Abstract
Objective
To describe the dispatch process for out-of-hospital cardiac arrest (OHCA) in bystander-witnessed patients with initial shockable rhythm, and to evaluate whether recognition of OHCA by the emergency medical dispatcher (EMD) has an effect on the outcome.
Methods
This study was part of the FINNRESUSCI study focusing on the epidemiology and outcome of OHCA in Finland. Witnessed [not by Emergency Medical Service (EMS)] OHCA patients with initial shockable rhythm in the southern and the eastern parts of Finland during a 6-month period from March 1 to August 31 2010, were electronically collected from eight dispatch centres and from paper case reports filled out by EMS crews.
Results
Of the 164 patients, 82.3% (n=135) were correctly recognized by the EMD as cardiac arrests. The majority of all calls (90.7%) were dispatched within 2 min. Patients were more likely to survive and be discharged from the hospital if the EMS response time was within 8 min (P<0.001). Telephone-guided cardiopulmonary resuscitation (T-CPR) was given in 53 cases (32.3%). Overall survival to hospital discharge was 43.4% (n=71). Survival to hospital discharge was 44.4% (n=60) when the EMD recognized OHCA and 37.9% (n=11) when OHCA was not recognized. The difference was not statistically significant (P=0.521).
Conclusion
The rate of recognition of cardiac arrest by EMD was high, but EMD recognition did not affect the outcome. The survival rate was high in both groups. Recognized cardiac arrest patients received bystander CPR more frequently than those for whom OHCA remained unrecognized.
Keywords: dispatch, emergency medical dispatcher, emergency medical service, out-of-hospital cardiac arrest
Introduction
Emergency Medical Service (EMS) systems annually encounter about 275 000 out-of-hospital cardiac arrest (OHCA) patients in Europe 1. Survival rates have been reported to be poor – ∼10% of cases survive to hospital discharge 2. Early recognition and EMS activation by the dispatch centre is the first link in the chain of survival 2–4. When processing emergency telephone calls, the emergency medical dispatcher (EMD) has to decide whether there is a medical emergency, find out the chief complaint/current state and/or rapidly identify cardiac arrest and prioritize and define an EMS response. The ability to recognize OHCA is a challenging task, but still the capacity to identify OHCA patients has been reported to be as high as 70–83% 5–7.
In cases of OHCA, the dispatcher can and should give telephone-guided cardiopulmonary resuscitation (T-CPR) instructions to the caller 4. It has previously been shown that bystander CPR improves the survival rates of OHCA patients, especially when started at an early stage 8. A similar improvement in outcome has been shown when evaluating the effects of T-CPR if the identification of OHCA is made correctly 2,3,6,9, but evidence of this is not clear 10.
To report OHCA uniformly, Utstein-style definitions and reporting templates have been used widely since 1991 11. However, these templates have not included the role of the EMD. It is suggested that dispatching centre variables should be included when reporting OHCA variables to compare results and improve the quality of the whole EMS system 12. There are few previous reports concerning the dispatch process with dispatch response times for OHCA 6,13,14.
Patients who suffer a witnessed cardiac arrest, receive bystander CPR and who initially have a shockable rhythm have the best chances to survive OHCA 15–18. EMS reaching the patient within a short window of time is also imperative for survival.
The aim of this study was to describe and report the dispatch process in bystander (not EMS)-witnessed OHCA with initial shockable rhythm, and to determine whether recognition of cardiac arrest by the EMD affects the outcome of these patients.
Methods
This study was a prospective observational cohort study conducted in southern and eastern Finland from 1 March 2010 to 31 August 2010. It includes data on all patients in the study areas who at dispatch fulfilled the criteria of suspected OHCA according to the national uniform emergency medical dispatch guidelines. Furthermore, all patients who developed OHCA before hospital admission were included. Further analyses were conducted on patients who experienced witnessed (not EMS) OHCA with initial shockable rhythm to minimize other confounding factors of survival. The overall population in the study area was 2 644 200 (49.1% of the total Finnish population).
