Abstract
Background
Disclosure of a cancer diagnosis to patients is a major problem for physicians in Lebanon. Our survey aimed to identify the attitudes of patients, families and friends, nurses, and physicians regarding disclosure of a cancer diagnosis.
Methods
Study participants included 343 physicians, nurses, cancer patients, families, and friends from clinics in two major hospitals in Lebanon. All completed a 29-item questionnaire that assessed, by demographic group, the information provided about cancer, opinions about the disclosure of the diagnosis to cancer patients, perceived consequences to patients, and the roles of family, friends, and religion.
Results
Overall, 7.8% of the patients were convinced that cancer is incurable. Nearly 82% preferred to be informed about their diagnosis. Similarly, 83% of physicians were in favour of disclosing a cancer diagnosis to their patients. However, only 14% of the physicians said that they revealed the truth to the patients themselves, with only 9% doing so immediately after confirmation of the diagnosis. Disclosure of a cancer diagnosis was preferred before the start of the treatment by 59% of the patients and immediately after confirmation of the diagnosis by 72% of the physicians. Overall, 86% of physicians, 51% of nurses, and 69% of patients and their families believed that religion helped with the acceptance of a cancer diagnosis. A role for family in accepting the diagnosis was reported by 74% of the patients, 56% of the nurses, and 88% of the physicians. All participants considered that fear was the most difficult feeling (63%) experienced by cancer patients, followed by pain (29%), pity (8%), and death (1%), with no statistically significant difference between the answers given by the participant groups.
Conclusions
The social background in Lebanese society is the main obstacle to revealing the truth to cancer patients. Lebanese patients seem to prefer direct communication of the truth, but families take the opposite approach. Physicians also prefer to communicate the reality of the disease at the time of diagnosis, but in actuality, they instead disclose it progressively during treatment. Faith is helpful for acceptance of the diagnosis, and families play a key role in the support of the patients. An open discussion involving all members of society is necessary to attain a better understanding of this issue and to promote timely disclosure of a cancer diagnosis.
Keywords: Communication, diagnosis, families, nurses, patients, physicians, truth disclosure
INTRODUCTION
The announcement of a diagnosis of cancer is difficult for physicians, patients, and their families alike1. However, as most in the medical community now agree2,3, every medical profession must give bad, sad, and difficult information to patients and their families. Unfortunately, too many patients leave their consultations with an insufficient understanding of their situation, diagnosis, and prognosis4.
Physicians have difficulty breaking bad news for many reasons. Research shows that those who feel insufficiently trained in communication skills experience significantly higher levels of distress when faced with patient suffering5. Another concern is how the bad news will affect the patient6. Physicians also consider breaking bad news to be an unpleasant task, because they do not wish to take hope away from their patients. They might be fearful of the patient’s or family’s reaction to the news, or uncertain about how to deal with an intense emotional response6. Other reasons that physicians tend to avoid disclosing the truth to cancer patients include lack of time, desire to avoid painful discussions, an overly optimistic view of the effectiveness of current therapies, and collusion between physicians and patients7.
Parties to the communication process include physicians, nurses, families, and the patients themselves8. Culture and religious beliefs play a major role with respect to the influence of each party9. In Western countries, physicians are less likely to withhold unfavourable information from the patient at the family’s request10; in Middle Eastern countries, the patient is not autonomous11, and physicians tend to address the family before disclosing any hurtful truth to the patient. But regardless of culture and origin, several studies have shown that 50%–90% of cancer patients want all possible information, both good and bad12–15. Optimal delivery of bad news is, in turn, associated with increased patient satisfaction4 and better adjustment to cancer4,6.
Disclosing a cancer diagnosis and the associated prognosis is a recurrent subject in Western countries. The growing interest in this area has therefore led to the publication of guidelines intended to help clinicians with this critical task6,16–18. By contrast, specific data of this kind for Middle Eastern medical communities is lacking. Moreover, Lebanese doctors and nurses dealing with cancer patients have not been exposed to formal training in medical ethics and breaking bad news. Given those factors, we conducted a survey whose main goal was to investigate the attitudes of patients, their families, and their physicians in Lebanon about the disclosure to patients of a cancer diagnosis and prognosis. The secondary objectives were to highlight the interest of patients in Lebanon (as a representative country of the Middle East) for knowing their true diagnosis, to define an appropriate method of disclosing diagnosis and prognosis in a Middle Eastern community, to describe the factors that could help in revealing the truth, and finally, to discuss what would help patients to accept their cancer diagnosis.
METHODS
Study Design
A cross-sectional survey was conducted over 12 months in two major hospitals in Lebanon. Neither institution has guidelines about the disclosure of a diagnosis or prognosis of cancer.
Target Population
All parties involved in the communication process—and therefore involved in the disclosure of a patient’s diagnosis or prognosis—were targeted. All oncologists affiliated with the Lebanese Order of Physicians were also addressed. An initial convenience sample of 362 subjects (65 oncologists, 100 nurses, 90 cancer patients, and 107 family members or friends) was collected. Before the subjects were interviewed, the purpose of the study was communicated, and verbal consent was obtained, with assurance of autonomy and anonymity in survey responses.
