understand the concept? What's the entanglement there, if any?
Bryan, Columbia: I have just recently published a book on this. It's a biography of Babcock and the history of pellagra during this era. I point out that today's appreciation for properly designed studies was simply nonexistent: the randomized prospective double-blind study that many would date to the streptomycin trials of 1948. I think that many people were reluctant to accept Goldberger's demonstrations at two Mississippi orphanages and on two wards in the Milledgeville, Georgia, asylum for exactly that reason. There were so many studies out there and both the Illinois Pellagra Commission and the Thompson-McFadden Pellagra Commission had concluded that diet was not the operative cause. So this issue immediately polarized people and there was no agreement. Goldberger also conducted human experiments — so called Rankin State Prison Farm experiments — in Mississippi which are a little bit controversial from the ethical perspective. But those studies as well — although he tried to control the variables — were confounded by the fact that he kept the prisoners indoors and out of sunlight in order to prevent them from getting mosquito bitten outside of that environment. He also gave them a small amount of coffee, which has been shown to contain niacin. It was correctly pointed out that the scrotal rash which was unusual might not really represent pellagra and indeed was probably due to riboflavin, vitamin B2, deficiency. So there were confounding variables and multivariate regression analysis, of course, was nonexistent.
REFERENCES
- 1.Kraut AM. Goldberger's War: The Life and Work of a Public Health Crusader. New York, NY: Hill and Wang; 2003. pp. 242–243. [Google Scholar]
- 2.Osler W. The Principles and Practice of Medicine. Sixth edition. New York, NY: D. Appleton Company; 1907. p. 384. [Google Scholar]
- 3.Searcy GH. An epidemic of acute pellagra. JAMA. 1907;49:37–8. [Google Scholar]
- 4.Ray WW, Taylor JH, Babcock J, et al. What are pellagra and pellagrous insanity? Does such a disease exist in South Carolina, and what are its causes? An inquiry and a preliminary report to the South Carolina State Board of Health. J SC Med Assoc. 1908;4:64–76. [Google Scholar]
- 5.Babcock JW. The diagnosis and treatment of pellagra. J SC Med Assoc. 1908;4:563–7. [Google Scholar]
- 6.Notes and comment. Am J Insanity. 1908;65:377–84. [Google Scholar]
- 7.BMJ. 1918;1:273. F. M. Sandwith, C.M.G., M.D., F.R.C.P. [Google Scholar]
- 8.Lancet. 1918;1:347–8. Fleming Mant Sandwith, M.D. DURH., F.R.C.P. LOND., C.M.G. [Google Scholar]
- 9.The late Colonel F. M. Sandwith. Lancet. 1918;1:754. [Google Scholar]
- 10.Livingstone DN. Tropical climate and moral hygiene: the anatomy of a Victorian debate. Br J Hist Sci. 1999;32:93–110. doi: 10.1017/s0007087498003501. [DOI] [PubMed] [Google Scholar]
- 11.Wilkinson L. AJE Terzi and LW Sambon: early Italian influences on Patrick Manson's “Tropical Medicine,” Entomology, and the Art of Entomological Illustration in London. Med Hist. 2002;46:569–79. [PMC free article] [PubMed] [Google Scholar]
- 12.Manson-Bahr-Bahr P. History of the School of Tropical Medicine in London (1899–1949) London: H. K. Lewis; 1956. pp. 132–6. [Google Scholar]
- 13.Sambon LW, Low GC. Reports on two experiments on the mosquito-malaria theory, instituted by the Colonial Office and the London School of Tropical Medicine. Med Chir Trans. 1901;84:497–552. [PMC free article] [PubMed] [Google Scholar]
- 14.Sambon LW. The elucidation of sleeping sickness. J Trop Med Hyg. 1904;7:61–3. 68–74, 87–91. [PMC free article] [PubMed] [Google Scholar]
