Abstract
Mobile, community-based HIV testing may help achieve universal HIV testing in South Africa. We compared the yield, geographic distribution, and demographic characteristics of populations tested by mobile- and clinic-based HIV testing programs deployed by iThembalabantu Clinic in Durban, South Africa. From July–November 2011, 4,701 subjects were tested; HIV prevalence was 35% among IPHC testers and 10% among mobile testers (p<0.001). Mobile testers varied in mean age (22–37 years) and % males (26–67%). HIV prevalence at mobile sites ranged from 0% to 26%. Testers traveled further than the clinic closest to their home; mobile testers were more likely to test ≥ 5 km away from home. Mobile HIV testing can improve testing access and identify testing sites with high HIV prevalence. Individuals often access mobile testing sites farther from home than their nearest clinic. Geospatial techniques can help optimize deployment of mobile units to maximize yield in hard-to-reach populations.
Keywords: Geospatial Analysis, HIV mobile testing, South Africa
INTRODUCTION
South Africa remains highly affected by the HIV epidemic, with a prevalence of 18% among people aged 15 to 49 (1). In an effort to improve access to HIV care and treatment, the South African government advocated for increased HIV screening and implemented a national testing campaign (1); by 2011, 13 million South Africans had been HIV tested (1). More recently, the South African National Strategic Plan reinforced the ambitious goal of testing for HIV at least annually (2). Though testing has increased recently, more remains to be done (3). Mobile HIV testing in community venues is becoming an increasingly attractive way of promoting HIV testing particularly among men, those with earlier stage HIV disease, and people who may not otherwise access testing through the healthcare system (4, 5). This novel screening method could help move South Africa towards achieving the goal of universal, annual HIV testing.
Though mobile units allow for expanded HIV case detection compared to clinic-based testing alone (4, 6), little is known about the characteristics of the mobile community-based testing sites where testing units are deployed. Geospatial analyses and geographic information systems (GIS) have been used to determine “hot spots” of infectious disease and their spatial variation (7–10). Having a better understanding of disease distribution in the community can help optimize deployment of mobile testing units; previous studies have shown the advantages of using GIS to determine factors impacting access to and use of healthcare services (11–13) and in healthcare intervention planning (9). We evaluated the yield and characteristics of population tested at sites visited by mobile HIV testing units deployed by the iThembalabantu Clinic in the Umlazi Township, in Durban, South Africa. Our objective was to better understand how to optimize deployment of mobile HIV testing units.
METHODS
Testing Sites
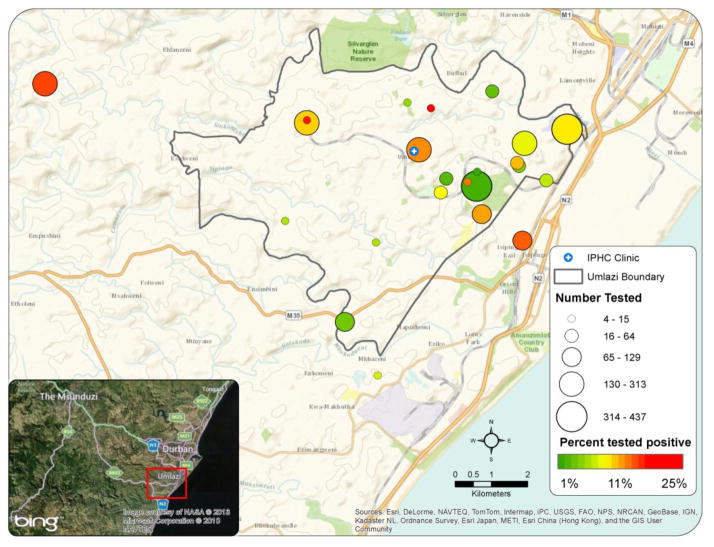
The study was conducted in Umlazi, a township located on the East Coast of KwaZulu-Natal province, southwest of Durban, South Africa (Figure 1). Umlazi is the largest township outside of Durban with a population of between 550,000 and 1,000,000 people, one third of whom live in informal housing (14, 15). iThembalabantu, “The People’s Hope,” Clinic has been offering HIV care in Umlazi since 2002. Funded by the AIDS Healthcare Foundation and working in collaboration with the South African Department of Health, iThembalabantu currently has close to 13,000 adults and children in HIV care. The clinic is located in a business district near a small mall and a post office, with dense residential areas nearby. iThembalabantu offers two different kinds of HIV testing: clinic-based testing and mobile community-based testing via 1–2 testing units deployed daily. The mobile units visit different venues, such as taxi stands, markets, and malls in Umlazi and surrounding areas, on a rotating basis. Currently, there is no algorithm to decide where to send the units to optimize yield. iThembalabantu raises awareness of the mobile testing campaign through print media, radio, and loudspeakers (16). In addition to iThembalabantu, 11 primary health clinics within Umlazi offer clinic-based HIV testing and treatment. The 11 clinics’ geospatial coordinates were used for calculating distances only; no participants were enrolled at these clinics.
