Abstract
Chlamydia spp. utilize multiple secretion systems, including the type III secretion system (T3SS), to deploy host-interactive effector proteins into infected host cells. Elucidation of secreted proteins has traditionally required ectopic expression in a surrogate T3SS followed by immunolocalization of endogenous candidate effectors to confirm secretion by chlamydiae. The ability to transform Chlamydia and achieve stable expression of recombinant gene products has enabled a more direct assessment of secretion. We adapted TEM-1 β-lactamase as a reporter system for assessment of chlamydial protein secretion. We provide evidence that this system facilitates visualization of secretion in the context of infection. Specifically, our findings provide definitive evidence that C. trachomatis CT695 is secreted during infection. Follow-up indirect immunofluorescence studies confirmed CT695 secretion and indicate that this effector can be secreted at multiple points during the chlamydial developmental cycle. Our results indicate that the BlaM-fusion reporter assay will allow efficacious identification of novel secreted proteins. Moreover, this approach can easily be adapted to enable more sophisticated studies of the secretion process in Chlamydia.
Introduction
Chlamydia trachomatis (serovars D-K and lymphogranuloma venereum serovars L1-L3) are agents of human sexually transmitted disease, whereas ocular infections with C. trachomatis serovars A-C can lead to blindness [1]. C. trachomatis is a member of a larger Chlamydiaceae family that contains numerous species that have likely co-evolved with a eukaryotic host for >700 million years [2]. All Chlamydia spp. are Gram-negative obligate intracellular bacteria that possess a conserved, biphasic developmental cycle [3]. Development is initiated when infectious particles termed elementary bodies (EBs) invade host cells and differentiate into noninfectious, vegetative forms termed reticulate bodies (RBs). RB growth is eventually accompanied by asynchronous conversion of RBs to EBs. Subsequent exit from the host cell is mediated by lysis or extrusion [4]. Intracellular development occurs entirely within a parasitophorous vacuole termed an inclusion. Chlamydiae develop effectively segregated from the host cytosol since the inclusion membrane is passively impermeable to molecules >520 Da [5]. Despite this physical separation, Chlamydia spp. are capable of directly modulating host cell biology. Members of the Chlamydiaceae all express a type III secretion system (T3SS) to promote survival from within a protected niche.
Similar to systems in other T3S-expressing pathogens, the chlamydial T3SS is a multi-protein nanomachine capable of secreting and subsequently translocating (hereafter collectively referred to as secretion) anti-host proteins termed effectors, (T3SE) directly into an associated eukaryotic cell [6]. The chlamydial T3SS is present, and apparently active throughout development. EBs contain abundant levels of effectors required for invasion [7], and secretion can be detected within minutes of attachment to a host cell [8,9]. Described effectors first secreted during invasion include the translocated actin-recruiting phosphoprotein TarP [9], the translocated early phosphoprotein TepP [10], and the human Ahnak interacting protein designated CT694 [11]. Subsequent to entry, chlamydiae begin to secrete a number of identified effectors, the most abundant of which are the inclusion membrane (Inc) class of effectors. Many Inc effectors interact with elements of host vesicular transport pathways [12] while others likely play key roles in maintaining inclusion membrane architecture through interactions with other Incs [13,14]. The continued accumulation of Incs in the expanding inclusion membrane indicates that T3S is likely active in RBs until completion of the developmental cycle.
Interaction with T3S chaperones [10,15,16] and in silico analyses have been used successfully to identify chlamydial T3S substrates [17]. However, the use of surrogate T3SSs has been perhaps most efficacious in discovering putative chlamydial effectors. Several recent studies have leveraged Yersinia [18] or Shigella [19] T3SS in large-scale screens for T3S substrates. These studies and others have yielded a long list of potential effectors that require further validation. Confirmation of secretion by Chlamydia typically employs the use of indirect immunofluorescence assays to detect localization of the effector within or beyond the inclusion membrane [20]. This approach requires the generation of effector-specific antibodies. In addition, the assay can be confounded by low abundance of a given effector. Therefore, there is a need for an efficacious system to easily detect secretion of chlamydial proteins during infection.
Reproducible transformation of Chlamydia with a stably-maintained shuttle vector [21] has overcome a significant barrier that impeded efficient progress in investigating chlamydial infection biology. This approach has enabled development of second generation vectors expressing fluorescent proteins [22] or enabling conditional gene expression [23,24]. This approach has already been used to express epitope-tagged effectors [24,25] for efficacious detection of Inc secretion. Inc proteins have the advantage of being easily detectible due to concentration in the inclusion membrane. We regard it likely that detection of low-abundance, effectors that do not concentrate in a particular compartment will require signal amplification for detection. Numerous enzymatic tags have been employed in other T3SSs to demonstrate cytosolic localization of secreted effectors [26]. The use of β-lactamase (BlaM) translational fusions, originally developed to detect pathogenic Escherichia coli effector secretion [27], has proven to be a convenient and sensitive tool for detection of bacterial protein secretion. Infected cells are treated with the cell-permeant reagent CCF2-AM which is subsequently converted to a membrane-impermeant molecule by esterases in the host cytosol. CCF2-AM is composed of the flourophores coumarin and fluorescein. Excitation of intact CCF2-AM at 409 nm results in green fluorescent via fluorescence energy transfer (FRET). Secretion of a given bacterial protein-BlaM fusion into the host cytosol is readily indicated when CCF2-AM is cleaved by the BlaM moiety to disrupt FRET and yield blue fluorescence. This approach is particularly desirable for an obligate intracellular pathogen such as Chlamydia since evidence of secretion can be detected directly in the absence of host cell lysis. We therefore designed a two-step vector system that would enable ectopic expression of T3SE-β-lactamase chimeras. We provide proof-of-principle evidence herein that this system allows the robust detection of T3SE secretion in a tissue-culture infection model. We focused efforts on characterization of CT695. This putative T3SE is secreted by the Yersinia T3SS [11] and binds the chlamydial T3S chaperone Slc1[10,16], yet secretion by chlamydiae has not been confirmed. We reveal for the first time that C. trachomatis CT695 is secreted by chlamydiae at multiple stages of the developmental cycle.
Methods
Cell cultures and organisms
C. trachomatis serovar L2 (LGV 434) was cultivated in HeLa 229 epithelial cell monolayers (ATCC CCL-1.2; American Type Culture Collection, Manassas, VA), routinely maintained at 37°C in an atmosphere of 5% CO2/95% humidified air in RPMI-1640 containing 2 mM L-glutamine (GibcoLife Technologies Corporation, Grand Island, NY) supplemented with 10% (vol/vol) heat-inactivated fetal bovine serum (HIFBS; Sigma-Aldrich Company, St. Louis, MO). Where appropriate, intrinsically fluorescent chlamydiae were generated by labeling bacteria with CellTracker Red CMPTX (Life technologies) as described [28]. All EBs were purified from HeLa cells by centrifugation through MD-76R (diatrizoate meglumine and diatrizoate sodium injection U.S.P.; Mallingckrodt Pharmaceuticals, Mulhuddart, Ireland) density gradients (DG-purified) as previously described [29] and were used as the infection source for all experiments. Assessment of chlamydial growth was accomplished by enumeration of progeny EBs from 24 hr cultures as described [30]. Chemically competent E. coli 10-beta (NEB, Ipswich, MA) was used for routine cloning, and dam -/dcm - E. coli (NEB) was used to propagate plasmids prior to transformation of chlamydiae. Where appropriate, 50 μg/ml carbenicillin was used for E. coli selection while 1.0 μg/ml cycloheximide and 0.6 μg/ml Penicillin G sodium (PenG) was used during chlamydial transformations.