The Finnish dispatcher training involves 1.5 years of formal education in emergency-telephone-call processing and dispatching. Eight regional dispatch centres are located within the study area, accessed through the common emergency number ‘112’. These dispatch centres are combined centres for EMS, police and fire and rescue services, and they are connected to a common database. Time points are registered automatically: the beginning of the emergency telephone calls, the dispatch of the first response unit and the time when the first unit is on scene. Medical call processing and medical priority criteria are described in the dispatcher’s guidebook and are based on the patient’s chief complaint (e.g. chest pain) and on the patient’s current condition (e.g. awake or not). EMS calls are prioritized into four categories from A to D, where A represents the highest medical priority. The dispatcher should quickly identify the site or the address of the emergency. To exclude cardiac arrest, the dispatcher initially verifies the patient’s consciousness (is the patient awake? What is he/she doing right now?) and the presence of breathing (is he/she breathing normally?). If the answer to both questions is ‘no’, the dispatcher continues processing the call as a cardiac arrest call and uses a tiered response strategy to alert the closest and the most appropriate EMS units to the scene. The dispatcher starts to give T-CPR instructions, unless CPR is already going on or the caller says he or she knows how to administer CPR. Since the year 2000, the T-CPR instructions have included only chest compressions unless the victim is a child or OHCA is probably due to drowning or choking 4,19.
Tieto Oy Ltd (http://www.intensium.com/web/english) has provided a uniform, common database to link the dispatch data to the data that were obtained from dedicated paper case reports (CRFs) submitted by the EMS crews that treated the patients. Information on the beginning of the emergency call, dispatch and scene times, priority categories and dispatched units were electronically transferred from the dispatch centres to this database. The CRFs were faxed to a research nurse who entered the data into this database and linked them to the dispatch data. Data of bystander CPR were collected by the EMS paramedics who were asked to report whether there was ongoing bystander CPR at arrival on the scene and whether it was based on dispatcher guidance or not. The principal investigator received information about the patient’s status at the time of hospital discharge from the National Institute for Health and Welfare (discharged home or discharged to another facility).
Data regarding OHCA survival at 1 year was obtained from The Finnish Population Information System, which is a computerized national registry containing basic data about persons residing permanently in Finland.
The Cerebral Performance Category (CPC) status of survivors was evaluated at 6 months after the OHCA by a neurologist (M.T.) who called the patients or their close relatives. The Institutional Review Board of the Helsinki University Central Hospital approved the study protocol.
Data were analysed using SPSS, version 18.0 (SPSS Inc., Chicago, Illinois, USA). Data were presented as medians with IQR or as frequencies and percentages. The association between categorical variables was assessed using cross tabulation and the χ2-test. A P-value less than 0.05 was considered statistically significant. A logistic regression model was used to determine factors related to survival at 1 year.
Results
The dispatch centres received 885 338 emergency telephone calls during the 6-month study period. Of these, 237 295 were medical (26.8% of all telephone calls), leading to 186 420 EMS missions (78.6% of all medical telephone calls) (Fig. 1).
Fig. 1.
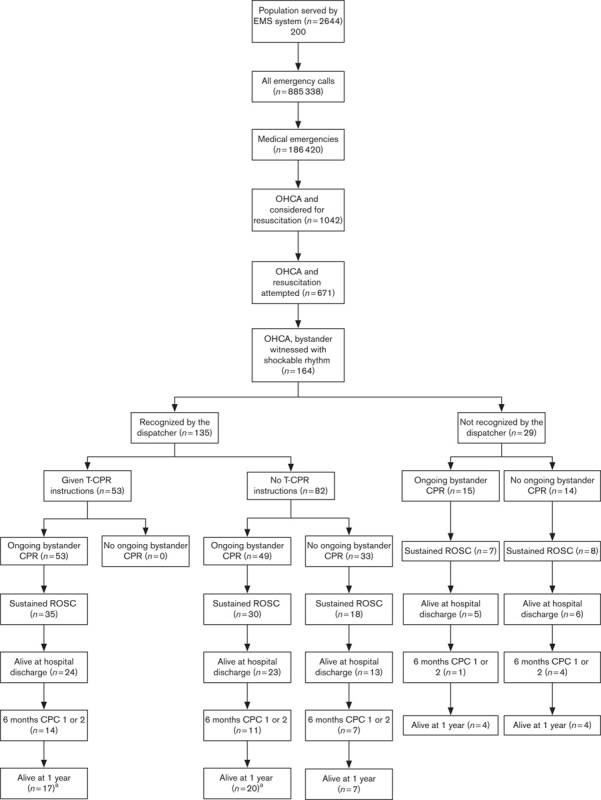
The study flow chart. aSurvival after 1 year could not be established in two patients who were discharged alive from hospital to their home countries. CPC, Cerebral Performance Category; EMS, Emergency Medical Service; OHCA, out-of-hospital cardiac arrest; ROSC, return of spontaneous circulation; T-CPR, telephone-guided cardiopulmonary resuscitation.