Figure 1. Geospatial distribution and HIV prevalence of mobile testing sites.
The grey line delineates the Umlazi Township boundary. The size of the circles show the number of patients tested at the specific mobile sites and the color of the circles illustrate the HIV prevalence at the sites during the study period. Green represents lowest prevalence, red is highest prevalence. Isipingo is not included in this map.
IPHC: iThembalabantu “the People’s Hope” Clinic
Study Population
We prospectively collected programmatic data for adults (≥15 years) who self-presented for testing at the mobile HIV testing units (mobile testers) and at the iThembalabantu HIV clinic (IPHC testers) from July to November 2011. The study was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee and the Partners Human Research Committee (2011-P-001195 and 2003-P-001019).
Demographic and Clinical Data Collection
Testers were offered HIV pre-test counseling and responded to an oral questionnaire. The questionnaire included demographic and health information. Participants underwent HIV testing using rapid HIV test kits as per South African guidelines (17) and results were available to the tester within 25 minutes. Testers at the mobile unit were taken to a separate area to receive their results, for privacy. Patients who were diagnosed with HIV, both on the mobile testing units and at IPHC, were offered phlebotomy for CD4 count testing and were asked to retrieve their CD4 count results at the iThembalabantu Clinic two weeks later.
Geospatial Data Collection
Routine clinical intake forms for all testers were used to obtain demographic details and self-reported residential addresses; clinic registers provided information regarding whether testers returned to iThembalabantu to retrieve their CD4 count results. The patients’ residential addresses were manually geocoded. We restricted our analysis to testers with home addresses within Umlazi Township due to the detailed nature of Umlazi addresses, which allowed for complete geocoding, as well as the availability of a municipal road shapefile of Umlazi. GPS coordinates were obtained at 24 mobile unit testing sites, iThembalabantu Clinic, and 11 other Umlazi clinics offering HIV testing and care; coordinates were mapped using ArcGIS (Esri, Redlands, CA, USA). ArcGIS and the municipal road shapefile were used to calculate distances by road between patients’ home and the site where they tested, as well as their nearest clinic. Each testing site was characterized by tester-specific factors (gender, age, and average distance traveled by clients) and by testing site-specific factors (number of subjects tested, newly-diagnosed HIV infection rates, likelihood of obtaining a CD4 test at the testing site and returning for results at IPHC, and type of venue, such as markets, taxi stands, and university campuses).
Statistical Analysis
We compared demographic characteristics, HIV prevalence, and distance traveled for testing among mobile unit testers compared to IPHC testers using chi-squared tests for categorical data and Wilcoxon rank-sum tests for continuous variables. Age was divided into 5-year intervals that approximated quartiles. We also assessed the yield and characteristics of different mobile testing sites, and mapped the geospatial distribution of the mobile testing sites, incorporating testers’ demographic information and HIV infection rates at each site. Mobile testing sites were classified as having a “high” newly diagnosed infection rate if the rate at that site was greater than the overall newly diagnosed rate across all sites.
RESULTS
Characteristics of mobile compared to IPHC testers
From July–November 2011, 5,327 participants who self-reported residential addresses within Umlazi underwent HIV testing at the mobile testing units and at the iThembalabantu clinic in Umlazi. Of those, 4,701 (88%) participants had addresses that were successfully geocoded, and this sub-sample was used for this analysis (2,802 mobile testers and 1,899 IPHC testers). Subjects whose addresses could not be geocoded had a statistically similar HIV prevalence as subjects included in the study (p=0.374).
Among the 4,701 participants included in this analysis, a greater proportion of mobile testers were male compared to IPHC testers: 47% vs. 43% (p = 0.002). Mobile testers were significantly younger than IPHC testers (mean age 28 years vs. 32 years, p =0.002). The HIV infection rate was substantially lower among mobile testers (10%) compared to IPHC testers (35%) (p<0.001, Table I). Among those infected with HIV, mobile testers were less likely to have a CD4 count done than those tested at IPHC (45% vs. 86%, p<0.001), and to return to IPHC for the results (23% vs. 77%, p<0.001).
