Abstract
Objectives
The aim of this study is to assess the contributions of care management as perceived by care managers themselves.
Study Design
Focus groups and interviews with care managers who coordinate care for chronic obstructive pulmonary disease and congestive heart failure patients, as well as patients undergoing major surgery.
Methods
We collected data in focus groups and interviews with 12 care managers working in the Keystone Beacon Community project, including 5 care managers working in hospitals, 2 employed in outpatient clinics and 4 telephoning discharged patients from a Transitions of Care (TOC) call center.
Results
Inpatient care managers believe that (1) ensuring primary care provider follow-up, (2) coordinating appropriate services, (3) providing patient education, and (4) ensuring accurate medication reconciliation have the greatest impact on patient clinical outcomes. In contrast, outpatient and TOC care managers believe that (1) teaching patients the signs and symptoms of acute exacerbations and (2) building effective relationships with patients improve patient outcomes most. Some care management activities were perceived to have greater impact on patients with certain conditions (e.g., outpatient and TOC care managers saw effective relationships as having more impact on patients with COPD). All care managers believed that relationships with patients have the greatest impact on patient satisfaction, while the support they provide clinicians has the greatest impact on clinician satisfaction.
Conclusions
These findings may improve best practice for care managers by focusing interventions on the most effective activities for patients with specific medical conditions.
Keywords: care manager, care coordination, case management, emergency treatment, hospital readmission, patient admission
Introduction
Poor care coordination is associated with negative patient outcomes, including hospital readmissions.[1, 2] Various approaches such as care management, a key component of the patient-centered medical home,[3–5] have been proposed for enhancing care coordination.[4, 6] Some studies have shown benefits of care management programs, such as reductions in 30-day readmissions,[7] acute hospital admissions and emergency department visits.[8] However, other care management programs have failed to achieve reductions in hospitalization and medical costs.[9] This highlights the need for a deeper understanding of the role of care management in improving outcomes.
In care management programs, nurses are often dedicated to managing high-risk patients with chronic diseases, and a few studies have begun to describe the role of care managers.[10–13] Care managers’ activities have been examined and categorized in studies of patients with atrial fibrillation,[10] congestive heart failure (CHF),[10, 12] coronary artery disease (CAD),[10, 12] chronic obstructive pulmonary disease (COPD),[10, 12] diabetes,[10, 12] and prostate cancer.[11] Several categories of activities were found: (1) initial and ongoing assessment of patients and their needs, (2) facilitation, coordination, arrangement, and/or scheduling of services, supplies, treatment, and interventions, (3) monitoring and following up with patients, (4) education of patient and/or family, (5) advocacy for patients, (6) collaborative problem solving and support, and (7) documentation. The specific contribution of each of these categories to patient outcomes is unknown. Therefore, this study aims to identify the specific aspects of their work that care managers perceive as producing benefits for patients and clinicians.
Care managers coordinate care at different stages of the patient journey,[14] including (1) pre-discharge interventions such as patient education and discharge planning, and (2) post-discharge interventions such as timely follow-up with primary care providers. We need, therefore, to understand contributions of care management at different points in the patient journey.
To systematically examine care managers’ activities, we use the work system model developed by Smith and Carayon [15–17] and later expanded into the SEIPS model [18] for application to patient safety. According to the work system model, care managers perform diverse tasks using various tools and technologies, these tasks are performed in various physical environments and influenced by a range of organizational conditions.
Methods
We conducted focus groups and interviews with care managers involved in the Keystone Beacon project. Care coordination in the Keystone Beacon project focuses on patients with CHF and COPD and, in the initial phase of the project, also included patients who had had major surgery such as abdominal, thoracic, and orthopedic surgery. These patients have complex care needs that require significant care coordination and monitoring during their hospitalization and after discharge, including review of medications, coordination of services such as home care, arranging for follow-up outpatient care, and patient education. A unique feature of the Keystone Beacon project is the implementation of health IT-supported care management across healthcare organizations in 5 counties in central Pennsylvania. The goal of Keystone Beacon care coordination is to help patients improve their health and well-being, in turn reducing hospital admissions, re-admissions, and emergency department visits.