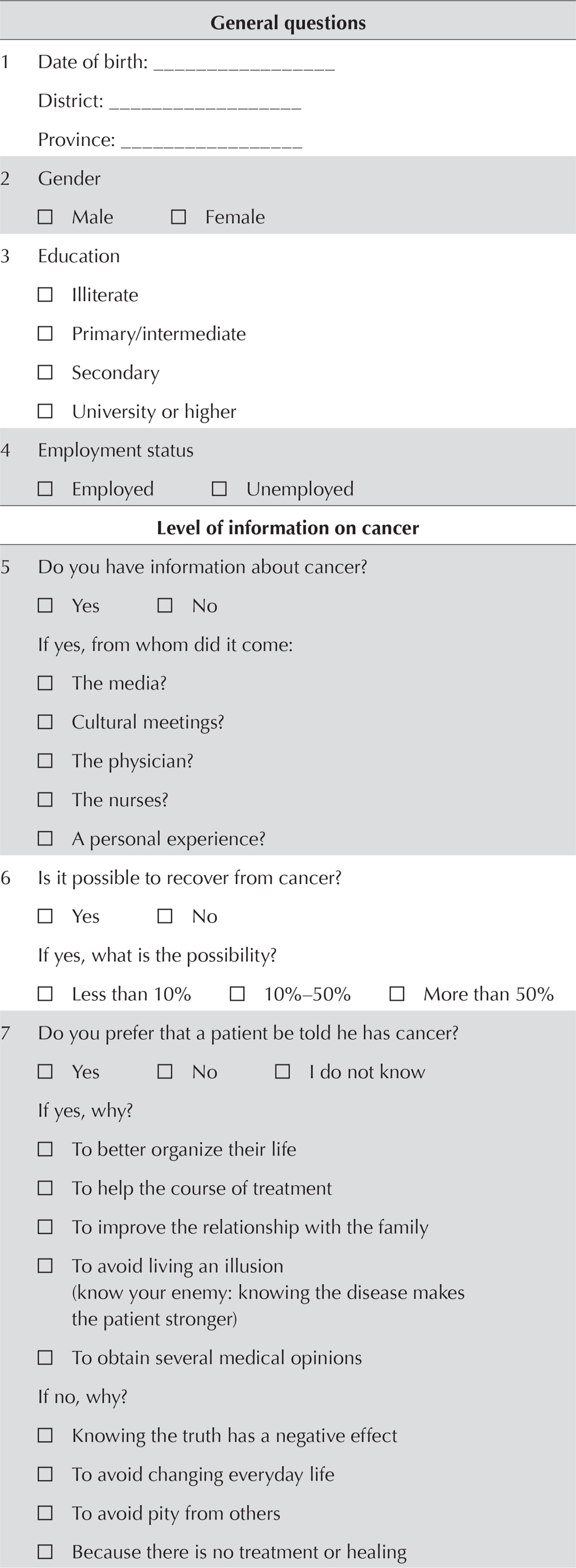
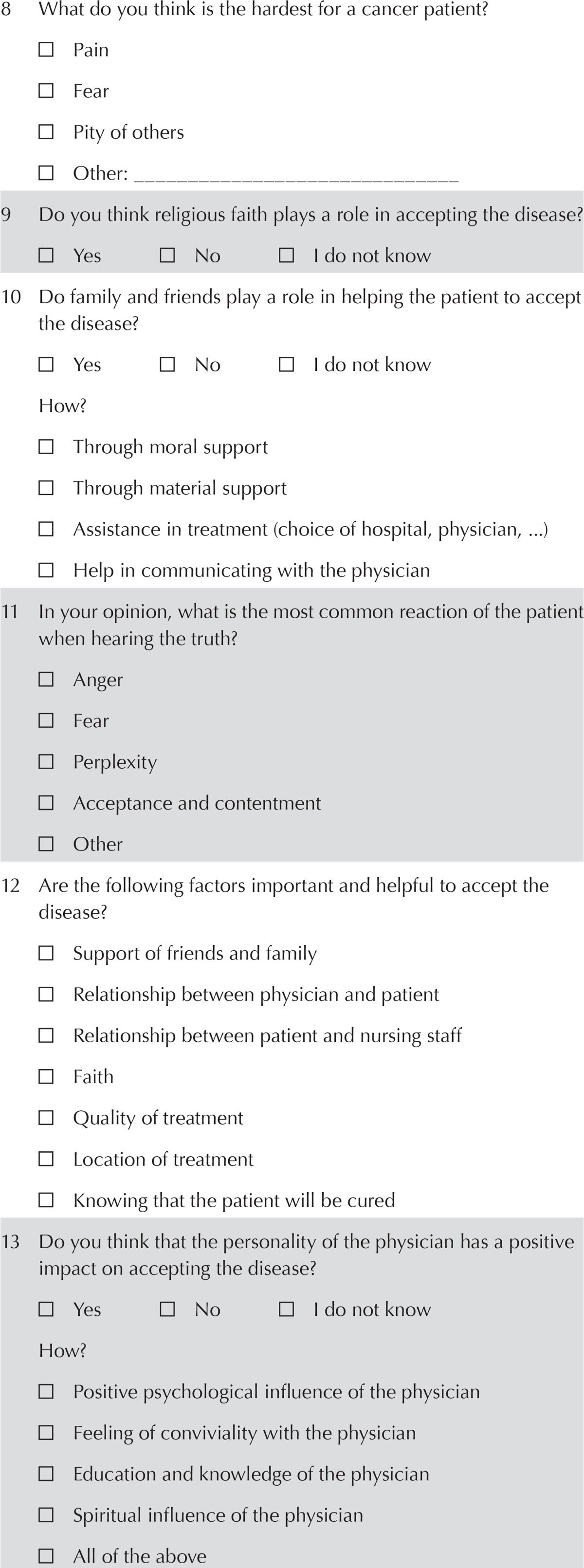
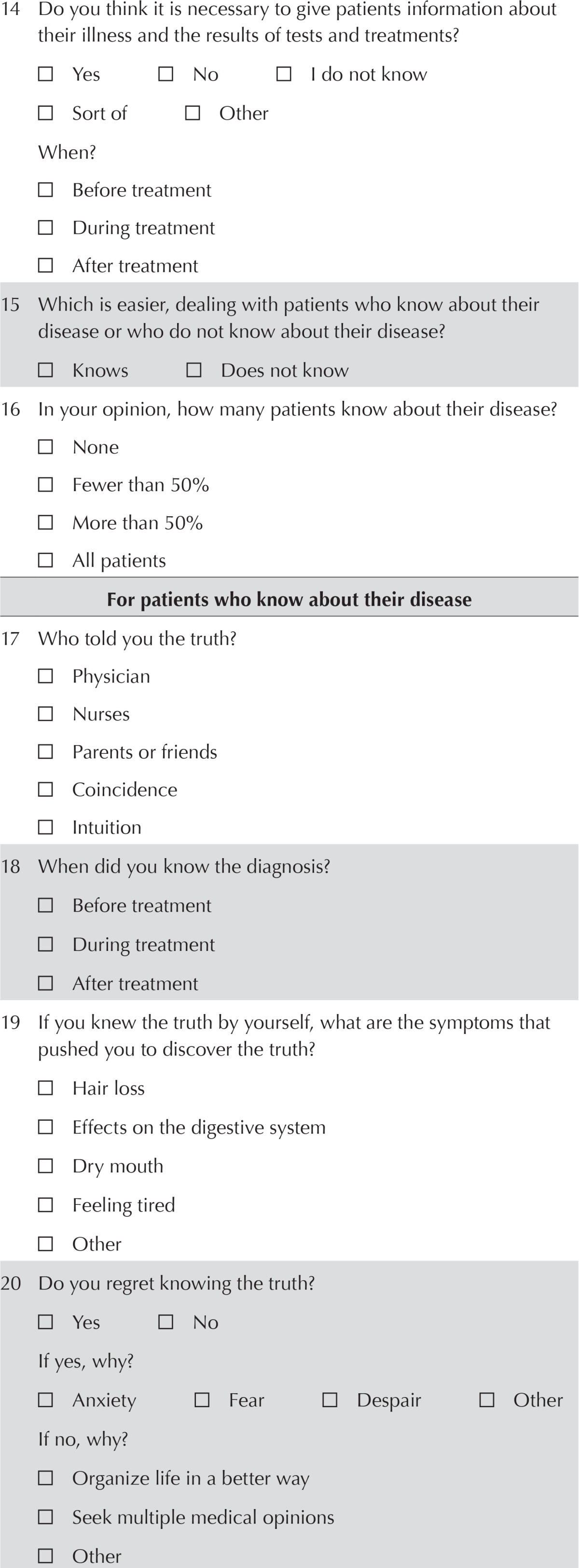
Survey Tool
In the absence of guidelines for the disclosure of cancer-related information in Middle Eastern countries, we developed a self-report questionnaire composed of 29 multiple-choice questions (Table i) based on validated questionnaires described by Baile et al.17. Questions were formulated based on a thorough review of earlier studies published in Europe, Asia, and the United States concerning disclosure of a diagnosis or prognosis to cancer patients10–13. However, for some sensitive questions and topics, we took into consideration the specificity of Middle Eastern culture and beliefs—for example, the influence of religion and faith in disclosing a cancer diagnosis, and the role of friends and family in decision-making.
TABLE I.
Questionnaire (translated from the Arabic)
| General questions | ||||
|---|---|---|---|---|
| 1 | Date of birth: _________________ | |||
| District: __________________ | ||||
| Province: _________________ | ||||
| 2 | Gender | |||
| □ Male | □ Female | |||
| 3 | Education | |||
| □ Illiterate | ||||
| □ Primary/intermediate | ||||
| □ Secondary | ||||
| □ University or higher | ||||
| 4 | Employment status | |||
| □ Employed | □ Unemployed | |||
| Level of information on cancer | ||||
| 5 | Do you have information about cancer? | |||
| □ Yes | □ No | |||
| If yes, from whom did it come: | ||||
| □ The media? | ||||
| □ Cultural meetings? | ||||
| □ The physician? | ||||
| □ The nurses? | ||||
| □ A personal experience? | ||||
| 6 | Is it possible to recover from cancer? | |||
| □ Yes | □ No | |||
| If yes, what is the possibility? | ||||
| □ Less than 10% | □ 10%–50% | □ More than 50% | ||
| 7 | Do you prefer that a patient be told he has cancer? | |||
| □ Yes | □ No | □ I do not know | ||
| If yes, why? | ||||
| □ To better organize their life | ||||
| □ To help the course of treatment | ||||
| □ To improve the relationship with the family | ||||
| □ To avoid living an illusion (know your enemy: knowing the disease makes the patient stronger) | ||||
| □ To obtain several medical opinions | ||||
| If no, why? | ||||
| □ Knowing the truth has a negative effect | ||||
| □ To avoid changing everyday life | ||||
| □ To avoid pity from others | ||||
| □ Because there is no treatment or healing | ||||
| 8 | What do you think is the hardest for a cancer patient? | |||
| □ Pain | ||||
| □ Fear | ||||
| □ Pity of others | ||||
| □ Other: ______________________________ | ||||
| 9 | Do you think religious faith plays a role in accepting the disease? | |||
| □ Yes | □ No | □ I do not know | ||
| 10 | Do family and friends play a role in helping the patient to accept the disease? | |||
| □ Yes | □ No | □ I do not know | ||
| How? | ||||
| □ Through moral support | ||||
| □ Through material support | ||||
| □ Assistance in treatment (choice of hospital, physician, ...) | ||||
| □ Help in communicating with the physician | ||||
| 11 | In your opinion, what is the most common reaction of the patient when hearing the truth? | |||
| □ Anger | ||||
| □ Fear | ||||
| □ Perplexity | ||||
| □ Acceptance and contentment | ||||
| □ Other | ||||
| 12 | Are the following factors important and helpful to accept the disease? | |||
| □ Support of friends and family | ||||
| □ Relationship between physician and patient | ||||
| □ Relationship between patient and nursing staff | ||||
| □ Faith | ||||
| □ Quality of treatment | ||||
| □ Location of treatment | ||||
| □ Knowing that the patient will be cured | ||||
| 13 | Do you think that the personality of the physician has a positive impact on accepting the disease? | |||
| □ Yes | □ No | □ I do not know | ||
| How? | ||||
| □ Positive psychological influence of the physician | ||||
| □ Feeling of conviviality with the physician | ||||
| □ Education and knowledge of the physician | ||||
