Abstract
OBJECTIVE
To assess knowledge of the human papillomavirus (HPV), cervical cancer, and HPV vaccination in African American women (AAW).
STUDY DESIGN
This study was a quantitative cross-sectional survey of English speaking, AAW, ages 18-70 recruited from a community fair in Chicago, IL. Surveys were distributed to a convenience sample to assess knowledge of HPV, cervical cancer, and the HPV vaccine. Cumulative knowledge scores were calculated for each participant and analysis was performed to identify factors associated with adequate knowledge scores.
RESULTS
322 surveys were distributed, 242 surveys were collected, and 215 met inclusion criteria. Mean knowledge score was 12.3 ± 4.2 (mean ± SD) out of a maximum score of 28 (range 3-23); 73% of participants scored <65% on the knowledge portion of the survey. Education level (P=0.007), household income (P=0.010), and having a child that had been offered the HPV vaccine (P=0.041) were associated with adequate (≥65% accuracy) knowledge scores.
CONCLUSION
Knowledge of HPV, cervical cancer and HPV vaccination was low in this urban African American adult female population. Targeted educational health programs are needed in order to increase awareness among these women who have the highest rate of cervical cancer mortality in the United States. Such patient educational programs need to be developed by physicians and should address the cultural and literacy needs of this particular group of women. In addition, AAW exert influence on the health of their communities and are integral in health-related decision making, thus educating them through their healthcare providers will have far ranging impact.
Keywords: barriers, cervical cancer, human papillomavirus, knowledge, vaccination
INTRODUCTION
Despite the advancements in early detection, cervical cancer remains the third most common gynecologic malignancy in women in the United States. In 2013, the American Cancer Society (ACS) estimates 12,340 new cases of cervical cancer will be diagnosed and 4,030 women will die from cervical cancer [1, 2]. More recently, further advances in the understanding of cervical cancer have led to the identification of the Human Papillomavirus (HPV) as the causative agent in over 99.7% of cervical cancer cases [3]. In the United States, HPV is the most common sexually transmitted disease, infecting 6.2 million people each year [3-5]. With the further identification of high-risk strains of HPV as the causative agent for cervical cancer, vaccines against these specific strains of HPV have subsequently been developed, leading to the hope that cervical cancer can become not just a highly detectable disease, but also a highly preventable one.
In June 2006, the United States Food and Drug Administration approved the vaccine Gardasil®, a quadrivalent vaccine that prevents infection against 4 strains of the HPV virus, two of which (16 and 18) are responsible for over 70% of cases of cervical cancer [4]. The drug initially was approved for use in girls and young women 9-26 years of age and in 2009, its use was expanded to boys and young men 9-26 years of age. Also in 2009, a second vaccine targeting high-risk HPV strains 16 and 18 (Cervarix) was approved by the FDA, joining Gardasil as the first approved vaccines targeted specifically to prevent any type of cancer. Since their release, studies have shown that these vaccines are effective in preventing nearly 100% of the precancerous cervical cell changes caused by the strains of HPV targeted by the vaccine [6]. With the advent of an HPV vaccination, cervical cancer rates are expected to decline even further, with the National Cancer Institute predicting that “widespread vaccination has the potential to reduce cervical cancer deaths around the world by as much as two-thirds ...” [7].
Despite the development of promising vaccines against the causative agent of cervical cancer, vaccination rates within the United States remain extremely low [8, 9]. Epidemiologic data further demonstrate that HPV vaccination rates vary according to certain demographics, with the lowest rates of vaccination occurring in low-income, minority groups. Specifically, African Americans have been documented as having the lowest HPV vaccination rates. This finding is particularly concerning because, of all women affected by cervical cancer, African American women are most likely to die as a result of the disease. This high mortality rate exists among African American women despite having one of the highest Pap smear participation rates compared to women of other races and ethnicities [2, 10].
Barriers to HPV vaccination in the general population include access to healthcare, cultural beliefs, and lack of communication and education between healthcare providers and patients regarding vaccination recommendations [11, 12]. In addition, several studies have been performed to investigate underlying causes of identified disparities, but have focused primarily on adolescent and young adult populations. To our knowledge, no studies have specifically addressed barriers to HPV vaccination among African American women.
The overall goal of this study is to explore targetable barriers to HPV vaccination among African American women in an urban Chicago population. Specifically, this study focuses on disease and vaccination knowledge, which have been shown to directly affect vaccination rates in other populations. Unlike prior studies, however, this report is specifically focused on urban adult African American women and their knowledge about HPV, cervical cancer, and HPV vaccination.
