Abstract
Ciguatera is the most commonly reported marine food-borne illness worldwide. Because there is a biological plausibility that ciguatera may be impacted by long-term climate variability and Florida is on the northern border of the geographic distribution of ciguatera, it is important to update our understanding of its epidemiology in Florida. We performed an analysis of 291 reports in Florida from 2000 to 2011 and an e-mail survey of 5,352 recreational fishers to estimate incidence and underreporting and identify high risk demographic groups, fish types, and catch locations. Incidence was 5.6 per 100,000 adjusted for underreporting. Hispanics had the highest incidence rate (relative risk [RR] = 3.4) and were more likely to eat barracuda than non-Hispanics. The most common catch locations for ciguatera-causing fish were the Bahamas and Florida Keys. Cases caused by fish from northern Florida were infrequent. These results indicate that ciguatera incidence is higher than estimated from public health reports alone. There is little evidence that incidence or geographic range has increased because of increased seawater temperatures since earlier studies.
Introduction
Ciguatera fish poisoning is a marine food-borne illness1 that causes severe gastrointestinal and neurologic symptoms.2 It results from the consumption of reef fish containing toxins produced by benthic dinoflagellates of the genus Gambierdiscus.3 Numerous ciguatoxins have been identified and are described elsewhere.4 Ciguatera is endemic to many tropical and subtropical areas worldwide,5,6 with a range of latitudes from 35° N to 35° S.4 Annual incidence worldwide has been estimated as 50,000–500,000 cases per year,4,7 and there are indications that ciguatera incidence is increasing in the Pacific Islands, where it was 60% higher in 1998–2008 compared with 1973–1983.8 In the Caribbean, there are limited data on changes in incidence over time. Although incidence is high in some parts of the Caribbean Sea,9,10 only one study has looked at a long-term time trend, and no increase was observed in the U.S. Virgin Islands.11 Because of hypotheses that increasing seawater temperatures associated with long-term climate variability may increase ciguatera incidence and range worldwide,6,9,12–15 due to the ideal water temperature of 29°C that favors Gambierdiscus growth,9,12 it is important to update our estimates of disease incidence and the geographic distribution of ciguatoxic fish.
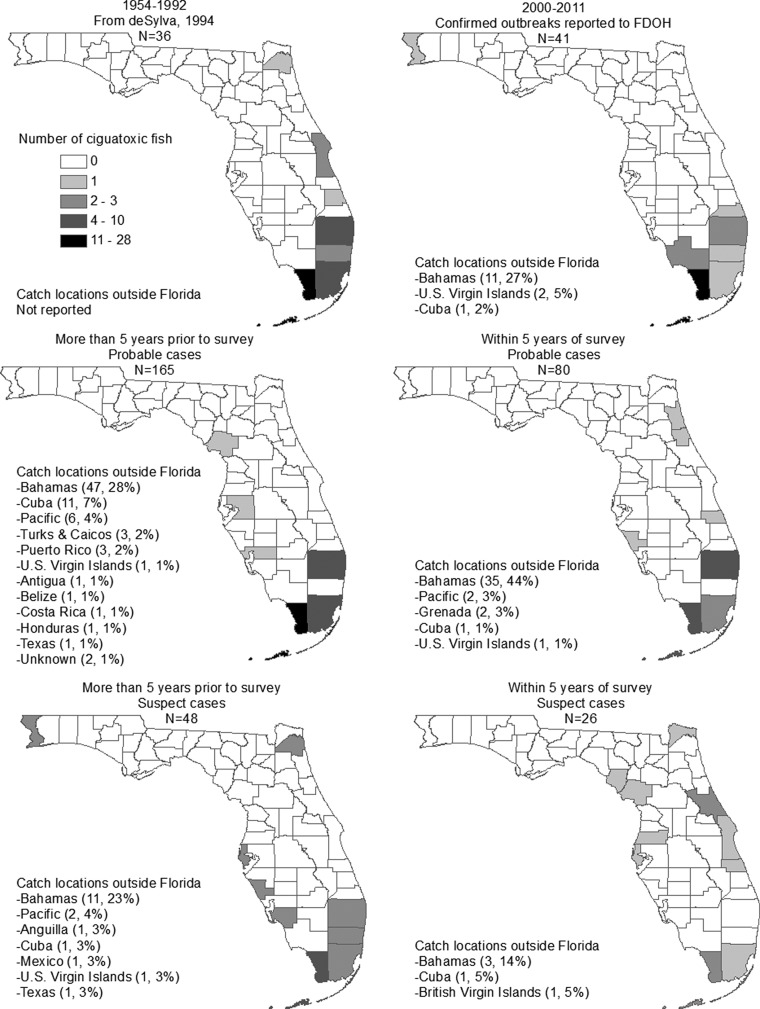
It is particularly useful to examine areas on the border of the current geographic range, as this provides a potentially useful marker of the impact of global climate variability on ciguatera. Although Florida is south of the northern latitude border mentioned above, the areas further north within the United States appear to have ciguatera only sporadically, and thus Florida is an ideal location for study. In Miami, FL, in 1980, incidence was estimated as 5–500 per 100,000,16 but a more recent and precise estimate is not available. From 1954 to 1991, the majority of ciguatera cases in Florida were associated with ingestion of fish either caught in the Bahamas or in Monroe or Miami-Dade counties in Florida.17 A few sporadic ciguatoxic fish were caught in counties in northern Florida, but all were migratory species such as barracuda, suggesting that the fish may have obtained the toxin in south Florida.17
Obtaining complete epidemiologic information on ciguatera is difficult. Ciguatera is a notifiable (i.e., reportable) illness in Florida and several other states, requiring health-care providers to report cases to the public health system. However, it is likely that case reports do not represent all poisoning cases. Underreporting occurs at multiple levels, which will be described below. A study in Florida found that only 43% of ciguatera calls to the Florida Poison Information Center in Miami were reported to the Florida Department of Health (FDOH),18 and experts estimate that only 20% or fewer of ciguatera cases are reported.2,4,8 However, reporting procedures from the Poison Information Center have improved since that study, and data-driven estimates of underreporting are needed to more accurately determine the burden of disease and improve surveillance.