| □ Spiritual influence of the physician | ||||
| □ All of the above | ||||
| 14 | Do you think it is necessary to give patients information about their illness and the results of tests and treatments? | |||
| □ Yes | □ No | □ I do not know | ||
| □ Sort of | □ Other | |||
| When? | ||||
| □ Before treatment | ||||
| □ During treatment | ||||
| □ After treatment | ||||
| 15 | Which is easier, dealing with patients who know about their disease or who do not know about their disease? | |||
| □ Knows | □ Does not know | |||
| 16 | In your opinion, how many patients know about their disease? | |||
| □ None | ||||
| □ Fewer than 50% | ||||
| □ More than 50% | ||||
| □ All patients | ||||
| For patients who know about their disease | ||||
| 17 | Who told you the truth? | |||
| □ Physician | ||||
| □ Nurses | ||||
| □ Parents or friends | ||||
| □ Coincidence | ||||
| □ Intuition | ||||
| 18 | When did you know the diagnosis? | |||
| □ Before treatment | ||||
| □ During treatment | ||||
| □ After treatment | ||||
| 19 | If you knew the truth by yourself, what are the symptoms that pushed you to discover the truth? | |||
| □ Hair loss | ||||
| □ Effects on the digestive system | ||||
| □ Dry mouth | ||||
| □ Feeling tired | ||||
| □ Other | ||||
| 20 | Do you regret knowing the truth? | |||
| □ Yes | □ No | |||
| If yes, why? | ||||
| □ Anxiety | □ Fear | □ Despair | □ Other | |
| If no, why? | ||||
| □ Organize life in a better way | ||||
| □ Seek multiple medical opinions | ||||
| □ Other | ||||
| For nurses | ||||
| 21 | If patients ask you a question about their treatment and they are unaware of their disease, do you tell them the truth? | |||
| □ Yes | □ No | □ I do not know | ||
| 22 | If your answer is no, to whom you refer the matter? | |||
| □ The physician | ||||
| □ Another nurse who has more experience | ||||
| □ A family member | ||||
| □ Other: _______________________________ | ||||
| For physicians | ||||
| 23 | In which stage of disease progression do you prefer to inform the patient about the truth? | |||
| □ Immediately after confirmation of the diagnosis | ||||
| □ During treatment | ||||
| □ After treatment | ||||
| □ At the patient’s request | ||||
| 24 | To whom you resort in the first stage to deliver the diagnosis? | |||
| □ Patient | □ Parents | □ Friends | ||
| 25 | What are the standards adopted in delivering the diagnosis? | |||
| □ Age of the patient | ||||
| □ Educational background of the patient | ||||
| □ Seriousness of the disease (curable or not) | ||||
| □ Stage of the disease | ||||
| □ Desire of parents | ||||
| □ Faith | ||||
| □ Other: ______________________________ | ||||
| 26 | What are the obstacles that you encounter when you tell the truth? | |||
| □ Psychosomatic consequences for the patient | ||||
| □ Family’s opposition to informing the patient | ||||
| □ Fear of not following the treatment | ||||
| □ Evasion of the burden of pain | ||||
| □ Other | ||||
| 27 | Do you tell the patient about the diagnosis? | |||
| □ Directly | □ Progressively | |||
| 28 | Do you change the way you interact with the patient depending on the patient’s condition? | |||
| □ Yes | □ No | |||
| 29 | Do you tell the whole truth about healing? | |||
| □ In all cases | □ In some cases (curable, incurable) | |||
Survey responses were collected from patients in hospitals; from oncologists by direct questioning, e-mail, and courier; from families in hospital; and from nurses in hospital oncology departments.
The questionnaire was developed in Arabic (the mother tongue in Lebanon), simplified because of the diverse socio-demographic backgrounds of the participants and to reduce bias and the incidence of unanswered questions. Some questions were addressed to all participants; others were specific to the category of each participant. Depending on the question, participants had to either write short answers or mark checkboxes.