MATERIALS AND METHODS
Subjects
This cross-sectional survey study was reviewed and approved by the Northwestern University Institutional Review Board. A convenience sample was recruited from attendees of a community fair in Chicago, IL. A designated area existed in which women could approach and receive a description of the study. Verbal consent was obtained from all study participants. Eligibility criteria included English-speaking women who self-identified as African American and were aged 18 to 70. Study participants were compensated for their time with $5.00 gift cards.
Surveys
Surveys were developed based on “The Awareness of HPV and Cervical Cancer Questionnaire,” a validated HPV Knowledge and Awareness tool developed by Ingledue et al. in 2004 to assess knowledge and beliefs related to HPV and cervical cancer [13]. Participants completed self-administered paper surveys, which included 28 items assessing knowledge of female anatomy, HPV and HPV vaccination, and demographic questions. Knowledge was assessed using multiple-choice response questions; e.g.. “There is a vaccine that protects against HPV: A) Yes B) No C) I don't know; and “A Pap smear is a screening test for: A) Ovary cancer B) Lung cancer C) Breast cancer D) Colon cancer E) Cervix cancer F) I don't know.” Surveys contained no personal identifying information.
Statistical Analyses
Study results were entered into a database and data entry accuracy was confirmed by two of the investigators. A cumulative HPV knowledge score was determined for each participant based on survey responses. Survey responses were dichotomized; each correct answer received a score of 1, whereas incorrect responses, including “I don't know,” received a score of 0. HPV knowledge was categorized as “adequate” if there were 18 or greater (approximately 2/3 or 64%) correct responses of the 28 knowledge questions. Chi-square analysis was used to test the association between categorical variables in this cross-sectional survey study. A p-value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS (PASW version 18) software.
RESULTS
A total of 322 surveys were distributed and 242 were completed, for a 75.2% response rate, and 215 met eligibility criteria. Of the 27 participants excluded, 19 surveys had missing data, 7 participants did not identify themselves as African American, and 1 did not meet age criteria. The mean age of participants was 48.2 years of age (SD 12.1 years). Eighty-seven percent of participants had an education level of high school or above and 32% of participants had household income levels of >$40,000/year. We had 26 participants eligible for the vaccine and 9 of them had been offered the vaccine, accounting for a total of 34.6% participants eligible for the vaccine personally being offered the vaccine. Furthermore, of those who had children, only 28% of the children had been offered the HPV vaccine. Tables 1, 2 and 3 provide additional details regarding participant demographic, personal health, and women's health information.
Table. 1.
Demographic Characteristics of Participants (N=215)
| Median (Range) | |
|---|---|
| Age | 50(18-70) |
| Number of Children | 2(1-6) |
| Number of Grandchildren | 4(1-18) |
| N(%) | |
| Race | |
| African American/Black | 215(100) |
| Ethnicity | |
| Hispanic/Latino | 4(1.9) |
| Non-Hispanic/Non-Latino | 156(72.6) |
| Education | |
| High school graduate | 56(26) |
| Some college courses | 75(34.9) |
| College graduate | 56(26) |
| Post-graduate courses | 15(7) |
| Other | 12(5.6) |
| Partnering Status | |
| Single | 118(54.9) |
| Married | 48(22.3) |
| Widowed | 12(5.6) |
| Divorced | 31(14.4) |
| Living with significant other | 3(1.4) |
| Income Level | |
| Less than $20,000 | 89(41.4) |
| $21,000 - $40,000 | 57(26.5) |
| $41,000 - $60,000 | 33(15.3) |
| $61,000 - $80,000 | 20(9.3) |
| Greater than $80,000 | 8(3.7) |
Table. 2.
Personal Medical History
| N (%) | |
|---|---|
| Health Insurance | |
| No Insurance | 57(26.5) |
| HMO | 35(16.3) |
| Medicaid/Medicare | 64(29.8) |
| Private Insurance | 45(20.9) |
| Not sure | 9(4.2) |
| Last Doctor Visit | |
| Within the last year | 164(76.4) |
| 2-3 years ago | 26(12.1) |
| 4-5 years ago | 11(5.1) |
| 6-10 years ago | 5(2.3) |
| Greater than 10 years ago | 5(2.3) |
| Pap Smear Ever | |
| Yes | 200(93) |
| No | 12(5.6) |
| Last Pap Smear | |
| Within the last year | 122(56.7) |
| 2-3 years ago | 53(24.7) |
| 4-5 years ago | 15(7) |
| 6-10 years ago | 13(6) |
| Greater than 10 years ago | 8(3.7) |
| Abnormal Pap Smear | |
| Yes | 74(34.4) |
| No | 128(59.5) |
Table. 3.