The Keystone Beacon care coordination model defined three types of care managers: inpatient, outpatient and transitions of care (TOC). Inpatient care managers work in four participating hospitals and support inpatient and transitional care until discharge. Outpatient care managers work in participating primary care clinics, and manage CHF and COPD patients as long as needed and surgical patients for 30 days post-discharge. TOC care managers support patients whose primary care providers do not have an outpatient care manager, contacting them by telephone for 30 days after hospital discharge, including those in skilled nursing facilities.
Sample
Research participants included all 12 Keystone Beacon care managers who had held their positions for more than one month at the time of data collection. Participation was voluntary. The Institutional Review Board (IRB) of Geisinger Health System approved this research. Ten of the 12 care managers participated in two focus groups, and all 12 care managers were interviewed. Because the activities of inpatient care managers differ from those of outpatient and TOC care managers, two separate focus groups were conducted. Five inpatient care managers and a “float” care manager who covers for inpatient care managers during vacation participated in the first focus group. Two outpatient and two TOC care managers participated in the second focus group. The care managers have 8 to 35 years nursing experience in various clinical domains. Five care managers had experience in case management prior to joining the Keystone Beacon project. All care managers work day shifts on weekdays.
Data collection methods
The objective of the focus groups was for care managers to describe their work activities that contributed to patient outcomes and patient and clinician satisfaction. The main question addressed by the focus groups was “What is it that you do as a care manager that you believe is responsible for preventing [type of condition: COPD, HF or post-surgical] patients from being (re)admitted to the hospital or presenting to the emergency department? Please be as specific as possible.” Care managers were asked to consider all elements of the work system model. To assist them in understanding the question, focus group facilitators provided examples of how care managers’ work can contribute to patient and clinician outcomes using data from prior care manager interviews.
The meeting rooms were organized to facilitate discussion and participation from all care managers. Three posters on the room’s walls displayed the work system model,[17] questions to be addressed by the participants, and the Keystone Beacon project target outcomes. Large blank sheets of white paper were attached to the walls and used to record information gathered from the care managers. Four researchers participated in each focus group as facilitators, timekeeper and note taker.
In each focus group, care managers were given post-it® notepads and sets of matching dot stickers, which were color coded to indicate each of the health conditions targeted by the Keystone Beacon project. The facilitator first asked the care managers to write on post-it® notes the activities that have an impact on COPD patient outcomes, with one activity per note; the care managers then posted the notes on a blank sheet of paper attached to the wall. Subsequently, care managers were asked to use five dot stickers in a matching color to identify the work activities that they considered as having the greatest impact on outcomes for COPD patients. The same procedure was then used for CHF patients, post-surgical patients with co-morbidities, and post-surgical patients without comorbidities. The post-surgical patients were separated at the care managers’ request because patients with and without comorbidities have different care management needs. At the end of the focus group, the care managers used post-it® notes and dot stickers to identify activities that increase patient satisfaction and either increase or decrease clinician satisfaction.
Interviews were conducted with 12 care managers between May 2011 and January 2012. These care managers worked in four hospitals (5 care managers), two clinics (2 care managers) and the TOC (5 care managers). A total of 32 hours of interview data were collected by two data collection teams comprised of two or three human factors engineers and social science researchers. A detailed description of the interview procedure can be found in Carayon et al.[19] For this study, we focused on care managers’ responses to an open-ended question: “What do you think is your role in influencing patient care? How does your role influence patient care for each of the following patient groups: heart failure patients, COPD patients, and post-surgical patients?”
Data analysis
During the focus groups, after identifying aspects of their work that contributed to patient outcomes and patient and clinician satisfaction, care managers combined similar activities into categories and sub-categories for each patient population. After the focus groups, two researchers transcribed the data into a spreadsheet. Three researchers reviewed the categories and made changes when similar activities needed to be grouped or labels for the categories needed to be clarified. This process occurred over 6 meetings that lasted a total of 12 hours. This analysis was complemented by interview data that provided specific instances when care managers believed their work contributed to patient outcomes or patient and clinician satisfaction.