Table I.
Characteristics of those tested, by testing site category
| Mobile testers (2,802) | IPHC testers (1,899) | p-value | |
|---|---|---|---|
| Gender (%) | 0.002 | ||
| Male | 47 | 43 | |
| Female | 53 | 57 | |
| Age, mean (SD) | 28 (12) | 32 (61) | 0.002 |
| Age distribution (%) | |||
| 15–20 | 32 | 20 | |
| 21–25 | 25 | 25 | |
| 26–30 | 14 | 21 | |
| >30 | 29 | 34 | |
| HIV prevalence by age (%) | |||
| 15–20 | 4 | 12 | |
| 21–25 | 10 | 25 | |
| 26–30 | 15 | 43 | |
| >30 | 14 | 50 | |
| Overall (%) | 10 | 35 | <0.001 |
| CD4 test performed (%) | 45 | 86 | <0.001 |
| Return for CD4 count result (% of those who got a CD4 test) | 23 | 77 | <0.001 |
| Distance between testers’ home and testing site (median, IQR) | 2.1 [0.8–4.9] | 2.5 [1.8–3.5] | <0.001 |
Characteristics of the mobile sites
Testers at mobile sites varied in mean age (22–37 years) and proportion male (26–67%). HIV prevalence from mobile sites varied depending on the kind of venue, from 0–4% at a university campus to 26% at a commercial venue (Figure 1; green is low prevalence, red is high). Taxi stands at major transport junctions and commercial sites had the highest HIV prevalence (17–26%). College residences had the lowest HIV prevalence (0–4%, Table II). Eleven mobile testing sites (46%) were classified as having high infection rates (greater than the overall rate for mobile sites). Compared to those testing at mobile testing sites with lower infection rates, the testers at the high infection rate sites were older (mean age 31 vs. 26, p<0.001) and more likely to be male (51% vs. 45%, p<0.001). On average, the people who tested the furthest away from home received their HIV test at the largest commercial center in Umlazi, Mega City (distance = 7.4 km).
Table II.
Mobile testing site characteristics from a study in Umlazi Township, Durban, South Africa
| Site Namea | HIV Prev. (%) [95% CI]) | Male (%) | Age (Mean) | N | Distance between patients’ home and testing site (km) (median [IQR])* | Site characteristics |
|---|---|---|---|---|---|---|
| Gama stores | 25.5 [15.0–40.0] | 29.8 | 32 | 47 | 0.3 [0.2–0.7] | Informal supermarket |
| J supermarket | 21.9 [13.3–33.7] | 51.6 | 33 | 64 | 1.0 [0.8–1.4] | Supermarket close to train station |
| Mhlabeni | 18.9 [9.2–35.0] | 40.5 | 31 | 37 | 0.5 [0.5–2.7] | Informal settlement; highly populated |
| Mkhanzini taxi rank | 16.7 [8.8–29.2] | 51.9 | 30 | 54 | N/A | Transport intersection to exit Umlazi |
| Engonyameni | 15.8 [11.3–21.6] | 56.1 | 30 | 196 | N/A | Rural settlement near Umlazi |
| Ithala Mall | 14.1 [10.1–19.3] | 50.2 | 31 | 227 | 2.4 [1.6–3.5] | Mall near iThembalabantu; intra-Umlazi taxi stand |
| St James | 13.3 [3.2–41.8] | 46.7 | 26 | 15 | N/A | Church; dense township environment |
| Uganda | 13.2 [8.3–20.2] | 31.8 | 35 | 129 | 4.9 [0.4–6.5] | Informal settlement; near water access site |
| Glebelands Hostel | 12.2 [5.1–26.4] | 48.8 | 28 | 41 | 1.3 [1.0–2.5] | Worker’s residential hostel |
| J Station | 11.0 [7.8–15.4] | 64.3 | 28 | 263 | 1.4 [0.7–2.1] | Main train station near dense housing |