We performed a survey of recreational fishermen and an analysis of reports of ciguatera to the FDOH to estimate incidence by adjusting for underreporting, by identifying high-risk demographic groups, high-risk fish types, and catch locations that cause ciguatera illness in Florida.
Methods
Data.
Public health reports.
The FDOH maintains records of cases of ciguatera reported through the statewide notifiable disease surveillance system. These cases are classified as “confirmed cases” (Table 1) based on the FDOH case definition, which has higher specificity than the survey based on self-report described below. The confirmed case definition requires a clinically compatible illness in a patient with a history of fish consumption in the 24 hours before onset of symptoms. We obtained de-identified data from FDOH on all cases of ciguatera with onset from 2000 to 2011. The following information was collected regarding the affected individuals: county of residence, age, gender, race and ethnicity, origin of fish, and case notes on fish meal. In analyzing fish types and catch locations, outbreaks were used instead of individuals to avoid overweighting fish involved in large outbreaks where a single fish poisoned multiple people. A “confirmed outbreak” was defined as one or multiple confirmed cases of ciguatera linked by a common fish meal described in the investigation by FDOH (Table 1).
Table 1.
Definition of ciguatera case classifications
| Classification | Definition |
|---|---|
| Confirmed case | Individual case of ciguatera reported to FDOH and classified according to Florida's case definition as confirmed |
| Confirmed outbreak | One or multiple confirmed cases of ciguatera reported to FDOH linked by a common fish meal |
| Likely case | Individual identified through e-mail survey, who reports having been diagnosed with ciguatera fish poisoning |
| Possible case | Individual identified through e-mail survey, who reports having experienced symptoms of ciguatera after eating saltwater fish |
FDOH = Florida Department of Health.
Testing of fish flesh for ciguatoxin was not required for any classification. Physician diagnosis was not verified for likely cases. Physician diagnosis was not required for confirmed cases, but was the most likely source of report.
Survey of recreational saltwater fishers.
We also performed an e-mail survey of recreational saltwater fishing license holders to identify cases of ciguatera not reported to FDOH. Fishers were selected rather than a sample of the general population because we believed they may be at higher risk because of fish consumption, which increased the likelihood of identifying cases. We also hypothesized that they would be more aware of where the fish was caught and of ciguatera. Contact information for all recreational saltwater fishing licenses in 2011 was obtained from the Florida Fish and Wildlife Conservation Commission. Approximately 41% of the license holders provided an e-mail address, and the survey was e-mailed from the University of Florida to all 311,799 of these individuals, of which 10% were undeliverable (total delivered approximately 280,619). The survey was sent to each e-mail address two times approximately 1 week apart. A Spanish language version was available.
The survey assessed the history of ciguatera illness using two questions. Participants were classified as “likely cases” of ciguatera (Table 1) if they responded affirmatively to the question: “Have you ever been diagnosed with ciguatera fish poisoning after eating saltwater fish?” They were classified as “possible cases” if they answered “No” to ciguatera diagnosis and “Yes” to “Have you ever experienced vomiting and/or diarrhea combined with numbness around the mouth or hands, or weakness in the legs, or reversal of hot and cold sensations after eating saltwater fish?” Likely and possible cases were not grouped into outbreaks as there were no shared exposures identified. Cases who self-reported that their symptoms were caused by eating shellfish were excluded from the case analyses as these illnesses were unlikely to be ciguatera.
Likely and possible cases were then asked whether they or someone they knew had caught the fish that caused their illness, where it was obtained, the type of fish, when their illness occurred, whether they sought medical attention (emergency room, private physician, called poison control, or other), whether they were a Florida resident when the illness occurred, whether the medical attention was obtained in Florida, ethnicity, and zip code of current residence. Cases were also asked to provide name and date of birth for linking to the FDOH public health reports, but this request for information was emphasized as optional. The first 75,000 recipients received a shorter survey that was limited to only ciguatera illnesses caused by fish caught by the participant or someone they knew and did not include collection of identifiers or ethnicity.
Analysis.
Incidence and demographic risk factors.