Vector construction
pGFP::SW2 was generously provided by Ian Clarke (University of Southampton). This template was modified using custom PCR primers (S1 Table; IDT, Coralville, IA). Sequence encoding mCherry was amplified from pmCherry-C1 vector using forward and reverse primers mC@GFP F and mC@GFP R, respectively. This was used to replace the GFP gene in pGFP::SW2 by insertion/deletion PCR as described [31] to produce pMC::SW2. Sequence encoding chloramphenicol drug resistance was amplified from pACD4K-C-loxP using forward and reverse primers SalI+AscI+Chlor F and SalI+AscI+Chlor R, respectively. In order to construct pL2dest, SalI restriction enzyme and Quick Ligation Kit (NEB) were used to digest and ligate the chloramphenicol drug resistance amplicon into pMC::SW2, simultaneously introducing AscI restriction sites around the chloramphenicol open reading frame. pUC19 was used as the backbone for construction of the β-lactamase translational fusions. The Neisseria meningitidis promoter was amplified from pGFP::SW2 and inserted into pUC19 by insertion/deletion PCR using forward and reverse primers NmP@puC F and NmP@pUC R, respectively, producing pUCNmP. ct694-, ct695-, ct696-, euo-, groEL-, and tarp-bla fusions were constructed by amplifying each open reading frame from C. trachomatis serovar L2 genomic DNA preparation, and by inserting each amplicon between the Neisseria meningitidis promoter and the full-length β-lactamase gene of pUCNmP by insertion/deletion PCR (primers listed in S1 Table). Each fusion was amplified from pUCNmP with primers NmP+BlaFus+AscI F and R, and inserted into pL2dest by AscI digestion followed by Quick Ligation (NEB). Loss of chloramphenicol resistance was used as a convenient marker for successful cloning of BlaM fusions in E. coli. Final constructs were transformed into dam-/dcm- E. coli, and plasmids were purified using a QIAfilter Plasmid Maxi Kit (Qiagen, Valencia, CA) prior to transformation into C. trachomatis L2. Q5 High-Fidelity DNA Polymerase (NEB) was used for all PCR amplifications and direct DNA sequencing (ACGT, Inc) was used to confirm all constructs.
Chlamydial transformation
C. trachomatis L2 were transformed as described [21] with modifications. 2.6 x 106 EBs and 2 μg of plasmid DNA were mixed in 50 μl CaCl2 buffer (10 mM Tris pH 7.4 and 50 mM CaCl2) and incubated at room temperature for 30 minutes. Each mixture was suspended in 2 ml Hanks Balanced Salt Solution (HBSS; Life Technologies) and applied to a 10-cm2 well containing a monolayer of confluent McCoy cells. Monolayers were infected by centrifugation at 900 x g for 1 hr at room temperature, after which HBSS was replaced with 2 ml RPMI + 10% FBS medium without drugs. At 7 hours post infection (hpi), cultures were supplemented with cycloheximide and PenG. Cells were harvested 48 hpi with a cell scraper and centrifuged at 20,000 x g for 30 min at 4°C. The pellet was suspended in 1 ml HBSS, centrifuged at 200 x g for 5 min at 4°C, and the supernatant was used to infect a new confluent monolayer of McCoy cells in a 10 cm2 well by centrifugation (900 x g, 1 hr, room temperature). Immediately after infection, medium containing both cycloheximide and PenG was added. Cells were harvested 48 hpi with a cell scraper, and the process of centrifugation and infection was repeated until transformed Chlamydia were recovered (typically 1 to 3 rounds of reinfection). In order to ensure clonal isolates, transformed C. trachomatis strains were diluted in HBSS and applied to confluent McCoy monolayers grown in 384-well plates (Greiner Cell Culture Microplate, catalog number 781091) at a concentration of one IFU for every 100 wells (approximately four inclusions per 384-well plate). Monolayers were infected by centrifugation with C. trachomatis at 900xg for 60 minutes at room temperature. Infection was allowed to continue in the absence of drug selection for seven days. Wells containing C. trachomatis (roughly one well for every 100) were then scraped with a p200 tip, and each isogenic population was then applied to new monolayers in T75 flasks for further expansion with antibiotic selection.
Expression assays
For assessment of gene expression, RNA was harvested at indicated times using the Aurum Total RNA Mini Kit (Bio-Rad, Hercules, Ca.) according to the manufacturer’s instructions. RNA was converted to cDNA using the QuantiTect Reverse Transcription Kit (Qiagen). Transcript levels were determined by quantitative real-time PCR using the Bio-Rad CFX96 Real-Time Systen (Bio-Rad), iTaq Universal SYBR Green Supermix (Bio-Rad), and appropriate primers (S2 Table). All quantitative real-time PCR primers were confirmed to amplify with efficiencies >95%. For assessment of ectopically expressed protein levels, samples were obtained from HeLa cells infected with C. trachomatis at an MOI of 1. Cells were gently harvested with ice cold PBS and immediately concentrated by the addition of trichloroacetic acid to 10% (v/v) and centrifugation at 20,000 x g for 30 min at 4°C. Protein pellets were analyzed by SDS-PAGE electrophoresis followed by immunoblot analysis using β-lactamase-specific antibodies (Pierce, Rockford, IL) or α-Hsp60 (Santa Cruz, Dallas, TX) as a loading control. Proteins were visualized by peroxidase-conjugated secondary antibodies followed by development with ECL Prime (GE Healthcare, Pittsburgh, PA).
BlaM Secretion Assay
The presence of fusion proteins in the cytosol of infected HeLa cells was observed directly with the use of the GeneBLAzer In Vivo Detection Kit (Invitrogen). HeLa monolayers were cultivated on glass cover slips to a confluence of ca. 75% and infected with C. trachomatis L2 expressing various β-lactamase-fusion proteins. CCF2-AM substrate was applied 24 hpi for 30 minutes, samples were fixed in 4% paraformaldehyde, and fluorescence was observed using a Leica TCS SP5 laser scanning confocal microscope. Images were processed equivalently using Adobe Photoshop CS2 version 9.0 (Adobe Systems, San Jose, CA).
BSA-EGTA release assay
Cell-free release of secreted proteins from EBs was accomplished essentially as described [32]. Briefly, volumes of 5 x 107 EBs were suspended in 50 mM acetate buffer and one replicate was supplemented with bovine serum albumin (BSA; Sigma) and EGTA pH 7.4 to 5 μM final concentration for each. EBs were incubated for 2 hrs at 37°C and bacteria were pelleted by centrifugation at 20,000 x g for 15 min. Proteins from bacterial pellets and cell-free supernatants were precipitated using trichloroacetic acid and subsequent pellets were suspended in equal volumes of SDS-PAGE solublization solution. Supernatant material was loaded at 5X bacterial pellets, proteins were resolved via SDS-PAGE, and probed in immunoblots with α-TarP [9], α-Hsp60 (Santa Cruz), and α-CT695 (described below). Proteins were visualized by peroxidase-conjugated secondary antibodies and chemiluminescence development.
Fluorescence microscopy localization assays
Localization of CT695 and TarP was determined via indirect immunofluorescence using CT695-specific antibodies or α-TarP [9]. Full-length, His-tagged CT695 was used as antigen for production of antibodies. The coding sequence for C. trachomatis L2 CT695 was amplified using Q5 DNA polymerase and primers sets (5’-GGGGACAAGTTTGTACAAAAAA GCAGGCTTCAG TAGCATAAGCCCTATAGGGGGG-3’ and 5’-GGGGACCACTT TGTACAAGAAAGCTGG GTCCTATTAGATATTCCCAACCGAAGAAGG-3’) for transfer into the GATEWAY (Life Technologies) entry vector pDONR-221. Donor sequence was mobilized into pDEST-17 and constructs were verified via DNA sequencing (GENEWIZ). His-Tagged CT695 was expressed in E. coli BL21-Al (Invitrogen), and protein was purified to homogeneity via passage of lysates over TALON affinity resin (Clontech, Mountain View, CA). Polyclonal antibodies were raised in female New Zealand White rabbits as previously described [33]. To assess invasion-related secretion of endogenous CT695, HeLa cultures were infected for 1 hr with CMPTX-labeled C. trachomatis L2 at an MOI of ca. 10. Cultures were thoroughly washed and fixed for 20 min by treatment with 4% paraformaldehyde. Samples were permeablized by treatment with 0.1% Triton X100 in Tris-buffered saline supplemented with 5% BSA. Chlamydia were visualized via either intrinsic CMPTX label or with MOMP-specific antibodies [11,34]. All images were acquired by epifluorescence microscopy using a 60x apochromat objective plus 1.5x intermediate magnification on a TE2000U inverted photomicroscope (Nikon, Melville, NY) equipped with a Retiga EXi 1394, 12-bit monochrome CCD camera (QImaging, Surrey, BC, Canada) and MetaMorph imaging software version 6.3r2 (Molecular Devices, Downington, PA). Images were processed equivalently using Adobe Photoshop CS2 version 9.0 (Adobe Systems).