| Mega City | 9.7 [7.2–13.0] | 45.6 | 28 | 421 | 7.4 [4.4–8.7] | Main shopping mall for Umlazi |
| V Fani’s supermarket | 9.6 [6.8–13.4] | 51.0 | 27 | 312 | 0.9 [0.5–2.7] | Mall by busy transportation junction |
| Kwa Mnyandu | 8.7 [4.6–16.0] | 55.3 | 26 | 103 | 2.3 [1.8–3.4] | Residential hostels; near train station |
| Jeenas | 8.2 [3.4–18.3] | 52.5 | 37 | 61 | 5.5 [2.7–7.7] | Area near mall; dense housing |
| Philani Mall | 7.5 [3.4–15.8] | 53.8 | 26 | 80 | 2.0 [0.8–4.4] | Mall; near informal settlement in western Umlazi |
| F Shell garage | 7.0 [2.2–19.7] | 44.2 | 24 | 43 | 0.9 [0.5–1.2] | Busy garage on taxi route |
| Z taxi rank | 5.9 [1.9–16.9] | 64.7 | 29 | 51 | 0.9 [0.5–1.8] | Busy intersection; major taxi rank |
| BB Fani’s supermarket | 3.9 [1.0–14.6] | 66.7 | 27 | 51 | 0.9 [0.7–1.4] | Small supermarket and convenience store |
| D wash | 3.5 [1.1–10.4] | 45.9 | 32 | 85 | 0.7 [0.5–1.5] | Car wash and mall; busy area |
| E Ezitolo | 3.6 [1.4–9.3] | 33.3 | 24 | 111 | 0.6 [0.3–0.8] | Mall; adjacent to several schools and butcher |
| MUT Main Campus | 3.6 [1.9–6.6] | 25.9 | 22 | 278 | 2.6 [1.5–4.8] | Technology University |
| V-FET Residence | 3.2 [1.0–9.5] | 40.4 | 22 | 94 | 3.4 [1.8–7.1] | Technical college residence hall |
| Uni Zulu | 0.0 [N/A] | 37.8 | 25 | 37 | 2.4 [1.7–3.5] | University campus |
| Isipingob | 50.0 [1.9–98.1] | 50.0 | 36 | 2 | N/A | Town neighboring Umlazi |
| Totalc | 9.9 | 47.1 | 28 | 2802 | 2.1 [0.8–4.9] |
Letters in site names refer to sections in Umlazi Township.
Isipingo had only 2 testers. The values from this site are not included in the map.
Total means are included for convenience but are not meant to represent population estimates.
N/A: Median distance not calculated for testing sites outside of Umlazi.
Distance results for mobile testers
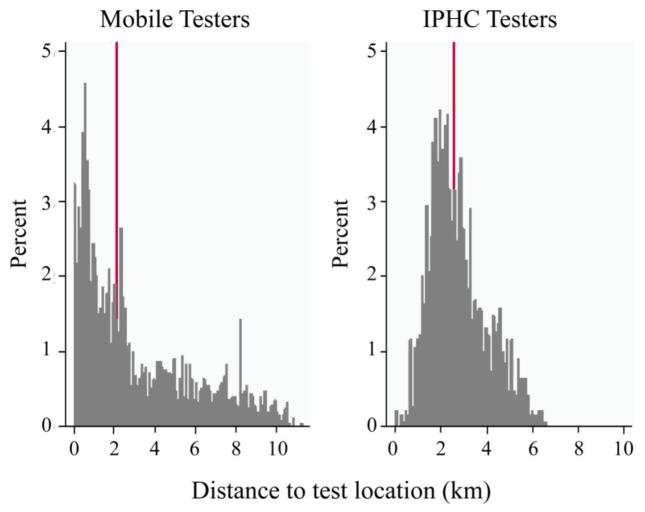
Although the median distance from participants’ homes to the nearest clinic offering HIV services was 1.4 km (IQR: 1.0–1.9 km), the median distance between all of the testers’ homes and their testing site was 2.4 km (IQR: 1.3–4.1 km) (p<0.001). Sixty-four percent of mobile testers lived closer to their nearest clinic than to the mobile site where they tested. Among mobile testers, the median distance between home and the site where they tested was less than among IPHC testers (2.1 km [IQR: 0.8–4.9 km] vs. 2.5 km [IQR: 1.8–3.5 km], p<0.001), and mobile testers were much more likely than IPHC testers to be tested within 1 km of where they lived (31% vs. 4%, p<0.001). However, mobile testers were also more likely than IPHC testers to be tested ≥ 5 km away from home (24% vs. 7%, p<0.001) (Figure 2).
Figure 2. Distribution of IPHC and mobile testers by distance traveled to test location.
This graph shows the distribution of IPHC and mobile testers by the distance between their home and the site of HIV testing. The red line represents the median distance (mobile testers 2.1 km [IQR: 0.8–4.9 km], IPHC testers 2.5 km [IQR: 1.8–3.5 km], p<0.001).