We calculated crude average annual incidence rates of ciguatera for each county in Florida based on case residence and the state overall using FDOH-confirmed ciguatera case data for 2007–2011 and U.S. 2010 Census data.19 Since these values account for only reported cases, we also estimated underreporting based on the e-mail survey to approximate the true incidence. We considered three levels of underreporting (Table 2). To do this, we first calculated the percent of likely and possible cases who did not seek medical attention (Level A) and the percent of cases who sought medical attention but were not diagnosed (i.e., possible cases that sought medical attention, Level B). To estimate the percentage of diagnosed cases from the survey data that were not reported to FDOH (Level C), we calculated the percentage of likely cases with illness in the previous 15 years (who sought medical attention, were residents of Florida at the time of their illness, and who provided identifiable information), who were not present in the FDOH database. The overall incidence for Florida and high-incidence counties was then adjusted for all the three levels of underreporting.
Table 2.
Levels of underreporting for persons affected with ciguatera
| Level | Definition |
|---|---|
| A | Affected persons who do not seek medical attention for their illness |
| B | Persons who seek medical attention for their illness but are not appropriately diagnosed |
| C | Persons who are diagnosed but not reported to FDOH or other jurisdiction. |
FDOH = Florida Department of Health.
In addition, we attempted to account for nonresponse bias in the survey. Because ciguatera is a very distinctive and memorable illness for those who have suffered from it, it is likely that persons who had sought medical attention for their illness and were diagnosed with ciguatera would be more likely to participate in a survey about ciguatera than those who were unaffected or who had experienced illness but were unaware of the cause and thus did not recognize the term ciguatera. This bias would tend to overestimate the percentage of likely cases compared with possible cases in the survey and overestimate the percent seeking medical attention and the percent diagnosed. To assess the impact of this bias, we performed a sensitivity analysis assuming that people with a known ciguatera diagnosis would be 5 or 10 times more likely to participate.20 We recalculated underreporting levels A and B after increasing the theoretical number of possible cases by these amounts. Because possible cases would not have a known diagnosis to influence their participation in the survey and because this analysis was related to the relative proportion of likely versus possible cases, adjustment of possible cases versus non-cases was not considered necessary.
We also estimated the risk associated with each demographic group (age, gender, and race/ethnicity) by calculating unadjusted group-specific incidence rates and relative risks for 2007–2011 using FDOH data. We repeated this analysis on Miami-Dade County alone as it is the county with the highest total case count and has a different demographic makeup than much of the state, with a high proportion of Hispanics, a group we hypothesized to be at high risk.
Types and catch locations of fish causing ciguatera illnesses.
We descriptively analyzed fish types associated with confirmed ciguatera outbreaks and likely and possible individual cases. Confirmed outbreaks were analyzed as one observation per outbreak to avoid bias toward large fish that are more likely to cause multiple illnesses, however, this does mean that it may be less clear which fish type caused the most individual cases. To approximately adjust for overall consumption and thus give a descriptive indication of which fish were particularly high risk for ciguatera rather than just frequently consumed (i.e., a higher percentage of consumed fish would be likely to be ciguatoxic than for other fish types), we normalized the fish types that caused ciguatera cases by the combined commercial and recreational fish landings in pounds for those fish types. Fish landings data were obtained from the National Oceanic and Atmospheric Administration's Office of Science and Technology, National Marine Fisheries Service, and estimated total catch by fish type and location.21 To assess ethnic differences, we also analyzed the most common fish types associated with illness by ethnicity using χ2 tests to determine whether there are ethnic variations in fish consumption.
We created separate maps of fish catch locations for confirmed, likely, and possible cases, with likely and possible further divided into more than 5 years and 5 years or less before survey (specific dates of illness were not collected). We also mapped data from a study by de Sylva17 that included ciguatoxic fish catch locations for outbreaks reported to a hotline maintained by the University of Miami from 1954 to 1992. The maps of different periods were used to qualitatively assess whether ciguatoxic fish have been more frequently caught outside south Florida in recent years.
Analyses were performed using SAS 9.2 (Cary, NC). The Institutional Review Board at the University of Florida approved this study. The Institutional Review Board at FDOH also approved the matching of survey data to ciguatera cases in the FDOH notifiable disease surveillance system.
Results
There were 291 cases of ciguatera reported to FDOH from 2000 to 2011. Of these, 245 provided some information about the fish that caused their illness, and these were divided into 97 distinct outbreaks. A total of 5,352 individuals responded to the fishermen survey (response rate = 5,352/280,619, 1.9%), of which 245 were classified as likely cases and 74 were classified as possible cases.
Incidence and demographic risk factors.