- 15.Cook GC. Patrick Manson (1844–1922) FRS: Filaria (Mansonella) perstans and sleeping sickness (African trypanosomiasis) J Med Biogr. 2012;20:69–70. doi: 10.1258/jmb.2010.010051. [DOI] [PubMed] [Google Scholar]
- 16.Anonymous. The importance of rational inductive methods in advancing knowledge. J Trop Med Hyg. 1908;11:41–2. [Google Scholar]
- 17.Manson P, Rost ER, Sambon LW, et al. A discussion on beri-beri. BMJ. 1902;2:830–9. [Google Scholar]
- 18.Sambon LW. Remarks on the geographical distribution and etiology of pellagra. BMJ. 1905;2:1272–5. [Google Scholar]
- 19.Conference on Pellagra Held under the Auspices of the State Board of Health of South Carolina at the State Hospital for the Insane; October 29th, 1908; Columbia, SC: State. 1909. [Google Scholar]
- 20.Babcock JW. The diagnosis and treatment of pellagra. J SC Med Assoc. 1908;4:563–7. [Google Scholar]
- 21.Claude H. College Park, Maryland: National Archives and Records Administration; Lavinder to the Surgeon General [Walter Wyman], November 24, 1908, Pellagra files of the U.S. Public Health Service, record group 90, file 1648, box 148. [Google Scholar]
- 22.Lavinder CH, Williams CF, Babcock JW. The prevalence of pellagra in the United States—a statistical and geographical note, with bibliography. Public Health Rep. 1909;24:849–52. [Google Scholar]
- 23.The conference on pellagra. JAMA. 1909;53:1645–6. [Google Scholar]
- 24.Transactions of the National Conference on Pellagra Held Under Auspices of South Carolina State Board of Health at the State Hospital for the Insane; November 3 and 4, 1909; Columbia, S.C.. 1910. Columbia, SC: State. [Google Scholar]
- 25.Goldberger J. The etiology of pellagra. The significance of certain epidemiological observations with respect thereto. Public Health Rep. 1914;29:1683–6. [Google Scholar]
- 26.Marie A. In: Pellagra. Lavinder C. H., Babcock J. W., translators. Columbia, SC: State; 1910. [Google Scholar]
- 27.Niles GM. Pellagra: An American Problem. Philadelphia, PA: W.B. Saunders; 1912. [Google Scholar]
- 28.Wood EJ. A Treatise on Pellagra for the General Practitioner. New York, NY: D. Appleton; 1912. [Google Scholar]
- 29.Roberts SR. Pellagra: History, Distribution, Diagnosis, Prognosis, Treatment, Etiology. St. Louis, MO: C.V. Mosby; 1913. [Google Scholar]
- 30.Report of the Pellagra Commission of the State of Illinois, November, 1911. Springfield, IL: Illinois State Journal; 1912. [Google Scholar]
- 31.Siler JF, Garrison PE, MacNeal WJ. Pellagra. First Progress Report of the Thompson McFadden Pellagra Commission of the New York Post-Graduate Medical School and Hospital. (n.p., 1913) [Google Scholar]
- 32.Siler JF, Garrison PE, MacNeal WJ. Pellagra II. Second Progress Report of the Thompson-McFadden Commission of the New York Post-Graduate Medical School and Hospital. (n.p, 1915) [Google Scholar]
- 33.Siler JF, Garrison PE, MacNeal WJ. Pellagra III. Third Report of the Robert M. Thompson Pellagra Commission of the New York Post-Graduate Medical School and Hospitaly. (n.p., 1917) [Google Scholar]
- 34.Funk C. The etiology of the deficiency diseases, beri-beri, polyneuritis in birds, epidemic dropsy, scurvy, experimental scurvy in animals, infantile scurvy, ship beri-beri, pellagra. J State Med. 1912;20:341–68. [Google Scholar]
- 35.Harrow B. Casimir Funk: Pioneer in Vitamins and Hormones. New York, NY: Dodd, Mead; 1955. pp. 46–7. [Google Scholar]
- 36.Blue R. The problem of pellagra in the United States. Transactions of the National Association for the Study of Pellagra. Second Triennial Meeting at Columbia; October 3 and 4, 1912; South Carolina. Columbia, SC: R.L. Bryan; 1914. pp. 1–7. [Google Scholar]