There was a small but statistically significant difference in median distance between HIV-infected and HIV-negative patients’ home and their chosen testing site (2.7 km [IQR: 1.8–4.0 km] vs. 2.3 km [IQR: 1.2–4.1 km], p<0.001). HIV-infected clients who underwent CD4 count testing lived closer to iThembalabantu clinic than those who did not (3.0 km [IQR 2.1–4.1 km] vs. 3.4 km IQR [2.4–4.4 km], p=0.0034). IPHC testers lived significantly closer to iThembalabantu Clinic than mobile testers (2.5 km [IQR: 1.8–3.5 km] vs. 3.8 km [IQR: 2.8–4.6 km], p<0.001). Testers for whom iThembalabantu was the closest clinic to home were more likely to receive a CD4 count test (82% vs. 72%, p=0.031) but not to return to iThembalabantu for their CD4 test results (73% vs. 66%, p=0.212).
DISCUSSION
The iThembalabantu People’s Hope Clinic mobile testing units in Umlazi Township, outside of Durban, attract a large number of HIV testers. Mobile unit testers had a lower HIV prevalence and were more likely to be younger and male than IPHC testers. The testing sites varied widely in HIV infection rates, number of people tested, and how far from home people chose to get tested. Those who tested at the mobile units had access to clinics closer to their homes, suggesting that testers valued other considerations over proximity to home in choosing location for testing.
The mobile testing units attracted hard-to-reach populations. Specifically, compared to the clinic, the mobile units test proportionally more men—who are less likely than women to get tested for HIV in clinic-based testing programs (3, 18). Mobile testing also attracts proportionally more young people, which is especially important since their HIV prevalence is high and prevalence increases rapidly with age (1, 3). As has been shown previously, mobile units also tend to test people at earlier stages of HIV disease (4). Though the overall HIV prevalence at the mobile units is lower than at the clinic, the mobile vans were able to detect 280 new cases of HIV in this five-month sample.
The sites with the highest HIV prevalence were supermarkets and taxi ranks. These areas attract mobile populations and have dense commercial activity, characteristics that have been associated with high HIV transmission in other studies (19, 20). The malls, taxi ranks, and transport junctions were high-volume testing sites that generally had a much higher percentage of male testers. The higher concentration of males in these sites could be due to the fact that males generally visit these sites more than women. Focusing on these sites may be a good strategy to increase the yield of male testers. In contrast, university campuses had generally much lower prevalence. The HIV infection rate of 0–4% at the campuses is consistent with the 3% rate reported in the 2010 nationwide survey and a survey conducted at the University of KwaZulu Natal (21, 22). The majority of people tested at the university campuses were women, who are more likely to be infected than men, even among students (23). The Mangosuthu University of Technology main university campus had one of the lowest HIV rates (4%).
Almost a quarter of mobile patients got tested for HIV more than 5 km away from their homes. This may indicate that some people prefer being tested for HIV further from their homes, where they will not be recognized. Stigma and discrimination have been shown to discourage people from attending health care facilities (24) and to reduce the effect of interventions (8). Similarly, one study in India found that women did not test at facilities in the area in which they lived, but rather traveled to a different location to get tested for HIV (25). In that way, mobile testing sites provide an additional opportunity for people who wish to test away from home. This effect could explain why more mobile testers traveled more than 5 km away from their home to get tested (Figure 2). However, the mobile testing units may also be located near patients’ place of work or venues they like to visit and therefore be more convenient. Since people who test at mobile units are less symptomatic and more likely HIV negative, deciding to test at a mobile unit, rather than at a clinic, may reflect convenience rather than stigma. More research is warranted to understand why patients choose their specific testing sites. Implementing interventions to encourage HIV testing where people actively seek testing, rather than where they live, may be efficient and still have substantial yield.
Although proximity has been shown to be a key factor in utilizing health services previously (11), living close to a clinic where testing is available does not mean that patients consider that clinic convenient. The typically long wait times in clinics in South Africa (26) may lead testers to go to mobile units where wait times may be shorter. Our data show that living near iThembalabantu did increase the rate of having a CD4 count performed but not of coming back to retrieve CD4 count results. These results reinforce the need for more point-of-care CD4 tests—especially for people who do not live near the clinic and are less likely to come back—since providing immediate results on the mobile unit has been shown at other sites to increase retention in care (27–29) and to be cost-effective (30). Undergoing CD4 count testing is a crucial step in evaluating eligibility for starting ART, which, in turn, is essential in curbing the HIV epidemic.