The EMS crews considered resuscitation for 1042 patients (0.56% of all EMS missions), and resuscitation was eventually attempted in 671 patients. Of these, 164 patients had suffered bystander-witnessed OHCA and had a shockable initial cardiac rhythm. The majority of these patients were presumed to have OHCA of cardiac origin (n=140, 85.4%). The OHCA took place mainly in an urban environment (n=109, 66.5%), whereas 15.9 and 17.7% occurred in semi-urban and rural areas, respectively.
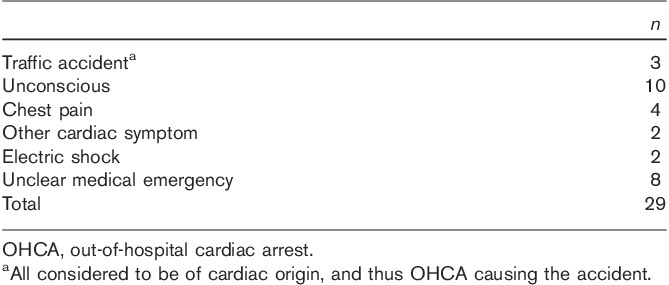
The dispatcher correctly recognized 82.3% (n=135) of the 164 patients with witnessed OCHA and in shockable rhythm during the emergency telephone call as cardiac arrests. Of those not recognized, 29 (17.7%) were primarily dispatched as other high-priority calls, that is, unconscious patient, chest pain or other cardiac symptom (Table 1).
Table 1.
Reasons for dispatching for those not recognized as OHCA by the dispatcher
Data of the dispatch process of the calls were received from 151 of the 164 missions with witnessed OHCA with shockable rhythm. The median time from the beginning of the telephone call to the dispatch of the first EMS unit was one minute (IQR 1–2 min), and for the majority (90.7%) of the calls, dispatch occurred within 2 min. For the survivors at 1 year, the dispatch time was less than 2 min in 30 patients (61.2%) and more than 2 min in 19 patients (38.8%, P=0.345).
Table 2 demonstrates a comparison of the dispatch response, CPR and survival data depending on whether the time from the beginning of the emergency telephone call to EMS arrival on scene was within 8 min or not. When the EMS response time was within 8 min, 53.9% of the patients were alive at hospital discharge, and when the time exceeded 8 min, the survival rate was 30.2% (P<0.001). Although there were twice as many (41.4%) patients alive in 1 year in the less than 8-min group compared with the more than 8-min group (21.0%), this number did not reach statistical significance (P=0.09).
Table 2.
Comparison of the response time within 8 min from the beginning of the emergency call to EMS arrival on the scene and dispatch recognizing OHCA, T-CPR instructions and CPR provided and survival
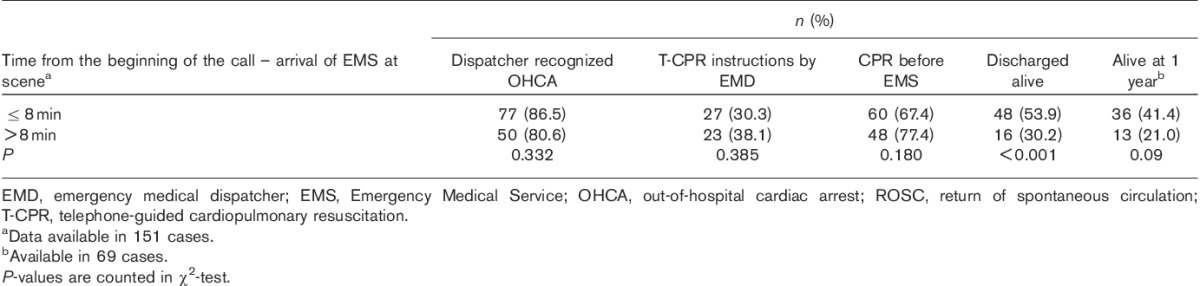
Table 3 shows the sex, dispatching times and outcomes for the OHCA patients with shockable rhythm with or without dispatcher-recognized OHCA. CPR was given more frequently among the patients in whom OHCA was recognized (75.6 vs. 51.7%, P=0.01).