Data Collected
The questionnaire had five sections:
□ Demographic variables: Date and place of birth, sex, education level, and profession were collected from all participants.
□ Level of information about cancer: This series of questions was addressed to all participants involved in the truth-telling process. However, it was obvious that question 5, “Do you have information on cancer? And how,” was not addressed to physicians. The data gathered in this section included information about cancer and the source of that information; disease curability; disclosure of the diagnosis to patients; the role of faith; acceptance of the truth by family, friends, and physicians; the patient’s reaction after knowing the truth; factors that help to accept a cancer diagnosis; the importance of disclosing; the actual diagnosis and treatment side effects; ease of communication with the cancer patient (depending on awareness or unawareness of the diagnosis); and the percentage of patients who know their diagnosis.
□ Specific questions for patients aware of their diagnosis
□ Specific questions for nurses
□ Specific questions for physicians
Statistical Analysis
Descriptive statistics are used to describe the general profile of the four categories of participants (oncologists, nurses, cancer patients, and their families and friends) and to describe the patterns of information disclosure. Bivariate chi-square analysis was used to test the differences between participant groups with respect to disclosure of information about cancer to patients and to examine the determinants of information disclosure. The Fisher exact test was used in cases of small numbers. The significance level was set at 5%, and p values of observations were two-sided. The statistical analysis was carried out using the SPSS software application (version 16.0 for Windows: SPSS, Chicago, IL, U.S.A.)
Ethics Considerations
The study was approved by the ethics committees of the participating institutions. The nature and purpose of the study were explained to all participants. It was emphasized that participation was voluntary and that the interview could be stopped at any time. Verbal consent was obtained before adult participants were interviewed, respecting their autonomy and anonymity. Verbal consent and completion of each patient interview were witnessed by the physicians, the nursing staff, and the family members. We included a mechanism for tracking participants who were approached about the study and who provided verbal consent. The study results are reported in aggregate. The ethics committees considered this observational study to be a less-than-minimal-risk study given that participants were exposed to no known physical, emotional, psychological, or economic risk, and no special populations (for instance, minors, prisoners, pregnant women) were involved. The survey required no specific consultation or invasive procedures, and no administration of any investigational product was involved. The study did not affect the clinical management of the patients. The ethics committees therefore approved the consent procedure as already outlined.
RESULTS
Response Rates
During the 12-month study period, 362 individuals were approached for study participation on a “first-come” basis during the study period, and 343 agreed to participate. Cancer patients constituted 25% of the people approached (n = 90) and 26% of the participants (n = 90); oncologists and other specialists constituted 18% of the people approached (n = 65) and 13% of the participants (n = 46). Reasons for refusal to participate in the survey included anxiety and alienation from society for the patients, and time constraints for the physicians. Response rates among nurses in the oncology and other departments, and among the family and friends of patients were both 100% (n = 100 nurses, and n = 107 family or friends).