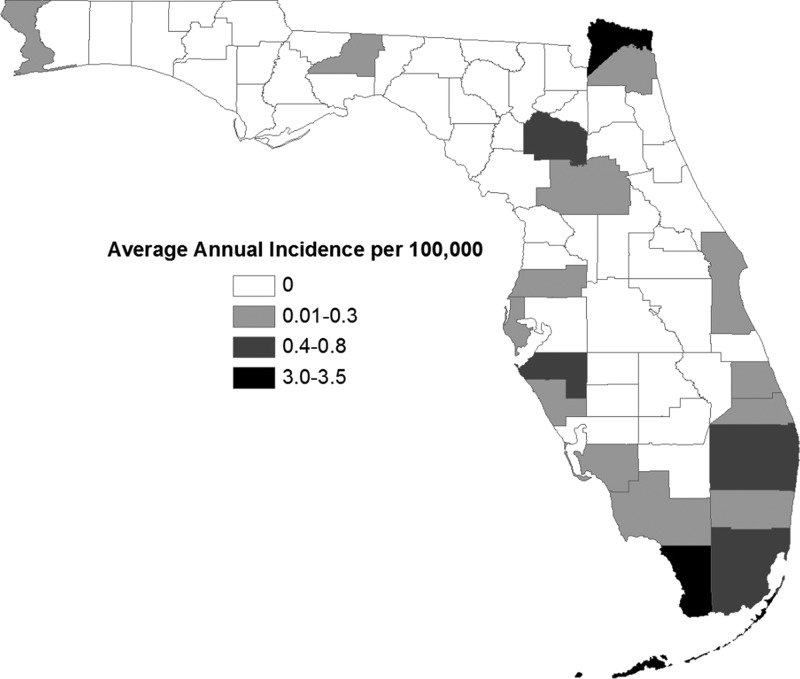
The unadjusted annual incidence rate of ciguatera in Florida based on FDOH cases was 0.2 per 100,000 (Table 3). Unadjusted estimates by county are displayed in Figure 1 . In estimating underreporting (Table 4), 183/319 (57%, 95% confidence interval [CI]: 52, 63) cases in the e-mail survey sought medical attention for their illness, with different rates of medical attention among likely (66%, 95% CI: 60, 72) and possible (30%, 95% CI: 19, 40) cases. Most cases identified in the survey (88%, 95% CI: 83, 93) who sought medical attention were diagnosed with ciguatera. Of the 27 likely cases with illness in the previous 15 years who provided identifiers, only 2 (7%, 95% CI: 0, 18) were reported to the FDOH database. The combination of all the three levels of underreporting (1/57% × 88% × 7%) increases the incidence by a factor of 28 to 5.6 per 100,000 for Florida (Table 3).
Table 3.
Ciguatera average annual incidence estimates for the State of Florida and Miami-Dade and Monroe Counties, 2007–2011, per 100,000
| Florida | Miami-Dade County | Monroe County | |
|---|---|---|---|
| Crude incidence of FDOH confirmed cases | 0.2 | 1 | 3 |
| Adjusted for underreporting (A × B × C) | 5.6 | 28 | 84 |
FDOH = Florida Department of Health.
Figure 1.
Unadjusted incidence of reported ciguatera in Florida by county of residence, 2007–2011. Incidence rates were calculated using the number of confirmed cases of ciguatera reported to the Florida Department of Health and population data from the 2010 U.S. Census.
Table 4.
Annual incidence of ciguatera in Florida from FDOH reports with adjustment for underreporting and nonresponse bias using data from a survey of recreational fishers
| Likely cases | Possible cases | Overall | |
|---|---|---|---|
| Crude incidence from FDOH reports per 100,000 | – | – | 0.2 |
| Observed responses | 245 | 74 | 319 |
| Seek medical attention | 161 (66%) | 22 (30%) | 183 (57%) |
| Diagnosed if sought medical attention | – | – | 161/183 (88%) |
| Reported if diagnosed | – | – | 7%† |
| Underreporting factor | – | – | 0.57 × 0.88 × 0.07 = 28 |
| Incidence per 100,000 | – | – | 28 × 0.2 = 5.6 |
| Adjusted for nonresponse bias (×5*) | 245 | 370 | 615 |
| Seek medical attention | 161 (66%) | 110 (30%) | 271 (44%) |
| Sought medical attention, diagnosed | – | – | 161/271 (59%) |
| Underreporting factor | – | – | 0.44 × 0.59 × 0.07 = 55 |
| Incidence per 100,000 | – | – | 11 |
| Adjusted for nonresponse bias (×10*) | 245 | 740 | 985 |
| Seek medical attention | 161 (66%) | 220 (30%) | 381 (39%) |
| Sought medical attention, diagnosed | – | – | 161/381 (42%) |
| Underreporting factor | – | – | 0.39 × 0.42 × 0.07 = 87 |
| Incidence per 100,000 | – | – | 17 |
FDOH = Florida Department of Health.
Factor by which possible cases were multiplied to account for nonresponse bias, in which individuals who are aware of their diagnosis (likely cases) are more likely to participate than others (possible cases and non-cases).
The same rate of reported if diagnosed was used for all three estimates.
In the sensitivity analysis accounting for nonresponse bias, adjusting the levels of percent seeking medical attention and percent diagnosed would increase incidence by a factor of 55–87 (Table 4), to 11–17 per 100,000 for Florida, and 55–87 and 165–261 per 100,000 for Miami-Dade and Monroe counties, respectively.
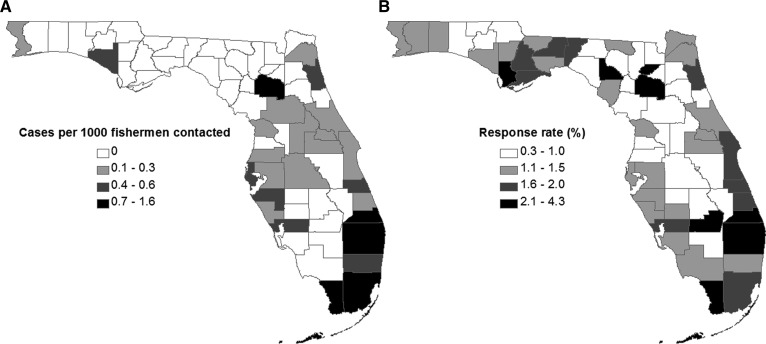
Cases per county among fishers normalized by number of fishers contacted are shown in Figure 2 . The crude incidence among fishers was approximately 400 per 100,000, or 2,000 times higher than the estimate based on FDOH reports, likely due at least in part to nonresponse bias in the survey.