Results
We identified 10 categories of care manager activities that are perceived to influence Keystone Beacon outcomes (see Table 1).
Table 1.
Care Manager Activities Contributing to Outcomes
| Care Manager Activities | Description |
|---|---|
| 1. Ensuring primary care physician (PCP) follow-up and contacting the PCP on behalf of patients | Ensuring that patients have a primary care physician and that follow-up appointments are scheduled within seven days of hospital discharge. Directly following up with primary care physicians when a patient has a question or experiences a problem. |
| 2. Coordinating appropriate services | Ensuring appropriate referrals are in place and contact facilities such as a home health agency or pharmacy to follow-up on patients. Providing patients with contact information for outpatient or TOC3 care managers so that patients can contact them when needed. Scheduling follow-up appointment with a specialist for surgical patient, if necessary. |
| 3. Providing patient education | Providing general education, education on medications, and education on signs and symptoms: e.g., weight gain for CHF4, continued shortness of breath for COPD5, and infection or bleeding for surgery). Teaching patients what to do if signs or symptoms occur. Asking patients whether they have any questions about their disease or condition. |
| 4. Using health information technology | Using case management software, electronic health record systems, and a health information exchange. |
| 5. Ensuring patients have proper equipment | Following up with clinicians and care facilities that provide patients with the required equipment. |
| 6. Performing medication reconciliation | Reviewing list of medications and identifying any discrepancies. |
| 7. Focusing on patients with higher need | Considering culture, education level, and psychosocial conditions of patients when managing their care. |
| 8. Building relationships with patients | Making patients feel valued so that they know someone will follow-up with them after discharge. |
| 9. Supporting or helping clinicians | Contacting doctors. Educating clinicians about the role of Keystone Beacon and the care managers. Identifying and following up on inaccuracies and omissions, and helping clinicians to achieve their goals (e.g., decreasing hospital readmissions). |
| 10. Building trust with clinicians | Interacting with clinicians in order to build trust over time. |
Care manager contributions to patient outcomes and patient and clinician satisfaction
Care managers ensure that patients follow-up with their PCP and contact the PCP on behalf of patients. An outpatient care manager (OP-CM-E6) stated, “That's a big thing that you stress. Don’t wait so long before you get back in [for a follow-up appointment with your PCP] that you end up over in the emergency room. We'd rather see you here first.” Care managers coordinate appropriate services with home health agencies, hospice, skilled nursing facilities, outpatient care managers, or a TOC care manager.
Care managers educate patients on diet, weight monitoring, smoking cessation, discharge instructions, disease management, and prevention of disease exacerbations or complications. For example, an inpatient care manager (IP-CM-C7) said, “[We have an impact by providing] the education, [by] getting in there and talking to them, and [saying] you’re in charge of your own health…. [J]ust that education, trying to teach them about their disease process.” Care managers also educate patients about specific signs and symptoms of disease and associated conditions. An inpatient care manager (IP-CM-C) tells patients, “If you’re getting short of breath, don’t run to the ER right away. Call your doctor, call your manager, and let them know. They can maybe stop it, before you get too bad.” A TOC care manager (TOC-CM1) found education to be important for CHF patients: “Probably the biggest thing would be the education, really focusing on the importance of the daily weights [for CHF patients], and the diet adherence, and the symptoms. Watch for these symptoms. Call if you see these symptoms.”
Care managers use health IT applications, such as the case management software, to communicate with each other and document care activities and patient progress. EHRs provide care managers with access to patient-related information and can also be used for communication with clinicians. Moreover, care managers have access to an HIE to obtain patient-related information from participating facilities, if the patient has provided authorization. Care managers ensure patients have proper equipment or devices needed for condition management.
Care managers perform medication reconciliation. An inpatient care manager (IP-CM-A) said: “Well, I know for a fact that the [mistakes] that were missed with discharge processes probably would've never been caught [without care manager medication reconciliations].”