Personal Experience with HPV
| N(%) | |
|---|---|
| Offered HPV Vaccine | |
| Yes | 33(15.3) |
| No | 163(75.8) |
| I don't know | 13(6.0) |
| Children Offered HPV Vaccine | |
| Yes | 47(28.7) |
| No | 85(51.8) |
| I don't know | 26(15.9) |
| Received HPV Vaccine | |
| Yes | 15(7.0) |
| No | 173(80.5) |
| I don't know | 17(7.9) |
| Children Received HPV Vaccine | |
| Yes | 29(17.7) |
| No | 100(61.0) |
| I don't know | 30(18.3) |
| Reason Child Did Not Get Vaccine | |
| Concern over side effects | 8(4.9) |
| Costs | 13(7.9) |
| Not enough information to make decision | 17(10.4) |
| Not offered | 27(16.5) |
| Concerns about sexual promiscuity | 3(1.8) |
| Other | 12(7.3) |
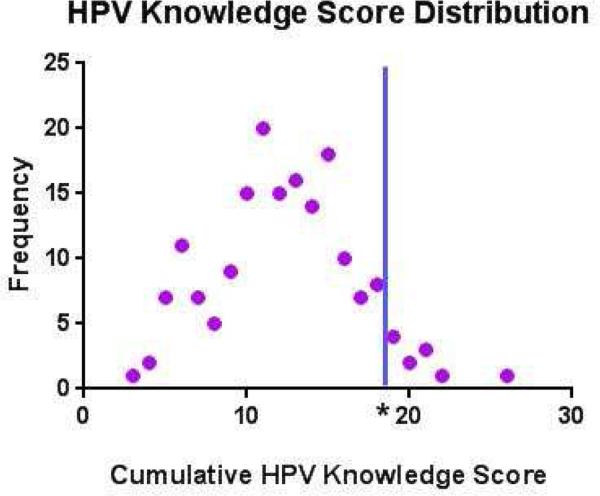
Out of 28 knowledge questions regarding HPV, cervical cancer, and HPV vaccines, the mean knowledge score was 12.3 ± 4.2 (mean ± SD). Overall knowledge scores ranged from 3 to 23. Three-fourths of the participants scored <65% on the knowledge score portion of the survey. Figure 1 demonstrates the distribution of knowledge scores by participants.
Figure 1.
Distribution of HPV Knowledge Scores. Frequencies of total cumulative HPV knowledge scores by participants are shown. *Indicates cutoff for adequate HPV knowledge (≥18 out of 28 questions answered correctly)
While 93% of participants were able to correctly identify the cervix when presented with a drawing, 33% were unable to correctly identify that a pap smear is performed on the cervix and only 58% recognized a pap smear as a screening test for cervical cancer.
The percentage of participants who knew there is a vaccine that protects against HPV was 61%; however, only 37% of participants correctly answered that a virus is the cause of cervical cancer. The participants who knew that cervical cancer can be diagnosed by a Pap smear were 74% while only 35% of participants could correctly identify factors that can prevent cervical cancer, including vaccination, pap smears, and delayed onset of sexual activity. When asked to identify risk factors for cervical cancer, participants identified risks factors correctly less than 50% of the time. Further, only 2% were able to identify women who were at highest risk of getting cervical cancer (Hispanics), while 42% of participants were able to identify African Americans as the group at highest risk of dying from cervical cancer.
Using a cut-off score of 18 out of 28 as an adequate knowledge score, 73% of participants demonstrated low knowledge scores regarding HPV, cervical cancer, and the HPV vaccine. Chi-square analysis demonstrated that education levelΧ2 (4, N = 175) = 13.96, P=0.007, household incomeΧ2 (4, N = 169) = 13.18, P=0.010 and having a child who had been offered the HPV vaccineΧ2 (2, N = 131) = 13.96, P=0.041 were factors positively associated with adequate knowledge scores. Having had a pap smear or having seen a doctor within the past year were not significantly associated with adequate knowledge scores.
COMMENT
Our findings demonstrate that the majority of middle-aged African American women demonstrated low knowledge scores regarding HPV, cervical cancer, and the HPV vaccine. These findings, generally consistent with results of previous reports in other target populations [14-16], emphasize the need for continuing health education in adults on these issues. While this study found that higher levels of education, higher household income, and having a child that had been offered the HPV vaccine were significantly associated with adequate knowledge scores in African American women, most women (73%), even those with demographics favoring high levels of health knowledge, still demonstrated a lack of HPV, cervical cancer, and HPV vaccine knowledge.