Figure 2.
Ciguatera cases and response rate of recreational fishing license holders by county of residence in e-mail survey. (A) Number of cases of ciguatera per 1,000 fishers contacted by e-mail and (B) percentage of e-mailed fishers that responded to the survey.
In the demographic risk factor analysis, Hispanics were the group with the highest incidence rate and their relative risk was 3.4 compared with non-Hispanics (Table 5). Blacks and other races had lower risk than whites, and those less than 20 and over 64 years had lower risk than those from 20 to 34 and 35 to 64 years.
Table 5.
Average unadjusted annual incidence of reported ciguatera by demographic group in Florida and Miami-Dade County, cases reported to FDOH 2007–2011
| Variable | Florida |
Miami-Dade county |
||||
|---|---|---|---|---|---|---|
| N = 206 n (%) | Incidence (per 100,000) | RR | N = 94 n (%) | Incidence (per 100,000) | RR | |
| Age (years) | ||||||
| < 20 | 20 (10) | 0.1 | 0.3 | 8 (9) | 0.3 | 0.3 |
| 20–34 | 45 (22) | 0.3 | Ref | 26 (28) | 1.0 | Ref |
| 35–64 | 134 (65) | 0.4 | 1.4 | 54 (57) | 1.1 | 1.1 |
| 65+ | 7 (3) | 0.04 | 0.2 | 6 (6) | 0.3 | 0.3 |
| Gender | ||||||
| Female | 92 (45) | 0.2 | Ref | 39 (41) | 0.6 | Ref |
| Male | 114 (55) | 0.2 | 1.3 | 55 (59) | 0.9 | 1.5 |
| Race | ||||||
| White | 167 (81) | 0.2 | Ref | 84 (89) | 0.9 | Ref |
| Black | 4 (2) | 0.03 | 0.1 | 2 (2) | 0.1 | 0.1 |
| Other | 7 (3) | 0.1 | 0.3 | 0 | – | – |
| Unknown | 28 (14) | 0.1 | 0.3 | 8 (9) | – | – |
| Ethnicity | ||||||
| Non-Hispanic | 93 (45) | 0.1 | Ref | 16 (17) | 0.4 | Ref |
| Hispanic | 92 (45) | 0.4 | 3.4 | 78 (83) | 1.0 | 2.6 |
| Unknown | 21 (10) | – | – | 0 | – | – |
FDOH = Florida Department of Health; RR = relative risk; Ref = reference group.
Types and catch locations of illness-causing fish.
Among confirmed outbreaks reported to FDOH, barracuda were the most commonly reported fish eaten (37%), followed by grouper (33%) and amberjack (8%) (Table 6). There was more variation in the fisher cases, with barracuda representing 13% of likely and 9% of possible cases. Looking at fish types from all the three case classifications combined, grouper was the most commonly reported (31%), followed by barracuda (18%), amberjack (8%), and hogfish (7%). All four of these fish types were overrepresented in ciguatera cases compared with their representation in the fish landings, with hogfish and barracuda having the highest ratios (28 and 23, respectively; Table 6). In looking at fish types by ethnicity, Hispanic cases were more likely to eat barracuda than non-Hispanic cases, while grouper and amberjack were more frequently eaten by non-Hispanics in both FDOH reports and the fishermen survey (Table 7).
Table 6.
Fish types associated with ciguatera cases in Florida, 2000–2011
| Type of fish | Confirmed outbreaks (FDOH) (N = 97) n (%) | Likely cases (e-mail survey) (N = 245) n (%) | Possible cases (e-mail survey) (N = 74) n (%) | Combined (N = 416) n (%) | Average commercial and recreational landings in Florida, 2000–2010 lb (% total) | Ratio of % combined ciguatera cases to % landings by fish type |
|---|---|---|---|---|---|---|
| Hogfish | 1 (1) | 28 (11) | 1 (1) | 30 (7) | 296,154 (0.3) | 28 |
| Barracuda | 36 (37) | 32 (13) | 7 (9) | 75 (18) | 897,461 (0.8) | 23 |
| Amberjack | 8 (8) | 23 (9) | 1 (1) | 32 (8) | 2,638,570 (2) | 4 |
| Grouper | 32 (33) | 83 (34) | 14 (19) | 129 (31) | 8,942,747 (8) | 3 |
| Snapper | 4 (4) | 16 (7) | 14 (19) | 34 (8) | 8,200,017 (7) | 1 |
| Other jack | 0 | 10 (4) | 1 (1) | 11 (3) | 4,717,613 (4) | 0.6 |
| Mackerel/kingfish | 3 (3) | 15 (6) | 4 (5) | 22 (5) | 16,825,185 (15) | 0.4 |
| Mahi mahi | 2 (2) | 4 (2) | 2 (3) | 8 (2) | 6,731,426 (6) | 0.3 |
| Other | 8 (8) | 17 (7) | 19 (26) | 44 (11) | – | – |
| Multiple fish | 1 (1) | 7 (3) | 6 (8) | 14 (3) | – | – |
| Unknown | 2 (2) | 10 (4) | 5 (7) | 17 (4) | – | – |
Table 7.