Care managers focus on specific patients who are at higher risk, such as patients with frequent readmissions, a history of non-compliance, or comorbidities and other patients that they are concerned about. Building effective relationships with patients is another activity that is perceived by care managers to influence patient satisfaction. For example, an inpatient care manager (IP-CM-A) said, “They seem to appreciate somebody being concerned for their well-being while they're in the hospital.” Similarly, a TOC care manager (TOC-CM1) said, “Some of [the patients] are very nice, and they like to hear from you, and to know that somebody cares. And they are appreciative, and they thank you for calling and asking.”
Care managers support and help clinicians. However, their activities can have either a positive or negative impact on clinician satisfaction. For example, ensuring that follow-up appointments with a PCP or specialist have been scheduled and providing clinicians with an extra set of eyes can increase clinician satisfaction. An inpatient care manager (IP-CM-A) said, “When we call [the clinician] and I'll say … you put this in. And, [they will respond] thanks for catching that.” Sometimes when care managers identify corrections to orders, this can have a negative impact on clinician satisfaction because clinicians consider this as interfering with their work. For instance, an inpatient care manager (IP-CM-C) said, “The doctors, there are days [when] there's been med reconciliation that I needed to go over with them. And sometimes they don't like the fact that I've brought to their attention that there's a mistake.”
Care managers build trust with clinicians over time, and they believe this has an impact on clinician satisfaction. For instance, an inpatient care manager (IP-CM-D) said, “After you establish that rapport with that physician in the clinic, he trusted you … because then … you’d look [in the EHR] at what [the patient’s] last labs were.”
Comparing inpatient and outpatient care manager activities
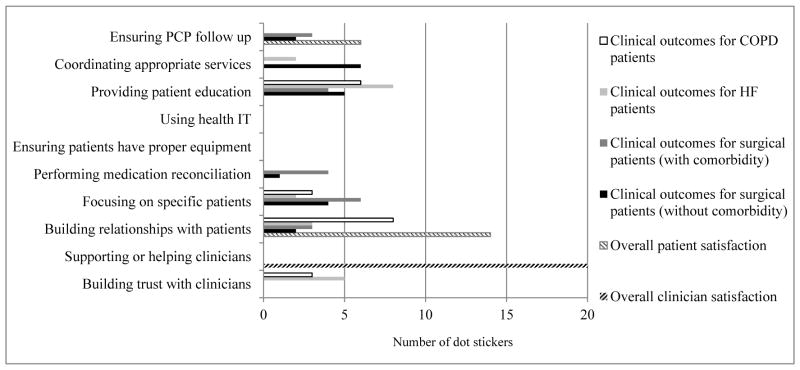
Inpatient care managers perceive a greater impact from activities such as performing medication reconciliation, coordinating appropriate services, and ensuring PCP follow-up, relative to outpatient and TOC care managers (see Figure 1). All care managers perceive that providing patient education and supporting or helping clinicians significantly contribute to outcomes. Outpatient and TOC care managers perceive a greater impact of building relationships with patients, focusing on specific high-risk patients, and building trust with clinicians, when compared to inpatient care managers. Overall, relative to other activities, care managers perceive that the use of health IT has less impact on Keystone Beacon outcomes.
Figure 1.
Perceived impact of inpatient versus outpatient care managers’ activities on Keystone Beacon outcomes
Note: Each of the 10 care managers identified 5 activities that they believed had the most impact on outcomes (using dot stickers). This graph compares the percent of dot stickers assigned by inpatient versus outpatient care managers to each activity.