In 2010, Dell and colleagues studied knowledge of HPV among high-school age adolescents in Canada and found that knowledge of HPV infection and cervical screening was low in this adolescent population, with only 13% of participants having heard of the HPV virus and only 39% knowing who should be receiving pap smears for cervical cancer screening [14]. Yacobi et al. found similar results in a study investigating university age students and their awareness of HPV. In their study, only 37% of students had ever heard of HPV and on a thirteen-item knowledge test, average scores were 3 [15]. Both of these studies, in addition to the findings of our current study, demonstrate that despite high prevalence of HPV in these populations, knowledge of HPV is low. If knowledge level affects vaccination decisions, a low knowledge level in this population of women could contribute to low vaccination rates.
Prior studies have focused primarily on adolescents or college-age women; this study, however, focuses on a unique demographic of African American women with a larger range of ages (18-70 years old) with a median age of 50 years. This population is important not because they are candidates themselves but are caretakers of young girls and boys who should be being faced with decisions for HPV vaccination. A study by Watts el al. in 2009 highlights the importance of vaccine knowledge in this age group of women. Watts et al. examined attitudes regarding HPV vaccination in Latina and non-Latina women and found that the most common barriers were insufficient knowledge about the vaccine and the belief that their daughter(s) did not have any risk factors for HPV infection [17]. The results of the Watts study highlight the importance of establishing a foundation of knowledge in not just at-risk individuals eligible for the vaccines, but also on their caretakers/role models (i.e., mothers, aunts, teachers, etc.) who may provide the path to vaccination for community children.
The goal of our healthcare system is for patients to see their healthcare providers as a trusted and reliable source of information. Having health care providers educate patients on HPV would increase HPV prevention and decrease incidence of cervical cancer. There have been a number of effective HPV educational programs involving health care providers which have either increased the knowledge of HPV or the intent of receiving the HPV vaccine. In a study by Wetzel et al., health care providers developed an HPV educational protocol for adolescents and found an increase in HPV knowledge in adolescents of different ages, gender, and races [18].
While the findings of this study are compelling, there are limitations to interpretation of the data. In this convenience sample of middle-aged women, we found that the focus on urban African American women may limit the generalizability of our findings. Despite these limitations, given the prevalence of HPV and the mortality of cervical cancer in the African American community, we feel that this study raises critical issues on the need for improved education and outreach in this community. Future targeted interventions should include partnerships with trusted community organizations (churches, schools, community-based clinics) to develop tailored, culturally informed and community supported education and decision making support.
In summary, our study focused on knowledge of cervical cancer, the HPV virus and the HPV vaccine within an urban African American community and found that knowledge was low. Given the promising advances in prevention and detection of early cervical cancer in the United States, disparities in the use of these resources is concerning and is a reflection of a number of inadequacies in our health system. Given our ability to largely eradicate cervical cancer, the stark racial disparities in prevalence and mortality rates are inexcusable. Future studies that incorporate health belief modeling and drivers of health behavior may be of benefit on this issue. Educational health programs and interventions that focus on improving knowledge of HPV, cervical cancer, and HPV vaccines in adult African American women is warranted.
Condensation.
African American women in urban setting demonstrate low levels of knowledge regarding HPV, cervical cancer and HPV vaccination.
ACKNOWLEDGEMENTS
We thank Northwestern University, Northwestern Memorial Hospital, Robert H. Lurie Comprehensive Cancer Center, National Institutes of Health, and the Apostolic Church of God, in addition to the Friends of Prentice organization for support of this research. We also thank the women taking part in this study, our research assistants, administrative assistants, and many others who made this study possible.
Support for this study was provided by the Robert H. Lurie Comprehensive Cancer Center, Northwestern Memorial Hospital and Northwestern University in Chicago, IL (EEM). Further support for this study was provided by the National Institutes of Health Grant K12HD050121, Agency for Healthcare Research and Quality 1 P01 HS021141-1 (KAC) the Northwestern University Women's Reproductive Health Research (WRHR) Scholar Award (EEM), the Harold Amos Medical Faculty Development Award, and the Robert Wood Johnson Foundation (EEM), and the Friends of Prentice Women's Health Research Award (EEM).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflicts of interest.