Statistical Analysis
All presented data are representative of a minimum of three independent experiments. Quantitative data were generated from experiments containing triplicate biological replicates. All data are shown as mean of these replicates with 1 standard deviation. Calculation of standard deviation of the mean and assessment via Student’s t-test statistical analyses were performed using GraphPad Prism 6 version 6.04 (Graphpad Software Inc., La Jolla, CA).
Results
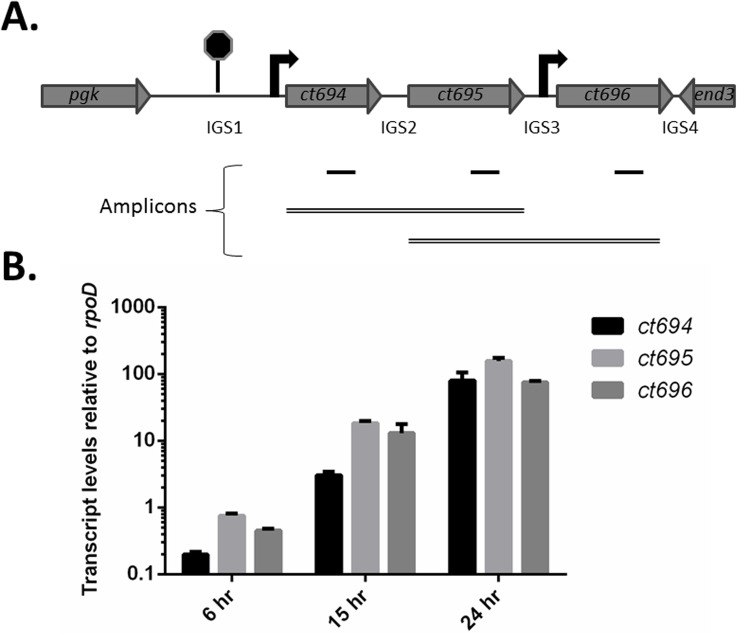
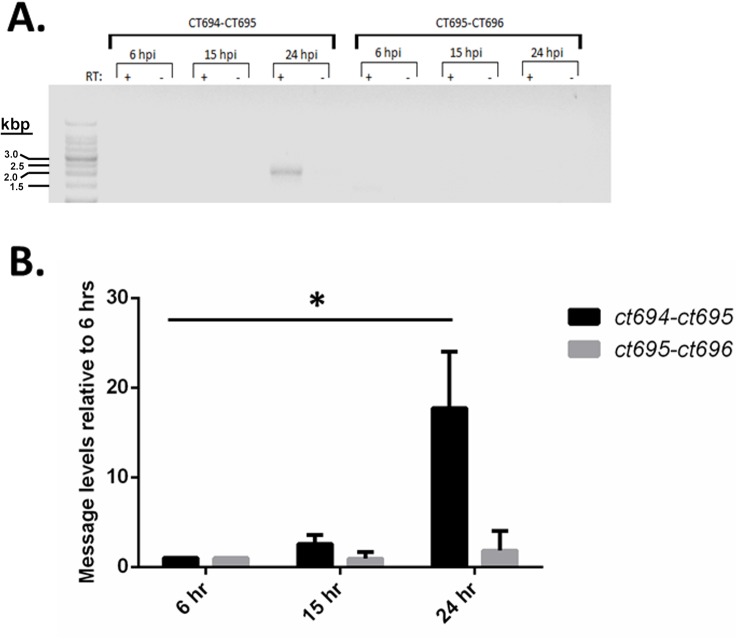
We began by assessing whether CT695 is encoded within a dedicated T3S-related locus. C. trachomatis CT695 is encoded [35] immediately downstream from the validated T3SE CT694 and upstream from the hypothetical CT696 (Fig 1A). Flanking gene orientation and a predicted rho-independent transcription terminator upstream from ct694 [36] indicate that ct694, ct695, and ct696 could comprise an operon. Transcriptional profiling of C. trachomatis serovar D via microarray indicated that ct694 is expressed much later than ct695 or ct696 [37]. However, deep-sequencing-based transcriptome analysis of C. trachomatis L2 revealed a common transcriptional start site for ct694 and ct695 [38], raising the possibility of polycistronic message. We assayed temporal gene transcription by RT-PCR from total culture RNA harvested from C. trachomatis L2 infected HeLa cells 6, 15, or 24 hpi. Samples were normalized to rpoD and transcript levels were assayed for ct694, ct695, and ct696 (Fig 1B). Basal levels of message were detected for all three genes as early as 6 hpi. As expected, these levels were increased (ca. 10-fold) at each of the later time-points. We next addressed transcriptional linkage using the previously reported approach [39] using RT-PCR and gene-spanning primer sets. A correctly sized amplicon (2.2 kb) was detectible only in the presence of RT and ct694-ct695 spanning primers at 24 hpi (Fig 2A). No product was detected using ct695-ct696 spanning primers even though these primers were capable of yielding the 2.4 kb product using DNA template (data not shown). A faint band was detected in the 6 hpi sample, but the apparent size was below 1.5 kb. Since qRT-PCR indicate the presence of message at earlier time-points, we used gene-spanning primers and qRT-PCR as a more sensitive means to detect polycistronic message (Fig 2B). In agreement with the RT-PCR data, an amplicon containing ct694 and ct695 was apparent at 24 hpi. Although a small (2.75-fold) increase over background was detected for ct694/ct695 at 15 hpi, this was not statistically significant. No product was detected for ct695-ct696. Taken together, these data are consistent with mid-cycle expression of ct694, ct695, and ct696. However, ct694 and ct695 are likely transcribed separately from ct696, and ct694/ct695 expression at 15 hpi is likely due to individual promoters and not co-transcription.
Fig 1. Gene arrangement and relative expression of ct694, ct695, and ct696.
(A). Schematic arrangement of the ct694-ct696. The locus is flanked by phosphoglycerate kinase (pgk) and endonuclease III (end3) genes and contains 4 intergenic regions (IGS1-4) of 261, 48, 54, and 3 nucleotides, respectively. TransTermHP [36] predicts a Rho-independent transcriptional terminator between pgk and ct694. Arrows indicate relative positions of previously reported transcriptional start sites [38]. Amplicons used for expression analyses are represented schematically. 100 bp amplicons (solid lines) were generated for qRT-PCR wherease gene-spanning amplicons (double lines) were employed to test the possibility of polycistronic message. (B). Transcription of ct694, ct695, and ct696 increases throughout chlamydial development. HeLa cells were infected with C. trachomatis L2 at an MOI of 0.5, and transcript levels were determined by quantitative real-time PCR at various time points throughout the chlamydial developmental life cycle. Expression levels were normalized against, and relative to, those for the constitutively expressed rpoD.
Fig 2. Co-transcription of ct694 and ct695.
(A). The presence of transcripts containing multiple open reading frames was determined by reverse-transcription (RT) PCR with primers surrounding ct694 and ct695 or ct695 and ct696. RNA was isolated from HeLa cells infected with C. trachomatis L2 at an MOI of 0.5 grown to various time points post infection. (B). The same samples were additionally analyzed by quantitative real-time PCR for increased sensitivity. Levels shown are relative to those detected 6 hpi. A Student’s T test with Welch’s correction was employed to assess statistical significance (*, P < 0.04).
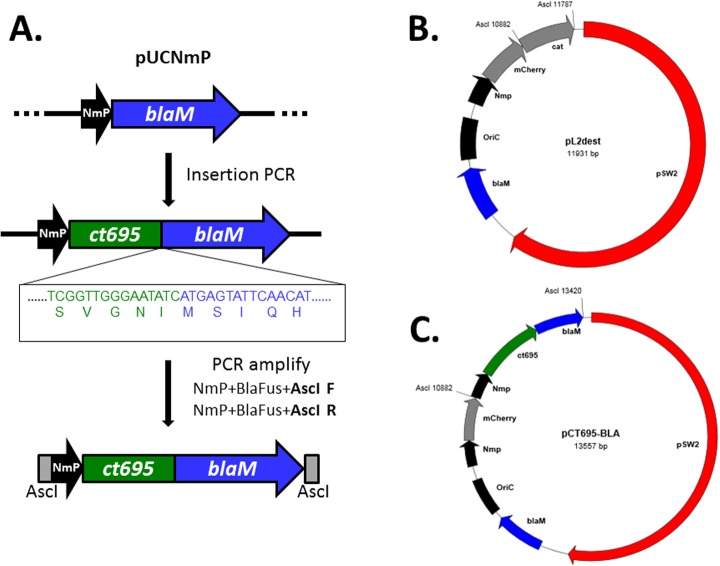
Transcriptional linkage of ct694 and ct695, coupled with previously reported secretion by the heterologous T3SS [11] and association with the chaperone Slc1 [10,16], predicts that CT695 is secreted by chlamydiae. We wanted to take advantage of the newly acquired ability to transform Chlamydia in order to construct a reporter system that would facilitate assessment of protein secretion during infection (Fig 3). The entry vector pUCNmP contains the N. meningitidis promoter (NmP) described by Wang, et al. [21] positioned upstream from the complete TEM-1 β-lactamase coding sequence. This enables insertion of any chlamydial gene using insertion PCR [31] to create an in-frame fusion with BlaM. PCR primers flanked with the AscI recognition-site sequence are then used to amplify the construct, followed by digestion and ligation with pL2dest, a derivative of pGFP::SW2 [21] with GFP in place of mCherry and an engineered AscI restriction site.