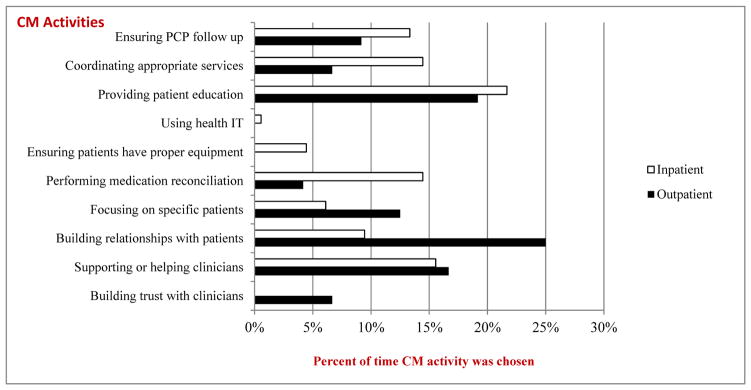
Impact of care manager activities on types of outcomes
Inpatient care managers believe that ensuring PCP follow-up, coordinating appropriate services, providing patient education, and performing medication reconciliation have the greatest impact on patient clinical outcomes; the impact is similar for CHF, COPD, and surgical patients (see Figure 2 and Table A). Supporting or helping clinicians has the greatest impact on clinician satisfaction and building relationships with patients has the greatest impact on patient satisfaction.
Figure 2.
Perceived impact of inpatient care managers’ activities on various types of Keystone Beacon outcomes
Note: Each of the 6 care managers (5 inpatient, 1float) identified 5 activities that they believed had the most impact on outcomes (using dot stickers). A total of 30 activities were identified for different outcomes. This graph shows the number of dot stickers assigned by inpatient care managers to each type of outcome.
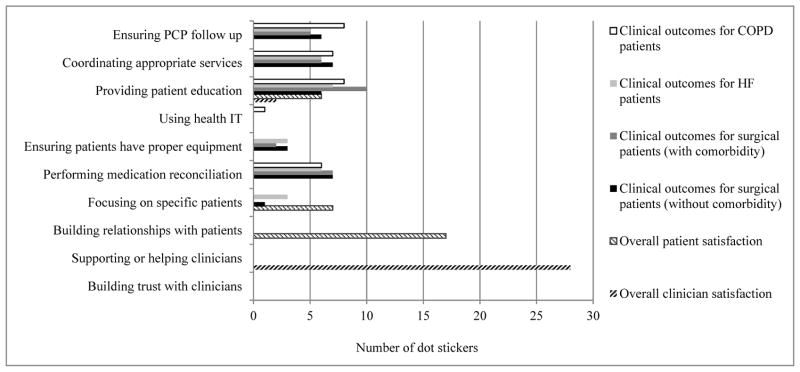
Outpatient and TOC care managers believe that providing patient education, building effective relationships with patients and building trust with clinicians all have a significant impact on patient clinical outcomes, especially for COPD and CHF patients (see Figure 3 and Table B). Reconciling medications and focusing on high-risk patients are believed to affect the clinical outcomes of surgical patients, especially surgical patients with comorbidities. Similar to inpatient care managers, outpatient and TOC care managers also believe that supporting or helping clinicians has the greatest impact on clinician satisfaction and building relationships with patients has the greatest impact on patient satisfaction.
Figure 3.
Perceived impact of outpatient and TOC care managers’ activities on various types of Keystone Beacon outcomes
Note: Each of the 4 care managers (2 outpatient, 2 TOC) identified 5 activities that they believed had the most impact on outcomes (using dot stickers). A total of 20 activities were identified for different outcomes. This graph shows the number of dot stickers assigned by outpatient and TOC care managers to each type of outcome.