Demographic Variables
The age of the participants ranged from 21 to 79 years. Table ii summarizes the demographic characteristics of all participants.
TABLE II.
Demographic characteristics by participant group
| Characteristic | Participant group [n (%)] | ||||
|---|---|---|---|---|---|
|
| |||||
| Physicians | Nurses | Patients | Family and friends | Totala | |
| Sex | |||||
| Men | 38 (90.5) | 30 (30.3) | 21 (23.9) | 66 (62.3) | 155 (46.3) |
| Women | 4 (9.5) | 69 (69.7) | 67 (76.1) | 40 (37.7) | 180 (53.7) |
| Education | |||||
| Illiterate | — | — | 13 (15.3) | 6 (5.7) | 20 (6.0) |
| Primary or intermediate | — | — | 38 (44.7) | 29 (27.4) | 70 (20.9) |
| Secondary | — | — | 24 (28.2) | 36 (34.0) | 77 (23.0) |
| University or higher | — | — | 10 (11.8) | 35 (33.0) | 168 (50.2) |
| Employment status | |||||
| Employed | 5 (21.7) | 95 (96.0) | 21 (27.33) | 65 (62.5) | 186 (61.4) |
| Unemployed | 18 (78.3) | 4 (4.0) | 56 (72.7) | 39 (37.5) | 117 (38.6) |
Because of missing data, does not always add to 343.
Level of Information on Cancer
Having information about cancer was reported by 82% of patients, their families, and their friends, and by all the nurses. Their sources of information were the media (66% and 9% respectively), cultural meetings (12% and 20%), personal experience (11% and 9%), physicians (8% and 20%), and nurses (4% and 42%).
In response to the question concerning the curability of cancer, 92% of the patients and their families, 44% of the nurses, and 87% of the physicians considered cancer to be curable. When they answered “yes” to curability, participants were asked to choose a curability rate. Beliefs about the rate of curability varied considerably. Some participants—51% of patients and their families, 47% of nurses, and 16% of physicians—thought that the likelihood of cure was less than 10%. Others—18% of patients and their families, 33% of nurses, and 16% of physicians—thought that 50% of cancers were curable.
In regard to preferences about disclosing a cancer diagnosis, we observed no statistically significant differences between the four participant groups, with 84% of participants overall reporting that they preferred truthful disclosure of a cancer diagnosis to the patient. Table iii shows the reasons for disclosing or concealing the truth. The participants who preferred revealing the diagnosis differed significantly with respect to the 5 possible reasons for disclosure (p = 0.003); they did not differ significantly about the 4 possible reasons for concealment.
TABLE III.
Disclosure of information about cancer and related variables by participant type
| Variable | Participant group [n (%)] | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Physicians | Nurses | Patients | Family and friends | Total | p Valuea | |
| Disclosure preference | 0.121 | |||||
| Yes | 38 (82.6) | 84 (87.5) | 79 (87.8) | 82 (76.6) | 283 (83.5) | |
| No/do not know | 8 (17.4) | 12 (12.5) | 11 (12.2) | 25 (23.4) | 56 (16.5) | |
| Reasons for disclosing | 0.003 | |||||
| Better organize remaining life | 28 (73.7) | 52 (57.1) | 34 (44.2) | 35 (42.7) | 149 (51.7) | |
| Help the course of treatment | 9 (23.7) | 27 (29.7) | 15 (19.5) | 24 (29.3) | 75 (26.0) | |
| Improve family relationships | 0 (0.0) | 0 (0.0) | 4 (5.2) | 2 (2.4) | 6 (2.1) | |
| Avoid living an illusion | 1 (2.6) | 11 (12.1) | 20 (26.0) | 16 (19.5) | 48 (16.7) | |
| Take several medical opinions | 0 (0.0) | 1 (1.1) | 4 (5.2) | 5 (6.1) | 10 (3.5) | |
| Reasons for not disclosing | 0.060 | |||||
| Negative effect of knowing the truth | 4 (66.7) | 7 (53.9) | 3 (42.9) | 14 (73.7) | 28 (62.2) | |
| Avoid changing everyday life | 2 (33.35) | 5 (38.5) | 0 (0.0) | 2 (10.5) | 9 (20.0) | |
| Avoid pity from others | 0 (0.0) | 0 (0.0) | 2 (28.6) | 3 (15.8) | 5 (11.1) | |
| No treatment or healing is available | 0 (0.0) | 1 (7.7) | 2 (28.6) | 0 (0.0) | 3 (6.7) | |
| Detailed information about the disease given | 0.006 | |||||
| Yes | 3 (6.5) | 10 (10.0) | 4 (4.6) | 21 (19.8) | 38 (11.2) | |
| No | 43 (93.5) | 90 (90.0) | 84 (95.5) | 85 (80.2) | 302 (88.8) | |
| Hardest for the patient to confront | 0.174 | |||||
| Pain | 15 (32.6) | 34 (34.0) | 28 (31.5) | 19 (18.1) | 96 (28.2) | |
| Fear | 29 (63.0) | 61 (61.0) | 53 (59.6) | 71 (67.6) | 214 (62.9) | |
| Pity of others | 2 (4.3) | 4 (4.0) | 7 (7.9) | 13 (12.4) | 26 (7.6) | |
| Other (death) | 0 (0.0) | 1 (1.0) | 1 (1.1) | 2 (1.9) | 4 (1.2) | |
| Estimation of patients aware of their diagnosis | 0.001 | |||||
| Fewer than 50 | 18 (39.1) | 71 (71.7) | 49 (56.3) | 71 (66.4) | 209 (61.7) | |
| More than 50 | 28 (60.9) | 28 (28.3) | 38 (43.7) | 36 (33.6) | 130 (38.3) | |
Values in boldface type are significant at the 5% level.