Most common three fish types consumed in ciguatera outbreaks reported to FDOH by ethnicity
| Type of fish | Confirmed outbreaks* (FDOH reports) | Likely and possible cases (fishermen survey) | ||
|---|---|---|---|---|
| Hispanic n (%) | Non-Hispanic n (%) | Hispanic n (%) | Non-Hispanic n (%) | |
| Barracuda | 29 (76) | 3 (7) | 10 (24) | 19 (9) |
| Grouper | 4 (11) | 26 (58) | 6 (14) | 70 (34) |
| Amberjack | 0 | 7 (16) | 4 (10) | 12 (6) |
| Other | 5 (13) | 9 (20) | 22 (52) | 102 (50) |
| P value | < 0.0001 | 0.007 | ||
FDOH = Florida Department of Health.
Ethnicity of all individuals affected by the outbreak.
The most common fish catch locations in all the three case classifications combined were the Bahamas (107, 34%) and the Florida Keys in Monroe County (63, 20%). Cuba and Palm Beach County were the next most common, each with 5%, followed by Miami-Dade County with 4%. Figure 3 shows the catch locations by case classification and period. Among confirmed outbreaks with catch location in Florida, 7 (17%) were caught outside Monroe or Miami-Dade County, while for likely cases, this value was 19 (29%) and for possible, it was 16 (62%). Overall, cases caused by fish caught in northern Florida were sporadic and infrequent in all periods and case classifications.
Figure 3.
Catch locations of ciguatera illness-causing fish. Time frames for fish causing likely and possible cases are based on responses to e-mail survey of fishers (survey options: within the past year; more than 1 year, but less than 5 years ago; more than 5 years ago). Specific dates of illness/fish catch were not collected.
Discussion
The results of this study suggest that incidence of ciguatera is likely significantly higher than estimated based on public health reports alone. However, there is little evidence that incidence or geographic range has increased because of increased seawater temperatures since earlier studies. Cases were associated with fish caught in parts of Florida north of Palm Beach County, but only sporadically. This is consistent with cases from 1954 to 1992.17 Compared with a 1980 estimate for Miami of 5 per 100,000 before adjusting for reporting, we estimated Miami's incidence as 1 per 100,000 based on FDOH reports, indicating that incidence has, if anything, decreased over the last three decades. This may be due to changes in fish consumption behavior as hypothesized in the U.S. Virgin Islands11 and/or changes in the fisheries or other environmental factors. However, the past and current studies were performed using different data sources, and therefore observed changes in rates are not directly comparable and should be interpreted with caution. In either case, there is a strong evidence of a relationship between seawater temperature and growth of the Gambierdiscus dinoflagellates that produce the toxin,6,9,12,22 so incidence and range in Florida should be monitored further in the future, particularly if an increase in seawater temperatures is observed.
In evaluating the magnitude of underreporting using survey data, we estimated that true cases were higher than FDOH reports by a factor of 28. However, because of the low response rate and the fact that ciguatera is a very distinctive and memorable illness for those who have suffered from it, it is extremely likely that the survey suffers from significant nonresponse bias. The sensitivity analysis presented in Table 4 recalculates the first two levels of underreporting assuming that likely cases were overrepresented and suggests that the true incidence may be higher than FDOH reports by a factor of 55–87. This adjustment should be interpreted with caution, as the correction is arbitrary, but we believe it may more closely represent the true magnitude of underreporting.
Our finding that only 7% of diagnosed cases were reported to the FDOH may at first glance be surprising. However, for many notifiable diseases, physicians rely on laboratory reporting of cases, which is not available for ciguatera because of the lack of a diagnostic laboratory test. In addition, because ciguatera is not a communicable disease, physicians may be unaware that it is a notifiable condition in the State of Florida. One survey in Miami-Dade County found that only 47% of physicians knew that ciguatera was notifiable,23 and this is likely to be lower in less endemic parts of the state. These two factors combined could explain the extremely low estimated rate of reporting. It is also possible that a physician could have reported an illness but FDOH determined that it did not meet the confirmed case definition. Given that no laboratory testing is required for ciguatera and only clinical criteria and fish consumption are necessary for confirmation, this is unlikely.
With regard to fish type, the fish species most commonly causing illness were consistent with past studies.10,24 Barracuda were extremely overrepresented in ciguatera cases compared with fish landings in Florida. Despite past public health education efforts on avoidance of high risk fish such as barracuda, commercial and recreational fishermen together produced an average of almost 900,000 pounds of barracuda per year over the last decade, therefore fishers should be further encouraged to avoid this species. However, barracuda were more commonly eaten by confirmed cases from FDOH reports than likely and possible cases from the e-mail survey. This may suggest a bias where cases involving barracuda are more likely to be diagnosed and reported because of public health awareness of the risk associated with barracuda. Since outbreaks with multiple cases are more likely to be reported than isolated individual cases,18 this bias could also be because a single large barracuda can feed many people. Besides barracuda, hogfish was a high-risk fish species in this study, which may be less commonly known. Although grouper were not as overrepresented as barracuda and hogfish when compared with landings, they were still responsible for the largest number of cases identified in this study and thus are deserving of their place on high-risk lists.