Using GIS mapping also allows an assessment of the spatial distribution of HIV in a dense township setting. HIV prevalence is not evenly distributed in South Africa and, as can be seen from these data, prevalence at different sites within Umlazi Township alone is heterogeneous. Although the overall HIV prevalence in KwaZulu Natal among 15 to 49 year olds is 28% (2012) (31), the prevalence at the different sites ranged from 0 to 26%, even between neighboring sites in close proximity. GIS data can therefore help inform the rationale for more targeted testing interventions (8, 32). Baseline data can also help identify hot spots in the community, based on both prevalence and on the number of people tested. Increasing the frequency of mobile unit visits to high infection rate areas may saturate the number of new HIV testers and yield the maximum number of new cases in the community. However, until linkage to care improves, the impact of any testing initiative will be limited (4, 7). Linkage to care interventions may be particularly important for mobile testers, who may be less symptomatic and not accessing a formal health care site at the time of testing.
This study has several limitations. First, some patient addresses were not specific enough to obtain a precise geocode. Second, we limited our analysis to people who lived within Umlazi, though people who live outside the township were also tested at the mobile units; they may have different characteristics compared to testers living in Umlazi. Third, some sites had a small number of testers. These small sample sizes could artificially magnify the overall prevalence. On the other hand, some sites were visited more than once and there may be some variability in HIV prevalence depending on the visit day. The data collected do not allow for sub-analyses based on specific visit days to any particular site. The HIV prevalence at each site should be carefully evaluated in the context of the number of people tested before specific sites are determined to be “hot spots.” Because we used programmatic patient data, we do not have additional patient characteristics that may inform patient preference for mobile or clinic testing. Lastly, we do not know if mobile testers sought CD4 count or other HIV services at clinics other than iThembalabantu in Umlazi. Assessment of CD4 count retrieval was only performed at iThembalabantu; if patients received their CD4 count results elsewhere, they would not be accounted for in this analysis.
Mobile, community-based HIV testing can identify areas of high HIV prevalence and improve access to testing. Individuals commonly access mobile testing sites that are farther from home than their nearest clinic. However, people who lived further away from the clinic were less likely to return to clinic to link to care. Geospatial techniques can be useful for optimizing deployment of mobile units in communities to maximize yield and access hard-to-reach populations by targeting sites that have either a higher yield of people who are HIV positive or higher number of males visiting them. Although it is possible that the patients who were diagnosed with HIV at the mobile units could have eventually been HIV-diagnosed at clinics, we have previously shown that mobile testers tend to have higher CD4 counts at diagnosis than testers diagnosed at the clinic (4, 33). Mobile testing presents a unique opportunity to identify people earlier in their HIV disease and is cost-effective when added to clinic-based screening in South Africa (34). GIS data illustrate the distribution of HIV in Umlazi in a tangible way (8), which may appeal to public health officials seeking to optimize mobile testing and other HIV testing initiatives. These results are multidimensional, providing information from the distance people travel to undergo testing—thereby providing some insight into the barriers patient may experience to access clinics to—actual infection rates and yield data. Deploying mobile units in the highest yield locations, combined with interventions to encourage linkage to care and prevention interventions in high activity areas (35), could dramatically increase the number of HIV cases detected, particularly among hard-to-reach populations such as men, and ultimately drive down the number of undetected infections and thereby HIV transmission.
Acknowledgments
We would like to acknowledge the assistance of Njabulo Mabaso and Philisiwe Luthuli and the dedication of the research team at the iThembalabantu People’s Hope Clinic. Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases and National Institute of Mental Health of the National Institutes of Health under Awards R01 MH090326, R01 AI058736 and R01 MH073445. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This project was also supported by the AIDS Healthcare Foundation and the Harvard Center for AIDS Research (P30 AI042851).
Footnotes
Conflict of Interest
The authors declare no conflicts of interest.
References
- 1.Republic of South Africa Department of Health. [Accessed 24 April 2014];Global AIDS Response Progress Report. 2012 Available at: http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_ZA_Narrative_Report.pdf.
- 2.Republic of South Africa Department of Health. [Accessed on 24 April 2014];National Strategic Plan on HIV, STIs and TB. 2012–2016 Available at: http://laylacassim.co.za/pdf/National%20Strategic%20Plan%20on%20HIV,%20STIs%20and%20TB.pdf.