Fig 3. A schematic of constructed plasmids using CT695 as an example.
(A). pUCNmP. The Neisseria meningitidis promoter (NmP) was inserted into pUC19 upstream from BlaM. Insertion/Deletion PCR is used to insert any chlamydial sequence (ct695 is shown) to create a translational fusion of the chlamydial gene (green) with the β-lactamase gene (blue). DNA elements can then be PCR amplified using primers NmP+BlaFus+AscI F and NmP+BlaFus+AscI R to generate a product flanked by AscI restriction sites. (B). pL2dest was created by replacement of the coding sequence for GFP/CAT of pGFP::SW2 with the mCherry gene. A chloramphenicol drug cassette flanked by AscI recognition sequences was introduced immediately downstream from mCherry coding sequence. (C). pCT659-BLA was created by ligation of AscI-digested PCR product into the AscI site in pL2dest. The resulting plasmid allows expression of CT695-Bla from the constitutive Nmp promoter.
The coding sequences for CT694, CT695, and CT696 were PCR-amplified from C. trachomatis L2 and mobilized into pUCNmP to create translational fusions with the downstream βlaM gene. Similar constructs containing Tarp and Euo or GroEL were generated as positive and negative secretion controls, respectively. Entry clones were subsequently transferred into pL2-dest and used to transform C. trachomatis L2. PenG selection was applied, and transformed chlamydiae were isolated by limiting dilution. None of the constructs appeared to impact chlamydial growth since progeny IFUs were unchanged at 24 hpi compared to untransformed chlamydiae (S1 Fig). HeLa cells were infected with respective strains and whole culture RNA or protein was isolated at 24 hpi to assess for trans-gene expression. qRT-PCR of total RNA was employed to assess respective transcript levels in comparison to mCherry message (Fig 4A). Similar levels of each message were detected, consistent with the use of a constitutive Nm-promoter. While mCherry transcript appeared more abundant that groEL-bla and tarp-bla, these differences were not statistically significant. Whole-culture proteins were probed in immunoblots with BlaM-specific antibodies to visualize individual chimeric proteins and Hsp60-specific antibodies as a loading control (Fig 4B). Both CT694-BLA and GroEL-BLA were detected in abundant amounts. Euo-BLA, TarP-BLA, and CT695-BLA were readily detectible but at comparably lower amounts. We were unable to detect CT696-BLA despite multiple attempts. With the exception of CT696, we therefore reasoned that chimeric proteins were expressed at sufficient levels to progress to secretion assays in Chlamydia-infected cells.
Fig 4. Expression of fusion constructs in C. trachomatis L2.
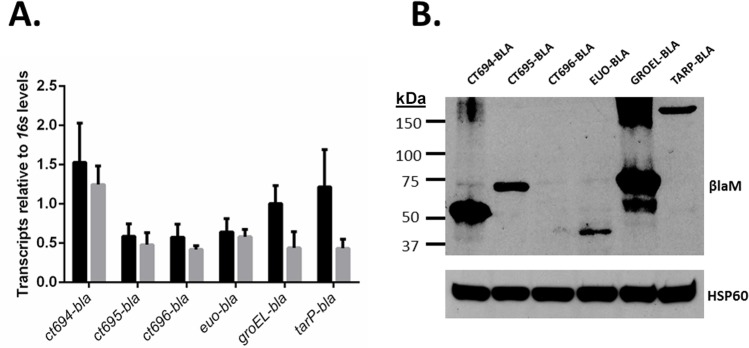
(A). Transcription of blaM fusions (grey bars) and mCherry (black bars) was measured by reverse transcription followed by quantitative real-time PCR. Levels were normalized to those of chlamydial 16s. Total RNA was isolated 24 hpi from HeLa cells infected with transformed C. trachomatis L2 at an MOI of 1. (B). Total protein was isolated 24 hpi from HeLa cells infected with transformed C. trachomatis L2 at an MOI of 1, and samples were probed with BlaM- or chlamydial Hsp60-specific monoclonal antibodies. Size standards are indicated in kDa.
We utilized the established [26] FRET disruption via BlaM-mediated cleavage of CCF2-AM to test the ability of chimeric proteins to gain access to the host cytosol. HeLa cells were infected for 24 hrs and then loaded with CCF2-AM for 30 min. Cultures were paraformaldehyde fixed and processed for confocal immunofluorescence (Fig 5). In each case, chlamydial inclusions were visualized by mCherry-derived signal. As expected, mature chlamydial inclusions were detectible in each expression strain. Disruption of FRET results in blue signal, and robust signal was detected in HeLa cytosols when CT694-BLA, CT695-BLA, or the positive control TarP-BLA were expressed by chlamydiae. Only green fluorescence—indicative of intact CCF2-AM—was prominently detected when either GroEL-BLA or Euo-BLA were expressed. The apparent lack of blue signal in the presence of CT696-BLA was inconclusive given our inability to detect this chimeric protein. We did not detect significant green or blue signal within the inclusion lumen or within bacteria. Hence it is likely that eukaryotic cytosolic esterases cleave CCF2-AM to preclude passage across the inclusion membrane. These data indicate that the BlaM reporter system is applicable during Chlamydia infection and indicate that, similar to CT694 and TarP, CT695 is a secreted chlamydial protein.
Fig 5. Detection of BlaM fusions in the cytosol of the host cell.
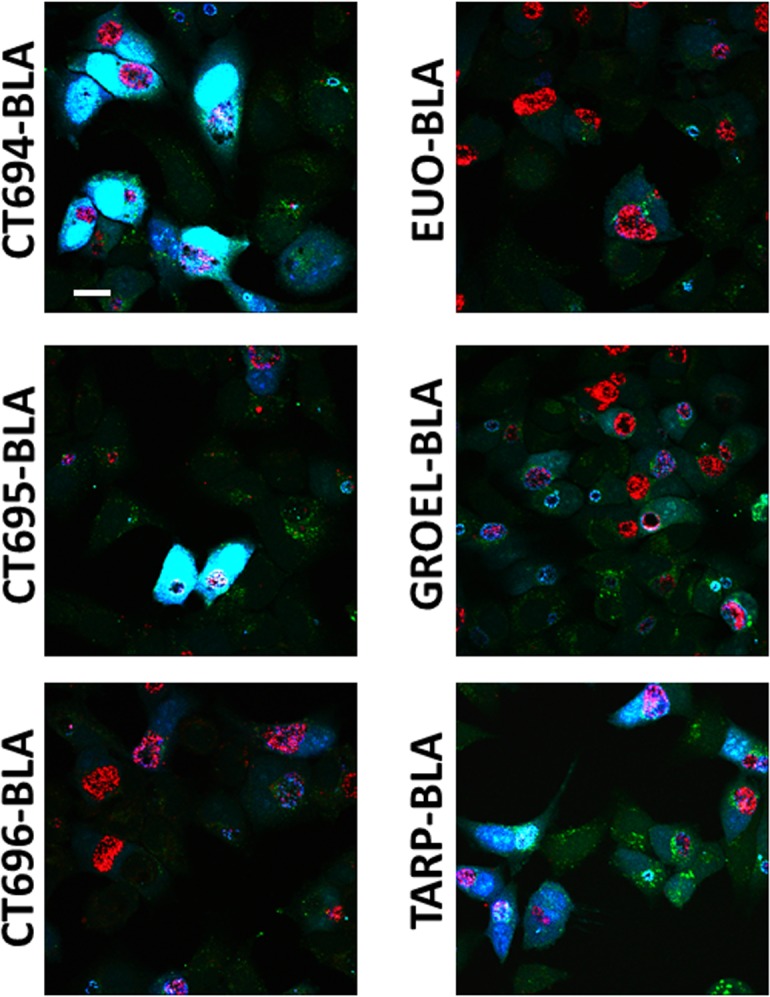
24 hpi, HeLa cells infected with transformed C. trachomatis L2 were examined for the presence of cytosolic BlaM with the GeneBLAzer Detection Kit. Samples were treated with CCF2-AM for 30 minutes, fixed with 4% paraformaldehyde, and examined by confocal microscopy. Chlamydial expression of CT694-, CT695-, and TarP-BlaM constructs produced significant blue-fluorescent signal in the cytosol of infected cells. Bar = 10 μm.