Discussion
We identified 10 categories of activities performed by inpatient, outpatient and TOC care managers that they perceive as contributing to patient and clinician outcomes. Six of the 10 categories of care manager activities are similar to those found in previous research:[10–12] ensuring PCP follow-up, providing patient education, ensuring patients have proper equipment, performing medication reconciliation, coordinating appropriate services, and focusing on specific patients. Because we used the work system model [15, 17] as a conceptual framework and systematically examine the care manager work system, we were able to identify new categories of care managers’ activities of importance to patient and clinician outcomes: building relationships with patients, building trust with clinicians, supporting or helping clinicians, and using health IT (i.e. case management software, EHRs and the HIE). These care manager activities contribute to creating management and information continuity of care for CHF and COPD patients. [20]
Care managers perceive the use of health IT as having less impact on Keystone Beacon outcomes as compared to other activities. This may be because health IT plays an indirect role through other activities that are supported or facilitated by the use of health IT. For instance, care managers use health IT to perform medication reconciliation, review patient medical records (e.g., medication list, lab results), and communicate with physicians regarding medication discrepancies. These are care coordination activities that can be supported by health IT. [21]
Our results are in line with findings of Hansen et al. [22] who emphasized that care managers’ interventions may vary in effectiveness across the patient care journey. Task-related activities such as performing medication reconciliation and coordinating appropriate services are perceived by inpatient care managers to have a greater impact on outcomes when compared to outpatient and TOC care managers. On the other hand, activities such as building relationships with patients and building trust with clinicians are perceived by outpatient and TOC care managers to have a greater impact on outcomes, relative to inpatient care managers. This reflects the different focus of care managers in the inpatient and outpatient settings. In the hospital, patients need specific care and inpatient care managers make sure that, for instance, patients receive the proper medications. After discharge, patients need to manage their illness and avoid re-hospitalization. Thus, building relationships with patients enables outpatient care managers to support patients in managing their disease. Relationship building is a key element to support care coordination among chronically ill patients. [23]
Care managers describe how certain activities are more important for outcomes depending on the patient’s condition. For instance, providing patient education is perceived to be more effective for COPD patients as compared to CHF and surgical patients. This result indicates that care managers need to emphasize different activities depending on the patient’s condition.
Because the study was conducted in the context of the Keystone Beacon project, the findings may not be generalizable to other settings. Also, all of the participating care managers had been working in their positions for less than a year; this could have limited their perspective on the potential impact of care management on patient outcomes. On the other hand, most of the care managers had previous work experience relevant to care coordination. Our data on the impact of care management on patient and clinician outcomes are based on the perceptions of care managers. Future research could build on these data and examine the contributions of specific care manager activities on clinical outcomes and patient and clinician satisfaction.
Conclusion
Our study examined the perceived impact of care managers’ work on admissions, readmissions, and emergency room visits of chronically ill patients with CHF and COPD, or those who had major surgery. Results of the study may be helpful to improve the effectiveness of inpatient and outpatient care management. Interventions (e.g., training and resources) can focus on care manager activities that are perceived to have the most significant impact on patient outcomes. Our findings can be used to help care managers tailor their activities to the patient’s setting and condition so that they can better help patients manage their illnesses.
Acknowledgments
The authors would like to thank the care managers who participated in the data collection. Funding for this research provided by the US Office of the National Coordinator for Health IT through the Beacon award program [award No. 90BC001301]. The project was also supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021.
Appendix
Table A.
Frequency with which inpatient care managers perceived their activities as significantly contributing to positive outcomes (N=6)
| Care manager activities | Clinical outcomes by patient type | Satisfaction | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| COPD8 | HF9 | Surgical with comorbidity | Surgical without comorbidity | Patient satisfaction | Clinician satisfaction | |
|
| ||||||
| 1. Ensuring PCP follow-up | 8 | 5 | 5 | 6 | ||
|
| ||||||
| 2. Coordinating appropriate services | 7 | 6 | 6 | 7 | ||
|
| ||||||
| 3. Providing patient education | 8 | 7 | 10 | 6 | 6 | 2 |
|
| ||||||
| 4. Using health IT | 1 | |||||
|
| ||||||
| 5. Ensuring patients have proper equipment | 3 | 2 | 3 | |||
|
| ||||||
| 6. Performing medication reconciliation | 6 | 6 | 7 | 7 | ||
|
| ||||||
| 7. Focusing on specific patients | 3 | 1 | 7 | |||
|
| ||||||
| 8. Building relationships with patients | 17 | |||||
|
| ||||||
| 9. Supporting or helping clinicians | 28 | |||||
|
| ||||||
| 10. Building trust with clinicians | ||||||
|
| ||||||
| Total | 30 | 30 | 30 | 30 | 30 | 30 |
Note: Numbers in the table are the total number of “dots” used by care managers to indicate the contribution of activities to outcomes. Therefore, since each of the 6 care managers allocated 5 dot stickers to each category, a total of 30 activities were identified.