Table 3.
Age, sex, dispatch, EMS response, CPR before EMS, ROSC and survival with CPC recognized as OHCA or not in the dispatch centre
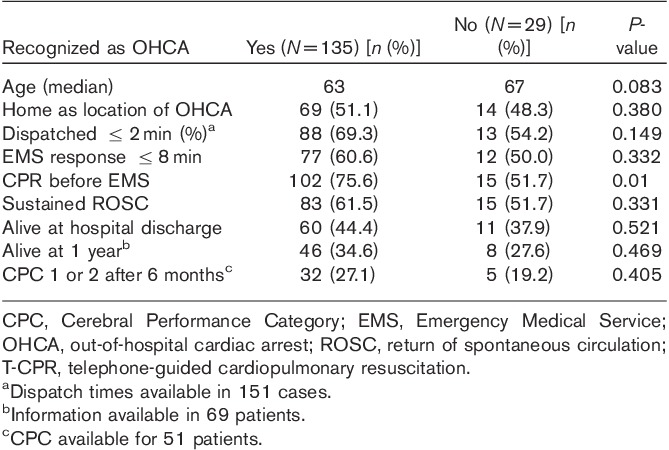
The overall survival to hospital discharge was 43.4% (n=71), and survival at 1 year was 32.9% (n=54). Survival to hospital discharge was 44.4% (n=60) when the dispatcher recognized OHCA and 37.9% (n=11) when it was missed (P=0.521). Survival rates at 1 year were 32.6% (n=44) and 27.6% (n=8), respectively, and there was no difference in the outcome at 1 year whether the OHCA was recognized or not (P=0.469). Of the patients surviving to hospital discharge, data of the CPC status at 6 months were available for 51 patients, and for 37 of these, CPC was 1 or 2.
In all, 117 patients (71.3%) received bystander CPR before EMS arrival, and the survival rates to hospital discharge and the survival at 1 year were 44.4% (n=52) and 35.7% (n=41), respectively. Of the 47 patients not receiving bystander CPR before EMS, survival rates to hospital discharge and at 1 year were 40.4% (n=19) and 27.7% (n=13), respectively. There was no difference in the survival to hospital discharge (P=0.639) or at 1 year (P=0.327) in relation to whether bystander CPR was given or not given before EMS arrival.
T-CPR instructions were given in 53 cases (32.3%). All of these patients received bystander CPR before EMS arrival, and their survival to hospital discharge was 46.6% (n=27).
In the logistic regression analysis, survival rates were higher at 1 year (P=0.018, odds ratio 2.82, 95% confidence interval: 1.19–6.67) if the EMS response was within 8 min. Other variables tested were the type of municipality, whether T-CPR instructions were given, if the emergency call was processed within 2 minutes or not (P=0.077, odds ratio 0.48, 95% CI: 0.21–1.082), whether CPR was given before EMS and whether OHCA was recognized by EMD.
Discussion
First, this study demonstrated that dispatchers in Finland recognize OHCA with high accuracy in the patient group with the best prognosis – witnessed OHCA with shockable initial rhythm. However, in this study, we found that this was not associated with increased survival to hospital discharge. Second, a short response time from the beginning of the emergency telephone call to EMS arrival on the scene was related to better survival for these patients. Third, it seems that a majority of OHCA patients in this subgroup received bystander CPR – a proportion that probably can be increased by T-CPR instructions.