We also found that Hispanics experience the highest rate of ciguatera illness in Florida, possibly due to more frequent consumption of barracuda than non-Hispanics. This may represent an opportunity for targeted, culturally relevant educational messaging after more narrowly identifying high-risk cultural groups. The disparity may also be due to socioeconomic factors, as illness in non-Hispanics was more commonly caused by amberjacks that are generally caught offshore in deepwater. Clarifying the reasons for differences in consumption would require further qualitative research, which could be partially done by adding questions to FDOH ciguatera case investigations about country of origin, reason for eating barracuda, and so forth. In addition, given this risk factor, it is important to note that undocumented immigrants may as a group be particularly prone to underreporting, and this was not accounted for in this study's underreporting estimates.
Our results also clearly show that the majority of ciguatera cases in Florida are caused by fish caught in the Bahamas and the Florida Keys, and fishers should be cautious in consuming high-risk fish from these locations. There is risk of catching ciguatoxic fish throughout the Caribbean, and a small risk throughout the State of Florida, possibly due to fish migration. FDOH reports included the smallest percent of fish caught in northern Florida, and also had fewer case residences in northern Florida than fishers. This may suggest another diagnosis and reporting bias, as physicians in this area may be less familiar with the disease than in south Florida.
In addition to the survey nonresponse bias already discussed, there are a few limitations that should be considered when interpreting our results. First, we relied on self-report, so the information provided may not be completely accurate. In particular, there may be false cases in the sample. Not all likely cases sought medical attention, and thus “diagnosis” may have been by someone other than a physician. Even confirmed and physician-diagnosed cases do not have laboratory confirmation. Fish types may also have been incorrectly identified. At the same time, the sample of cases may be biased toward the traditional ciguatera range due to contacted individuals being more likely to participate if they were already familiar with ciguatera (Figure 2). Finally, the survey sampled only fishermen with current saltwater fishing licenses. Fishers who are exempt, those with only a shoreline fishing license, as well as those who ignore the licensing laws, would not have been captured. Relevant exemptions include fishing from a vessel with a vessel license, as tourists would be likely to do, and Florida residents age 65 years or older.25 There is no reason to think that any of these missing fishers would get ciguatera from different fish types or catch locations than those described here, but it is possible that we are missing important information on risk.
Despite these limitations, we were able to identify over 300 likely or possible cases of ciguatera, the majority of which were not reported to FDOH. This increased our sample of fish types and catch locations, and gave us valuable information on potential biases in the current surveillance system. Moving forward, FDOH may be able to improve reporting by educating physicians on the possibility of acquiring ciguatera from fish caught outside typical areas, and emphasizing the unique clinical presentation of ciguatera illness. There is a continuing need to monitor ciguatera in Florida.
ACKNOWLEDGMENTS
We thank Kevin Hanson at the University of Florida for his technical assistance with the e-mail survey.
Footnotes
Financial support: Study data were collected using REDCap electronic data capture tools hosted at University of Florida, which is supported by NIGH National Center for Advancing Translational Sciences grant UL1 TR000064.
Authors' addresses: Elizabeth G. Radke, Arlington Public Health Division, Arlington, VA, E-mail: bethradke@gmail.com. Andrew Reich, Florida Department of Health, Tallahassee, FL, E-mail: andy.reich@flhealth.gov. John Glenn Morris Jr., Emerging Pathogens Institute, University of Florida, Gainesville, FL, E-mail: jgmorris@epi.ufl.edu.