Table B.
Frequency with which outpatient and TOC care manager perceived their activities as significantly contributing to positive outcomes (N=4)
| Care manager activities | Clinical outcomes by patient type | Satisfaction | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| COPD10 | HF11 | Surgical with comorbidity | Surgical without comorbidity | Patient satisfaction | Clinician satisfaction | |
|
| ||||||
| 1. Ensuring PCP follow-up | 3 | 2 | 6 | |||
|
| ||||||
| 2. Coordinating appropriate services | 2 | 6 | ||||
|
| ||||||
| 3. Providing patient education | 6 | 8 | 4 | 5 | ||
|
| ||||||
| 4. Using health IT | ||||||
|
| ||||||
| 5. Ensuring patients have proper equipment | ||||||
|
| ||||||
| 6. Performing medication reconciliation | 4 | 1 | ||||
|
| ||||||
| 7. Focusing on specific patients | 3 | 2 | 6 | 4 | ||
|
| ||||||
| 8. Building relationships with patients | 8 | 3 | 3 | 2 | 14 | |
|
| ||||||
| 9. Supporting or helping clinicians | 20 | |||||
|
| ||||||
| 10. Building trust with clinicians | 3 | 5 | ||||
|
| ||||||
| Total | 20 | 20 | 20 | 20 | 20 | 20 |
Note: Numbers in the table are the total number of “dots” used by care managers to indicate the contribution of activities to outcomes. Therefore, since each of the 4 care managers allocated 5 dot stickers to each category, a total of 20 activities were identified.
Footnotes
Transitions of Care
Congestive Heart Failure
Chronic Obstructive Pulmonary Disease
Outpatient care manager at health care organization E
Inpatient care manager at hospital C
Chronic Obstructive Pulmonary Disease
Heart Failure
Chronic Obstructive Pulmonary Disease
Heart Failure
Contributor Information
Pascale Carayon, Email: carayon@engr.wisc.edu.
Ann Schoofs Hundt, Email: ahundt@cqpi.engr.wisc.edu.
Peter Hoonakker, Email: phoonakker@cqpi.engr.wisc.edu.
Sarah Kianfar, Email: skianfar@cqpi.engr.wisc.edu.
Bashar Alyousef, Email: bashar.m.alyousef@gmail.com.
Doreen Salek, Email: dmsalek@thehealthplan.com.
Randi Cartmill, Email: rcartmill@cqpi.engr.wisc.edu.
James M. Walker, Email: james.m.walker@siemens.com.
Janet Tomcavage, Email: jtomcavage@thehealthplan.com.
References
- 1.O'Malley AS. Tapping the unmet potential of health information technology. New England Journal of Medicine. 2011;364(12):1090–1091. doi: 10.1056/NEJMp1011227. [DOI] [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. New England Journal of Medicine. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3.Stange KC, Nutting PA, Miller WL, Jaen CR, Crabtree BF, Flocke SA, Gill JM. Defining and measuring the patient-centered medical home. Journal of general internal medicine. 2010;25(6):601–612. doi: 10.1007/s11606-010-1291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilfillan RJ, Tomcavage J, Rosenthal MB, et al. Value and the medical home: effects of transformed primary care. American Journal of Managed Care. 2010;16(8):607–614. [PubMed] [Google Scholar]
- 5.Taylor EF, Machta RM, Meyers DS, Genevro J, Peikes DN. Enhancing the primary care team to provide redesigned care: The roles of practice facilitators and care managers. Annals of Family Medicine. 2013;11(1):80–83. doi: 10.1370/afm.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McDonald KM, Schultz E, Albin L, Pineda N, Lonhart J, Sundaram V, Smith-Spangler C, Brustrom J, Malcolm E. Care Coordination Measures Atlas. Rockville, MD: Agency for Healthcare Research and Quality; 2010. Contract No.: AHRQ Publication No. 11–0023-EF. [Google Scholar]