By contrast, 89% of participants overall were against giving detailed information about the disease to the patient. However, significant differences between the groups were evident, with families and friends of cancer patients being more in favour than the other groups of withholding details (20% of nurses, 10% of physicians, 7% of patients, and 5% of families; p = 0.006, Table iii). Moreover, where 59% of patients considered that disclosure would be appropriate before treatment, 50% of families and friends preferred disclosure after treatment. Nurses and physicians were equally favourable to disclosing the diagnosis to patients during treatment (52%).
We also compared participant answers about the most difficult issues for cancer patients to confront. Our findings revealed that fear was the most difficult issue (63%), followed by pain (29%), pity (8%), and death (1%), with no statistically significant differences between the answers given by the participant groups (Table iii).
A nonsignificant difference of opinion about the role of religion in the acceptance of illness between the participant groups emerged (69% of patients and their families and friends, 51% of nurses, and 86% of physicians). Responses about the role of family were similar, with 74% of patients and of families, 57% of nurses, and 86% of physicians stating that family helped patients to cope with the impact of a cancer diagnosis. In that context, all groups agreed that role of family implied helping with communication with the oncologist (14%), choosing the hospital for treatment and the physician (18%), providing material support (23%), and providing moral support (44%).
We also observed nonsignificant differences between the participant groups with respect to reaction to knowing the diagnosis. Comparing the reactions of nurses with the reactions of patients and family members, “perplexity” was the most common reaction in the patient and family groups (35% for nurses), followed by fear at 33% (28% for nurses), anger at 22% (14% for nurses), and acceptance at 2% (14% for nurses). Physicians reported that cancer patients express mainly fear (57%) and said that no one accepts the truth.
In looking at factors correlated with acceptance of the diagnostic truth, patients and their families thought that the quality of treatment played the most important role in facilitating acceptance (37%), followed by familial support (29%), and religion (16%). Additional factors included the patient–physician relationship (14%), the patient–nurse relationship (11%), the location of treatment (11%), and finally, the curability of cancer (10%). All the aforementioned factors were considered equally important by 29% of the nurses. Among physicians, cancer curability, the patient–physician relationship, and familial support were the most important factors in accepting the truth (29% each).
Overall, 71% of patients and their families, 57% of nurses, and 86% of physicians reported that the personality of the physician has a positive effect on acceptance of a cancer diagnosis. All participants said that the psychological influence of the physician played the greatest role in acceptance (42%), followed by the spiritual influence of the physician (17%), the education and knowledge of the physician (17%), and a sense of conviviality (12%).
The survey showed that 77% of all participants agreed that communication would be easier when the cancer patient is aware of the diagnosis. Finally, 62% of all participants estimated that fewer than 50% of patients are aware of their diagnosis, with significant group differences between the answers: 72% for nurses, 66% for family and friends, and 39% for physicians (p = 0.001, Table iii).
Specific Questions for Patients Aware of Their Diagnosis
The survey showed that 62% of patients were informed of their diagnosis by their physician, 16% knew by intuition, 11% were told by family or friends, and 11% found out by chance. With respect to the timing of diagnosis disclosure, 63% of patients knew that they had cancer before starting treatment, 36% found out during treatment, 1% were informed about their cancer diagnosis after treatment start, and 47% spontaneously discovered the truth because of fatigue, alopecia (33%), and dry mouth (20%). Importantly, most patients (93%) did not regret knowing the truth. In fact, it helped 80% of them to better organize their lives. For 10%, knowing the truth was essential in seeking to obtain several medical opinions. Feelings of despair, fear, and anxiety were the main reasons given by patients for regretting being aware of their disease.
Specific Questions for Nurses
None of the nurses disclosed the cancer diagnosis to patients who were unaware but who asked about their disease. Interestingly, 23% of the nurses did not know whether they would inquire about their diagnosis in similar circumstances. Overall, nurse participants said they would delegate disclosure to the physician (56%), to a more experienced nurse (25%), or to the patient’s family (19%).
Specific Questions for Physicians
When asked about the timing of disclosure, 72% of physicians reported revealing the diagnosis immediately after confirmation. Another 15% informed the patient only when specifically asked, and the remaining 13% informed the patient during the course of treatment. Overall, 60% of physicians reported disclosing a cancer diagnosis first to the parents of the patient; 40% first disclosed it to patients themselves.
The main factors influencing disclosure of the diagnosis were the patient’s educational background (60%) and age (33%). Other factors—such as the family’s wish, religion, and stage of the disease—were also considered (2% each). Notably, physicians can face several obstacles when disclosing a cancer diagnosis. Specifically, they worry equally about the psychosomatic consequences of the news (50%) and family opposition to informing the patient (50%).
Furthermore, 9% of physicians reported directly informing their patients about their disease; the remaining 91% reported progressive disclosure. Physicians also reported that they communicated with all patients in the same way, regardless of the curability of the cancer.
Socio-demographic Variables and Cancer Truth Disclosure
With respect to the socio-demographic variables of the participants, only employment (p = 0.001) and education (p = 0.002) were significantly related to truth disclosure. Employed patients were more in favour of the truth about cancer being disclosed (90% versus 74% among those not employed. The preference for disclosure also increased with the education level of the patient. A preference in favour of revealing the diagnosis rose from 70% among illiterate participants, to 73% of those with a primary or intermediate education, 84% of those with a secondary education, and 91% of those with a university degree.
DISCUSSION
Disclosing the truth about a cancer diagnosis to a patient can never follow a standard procedure; it depends on many cultural elements. Factors such as socioeconomic status, education, spoken language, geographic area, urban or rural context, religion, sex, occupation, and disability define each culture19. As reflected in our survey, Lebanese and Middle Eastern cultures have specific beliefs and values, with religion, family, and the relationship to the physician playing major roles. Cultural competence is therefore essential for communicating a diagnosis in our setting, and awareness of this Middle Eastern specificity among the oncology professionals is presupposed19.