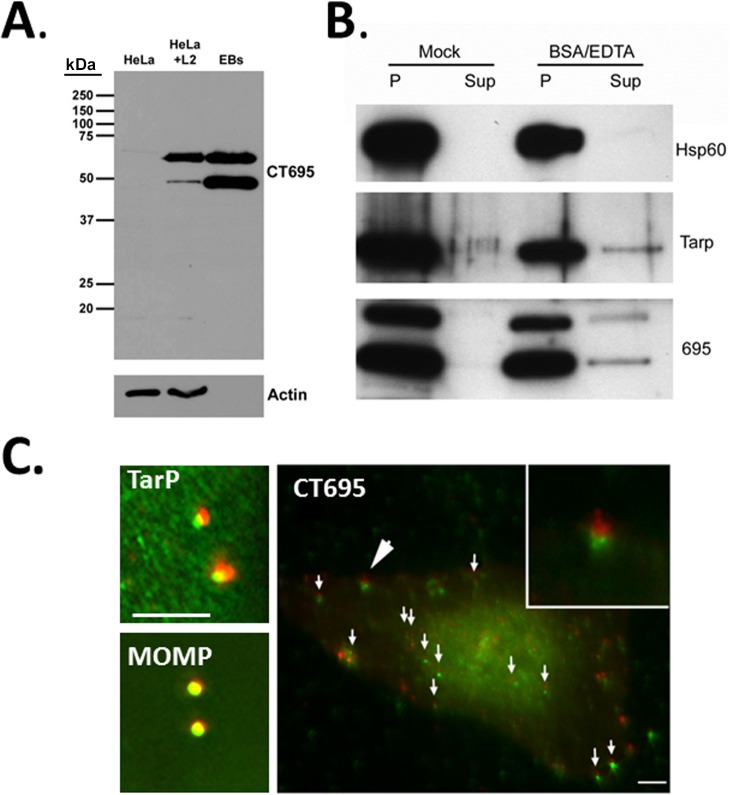
While the BlaM reporter indicates secretion, this approach does not indicate specific protein localization. We generated antibodies specific for full-length CT695 to examine CT695 immunolocalization and confirm secretion of endogenous protein. Antiserum specificity was confirmed by probing lysates of uninfected HeLa cells, C. trachomatis-infected HeLa cells or density-gradient-purified C. trachomatis EBs (Fig 6A). Interestingly, CT695 migrated as a doublet with the lower band being most abundant in EB lysates. Despite a faint cross-reactive band apparent in HeLa lysates, these antibodies appeared specific and were used in subsequent analyses. TarP is packaged in EBs and low levels of this effector can be released by treatment of purified EBs with BSA and EDTA [32,40]. To test whether CT695 behaved similarly, EBs were mock-treated or treated with BSA/EDTA followed by centrifugation to generate an EB-containing pellet and a cell-free supernatant (Fig 6B). These fractions were probed in immunoblots with our CT695-specific antibodies. Material was probed with α-Tarp as a positive control or α-Hsp60 as a negative control. All proteins were detected in EB pellets, and CT695 reproducibly migrated as a doublet. Similarly to TarP, CT695 was detected in the cell-free supernatant only after treatment with BSA and EDTA. Hsp60 was not released from EBs by this treatment. We next asked whether immunolocalization of CT695 resembled that reported for TarP and CT694 during infection [11]. HeLa cells were infected with intrinsically-labeled C. trachomatis L2 at an MOI of ca. 10 for 1 hr, fixed with paraformaldehyde, and processed for analysis via epifluorscence (Fig 6C). Red-labeled EBs marked the position of chlamydiae while MOMP, TarP, and CT695 were detected using antibodies (green). While typical background staining was visible, both TarP- and CT695-specific signal was typically detected concentrated immediately adjacent to EBs in a pattern consistent with secretion of these proteins. In contrast, MOMP-specific signal overlapped with red EBs. Taken together, these data indicate that EBs are loaded with CT695, and this pool of protein can be secreted during the invasion process.
Fig 6. CT695 is secreted by EBs during invasion.
(A). CT695-specific antibodies were used to probe lysates of Chlamydia-infected culture lysates (HeLa + L2) or lysates of purified C. trachomatis L2 EBs (EB). Lysates of corresponding uninfected HeLa cells (HeLa) were added as a negative control and all lysates were probed with α-actin as a loading control for whole-culture material. (B). Purified preparations of C. trachomatis L2 EBs were mock treated or treated with BSA and EDTA. Samples were subsequently centrifuged and material from cell-free supernatants (Sup) and chlamydiae-containing pellets (P) were probed in immunoblots with Hsp60, TarP, or CT695-specific antibodies. All proteins were visualized with HRP-conjugated secondary antibodies and subsequent chemiluminescence development. (C). HeLa cells were infected with CMPTX-labelled C. trachomatis L2 at an MOI of 10 and fixed paraformaldehyde fixed at 1 hpi. Cells were probed with TarP-, MOMP- or CT695-specific antibodies. Chlamydiae are shown in red while CT695, MOMP, and TarP localization was visualized with secondary antibodies conjugated to Alexa-488 (green). Merged channels of epifluorscence images are shown. Large arrow designates area of inset and small arrows signify other areas where CT695 appears as punctate signal adjacent to EBs. Scale bar = 5 μm.
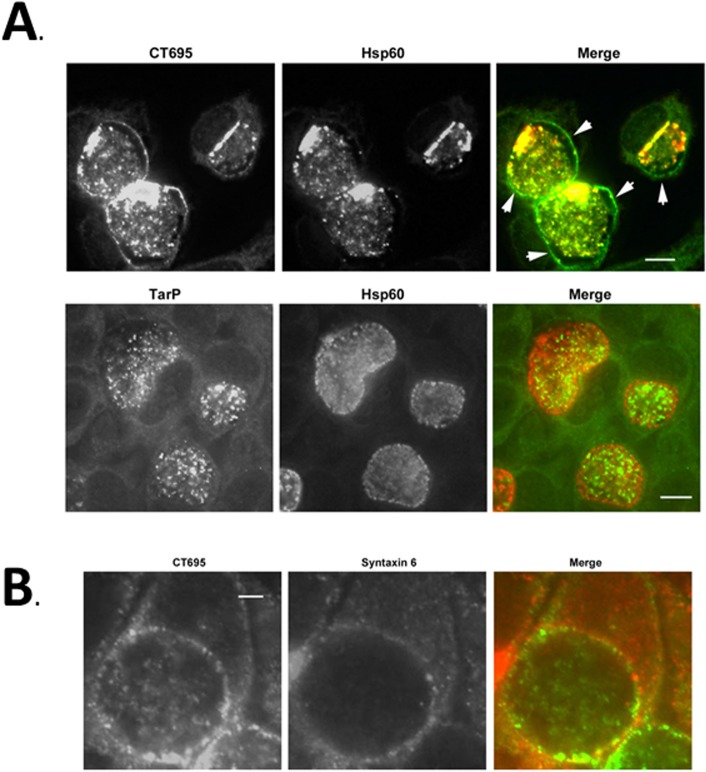
Finally, we extended our analysis to test localization of CT695 during a later stage of development. HeLa cells were infected with C. trachomatis L2 and processed for immunofluorescence microscopy at 24 hpi (Fig 7A). Staining with α-CT695 revealed signal that co-localized with Hsp60-stained chlamydiae as well as in a rim-like staining pattern typical of inclusion membrane staining. In contrast, TarP-specific staining was confined to intra-inclusion chlamydiae. The pattern was consistent with staining of EBs since inclusion membrane-localized RBs seemed to lack significant staining with α-TarP. TarP staining is comparable to CT694 which can only be detected co-localizing with bacteria at this time-point [11,41]. Host syntaxin 6 has been previously shown to associate with the C. trachomatis inclusion membrane [42]. We therefore stained inclusions with syntaxin-6 and CT695-specific antibodies to confirm inclusion membrane association of CT695 (Fig 7B). The rim-like pattern of CT695 signal overlapped with syntaxin 6-specific signal, indicating that CT695 likely accumulates in the host cytosol adjacent to the inclusion membrane. These data indicate that CT695 is secreted at later stages of development where it can associate with the inclusion membrane.