- 7.Harrison PL, Hara PA, Pope JE, Young MC, Rula EY. The impact of postdischarge telephonic follow-up on hospital readmissions. Population Health Management. 2011;14(1):27–32. doi: 10.1089/pop.2009.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steele GD, Haynes JA, Davis DE, Tomcavage J, Stewart WF, Graf TR, Paulus RA, Weikel K, Shikles J. How Geisinger's advanced medical home model argues the case for rapid-cycle innovation. Health Affairs. 2010;29(11):2047–2053. doi: 10.1377/hlthaff.2010.0840. [DOI] [PubMed] [Google Scholar]
- 9.Boult C, Reider L, Leff B, et al. The effect of guided care teams on the use of health services: Results from a cluster-randomized controlled trial. Archives of Internal Medicine. 2011;171(5):460–466. doi: 10.1001/archinternmed.2010.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oliva NL. A closer look at nurse case management of community-dwelling older adults: Observations from a longitudinal study of care coordination in the chronically Ill. Professional Case Management. 2010;15(2):90–100. doi: 10.1097/NCM.0b013e3181bc85a6. [DOI] [PubMed] [Google Scholar]
- 11.Maliski SL, Clerkin B, Litwin MS. Describing a nurse case manager intervention to empower low-income men with prostate cancer. Oncology Nursing Forum. 2004;31(1):57–64. doi: 10.1188/04.ONF.57-64. [DOI] [PubMed] [Google Scholar]
- 12.Brown RS, Peikes D, Peterson G, Schore J, Razafindrakoto CM. Six features of medicare coordinated care demonstration programs that cut hospital admissions of high-risk patients. Health Affairs. 2012;31(6):1156–1166. doi: 10.1377/hlthaff.2012.0393. [DOI] [PubMed] [Google Scholar]
- 13.Hoonakker PLT, Carayon P, Kern L, et al. Inside the Black Box: What do inpatient case managers do?. 2013 Symposium on Human Factors and Ergonomics in Health Care; March 11–13, 2013; Baltimore, MD. 2013. [Google Scholar]
- 14.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: A systematic review. Annals of internal medicine. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 15.Carayon P. The Balance Theory and the work system model... Twenty years later. International Journal of Human-Computer Interaction. 2009;25(5):313–327. [Google Scholar]
- 16.Carayon P, Smith MJ. Work organization and ergonomics. Applied Ergonomics. 2000;31:649–662. doi: 10.1016/s0003-6870(00)00040-5. [DOI] [PubMed] [Google Scholar]
- 17.Smith MJ, Carayon-Sainfort P. A balance theory of job design for stress reduction. International Journal of Industrial Ergonomics. 1989;4(1):67–79. [Google Scholar]
- 18.Carayon P, Hundt AS, Karsh B-T, Gurses AP, Alvarado CJ, Smith M, Brennan PF. Work system design for patient safety: The SEIPS model. Quality & Safety in Health Care. 2006;15(Supplement I):i50–i58. doi: 10.1136/qshc.2005.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carayon P, Alyousef B, Hoonakker P, et al. Challenges to care coordination posed by the use of multiple health IT applications. Work: A Journal of Prevention, Assessment and Rehabilitation. 2012;41(0):4468–4473. doi: 10.3233/WOR-2012-0746-4468. [DOI] [PubMed] [Google Scholar]
- 20.van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: A systematic and critical review. Journal of evaluation in clinical practice. 2010;16(5):947–956. doi: 10.1111/j.1365-2753.2009.01235.x. [DOI] [PubMed] [Google Scholar]
- 21.Rudin RS, Bates DW. Let the left hand know what the right is doing: A vision for care coordination and electronic health records. Journal of the American Medical Informatics Association. 2014;21(1):13–16. doi: 10.1136/amiajnl-2013-001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: A systematic review. Annals of Internal Medicine. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 23.Cramm JM, Nieboer AP. Relational coordination promotes quality of chronic care delivery in Dutch disease-management programs. Health Care Management Review. 2012;37(4):301–309. doi: 10.1097/HMR.0b013e3182355ea4. [DOI] [PubMed] [Google Scholar]