Portions of this data were presented at the 60th Annual Scientific Meeting of the Society for Gynecologic Investigation, Orlando, FL, March 20-23, 2013.
REFERENCES
- 1.American Cancer Society Cervical Cancer. 2013 Available at: http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-key-statistics.
- 2.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2010. National Cancer Institute; Bethesda, MD: 2013. Available at: http://seer.cancer.gov/csr/1975_2010/, based on November 2012 SEER data submission, posted to the SEER website, April. [Google Scholar]
- 3.Bosch FX, Lorincz A, Muñoz N, Meijer CJ, Shah KV. The Causal Relation Between Human Papillomavirus and Cervical Cancer. J Clinical Pathology. 2002;55(4):244–65. doi: 10.1136/jcp.55.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER, Centers for Disease Control and Prevention (CDC); Advisory Committee on Immunization Practices (ACIP) Quadrivalent Human Papillomavirus Vaccine: Recommendations of the Advisory Committee on Immunization Practice (ACIP). MMWR: Recommendations and Reports. 2007;56(2):1–24. [PubMed] [Google Scholar]
- 5.Parkin D. The Global Health Burden of Infection-Associated Cancers in the Year 2002. International Journal of Cancer. 2002;118:3030–44. doi: 10.1002/ijc.21731. [DOI] [PubMed] [Google Scholar]
- 6.National Cancer Institute Human Papillomavirus (HPV) Vaccines. 2011 [Google Scholar]
- 7.Steinbrook R. The Potential of Human Papillomavirus Vaccines. N Engl J Med. 2006;354:1109–12. doi: 10.1056/NEJMp058305. [DOI] [PubMed] [Google Scholar]
- 8.Watson M, Saraiya M, Benard V, et al. Burden of cervical cancer in the United States, 1998-2003. Cancer. 2008;113(10 Suppl):2855–2864. doi: 10.1002/cncr.23756. [DOI] [PubMed] [Google Scholar]
- 9.Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors Associated with HPV Vaccine Uptake in Teenage Girls: A Systematic Review. Vaccine. 2012;30(24):3546–56. doi: 10.1016/j.vaccine.2012.03.063. [DOI] [PubMed] [Google Scholar]
- 10.National Center for Health Statistics . Health, United Stated, 2009: With Special Feature on Medical Technology. Hyattsville, MD.: 2010. [PubMed] [Google Scholar]
- 11.Garner E. Cervical Cancer: Disparities in Screening, Treatment, and Survival. Cancer Epidemiology, Biomarkers, and Prevention. 2003;12:242s–7s. [PubMed] [Google Scholar]
- 12.Downs LS, Scarinci I, Einstein MH, Collins Y, Flowers L. Overcoming the Barriers to HPV Vaccination in High-Risk Populations in the US. Gynecologic Oncology. 2010;117:486–90. doi: 10.1016/j.ygyno.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 13.Ingledue K, Cotrell R, Bernard A. College women's knowledge, perceptions, and preventative behaviors regarding HPV and cervical cancer. American Journal of Health Studies. 2004;19(1):28–35. [Google Scholar]
- 14.Dell DL, Chen H, Ahmad F, Stewart DE. Knowledge About Human Papillomavirus Among Adolescents. American Journal of Obstetrics and Gynecology. 2000;96(5 Pt 1):653–6. doi: 10.1016/s0029-7844(00)01009-7. [DOI] [PubMed] [Google Scholar]
- 15.Yacobi E, Tennant C, Ferrante J, Pal N, Roetzheim R. University Students' Knowledge and Awareness of HPV. Preventative Medicine. 1999;28:535–41. doi: 10.1006/pmed.1999.0486. [DOI] [PubMed] [Google Scholar]
- 16.Kennedy S, Osgood R, Rosenbloom L, Feinglass J, Simon MA. Knowledge of Human Papillomavirus Among Publicly and Privately Insured Women. J Midwifery & Women's Health. 2011;56(5):481–7. doi: 10.1111/j.1542-2011.2011.00040.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watts LA, Joseph N, Wallace M, et al. HPV Vaccine: A Comparison of Attitudes and Behavioral Perspectives Between Latino and non-Latino Women. Gynecologic Oncology. 2010;112(3):577–582. doi: 10.1016/j.ygyno.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 18.Wetzel C, Tissot A, Kollar LM, Hillard PA, Stone R, Kahn JA. Development of an HPV Educational Protocol for Adolescents. J Pediatr Adolesc Gynecol. October. 2007;20(5):281–87. doi: 10.1016/j.jpag.2006.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]