Fig 7. CT695 is secreted during late-cycle development and co-localizes with the chlamydial inclusion.
HeLa cells were infected with C. trachomatis L2 at an MOI of 1 and paraformaldehyde fixed at 24 hpi. (A). CT695 or TarP localization were assessed using α-CT695 or α-TarP, respectively. Chlamydiae were detected using α-Hsp60. Individual and merged channels of epifluorscence images are shown with specific detection of Chlamydia (red) and CT695 or TarP (green). Arrows indicate apparent inclusion membrane localization and scale bar = 10 μm. (B) HeLa cells were infected with C. trachomatis L2 at an MOI of 1 and paraformaldehyde fixed at 24 hpi. CT695 was detected with α-CT695 (green) wherease the position of the chlamydial inclusion membrane was visualized via staining with antibodies specific for Syntaxin-6 (red). Scale bar = 5 μm.
Discussion
Prior to development of techniques to genetically manipulate chlamydiae, detection of protein secretion during infection traditionally involved the use of specific antibodies to examine protein localization via indirect immunofluorescence. Detection of the putative effector in the inclusion membrane or extra-inclusion spaces represented the sole indicator that a protein was secreted by chlamydiae. The recently acquired ability to reproducibly transform Chlamydia with a stably-maintained shuttle vector [21] has opened the door to more efficacious approaches to directly test for protein secretion. For example, ectopic expression of epitope-tagged Inc proteins has surmounted the need to generate antigen-specific antibodies for a putative secreted protein [24,25]. This approach was also used to confirm secretion of the type II secretion substrate CPAF [24]. These data suggest that effector-reporter fusion proteins represent a useful approach for examination of protein secretion in a tissue-culture infection model.
Fusion of TEM-1 β-lactamase to secretion substrates was originally developed to examine T3SE secretion in pathogenic E. coli [27] and has become widely used to study secretion by extracellular and facultative-intracellular bacteria [26]. We wondered whether this approach could be adapted to an obligate intracellular pathogen such as Chlamydia. In support of this concept, BlaM fusions have been used successfully to examine protein secretion by Coxiella burnetti [43–45]. We chose to focus initial proof-of-principle experiments on the locus containing ct694-ct696. CT694 is a validated T3SE that is secreted during the invasion process and interacts with host cell AHNAK [11]. We thought it likely that CT695 could also be secreted by chlamydiae since this protein can be secreted by the heterologous Yersinia T3SS [11]. In addition, CT695 shares a common transcriptional start site [38] and chaperone [10] with CT694. We did not detect secretion of CT696 in Yersinia [11], yet de Cunha, et al [18] reported indeterminate results leaving open the possibility of low-level secretion of CT696 by yersiniae.
Hence this locus was ideal for the development of our chlamydial secretion reporter system since it contained a bona fide secretion substrate, a putative secretion substrate, and a questionable substrate.
To accomplish our goal, we generated a two-vector system to first enable general construction of BlaM fusions with any chlamydial gene downstream from a constitutive N. meningitidis promoter. We chose the constitutive Nmp promoter since it has been functionally validated in Chlamydia [21] and to avoid any regulatory complications that could arise from ectopic-overexpression from endogenous promoters. Standard primer sets enable amplification and subsequent AscI-mediated cloning into a Chlamydia shuttle vector. Transformation of Chlamydia is selected for by resistance to PenG. Constitutive expression of mCherry serves as an easily identifiable indication of transformation and as an internal control for normalization of gene expression. Genes encoding CT694, CT695, and CT696 were mobilized into Chlamydia using this system. We also included the T3SE TarP as a positive control and two non-secreted proteins, Euo and GroEL, as negative controls. The presence of neither vector-only nor chlamydial genes interfered with chlamydial development. This was true for Euo, which has been shown to repress gene transcription [46,47]. However, we anticipate that this result is likely specific to the chlamydial gene being expressed. We recommend that growth be directly assessed for each new construct since we cannot rule out the possibility that ectopic expression of other chlamydial genes could alter chlamydial development. Ectopic expression of genes in the presence of endogenous, genomic copies of respective genes was another potential complication since competition for the secretion apparatus or chaperones could have interfered with secretion. In agreement with previous studies overexpressing IncD [24,25], this did not appear to be a factor. Indeed, trans-encoded overexpression of T3SE is routine in other T3SS-expressing bacteria. Although Tarp, CT694, and CT695 share Slc1 as a secretion chaperone [10], most T3SE contain both chaperone-dependent and independent secretion signals [48]. Therefore, it is perhaps not surprising that overexpression of secretion substrates in Chlamydia is a productive approach. We cannot exclude the possibility, however, that competition among recombinant and endogenous proteins could result in false negative results in this assay.
With the exception of CT696, all constructs were well expressed in Chlamydia. Although ct696-bla transcript was produced at levels comparable to the other constructs, protein levels were below detectable limits. The precise cause of this is unclear. However, we recognize the possibility that certain proteins which are natively expressed at extremely low levels may lack the translational machinery to allow for expression of additional constructs regardless of transcript levels. This result highlights the possibility that ectopic expression may not be possible for all chlamydial gene products. Regardless, results for the remaining constructs were conclusive. BlaM fusion to CT694, CT695, and TarP all resulted in blue signal indicative of cytosolic CCF2-AM cleavage. Hence, these proteins were clearly secreted into the host cytosol. Our vector contains an additional vector-encoded blaM conferring penicillin resistance, that could have confounded results. For example, chlamydial lysis in conjunction with an unexpectedly permeable inclusion membrane could have led to spurious BlaM in the HeLa cytosol. However, Euo and especially the abundant GroEL BlaM fusions did not yield significant blue signal. In addition, an extra copy of BlaM did not confound a similar approach in C. burnetti [43]. Finally, strains have been passaged at least 8 times without loss of the intact plasmid (data not shown). Therefore recombination among multiple gene copies does not seem to be an issue. We currently have no means to confirm that secretion by Chlamydia is dependent on the T3SS. Any genetic lesion rendering T3S inactive is likely to be lethal to the bacteria. Although chemical inhibitors of type III secretion such as salicylidene acylhydrazides have been employed [49], they appear to not specifically target T3SS [50,51]. Based on secretion in heterologous T3SS [11] we can only infer this pathway for deployment.
Evidence for secretion of TarP [9] and CT694 [11,41] has been restricted to invasion. Our results are clearly consistent with continued secretion of TarP- and CT694-containing fusion proteins later in development. Whether this finding reflects temporal secretion patterns for endogenous proteins remains unclear. The T3SS is clearly active throughout chlamydial development [52], and it is possible that forced expression of TarP and CT694 could result in atypical timing for secretion. However, we were able to detect endogenous CT695 at later times since the protein was concentrated at the inclusion membrane. Since CT694 and CT695 can be transcriptionally linked, it is plausible that CT694 is also secreted during later development. Although immunoblot revealed detectible levels of CT694 throughout development [11], detection of endogenous protein via immunolocalization was likely confounded by low abundance and/or the lack of effector concentration in a specific cellular compartment.
How CT695 may be contributing to chlamydial infection remains to be determined. We detected evidence of endogenous CT695 secretion during invasion and subsequent development. We conclude that, similar to TarP, TepP, and CT694, CT695 is involved in early events necessary for chlamydiae to gain entry and-or establish an intracellular replication niche. Unlike, TarP, TepP, and CT694, ectopic expression of CT695 in yeast did not result in an overt phenotype that would give hints with regard to function [53]. The apparent localization of CT695 adjacent to the inclusion membrane is interesting. CT695 does not contain predicted trans-membrane domains and may associate with membranes through interactions with other proteins or via direct association with lipids. CT694 contains a membrane localization domain found in effectors such as Yersinia YopE and Pseudomonas ExoS [54]. It is therefore possible that CT695 could associate with membranes via a similar mechanism. Regardless, our immunolocalization studies imply that CT695 is likely a multifunctional effector necessary at multiple stages of chlamydial development.