Culture is not static, and like the beliefs and values surrounding many practices, the beliefs and values about disclosure of a cancer diagnosis are changing. The authors of a cross-sectional survey that used a modified version of a questionnaire by Novack et al.20 to sample 212 physicians practicing in Beirut in 1996 reported that only 47% usually disclose the truth about a cancer diagnosis to patients. Patient-related factors (age, education, patient’s desire to know the diagnosis, compliance jeopardized) were essential in determining their decision to disclose the truth (p < 0.05)21. However, in another study that aimed to evaluate changes in the attitude to cancer disclosure after introduction of a course on medical ethics in a medical school’s education program, a large majority of the 70 students surveyed at two time points (84% in 1995, 86% in 1998) preferred to disclose the cancer diagnosis directly to the patient22. Similarly, our study shows that 83% of oncology professionals and other specialists in Lebanon favour disclosing information about a diagnosis or prognosis to their patients. However, only 40% of the physicians reveal the truth to the patients themselves, and just 9% disclose the information immediately.
Despite opinion in favour of disclosure being common, partial disclosure or nondisclosure is still a common practice in Lebanon and Middle Eastern countries, where the culture is centred on family and community values19. This cultural context makes the physician’s position on truth disclosure more sensitive. Our study revealed that 80% of the relatives and friends of cancer patients in Lebanon are not in favour of revealing detailed information about the disease. Physicians and oncology professionals are aware of this factor and try to adapt their communication out of respect for each patient’s context. In fact, before disclosing any cancer diagnosis, 60% of physician first address the parents of the patient for a “green light,” informing the family about a cancer diagnosis before informing patients themselves.
Honesty matters to patients, who need it because they are ill, vulnerable, and burdened with pressing questions that require truthful answers. Not telling the truth in the physician–patient relationship requires special attention, because today, more than ever, patients might experience serious harm if not told the truth. But harm can also result from telling the truth about death or a dreaded diagnosis. Harm might be rare, but it must still be guarded against. Consequently, truth-telling must be sensitive to the clinical context and must consider the patient’s personality, clinical history, and cultural and societal background. Indeed, our study found that all participants reported fear to be a major concern of cancer patients, followed by pain, pity, and death. Our findings highlight the negative emotional impact of a cancer diagnosis on patients in our society. Physicians might therefore be fearful of the patient’s reaction to the news and might find communication about a cancer diagnosis difficult. Nonetheless, the physician who tells a dreadful truth must do so at a particular time, and in a particular way, because cancer truth disclosure must be matched with many cultural and emotional nuances, such as pain and pity.
Physicians must not lie to their patients, but they currently tend to address the family before disclosing a cancer diagnosis to the patient. That approach is important, because in our society, familial support plays a major role in helping patients cope with a cancer diagnosis23. The authors of a previous qualitative study in Lebanon highlighted the need to shift from a paternalistic approach to patient-centered care24, which can help to promote the patient’s autonomy. Controversially, family opposition to informing the patient is one of the obstacles that prevents 50% of physicians from telling the truth to patients. Thus, the first level of attitude change concerns the physicians themselves.
In certain cultures (such as the Middle Eastern culture), cancer is a “bad word”19. Thus, when addressing patients, the right words must be carefully chosen. Indeed, in addition to family influence, the second obstacle that prevents physicians from disclosing the truth to their patients is their concern about the psychosomatic consequences flowing from the metaphorical implications of the word “cancer” in the patient’s mind. Of the physicians surveyed in our study, 68% did not disclose the truth to their patients “knowing that it will have a negative effect.” In contrast, two studies in Greece revealed that 89% of Greek oncologists acknowledged information to be beneficial to the professional’s good therapeutic relationship and peacefulness, the patients’ good therapeutic relationship, and better palliation and support25,26. Those studies also showed that a reduction in anxiety, increased satisfaction, and improved compliance by patients are recognized benefits of information provision25,26.
Accepting a cancer diagnosis is hard for any patient in any culture, but physicians should acknowledge that about 88% of their patients are in favour of knowing the reality of their diagnosis. The authors of a qualitative interview study performed in 2005 in Lebanon found that communication was an important part of the disease trajectory and that patients considered it their right to be told the truth about their condition24,27.
It is therefore time to start considering the autonomy of cancer patients in Middle Eastern communities; they need to be the first line of communication for physicians when it comes to truth disclosure. The truth is essential for patients to be able to better organize their lives (44%) and to avoid living an illusion (26%). Timing is also an important factor to consider in this context, because revealing a cancer diagnosis is preferred before the start of treatment by 59% of patients and immediately after confirmation of the diagnosis by 72% of physicians.
CONCLUSIONS
Western bioethics tends to rely on a narrow understanding of individual autonomy that is based on an ideal concept of rational people who are capable of making the best choices for their own life and health and who are free to enact their choices. That view ignores the fact that people are immersed in a web of relationships and connections with other people19. In Middle Eastern medical communities, health care providers must also incorporate the role and influence of family and friends whenever a cancer diagnosis has to be revealed to a patient. Given the findings in our survey, we recommend that cancer patients should be informed about their true diagnosis and exam results before starting treatment. Communication methods should be the same regardless of cancer type, curability, or the country of residence of the patient. In fact, physicians should always consider the cultural background of the patient regardless of place of residency, even when the patient lives in a Western society. Although Lebanese society is becoming more aware of cancer because of awareness campaigns, both Western and Middle Eastern physicians should consider the emotional impact of a diagnosis on the patient. Moreover, we recommend that physicians and medical staff involved in the care of cancer patients be flexible when breaking bad news, because a “one size fits all” approach is not appropriate. Finally, we strongly encourage formal training in breaking bad news, because such training is designed to enhance the performance of physicians and other health care providers. We also encourage training for nursing personnel in oncology settings because those professionals often play a key role in helping cancer patients and their families to cope with a cancer diagnosis.