Previous studies have shown a high rate of recognition of OHCA in Finland by dispatchers, who correctly identified 79–83% of OHCA patients 6,7. Our study corroborated these results, showing a high identification rate of OHCA. In a study by Axelsson et al. 20, the recognition rate of OHCA by EMD was only 20%. The reason for such a low recognition rate could have been the national protocol, where the dispatch criteria were symptom-related rather than condition-related (i.e. cardiac arrest). If the dispatcher clearly suspects OHCA and wants to code the call as such, he/she has to create this in a free text rather than just launching the mission with a specific code. Moreover, the study did not describe the EMD training programme or the background of the dispatchers in Sweden. Could the lower rate of recognizing OHCA patients be explained by differences in EMD training?
The Finnish nationwide EMD protocol is based on questions that the dispatcher asks about what has happened and whether the patient is awake and breathing normally (if the patient is not alert or breathing normally, the dispatch code is suspected cardiac arrest) 21. This seems practical and results in a high sensitivity of OHCA recognition. Heward et al. 22 showed a 200% increase in the recognition of cardiac arrest by dispatchers when these three questions were asked. However, in a Finnish study 7, it was shown that the dispatchers adhered to the protocol in only 52.4% of the calls, and still the sensitivity in recognizing OHCA was high: more than 80%. The records of the emergency calls were reviewed, and they revealed that if the OHCA was witnessed, the protocol was followed significantly more often than if it was unwitnessed. This, however, did not lead to an increased rate of correct identification in witnessed compared with unwitnessed OHCA patients. If the protocol was followed, however, the dispatch time of the first response unit was shorter in witnessed OHCAs (median, 71 vs. 91 s, P<0.001), which may have a profound effect on the outcome for these patients.
It seems important that the protocol includes the question of the presence of normal breathing. Berdowski et al. 9 demonstrated that when the OHCA was unrecognized, in 51% of the calls the dispatcher did not ask about the normality of breathing, and if asked, all OHCAs would have been recognized. This commends the use of these important questions recommended by Eisenberg et al. 23. However, it is unrealistic to assume that an EMD could yield 100% detection of cardiac arrest in a real-world setting.
In this study, the unrecognized OHCAs were mostly coded as ‘unconscious’ (n=10), but the EMS was still alerted at highest priority. There were also three traffic accidents that were a consequence of cardiac arrest, and three patients whose cardiac arrests were due to electric shock. In these situations, the dispatcher coded the emergency correctly, although the patient was having a cardiac arrest. This additional information may have been given to EMS by radio.
We found that the recognition of OHCA did not affect the outcome. This may be due to the fact that there was a high recognition rate of OHCAs overall, or that the number of patients was too small to show differences in this setting. CPR was given more frequently to those whose OHCA was recognized by the dispatcher (75.6 vs. 51.7%), P=0.01, but this did not have an impact on the survival. It has been shown in several studies that CPR before EMS increases survival rates two-fold to three-fold 24. Previous reports have also demonstrated the positive effect on the outcome when the dispatcher recognized the OHCA during the emergency call 9,25. Thus, the size of our study group may lack the power to show the effects of bystander CPR or OHCA recognition on the outcome.
Survival to hospital discharge was better for those patients who were reached by EMS within 8 min from the time the emergency call was placed (P<0.001). A short delay from the call to EMS arrival on the scene has been shown to improve the outcome in previous studies when treating OHCA 15,26–28, and thus our results are similar to those reported previously. A time within 480 s (8 min) from alerting EMS to the EMS response to the patient in life-threatening situations is a widely accepted indicator of EMS performance (Cited 30 September 2013 at: www.eed-project.de) and was also used in this study.
This study showed that 32.3% of OHCA patients were given dispatcher T-CPR instructions. In a previous study from Finland by Kuisma et al. 6, this number was 35.5%. In a study from Seoul, South Korea, this number was 24.2%, with only 5.2% of the patients actually receiving CPR 29. In another study, about one-third of OHCA bystanders received T-CPR instructions 30. In our study, the overall number of patients receiving bystander CPR was 71.3%. According to the Finnish dispatcher protocol, the dispatcher does not give T-CPR instructions if the caller says that he/she knows how to perform CPR, or if CPR is already being administered. Guidelines exist for giving appropriate T-CPR instructions 31.