While the BlaM reporter system does not provide information regarding effector localization, there are several advantages to using this approach. Chlamydia employ T2S, T3S, and T5S to deploy host-interactive proteins and estimates based on current findings suggest as many as 80 proteins in the chlamydial secretome [55]. Therefore, there is certainly a need for an approach to screen for secreted proteins in the context of a chlamydial infection. Although we used fixed samples for microscopy, secretion can easily be visualized in live cells using this reporter [26]. This opens numerous possibilities that include quantitative and kinetic studies of effector secretion and translocation [56]. In addition, the BlaM reporter system has been employed during animal infection studies to discriminate cell types susceptible to effector injection [57] or separate infected from bystander cells [58]. This system would also provide an efficacious platform to study the nature of T3 secretion signals. All of these approaches are adaptable for the study of Chlamydia pathogenesis. We conclude that use of BlaM fusion constructs will prove to be an efficacious approach for the study of protein secretion by chlamydiae.
Supporting Information
Triplicate cultures of HeLa cells were infected at an MOI of 1 with untransformed C. trachomatis (L2), C. trachomatis expressing pL2Dest (Vector), or C. trachomatis expressing individual BlaM-fusions. Cultures were harvested at 24 hpi and lysates were plated onto fresh HeLa monolayers. Progeny IFU counts were enumerated at 24 hpi. Mean progeny counts are shown and error bars represent one standard deviation. No statistically significant differences were observed.
(TIF)
(DOCX)
(DOC)
Acknowledgments
We thank Dr. Ian Clarke (University of Southampton) for kindly sharing pGFP::SW2. We also thank Josh Ferrell and Dr. K. Wolf critical reading of the manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work is supported by a grant from NIAID: AI065530.
References
- 1. Schachter J (1999) Infection and disease epidemiology In: Stephens RS, editor. Chlamydia; Intracellular biology, pathogenesis, and immunity. Washington, D.C.: ASM Press; pp. 139–169. [Google Scholar]
- 2. Nunes A, Gomes JP (2014) Evolution, phylogeny, and molecular epidemiology of Chlamydia . Infection, Genetics and Evolution 23: 49–64. 10.1016/j.meegid.2014.01.029 [DOI] [PubMed] [Google Scholar]
- 3. Moulder JW (1991) Interaction of chlamydiae and host cells in vitro . Microbiol Rev 55: 143–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hybiske K, Stephens RS (2007) Mechanisms of host cell exit by the intracellular bacterium Chlamydia . PNAS 104: 11430–11435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Heinzen RA, Hackstadt T (1997) The Chlamydia trachomatis parasitophorous vacuolar membrane is not passively permeable to low-molecular-weight compounds. Infect Immun 65: 1088–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Betts-Hampikian HJ, Fields KA (2010) The chlamydial type III secretion mechanism: revealing cracks in a tough nut. Frontiers in Microbiol 1: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Saka HA, Thompson JW, Chen Y-S, Kumar Y, Dubois LG, Moseley M, et al. (2011) Quantitative proteomics reveals metabolic and pathogenic properties of Chlamydia trachomatis developmental forms. Molecular Microbiology 82: 1185–1203. 10.1111/j.1365-2958.2011.07877.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fields K, Mead D, Dooley C, Hackstadt T (2003) Chlamydia trachomatis type III secretion: evidence for a functional apparatus during early-cycle development. Mol Microbiol 48: 671–683. [DOI] [PubMed] [Google Scholar]
- 9. Clifton D, Fields K, Grieshaber N, Dooley C, Fischer E, Mead D, et al. (2004) A chlamydial type III translocated protein is tyrosine-phosphorylated at the site of entry and associated with recruitment of actin. Proc Natl Acad Sci USA 101: 10166–10171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen Y-S, Bastidas RJ, Saka HA, Carpenter VK, Richards KL, Plano G, et al. (2014) The Chlamydia trachomatis Type III Secretion Chaperone Slc1 Engages Multiple Early Effectors, Including TepP, a Tyrosine-phosphorylated Protein Required for the Recruitment of CrkI-II to Nascent Inclusions and Innate Immune Signaling. PLoS Pathog 10: e1003954 10.1371/journal.ppat.1003954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hower S, Wolf K, Fields KA (2009) Evidence that CT694 is a novel Chlamydia trachomatis T3S substrate capable of functioning during invasion or early cycle development. Mol Microbiol 72: 1423–1437. 10.1111/j.1365-2958.2009.06732.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Betts HJ, Wolf K, Fields KA (2009) Effector protein modulation of host cells: examples in the Chlamydia spp. arsenal. Curr Opin Microbiol 12: 81–87. 10.1016/j.mib.2008.11.009 [DOI] [PubMed] [Google Scholar]
- 13. Gauliard E, Ouellette SP, Rueden KJ, Ladant D (2015) Characterization of interactions between inclusion membrane proteins from Chlamydia trachomatis . Front Cell Infect Microbiol 5: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mital J, Miller NJ, Dorward DW, Dooley CA, Hackstadt T (2013) Role for Chlamydial Inclusion Membrane Proteins in Inclusion Membrane Structure and Biogenesis. PLoS ONE 8: e63426 10.1371/journal.pone.0063426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fields KA, Fischer ER, Mead DJ, Hackstadt T (2005) Analysis of putative Chlamydia trachomatis chaperones Scc2 and Scc3 and their use in the identification of type III secretion substrates. J Bacteriol 187: 6466–6478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pais SV, Milho C, Almeida F, Mota LJ (2013) Identification of Novel Type III Secretion Chaperone-Substrate Complexes of Chlamydia trachomatis . PLoS ONE 8: e56292 10.1371/journal.pone.0056292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hovis KM, Mojica S, McDermott JE, Pedersen L, Simhi C, Rank R, et al. (2013) Genus optimized strategy for the identification of chlamydial type III secretion substrates. Pathog Dis 0: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. da Cunha M, Milho C, Almeida F, Pais S, Borges V, Mauricio R, et al. (2014) Identification of type III secretion substrates of Chlamydia trachomatis using Yersinia enterocolitica as a heterologous system. BMC Microbiology 14: 40 10.1186/1471-2180-14-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Subtil A, Delevoye C, Balana M, Tastevin L, Perrinet S, Dautry-Varsat A (2005) A directed screen for chlamydial proteins secreted by a type III mechanism identifies a translocated protein and numerous other new candidates. Mol Microbiol 56: 1636–1647. [DOI] [PubMed] [Google Scholar]
- 20. Fields K, Hackstadt T (2000) Evidence for the secretion of Chlamydia trachomatis CopN by a type III secretion mechanism. Mol Microbiol 38: 1048–1060. [DOI] [PubMed] [Google Scholar]
- 21. Wang Y, Kahane S, Cutcliffe LT, Skilton RJ, Lambden PR, Clarke IN (2012) Development of a Transformation System for Chlamydia trachomatis: Restoration of Glycogen Biosynthesis by Acquisition of a Plasmid Shuttle Vector. PLoS Pathog 7: e1002258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Agaisse H, Derré I (2013) A C. trachomatis Cloning Vector and the Generation of C. trachomatis Strains Expressing Fluorescent Proteins under the Control of a C. trachomatis Promoter. PLoS ONE 8: e57090 10.1371/journal.pone.0057090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wickstrum J, Sammons LR, Restivo KN, Hefty PS (2013) Conditional Gene Expression in Chlamydia trachomatis Using the Tet System. PLoS ONE 8: e76743 10.1371/journal.pone.0076743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bauler LD, Hackstadt T (2014) Expression and Targeting of Secreted Proteins from Chlamydia trachomatis . Journal of Bacteriology 196: 1325–1334. 10.1128/JB.01290-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Agaisse H, Derré I (2014) Expression of the Effector Protein IncD in Chlamydia trachomatis Mediates Recruitment of the Lipid Transfer Protein CERT and the Endoplasmic Reticulum-Resident Protein VAPB to the Inclusion Membrane. Infection and Immunity 82: 2037–2047. 10.1128/IAI.01530-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Campbell-Valois FX, Sansonetti PJ (2014) Tracking bacterial pathogens with genetically-encoded reporters. FEBS Letters 588: 2428–2436. 10.1016/j.febslet.2014.05.022 [DOI] [PubMed] [Google Scholar]