- 3.Shisana O, Rehle T, Simbayi L, Zuma K, Jooste S, Zungu N, et al. South African National HIV Prevalence, Incidence and Behaviour Survey 2012. Cape Town: HSRC Press; 2014. [DOI] [PubMed] [Google Scholar]
- 4.Bassett IV, Regan S, Luthuli P, Mbonambi H, Bearnot B, Pendleton A, et al. Linkage to care following community-based mobile HIV testing in Umlazi township, Durban, South Africa. HIV Medicine. 2014;15(6):367–72. doi: 10.1111/hiv.12115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Govindasamy D, Kranzer K, van Schaik N, Noubary F, Wood R, Walensky RP, et al. Linkage to HIV, TB and non-communicable disease care from a mobile testing unit in Cape Town, South Africa. PLoS One. 2013;8(11):e80017. doi: 10.1371/journal.pone.0080017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mabuto T, Latka MH, Kuwane B, Churchyard GJ, Charalambous S, Hoffmann CJ. Four models of HIV counseling and testing: utilization and test results in South Africa. PLoS One. 2014;9(7):e102267. doi: 10.1371/journal.pone.0102267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goswami ND, Hecker EJ, Vickery C, Ahearn MA, Cox GM, Holland DP, et al. Geographic information system-based screening for TB, HIV, and syphilis (GIS-THIS): a cross-sectional study. PLoS One. 2012;7(10):e46029. doi: 10.1371/journal.pone.0046029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kandwal R, Garg PK, Garg RD. Health GIS and HIV/AIDS studies: Perspective and retrospective. J Biomed Inform. 2009;42(4):748–55. doi: 10.1016/j.jbi.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 9.Geanuracos CG, Cunningham SD, Weiss G, Forte D, Reid LM, Ellen JM. Use of geographic information systems for planning HIV prevention interventions for high-risk youths. Am J Public Health. 2007;97(11):1974–81. doi: 10.2105/AJPH.2005.076851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tanser F, Barnighausen T, Grapsa E, Zaidi J, Newell ML. High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science. 2013;339(6122):966–71. doi: 10.1126/science.1228160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tanser F, Gijsbertsen B, Herbst K. Modelling and understanding primary health care accessibility and utilization in rural South Africa: an exploration using a geographical information system. Soc Sci Med. 2006;63(3):691–705. doi: 10.1016/j.socscimed.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 12.Yao J, Agadjanian V, Murray AT. Spatial and social inequities in HIV testing utilization in the context of rapid scale-up of HIV/AIDS services in rural Mozambique. Health Place. 2014;28:133–41. doi: 10.1016/j.healthplace.2014.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yao J, Murray AT, Agadjanian V, Hayford SR. Geographic influences on sexual and reproductive health service utilization in rural Mozambique. Appl Geogr. 2012;32(2):601–607. doi: 10.1016/j.apgeog.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.KA Economic Development Consulting CC. [Accessed 24 April 2014];Umlazi local economic development plan. 2008 Available at: http://www.durban.gov.za/Documents/Invest_Durban/Economic%20Development/5.pdf.
- 15.United Nations Human Settlements Programme. Situational analysis of informal settlements in the city of Durban (Ethekwini) Umlazi & Kenville/Sea-Cow Lake. [Accessed 7 July 2014];Cities without slums sub-regional programme for Eastern and Southern Africa. 2007 Available at: http://mirror.unhabitat.org/pmss/listItemDetails.aspx?publicationID=2336.
- 16.Mbonambi H, Mukuvisi D, Ngwenya P, Maphlala N, Thulare H, Buzaalirwa L, et al. First steps in HIV: how people get to know about mobile outreach testing HIV testing events—a review of self reported data from Umlazi, KwaZulu-Natal Province, South Africa. 19th International AIDS Conference; Washington, DC, USA. 2012; [abstract TUPE743] [Google Scholar]
- 17.Republic of South Africa Department of Health. [Accessed on 24 April 2014];HIV counselling and testing (HCT) policy guidelines. Available at: http://www.sanac.org.za/resources/cat_view/1-resources.
- 18.World Health Organization, UNAIDS, UNICEF. [Accessed 24 April 2014];Global HIV/AIDS Response. Epidemic update and health sector progress towards Universal Access. 2011 Available at: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/20111130_UA_Report_en.pdf.
- 19.Ferguson AG, Morris CN. Mapping transactional sex on the Northern Corridor highway in Kenya. Health Place. 2007;13(2):504–19. doi: 10.1016/j.healthplace.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Tanser F, Barnighausen T, Cooke GS, Newell ML. Localized spatial clustering of HIV infections in a widely disseminated rural South African epidemic. Int J Epidemiol. 2009;38(4):1008–16. doi: 10.1093/ije/dyp148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.IRIN. [Accessed 24 April 2014];South Africa: low HIV prevalence rates on campus. 2010 Available at: http://www.irinnews.org/report/88611/south-africa-low-hiv-prevalence-rates-on-campus.