- 37.Sandwith F. Can pellagra be a disease due to deficiency in nutrition?. Transactions of the National Association for the Study of Pellagra. Second Triennial Meeting at Columbia; October 3 and 4, 1912; South Carolina. Columbia, SC: R.L. Bryan; 1914. pp. 97–100. [Google Scholar]
- 38.Columbia, SC: South Caroliniana Library, University of South Carolina; 1912. Aug 4, James Woods Babcock papers, box 8, folder 10. F. M. Sandwith to J. W. Babcock. [Google Scholar]
- 39.Sambon LW. Special points of epidemiological interest in pellagra. Transactions of the National Association for the Study of Pellagra. Second Triennial Meeting at Columbia; October 3 and 4, 1912; South Carolina. Columbia, SC: R.L. Bryan; 1914. pp. 81–96. [Google Scholar]
- 40.Tucker BR. The nervous and mental symptoms of pellagra. Transactions of the Forty-Third Annual Session of the Medical Society of Virginia held in Norfolk; October 22–25, 1912; Richmond, VA: Richmond Press; 1913. pp. 167–70. [Google Scholar]
- 41.Carl L. Columbia, SC: South Caroliniana Library, University of South Carolina; Alsberg to J. W. Babcock, October 23, 1912. James Woods Babcock papers, box 7, folder 10. [Google Scholar]
- 42.Sandwith FM. Is pellagra a disease due to deficiency in nutrition? Trans R Soc Trop Med Hyg. 1913;6:143–8. [Google Scholar]
- 43.Prof. Louis Sambon here. Comes from London to address Southern Pellagra Conference. New York Times. 1913 Sep 1; [Google Scholar]
- 44.Insect carries pellagra. English scientist says Spartanburg conference established this. New York Times. 1913 Sep 13; [Google Scholar]
- 45.Pellagra is not transmissible by direct contact. Spartanburg (SC) Herald. 1913 Sep 4; [Google Scholar]
- 46.Pellagra discussed by eminent doctors; its cause a mystery. Greenville (SC) Daily News. 1913 Sep 4; [Google Scholar]
- 47.Wilson R. Discussion of Hayne JA. The history of pellagra in South Carolina. J SC Med Assoc. 1932;28:205–9. [Google Scholar]
- 48.Notes on Barbadoes [1914] College Park, Maryland: National Archives and Records Administration; Pellagra files of the U.S. Public Health Service, record group 90, file 1648, box 149. [Google Scholar]
- 49.No buffalo gnats but finds pellagra. The State (Columbia, SC) 1913 Nov 15; [Google Scholar]
- 50.Buffalo gnat is no carrier of pellagra. Columbia (SC) Record. 1913 Nov 16; [Google Scholar]
- 51.Columbia, SC: South Caroliniana Library, University of South Carolina; 1914. Apr 18, James Woods Babcock papers, box 8, folder 4. J. F. Siler to J. W. Babcock. [Google Scholar]
- 52.Lavinder CH. The prevalence and geographical distribution of pellagra in the United States. Public Health Rep. 1912;27:2076–88. [Google Scholar]
- 53.Columbia, SC: South Caroliniana Library, University of South Carolina; 1912. May 8, James Woods Babcock papers, box 8, folder 9. C. H. Lavinder to J. W. Babcock. [Google Scholar]
- 54.Lavinder CH, Francis E, Grimm RM, et al. Attempts to transmit pellagra to monkeys. JAMA. 1914;63:1093–4. [Google Scholar]
- 55.Chapel Hill, NC: Southern Historical Collection, Wilson Library, University of North Carolina; 1914. Feb 7, Joseph Goldberger papers, box 1641, folder 16. Rupert Blue to Joseph Goldberger. [Google Scholar]
- 56.Chapel Hill, NC: Southern Historical Collection, Wilson Library, University of North Carolina; 1914. Feb 17, Joseph Goldberger papers, box 1641, folder 16. Rupert Blue to Joseph Goldberger. [Google Scholar]
- 57.Parsons RP. Trail to Light. A Biography of Joseph Goldberger. Indianapolis, IN: Bobbs-Merrill; 1943. p. 280. [Google Scholar]
- 58.Elmore JG, Feinstein AR. Joseph Goldberger: an unsung hero of American clinical epidemiology. Ann Intern Med. 1994;121:372–5. doi: 10.7326/0003-4819-121-5-199409010-00010. [DOI] [PubMed] [Google Scholar]