- 27. Charpentier X, Oswald E (2004) Identification of the Secretion and Translocation Domain of the Enteropathogenic and Enterohemorrhagic Escherichia coli Effector Cif, Using TEM-1 β-Lactamase as a New Fluorescence-Based Reporter. Journal of Bacteriology 186: 5486–5495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carabeo R, Grieshaber S, Hasenkrug A, Dooley C, Hackstadt T (2004) Requirement for the Rac GTPage in Chlamydia trachomatis invasion of non-phagocytic cells. Traffic 5: 418–425. [DOI] [PubMed] [Google Scholar]
- 29. Caldwell HD, Kromhout J, Schachter J (1981) Purification and partial characterization of the major outer membrane protein of Chlamydia trachomatis . Infect Immun 31: 1161–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chellas-Gery B, Linton CN, Fields KA (2007) Human GCIP interacts with CT847, a novel Chlamydia trachomatis type III secretion substrate, and is degraded in a tissue-culture infection model. Cell Microbiol 9: 2417–2430. [DOI] [PubMed] [Google Scholar]
- 31. Geiser M, Cebe R, Drewello D, Schmitz R (2001) Integration of PCR fragments at any specific site within cloning vectors without the use of restriction enzymes and DNA ligase. BioTechniques 31: 88–92. [DOI] [PubMed] [Google Scholar]
- 32. Jamison WP, Hackstadt T (2008) Induction of type III secretion by cell-free Chlamydia trachomatis elementary bodies. Microb Pathog 45: 435–440. 10.1016/j.micpath.2008.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Scidmore-Carlson M, Shaw E, Dooley C, Fischer E, Hackstadt T (1999) Identification and characterization of a Chlamydia trachomatis early operon encoding four novel inclusion membrane proteins. Mol Microbiol 33: 753–765. [DOI] [PubMed] [Google Scholar]
- 34. Baehr W, Zhang YX, Joseph T, Su H, Nano FE, Everett KD, et al. (1988) Mapping antigenic domains expressed by Chlamydia trachomatis major outer membrane protein genes. Proc Natl Acad Sci U S A 85: 4000–4004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stephens RS, Kalman S, Lammel C, Fan J, Marathe R, Aravind L, et al. (1998) Genome sequence of an obligate intracellular pathogen of humans: Chlamydia trachomatis . Science 282: 754–759. [DOI] [PubMed] [Google Scholar]
- 36. Kingsford C, Ayanbule K, Salzberg SL (2007) Rapid, accurate computational discovery of Rho-independent transcription terminators illuminates their relationship to DNA uptake. Genome Biol 8: R22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Belland RJ, Zhong G, Crane DD, Hogan D, Sturdevant D, Sharma J et al. (2003) Genomic transcriptional profiling of the developmental cycle of Chlamydia trachomatis . Proc Natl Acad Sci U S A 100: 8478–8483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Albrecht M, Sharma CM, Reinhardt R, Vogel J, Rudel T (2010) Deep sequencing-based discovery of the Chlamydia trachomatis transcriptome. Nucleic Acids Research 38: 868–877. 10.1093/nar/gkp1032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hefty PS, Stephens RS (2007) Chlamydial type III secretion system is encoded on ten operons preceded by sigma 70-like promoter elements. J Bacteriol 189: 198–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Spaeth KE, Chen YS, Valdivia RH (2009) The Chlamydia type III secretion system C-ring engages a chaperone-effector protein complex. PLoS Pathog 5: e1000579 10.1371/journal.ppat.1000579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sharma J, Zhong Y, Dong F, Piper JM, Wang G, Zhong G (2006) Profiling of human antibody responses to Chlamydia trachomatis urogenital tract infection using microplates with 156 chlamydial fusion proteins. Infect Immun 74: 1490–1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Moore ER, Mead DJ, Dooley CA, Sager J, Hackstadt T (2011) The trans-Golgi SNARE syntaxin 6 is recruited to the chlamydial inclusion membrane. Microbiology 157: 830–838. 10.1099/mic.0.045856-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Beare P, Sandoz K, Omsland A, Rockey D, Heinzen R (2011) Advances in genetic manipulation of obligate intracellular bacterial pathogens. Frontiers in Microbiology 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Voth DE, Beare PA, Howe D, Sharma UM, Samoilis G, Cockrell DC, et al. (2011) The Coxiella burnetii Cryptic Plasmid Is Enriched in Genes Encoding Type IV Secretion System Substrates. Journal of Bacteriology 193: 1493–1503. 10.1128/JB.01359-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Carey KL, Newton HJ, Lührmann A, Roy CR (2011) The Coxiella burnetii Dot/Icm System Delivers a Unique Repertoire of Type IV Effectors into Host Cells and Is Required for Intracellular Replication. PLoS Pathog 7: e1002056 10.1371/journal.ppat.1002056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rosario CJ, Hanson BR, Tan M (2014) The transcriptional repressor EUO regulates both subsets of Chlamydia late genes. Molecular Microbiology 94: 888–897. 10.1111/mmi.12804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rosario CJ, Tan M (2012) The early gene product EUO is a transcriptional repressor that selectively regulates promoters of Chlamydia late genes. Molecular Microbiology 84: 1097–1107. 10.1111/j.1365-2958.2012.08077.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hueck CJ (1998) Type III protein secretion systems in bacterial pathogens of animals and plants. Microbiol Mol Biol Rev 62: 379–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Keyser P, Elofsson M, Rosell S, Wolf-Watz H (2008) Virulence blockers as alternatives to antibiotics: type III secretion inhibitors against Gram-negative bacteria. J Intern Med 264: 17–29. 10.1111/j.1365-2796.2008.01941.x [DOI] [PubMed] [Google Scholar]
- 50. Engström P, Nguyen BD, Normark J, Nilsson I, Bastidas RJ, Gylfe A, et al. (2013) Mutations in hemG mediate resistance to Salicylidene acylhydrazides: A novel link between protoporphyrinogen oxidase (HemG) and Chlamydia trachomatis infectivity. Journal of Bacteriology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Slepenkin A, Enquist P, Hagglund U, de la Maza L, Elofsson M, Peterson EM (2007) Reversal of the antichlamydial activity of putative type III secretion inhibitors by iron. Infect Immun 75: 3478–3489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Mueller KE, Plano GV, Fields KA (2014) New Frontiers in Type III Secretion Biology: the Chlamydia Perspective. Infection and Immunity 82: 2–9. 10.1128/IAI.00917-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sisko J, Spaeth K, Kumar Y, Valdivia R (2006) Multifunctional analysis of Chlamydia-specific genes in a yeast expression system. Mol Microbiol 60: 51–66. [DOI] [PubMed] [Google Scholar]
- 54. Bullock HD, Hower S, Fields KA (2012) Domain analyses reveal that C. trachomatis CT694 belongs to the membrane-localized family of type III effector proteins. J Biol Chem 287: 28078–28086. 10.1074/jbc.M112.386904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Fields KA (2012) Secretion Mechanisms and Chlamydia pathogenesis In: Tan M, Bavoil P, editors. Intracellular Pathogens I: Chlamydiales. Washington, DC: ASM Press; pp. 192–216. [Google Scholar]
- 56. Mills E, Baruch K, Charpentier X, Kobi S, Rosenshine I (2008) Real-Time Analysis of Effector Translocation by the Type III Secretion System of Enteropathogenic Escherichia coli . Cell Host & Microbe 3: 104–113. [DOI] [PubMed] [Google Scholar]
- 57. Marketon MM, DePaolo RW, DeBord KL, Jabri B, Schneewind O (2005) Plague Bacteria Target Immune Cells During Infection. Science 309: 1739–1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Copenhaver AM, Casson CN, Nguyen HT, Fung TC, Duda MM, Roy CR, et al. (2014) Alveolar Macrophages and Neutrophils Are the Primary Reservoirs for Legionella pneumophila and Mediate Cytosolic Surveillance of Type IV Secretion. Infection and Immunity 82: 4325–4336. 10.1128/IAI.01891-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Triplicate cultures of HeLa cells were infected at an MOI of 1 with untransformed C. trachomatis (L2), C. trachomatis expressing pL2Dest (Vector), or C. trachomatis expressing individual BlaM-fusions. Cultures were harvested at 24 hpi and lysates were plated onto fresh HeLa monolayers. Progeny IFU counts were enumerated at 24 hpi. Mean progeny counts are shown and error bars represent one standard deviation. No statistically significant differences were observed.
(TIF)
(DOCX)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.