- 22.University of KwaZulu-Natal. [Accessed 24 April 2014];Results of HIV survey. Available at: http://www.ukzn.ac.za/media-publications-reports/reports/results-of-hiv-survey.
- 23.Mbabela Z. Student have lower HIV rate. [Accessed 24 April 2014];Times Live. 2010 Available at: http://www.timeslive.co.za/local/article379275.ece/Students-have-lower-HIV-rate.
- 24.Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sex Transm Infect. 2003;79(6):442–7. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kandwal R, Augustijn EW, Stein A, Miscione G, Garg PK, Garg RD. Geospatial analysis of HIV-related social stigma: a study of tested females across mandals of Andhra Pradesh in India. Int J Health Geogr. 2010;9:18. doi: 10.1186/1476-072X-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schneider H, Naidoo N, Ngoma B, Goudge J, Williams E, Pursell R, Nyatela H, Lubwama J. Performance and capacity of second-generation Comprehensive care Management and Treatment (CCMT) sites in Gauteng Province. [Accessed April 24, 2014];Research Report. 2008 Available at: http://www.wits.ac.za/files/res80af2836b7614a19ab43d30a3df6fd6e.pdf.
- 27.Jani IV, Sitoe NE, Alfai ER, Chongo PL, Quevedo JI, Rocha BM, et al. Effect of point-of-care CD4 cell count tests on retention of patients and rates of antiretroviral therapy initiation in primary health clinics: an observational cohort study. Lancet. 2011;378(9802):1572–9. doi: 10.1016/S0140-6736(11)61052-0. [DOI] [PubMed] [Google Scholar]
- 28.Larson BA, Schnippel K, Ndibongo B, Xulu T, Brennan A, Long L, et al. Rapid point-of-care CD4 testing at mobile HIV testing sites to increase linkage to care: an evaluation of a pilot program in South Africa. J Acquir Immune Defic Syndr. 2012;61(2):e13–7. doi: 10.1097/QAI.0b013e31825eec60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Faal M, Naidoo N, Glencross DK, Venter WD, Osih R. Providing immediate CD4 count results at HIV testing improves ART initiation. J Acquir Immune Defic Syndr. 2011;58(3):e54–9. doi: 10.1097/QAI.0b013e3182303921. [DOI] [PubMed] [Google Scholar]
- 30.Hyle E, Jani I, Lehe J, Wood R, Su AE, Quevedo J, et al. The Clinical and Economic Impact of Point of Care CD4 Testing in Resource-Limited Settings: a Cost-Effectiveness Analysis. PLoS Med. 11(9):e1001725. doi: 10.1371/journal.pmed.1001725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van der Linde I. [Accessed 24 April 2014];Plenary Session 3, 20 June 2013 - “HIV/AIDS in South Africa: At last the glass is half full”. Available at: http://www.hsrc.ac.za/en/media-briefs/hiv-aids-stis-and-tb/plenary-session-3-20-june-2013-hiv-aids-in-south-africa-at-last-the-glass-is-half-full.
- 32.McNabb ME, Hiner CA, Pfitzer A, Abduljewad Y, Nadew M, Faltamo P, et al. Tracking working status of HIV/AIDS-trained service providers by means of a training information monitoring system in Ethiopia. Hum Resour Health. 2009;7:29. doi: 10.1186/1478-4491-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Schaik N, Kranzer K, Wood R, Bekker LG. Earlier HIV diagnosis--are mobile services the answer? S Afr Med J. 2010;100(10):671–4. doi: 10.7196/samj.4162. [DOI] [PubMed] [Google Scholar]
- 34.Bassett IV, Govindasamy D, Erlwanger AS, Hyle EP, Kranzer K, van Schaik N, et al. Mobile HIV screening in Cape Town, South Africa: clinical impact, cost and cost-effectiveness. PLoS One. 2014;9(1):e85197. doi: 10.1371/journal.pone.0085197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barnighausen T, Tanser F, Gqwede Z, Mbizana C, Herbst K, Newell ML. High HIV incidence in a community with high HIV prevalence in rural South Africa: findings from a prospective population-based study. AIDS. 2008;22(1):139–44. doi: 10.1097/QAD.0b013e3282f2ef43. [DOI] [PubMed] [Google Scholar]