References
- 1.Bagnis R, Chanteau S, Chungue E, Hurtel JM, Yasumoto T, Inoue A. Origins of ciguatera fish poisoning: a new dinoflagellate, Gambierdiscus toxicus Adachi and Fukuyo, definitively involved as a causal agent. Toxicon. 1980;18:199–208. doi: 10.1016/0041-0101(80)90074-4. [DOI] [PubMed] [Google Scholar]
- 2.Friedman MA, Fleming LE, Fernandez M, Bienfang P, Schrank K, Dickey R, Bottein MY, Backer L, Ayyar R, Weisman R, Watkins S, Granade R, Reich A. Ciguatera fish poisoning: treatment, prevention and management. Mar Drugs. 2008;6:456–479. doi: 10.3390/md20080022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewis RJ, Ruff TA. Ciguatera—ecological, clinical, and socioeconomic perspectives. Crit Rev Environ Sci Technol. 1993;23:137–156. [Google Scholar]
- 4.Dickey RW, Plakas SM. Ciguatera: a public health perspective. Toxicon. 2010;56:123–136. doi: 10.1016/j.toxicon.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Lewis RJ. The changing face of ciguatera. Toxicon. 2001;39:97–106. doi: 10.1016/s0041-0101(00)00161-6. [DOI] [PubMed] [Google Scholar]
- 6.Llewellyn LE. Revisiting the association between sea surface temperature and the epidemiology of fish poisoning in the South Pacific: reassessing the link between ciguatera and climate change. Toxicon. 2010;56:691–697. doi: 10.1016/j.toxicon.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Fleming LE, Baden DG, Bean JA, Weisman R, Blythe DG. Marine seafood toxin diseases: issues in epidemiology and community outreach. In: Reguera B, Blanco J, Fernandez ML, Wyatt T, editors. Harmful Algae. Galicia, Spain: Xunta de Galicia and Intergovernmental Commission of UNESCO; 1998. pp. 245–248. [Google Scholar]
- 8.Skinner MP, Brewer TD, Johnstone R, Fleming LE, Lewis RJ. Ciguatera fish poisoning in the Pacific islands (1998 to 2008) PLoS Negl Trop Dis. 2011;5:e1416. doi: 10.1371/journal.pntd.0001416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tester PA, Feldman RL, Nau AW, Kibler SR, Wayne Litaker R. Ciguatera fish poisoning and sea surface temperatures in the Caribbean Sea and the West Indies. Toxicon. 2010;56:698–710. doi: 10.1016/j.toxicon.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 10.Azziz-Baumgartner E, Luber G, Conklin L, Tosteson TR, Granade HR, Dickey RW, Backer LC. Assessing the incidence of ciguatera fish poisoning with two surveys conducted in Culebra, Puerto Rico, during 2005 and 2006. Environ Health Perspect. 2012;120:526–529. doi: 10.1289/ehp.1104003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Radke EG, Grattan LM, Cook RL, Smith TB, Anderson DM, Morris JG. Ciguatera incidence in the U.S. Virgin Islands has not increased over a 30 year time period despite rising seawater temperatures. Am J Trop Med Hyg. 2013;88:908–913. doi: 10.4269/ajtmh.12-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hales S, Weinstein P, Woodward A. Ciguatera (fish poisoning), el Nino, and Pacific sea surface temperatures. Ecosyst Health. 1999;5:20–25. [Google Scholar]
- 13.Chateau-Degat ML, Chinain M, Cerf N, Gingras S, Hubert B, Dewailly E. Seawater temperature, Gambierdiscus spp. variability and incidence of ciguatera poisoning in French Polynesia. Harmful Algae. 2005;4:1053–1062. [Google Scholar]
- 14.Moore SK, Trainer VL, Mantua NJ, Parker MS, Laws EA, Backer LC, Fleming LE. Impact of climate variability and future climate change on harmful algal blooms and human health. Environ Health. 2008;7:S4. doi: 10.1186/1476-069X-7-S2-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gingold DB, Strickland MJ, Hess JJ. Ciguatera fish poisoning and climate change: analysis of national poison center data in the United States, 2001–2011. Environ Health Perspect. 2014;122:580–586. doi: 10.1289/ehp.1307196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lawrence DN, Enriquez MB, Lumish RM, Maceo A. Ciguatera fish poisoning in Miami. JAMA. 1980;244:254–258. [PubMed] [Google Scholar]
- 17.de Sylva DP. Distribution and ecology of ciguatera fish poisoning in Florida, with emphasis on the Florida Keys. Bull Mar Sci. 1994;54:944–954. [Google Scholar]
- 18.Begier EM, Backer LC, Weisman RS, Hammond RM, Fleming LE, Blythe D. Outbreak bias in illness reporting and case confirmation in ciguatera fish poisoning surveillance in south Florida. Public Health Rep. 2006;121:658–665. doi: 10.1177/003335490612100605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.United States Census Bureau Census Summary File 1. 2010. http://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml Available at.
- 20.Rupp I, Triemstra M, Boshuizen HC, Jacobi CE, Dinant HJ, van den Bos GAM. Selection bias due to non-response in a health survey among patients with rheumatoid arthritis. Eur J Public Health. 2002;12:131–135. doi: 10.1093/eurpub/12.2.131. [DOI] [PubMed] [Google Scholar]
- 21.National Marine Fisheries Service, Fisheries Statistics Division Commercial and Recreational Finfish Landings. http://www.st.nmfs.noaa.gov/index Available at. Accessed 2013.
- 22.Bomber J, Guillard R, Nelson W. Roles of temperature, salinity, and light in seasonality, growth, and toxicity of ciguatera-causing Gambierdiscus toxicus Adachi et Fukuyo. J Exp Mar Biol Ecol. 1988;115:53–65. [Google Scholar]
- 23.McKee DB, Fleming LE, Tamer R, Weisman R, Blythe D. Physician diagnosis and reporting of ciguatera fish poisoning in an endemic area. Harmful Algal Blooms. 2000:451–453. [Google Scholar]
- 24.Chateau-Degat M, Huin-Blondey M, Chinain M, Darius T, Legrand A, Nguyen NL, Laudon F, Chansin R, Dewailly E. Prevalence of chronic symptoms of ciguatera disease in French Polynesian adults. Am J Trop Med Hyg. 2007;77:842–846. [PubMed] [Google Scholar]
- 25.Florida Fish and Wildlife Conservation Commission Exemptions—Do I Need a License or Permit? http://myfwc.com/license/recreational/do-i-need-a-license/ Recreational Hunting and Fishing License and Permit. Available at. Accessed 2013.