ACKNOWLEDGMENTS
We are grateful to all the participants in our survey study.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Ferraton-Rollin M, Magné N, Gonthier R, Merrouche Y, Bois C. The announcement of the diagnosis of cancer: point of view of the general practitioner [French] Bull Cancer. 2013;100:955–62. doi: 10.1684/bdc.2013.1825. [DOI] [PubMed] [Google Scholar]
- 2.Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet. 2004;363:312–19. doi: 10.1016/S0140-6736(03)15392-5. [DOI] [PubMed] [Google Scholar]
- 3.Schofield PE, Butow PN, Thompson JF, Tattersall MH, Beeney LJ, Dunn SM. Psychological responses of patients receiving a diagnosis of cancer. Ann Oncol. 2003;14:48–56. doi: 10.1093/annonc/mdg010. [DOI] [PubMed] [Google Scholar]
- 4.Fallowfield L, Jenkins V. Current concepts of communication skills training in oncology. In: Schlag PM, Senn HJ, Stiefel F, editors. Communication in Cancer Care. New York, NY: Springer; 2006. pp. 105–12. [DOI] [PubMed] [Google Scholar]
- 5.Ramirez AJ, Graham J, Richards MA, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263–9. doi: 10.1038/bjc.1995.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vandekieft JK. Breaking bad news. Am Fam Physician. 2001;64:1975–8. [PubMed] [Google Scholar]
- 7.Friedrichsen M, Lindholm A, Milberg A. Experiences of truth disclosure in terminally ill cancer patients in palliative home care. Palliat Support Care. 2011;9:173–80. doi: 10.1017/S1478951511000046. [DOI] [PubMed] [Google Scholar]
- 8.Miyata H, Takahashi M, Saito T, Tachimori H, Kai I. Disclosure preferences regarding cancer diagnosis and prognosis: to tell or not to tell? J Med Ethics. 2005;31:447–51. doi: 10.1136/jme.2003.007302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salem A, Salem AF. Breaking bad news: current prospective and practical guideline for Muslim countries. J Cancer Educ. 2013;28:790–4. doi: 10.1007/s13187-013-0523-8. [DOI] [PubMed] [Google Scholar]
- 10.Baile W, Lenzi R, Parker P, Buckman R, Cohen L. Oncologists’ attitudes toward and practices in giving bad news: an exploratory study. J Clin Oncol. 2002;20:2189–96. doi: 10.1200/JCO.2002.08.004. [DOI] [PubMed] [Google Scholar]
- 11.Sparling TG. Caring for Fatima. J Clin Oncol. 2006;24:2589–91. doi: 10.1200/JCO.2006.04.7910. [DOI] [PubMed] [Google Scholar]
- 12.Cox A, Jenkins V, Catt S, Langridge C, Fallowfield L. Information needs and experiences: an audit of UK cancer patients. Eur J Oncol Nurs. 2006;10:263–72. doi: 10.1016/j.ejon.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Jiang Y, Liu C, Li JY, et al. Different attitudes of Chinese patients and their families toward truth telling of different stages of cancer. Psychooncology. 2007;16:928–36. doi: 10.1002/pon.1156. [DOI] [PubMed] [Google Scholar]
- 14.Marwit SJ, Datson SI. Disclosure preferences about terminal illness: an examination of decision-related factors. Death Stud. 2002;26:1–20. doi: 10.1080/07481180210144. [DOI] [PubMed] [Google Scholar]
- 15.Cavanna L, Di Nunzio C, Seghini P, et al. Elderly cancer patients’ preferences regarding the disclosure of cancer diagnosis. Experience of a single institution in Italy. Tumori. 2009;95:63–7. doi: 10.1177/030089160909500111. [DOI] [PubMed] [Google Scholar]
- 16.Guerra-Tapia A, González-Guerra E. Communicating bad news during an office visit [Spanish] Actas Dermosifiliogr. 2013;104:1–3. doi: 10.1016/j.ad.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. spikes—a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5:302–11. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 18.Elwyn TS, Fetters MD, Sasaki H, Tsuda T. Responsibility and cancer disclosure in Japan. Soc Sci Med. 2002;54:281–93. doi: 10.1016/S0277-9536(01)00028-4. [DOI] [PubMed] [Google Scholar]
- 19.Surbone A. Cultural aspects of communication in cancer. Support Care Cancer. 2008;16:235–40. doi: 10.1007/s00520-007-0366-0. [DOI] [PubMed] [Google Scholar]
- 20.Novack DH, Plumer R, Smith RL, Ochitill H, Morrow GR, Bennett JM. Changes in physicians attitudes toward telling the cancer patient. JAMA. 1979;241:897–900. doi: 10.1001/jama.1979.03290350017012. [DOI] [PubMed] [Google Scholar]
- 21.Hamadeh GN, Adib SM. Cancer truth disclosure by Lebanese doctors. Soc Sci Med. 1998;47:1289–94. doi: 10.1016/S0277-9536(98)00203-2. [DOI] [PubMed] [Google Scholar]
- 22.Hamadeh GN, Adib SM. Changes in attitudes regarding cancer disclosure among medical students at the American University of Beirut. J Med Ethics. 2001;27:354. doi: 10.1136/jme.27.5.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doumit MA, Huijer HA, Kelley JH, El Saghir N, Nassar N. Coping with breast cancer: a phenomenological study. Cancer Nurs. 2010;33:E33–9. doi: 10.1097/NCC.0b013e3181c5d70f. [DOI] [PubMed] [Google Scholar]
- 24.Doumit MA, Abu-Saad Huijer H, Kelley JH. The lived experience of Lebanese oncology patients receiving palliative care. Eur J Oncol Nurs. 2007;11:309–19. doi: 10.1016/j.ejon.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 25.Georgaki S, Kalaidopoulou O, Liarmakopoulos I, Mystakidou K. Nurses’ attitudes toward truthful communication with patients with cancer. A Greek study. Cancer Nurs. 2002;25:436–41. doi: 10.1097/00002820-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Tsoussis S, Papadogiorgaki M, Markodimitraki E, et al. Disclosure of cancer diagnosis: the Greek experience. J BUON. 2013;18:516–26. [PubMed] [Google Scholar]
- 27.Doumit MA, Abu-Saad HH. Lebanese cancer patients: communication and truth telling preferences. Contemp Nurse. 2008;28:74–82. doi: 10.5172/conu.673.28.1-2.74. [DOI] [PubMed] [Google Scholar]