There are some limitations to be considered in this study. The quality of bystander CPR was not evaluated, and we received the information on whether or not T-CPR was administered from the paramedics, and not from the dispatch centre. This lack of quality of T-CPR data may have caused bias in the data when evaluating the effectiveness of T-CPR to the outcome. It has been previously demonstrated that CPR provided by bystanders may be insufficient 30.
Time points regarding the dispatch process were registered in minutes and not in seconds, which reduced the accuracy of the dispatching times. Data on these times were missing in 13 cases. Records of the conversation between the caller and the dispatcher were not collected. These data would have made it possible for researchers to evaluate the dispatching process thoroughly and analyse the unidentified OHCA emergency calls and the protocol used by dispatchers during the call.
The small size of the study group might lack the power to show statistical differences in outcomes. However, as shown in Table 3, there are fewer survivors (return of spontaneous circulation, to hospital discharge and at 1 year) if OHCA is not recognized. This suggests that the correct recognition of cardiac arrest may further increase the chances of survival, a result that could be shown more clearly in a larger study group and with a longer follow-up.
Conclusion
This study showed a high rate of recognition of OHCA by dispatchers in Finland, probably due to the national EMD protocol and trained dispatchers. This did not, however, have an effect on the outcome in patients with witnessed cardiac arrest and initial shockable rhythm. If the time of the beginning of the emergency call to EMS arrival at the patient’s side was within 8 min, the patients were more likely to be alive at hospital discharge. Bystander CPR was given more often if the dispatcher recognized the cardiac arrest. However, this did not influence the patient outcome in this study.
Acknowledgements
The authors thank Elina Halonen, Sari Rahikainen, Saija Rissanen, Nina Nakari and Jani Ikonen for their help with data collection. They also thank all the paramedics, nurses and doctors for their efforts in this study, and the Foundation of Emergency Medicine and Finska Läkaresällskapet Foundation for the financial support. For the FINNRESUSCI Prehospital Study Group: James Boyd, EMS, Department of Anaesthesia and ICM, Helsinki University Central Hospital, Helsinki, Finland; Tero Varpula, Department of Intensive Care, Helsinki University Central Hospital, Helsinki, Finland; Tuomas Oksanen, Department of Intensive Care, Helsinki University Central Hospital, Helsinki, Finland; Janne Virta, FinnHEMS, Vantaa, Finland; Teuvo Määttä, EMS, Department of Anaesthesia and ICM, Helsinki University Central Hospital, Helsinki, Finland; Mikko Lintu, Department of Emergency Care, Central Finland Central Hospital Jyvaskyla, Finland; Susanna Wilen, Emergency Department, North Carelia Central Hospital, Joensuu, Finland; Kari Pullinen, Department of Anesthesia, Savonlinna Central Hospital, Savonlinna, Finland; Heikki Laine, Department of Anesthesia and Intensive Care, Mikkeli Central Hospital, Mikkeli, Finland; Hetti Kirves, Hyvinkää, EMS, Helsinki and Uusimaa District, Hyvinkää, Finland; Jarmo Lehtonen, Turku University Hospital, Turku, Finland; Petri Loikas, Kymenlaakso Social and Health Services, Kotka, Finland; Tom Löfstedt, Länsi-Uusimaa, EMS, Helsinki and Uusimaa hospital district, Raasepori, Finland; Ulla Martin, MD; Porvoo Hospital, Helsinki and Uusimaa Hospital District, Porvoo, Finland. Heimo Niemelä, South Karelia District of Social and Health Services, Lappeenranta, Finland; Arto Tennilä, Jorvi EMS, Helsinki University Hospital, Espoo, Finland; Juha Valli, Hyvinkää Hospital, Helsinki and Uusimaa Hospital District, Hyvinkää, Finland.