- 59.Frankenburg FR. Vitamin Discoveries and Disasters: History, Science, and Controversies. Santa Barbara, CA: Praeger; 2009. p. 40. [Google Scholar]
- 60.Anderson JF, Goldberger J. An attempt to infect the rhesus monkey with blood and spinal fluid from pellagrins. Public Health Rep. 1911;26:1003–4. [Google Scholar]
- 61.Terris M. Goldberger on Pellagra. Baton Rouge, LA: Louisiana State University Press; 1964. [Google Scholar]
- 62.Blue R. Pellagra in California. Cal State J Med. 1910;8:101–2. [PMC free article] [PubMed] [Google Scholar]
- 63.Goldberger J, Waring CH, Willets DG. The prevention of pellagra: a test of diet among institutional inmates. Public Health Rep. 1915;30:3117–31. [Google Scholar]
- 64.Etheridge EW. Pellagra: An unappreciated reminder of Southern distinctiveness. In: Savitt TL, Young JH, editors. Disease and Distinctiveness in the American South. Knoxville, TN: University of Tennessee Press; 1988. pp. 100–19. [Google Scholar]
- 65.Crabb MK. An epidemic of pride: pellagra and the culture of the American South. Anthropologica. 1992;34:89–103. [Google Scholar]
- 66.Chacko E. Understanding the geography of pellagra in the United States: the role of social and place-based identities. Gend Place Cult. 2005;12:197–212. [Google Scholar]
- 67.Funk C. Studies on beri-beri VII. Chemistry of the vitamine-fraction from yeast and rice polishing. J Physiol. 1913;47:389–92. doi: 10.1113/jphysiol.1913.sp001585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Seidell A. A stable form of vitamine, efficient in the preparation and cure of certain nutritional deficiency diseases. Public Health Rep. 1916;31:364–70. [Google Scholar]
- 69.Spencer TN. Is “black tongue” in dogs pellagra? Am J Vet Med. 1916;11:325. [Google Scholar]
- 70.Chittenden RH, Underhill FP. The production in dogs of a pathological condition which closely resembles human pellagra. Am J Physiol. 1917;44:13–6. doi: 10.1073/pnas.3.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wheeler GA, Goldberger J, Blackstock MR. On the probable identity of the Chittenden-Underhill pellagralike syndrome in dogs and “black tongue.”. Public Health Rep. 1922;37:1063–9. [Google Scholar]
- 72.Goldberger J, Tanner WF. A study of the pellagra-preventive action of dried beans, casein, dried milk, and brewers' yeast, with a consideration of the essential factors involved. Public Health Rep. 1922;40:54–80. [Google Scholar]
- 73.Goldberger J, Wheeler GA, Tanner WF. Yeast in the treatment of pellagra and black tongue. A note on dosage and mode of administration. Public Health Rep. 1925;40:927–8. [Google Scholar]
- 74.Flannery MA. Fighting pellagra in Alabama: Carl A. Grote's forgotten contribution to conquering a southern scourge. [Accessed September 27, 2014]. Available at: http://contentdm.mhsl.uab,edu/u?PELLAGRA,13.
- 75.Chase A. The Legacy of Malthus: The Social Costs of the New Scientific Racism. Urbana: University of Illinois Press; 1980. A few false correlations = a few million real deaths: Scientific racism prevails over scientific truth. In Chase A; pp. 201–225. [Google Scholar]
- 76.MacNeal WJ. The infectious etiology of pellagra. South Med J. 1922;15:899–902. [Google Scholar]
- 77.Goldberger J. The transmissibility of pellagra. Experimental attempts at transmission to the human subject. Public Health Rep. 1916;31:3159–73. doi: 10.1111/j.1753-4887.1973.tb05173.x. [DOI] [PubMed] [Google Scholar]
- 78.Louis Sambon, M.D. BMJ. 1931;2:514–5. [PMC free article] [PubMed] [Google Scholar]
- 79.Louis Sambon, M.D., Naples. Lancet. 1931;2:613. [Google Scholar]
- 80.Manson-Bahr P. History of the School of Tropical Medicine in London (1899–1949) London, UK: H. K. Lewis; 1956. pp. 132–6. [Google Scholar]