This study was supported by the EVO funding of Kuopio University Hospital, by the Foundation of Emergency Medicine, by the Finska Läkaresällskapet Foundation and by the Päivikki and Sakari Sohlberg Foundation. The study sponsors had no involvement in the study design, in the collection, analysis and interpretation of data, in the writing of the manuscript or in the decision to submit the manuscript for publication.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Atwood C, Eisenberg MS, Herlitz J, Rea TD. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation 2005; 67:75–80. [DOI] [PubMed] [Google Scholar]
- 2.Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 2010; 81:1479–1487. [DOI] [PubMed] [Google Scholar]
- 3.Bobrow BJ, Panczyk M, Subido C. Dispatch-assisted cardiopulmonary resuscitation: the anchor link in the chain of survival. Curr Opin Crit Care 2012; 18:228–233. [DOI] [PubMed] [Google Scholar]
- 4.Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation 2010; 81:1219–1276. [DOI] [PubMed] [Google Scholar]
- 5.Garza AG, Gratton MC, Chen JJ, Carlson B. The accuracy of predicting cardiac arrest by emergency medical services dispatchers: the calling party effect. Acad Emerg Med 2003; 10:955–960. [DOI] [PubMed] [Google Scholar]
- 6.Kuisma M, Boyd J, Vayrynen T, Repo J, Nousila-Wiik M, Holmstrom P. Emergency call processing and survival from out-of-hospital ventricular fibrillation. Resuscitation 2005; 67:89–93. [DOI] [PubMed] [Google Scholar]
- 7.Nurmi J, Pettila V, Biber B, Kuisma M, Komulainen R, Castren M. Effect of protocol compliance to cardiac arrest identification by emergency medical dispatchers. Resuscitation 2006; 70:463–469. [DOI] [PubMed] [Google Scholar]
- 8.Holmberg M, Holmberg S, Herlitz J. Swedish Cardiac Arrest Registry. Factors modifying the effect of bystander cardiopulmonary resuscitation on survival in out-of-hospital cardiac arrest patients in Sweden. Eur Heart J 2001; 22:511–519. [DOI] [PubMed] [Google Scholar]
- 9.Berdowski J, Beekhuis F, Zwinderman AH, Tijssen JG, Koster RW. Importance of the first link: description and recognition of an out-of-hospital cardiac arrest in an emergency call. Circulation 2009; 119:2096–2102. [DOI] [PubMed] [Google Scholar]
- 10.Bohm K, Vaillancourt C, Charette ML, Dunford J, Castren M. In patients with out-of-hospital cardiac arrest, does the provision of dispatch cardiopulmonary resuscitation instructions as opposed to no instructions improve outcome: a systematic review of the literature. Resuscitation 2011; 82:1490–1495. [DOI] [PubMed] [Google Scholar]
- 11.Chamberlain D, Cummins R, Abramson N, Allen M, Baskett P, Becker L. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the ‘Utstein style’. Prepared by a Task Force of Representatives from the European Resuscitation Council, American Heart Association, Heart and Stroke Foundation of Canada, Australian Resuscitation Council. Resuscitation 1991; 22:1–26. [PubMed] [Google Scholar]
- 12.Castren M, Bohm K, Kvam AM, Bovim E, Christensen EF, Steen-Hansen JE, et al. Reporting of data from out-of-hospital cardiac arrest has to involve emergency medical dispatching – taking the recommendations on reporting OHCA the Utstein style a step further. Resuscitation 2011; 82:1496–1500. [DOI] [PubMed] [Google Scholar]
- 13.Morici N, De Luca G, Lucenteforte E, Chatenoud L, Fontana G, La Vecchia C, et al. Emergency Medical System response to out-of-hospital cardiac arrest in Milan, Italy. Eur J Emerg Med 2010; 17:234–236. [DOI] [PubMed] [Google Scholar]
- 14.Weiser C, van Tulder R, Stockl M, Schober A, Herkner H, Chwojka CC, et al. Dispatchers impression plus Medical Priority Dispatch System reduced dispatch centre times in cases of out of hospital cardiac arrest. Pre-alert – a prospective, cluster randomized trial. Resuscitation 2013; 84:883–888. [DOI] [PubMed] [Google Scholar]
- 15.Kuisma M, Maatta T. Out-of-hospital cardiac arrests in Helsinki: Utstein style reporting. Heart 1996; 76:18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA 2008; 300:1423–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vaahersalo J, Hiltunen P, Tiainen M, Oksanen T, Kaukonen KM, Kurola J, et al. Therapeutic hypothermia after out-of-hospital cardiac arrest in Finnish intensive care units: the FINNRESUSCI study. Intensive Care Med 2013; 39:826–837. [DOI] [PubMed] [Google Scholar]
- 18.Hiltunen P, Kuisma M, Silfvast T, Rutanen J, Vaahersalo J, Kurola J, et al. Regional variation and outcome of out-of-hospital cardiac arrest (ohca) in Finland – the Finnresusci study. Scand J Trauma Resusc Emerg Med 2012; 20:80–7241-20-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Part 3: adult basic life support. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation. Circulation 2000; 102:I22–I59. [PubMed] [Google Scholar]
- 20.Axelsson C, Borgstrom J, Karlsson T, Axelsson AB, Herlitz J. Dispatch codes of out-of-hospital cardiac arrest should be diagnosis related rather than symptom related. Eur J Emerg Med 2010; 17:265–269. [DOI] [PubMed] [Google Scholar]
- 21.Clawson JJ, Martin RL, Hauert SA. Protocols vs. guidelines. Choosing a medical-dispatch program. Emerg Med Serv 1994; 23:52–60. [PubMed] [Google Scholar]
- 22.Heward A, Damiani M, Hartley-Sharpe C. Does the use of the Advanced Medical Priority Dispatch System affect cardiac arrest detection? Emerg Med J 2004; 21:115–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eisenberg MS, Carter W, Hallstrom A, Cummins R, Litwin P, Hearne T. Identification of cardiac arrest by emergency dispatchers. Am J Emerg Med 1986; 4:299–301. [DOI] [PubMed] [Google Scholar]
- 24.Herlitz J, Andersson E, Bang A, Engdahl J, Holmberg M, lindqvist J, et al. Experiences from treatment of out-of-hospital cardiac arrest during 17 years in Goteborg. Eur Heart J 2000; 21:1251–1258. [DOI] [PubMed] [Google Scholar]
- 25.Vaillancourt C, Verma A, Trickett J, Crete D, Beaudoin T, Nesbitt L, et al. Evaluating the effectiveness of dispatch-assisted cardiopulmonary resuscitation instructions. Acad Emerg Med 2007; 14:877–883. [DOI] [PubMed] [Google Scholar]
- 26.Wallace SK, Abella BS, Shofer FS, Leary M, Agarwal AK, Mechem CC, et al. Effect of time of day on prehospital care and outcomes after out-of-hospital cardiac arrest. Circulation 2013; 127:1591–1596. [DOI] [PubMed] [Google Scholar]
- 27.Stiell IG, Wells GA, DeMaio VJ, Spaite DW, Field BJ, 3rd, Munkley DP, et al. Modifiable factors associated with improved cardiac arrest survival in a multicenter basic life support/defibrillation system: OPALS Study Phase I results. Ontario Prehospital Advanced Life Support. Ann Emerg Med 1999; 33:44–50. [DOI] [PubMed] [Google Scholar]
- 28.De Maio VJ, Stiell IG, Wells GA, Spaite DW. Ontario Prehospital Advanced Life Support Study Group. Optimal defibrillation response intervals for maximum out-of-hospital cardiac arrest survival rates. Ann Emerg Med 2003; 42:242–250. [DOI] [PubMed] [Google Scholar]
- 29.Song KJ, Shin SD, Park CB, Kim JY, Kim DK, Kim CH, et al. Dispatcher-assisted bystander cardiopulmonary resuscitation in a metropolitan city: A before-after population-based study. Resuscitation 2014; 85:34–41. [DOI] [PubMed] [Google Scholar]
- 30.Ma MH, Lu TC, Ng JC, Lin CH, Chiang WC, Ko PC, et al. Evaluation of emergency medical dispatch in out-of-hospital cardiac arrest in Taipei. Resuscitation 2007; 73:236–245. [DOI] [PubMed] [Google Scholar]
- 31.Lerner EB, Rea TD, Bobrow BJ, Acker JE, 3rd, Berg RA, Brooks SC, et al. Emergency medical service dispatch cardiopulmonary resuscitation prearrival instructions to improve survival from out-of-hospital cardiac arrest: a scientific statement from the American Heart Association. Circulation 2012; 125:648–655. [DOI] [PubMed] [Google Scholar]


