Abstract
Attention-deficit/hyperactivity disorder (ADHD) is associated with interpersonal dysfunction during childhood and adolescence, yet little is known about the romantic relationships of young women with childhood ADHD. In the present study, we draw from a longitudinal sample of girls followed prospectively into young adulthood, comparing those with (n = 114) and without (n = 79; comparisons) childhood ADHD in terms of their risk for physical victimization by an intimate partner (physical IPV; e.g., slapping, punching) by 17–24 years of age. We examined ADHD both diagnostically and dimensionally, at the same time establishing reliable indicators of young adult physical IPV. Externalizing and internalizing problems, and academic achievement during adolescence, were tested as potential mediators. Overall, participants with a childhood diagnosis of ADHD experienced more physical IPV than did comparisons (30.7% vs. 6.3%). In parallel, IPV was associated with higher levels of childhood ADHD symptomatology (d = .73). Young women with persistent ADHD stood the highest risk of experiencing IPV (37.3%), followed by those with transient ADHD (19.0%) and those never-diagnosed (5.9%). Academic achievement measured during adolescence was a significant partial mediator of the childhood ADHD symptomatology-young adult IPV relationship, even with control of sociodemographic, psychiatric, and cognitive factors, including childhood reading and math disorders. Findings indicate that in young women, childhood ADHD is a specific and important predictor of physically violent victimization in their intimate relationships. This vulnerable population requires IPV prevention and intervention, with academic empowerment as a key target.
Keywords: Attention-deficit/hyperactivity disorder (ADHD), intimate partner violence (IPV), victimization, females, longitudinal, academic achievement
Despite accumulating evidence implicating childhood attention-deficit/hyperactivity disorder (ADHD) in a host of long-term psychiatric, educational/vocational, and health-related difficulties (e.g., Barkley, Murphy, & Fisher, 2008; Biederman et al., 2010; Biederman, Petty, O’Connor, Hyder, & Faraone, 2012; Hinshaw et al., 2012), research examining the relationship functioning of adults, particularly women, with childhood histories of ADHD is extremely limited. Flory, Molina, Pelham, Gnagy, and Smith (2006) found that childhood ADHD independently predicted young adult (ages 18 to 26) risky sexual behavior, including earlier initiation of sexual activity and intercourse, more sexual partners, more casual sex, and more partner pregnancies; however, their sample was limited to men. In a related investigation, Babinski et al. (2011) found fewer romantic relationships in young adult women with childhood ADHD versus comparisons (M age = 20 years). Yet the quality of these relationships was not examined, and the sample size was relatively small.
During childhood and adolescence, ADHD in females has consistently been linked to interpersonal dysfunction and social impairments (Bagwell, Molina, Pelham, & Hoza, 2001; Greene et al., 2001; Hoza, 2007; Humphrey, Storch, & Geffken, 2007; Mikami & Lorenzi, 2011; Wiener & Mak, 2009). For instance, Blachman and Hinshaw (2002) found that school-aged girls with ADHD experienced higher levels of peer conflict and relational aggression than comparison girls (see also Zalecki & Hinshaw, 2004). Sciberras and colleagues (2012) found that adolescent girls with ADHD experienced more overt and relational bullying and peer victimization compared to those without ADHD. Peer relationship dysfunction in youth has been found to be primarily attributable to ADHD rather than to comorbidities, such as oppositional defiant disorder or anxiety disorders (Hoza et al., 2005). However, the extent to which these adverse relational experiences persist into young, or emerging (i.e., ages 18–25; Arnett, 2000) adulthood has not been sufficiently explored. Given that emerging adulthood is a developmental period during which romantic/intimate relationships take on major importance (Arnett, 2000, 2001; Erikson, 1968), exploration of whether young women with childhood-diagnosed ADHD are at risk, relative to their healthy peers, for experiencing victimization in their intimate relationships is clearly warranted.
Intimate partner violence (IPV) describes physical, sexual, or psychological/emotional abuse by a current or former partner or spouse (Centers for Disease Control and Prevention [CDC], 2014; Saltzman, Fanslow, McMahon, & Shelley, 1999). Although the term has been applied to both violence perpetration and victimization by an intimate partner, “IPV” in the present paper refers to victimization unless otherwise indicated. IPV against women is a major and costly public health problem (CDC, 2003). In addition to increasing the risk of injury and death, IPV is associated with a vast range of adverse mental and physical health outcomes, such as asthma, diabetes, chronic headaches and pain, suicidal behavior, and post-traumatic stress disorder (PTSD; Black et al., 2011; Max et al., 2004; CDC, 2014). Peak risk for IPV among women generally occurs during the period of emerging adulthood (Capaldi, Knoble, Shortt, & Kim, 2012). In addition, relative to healthy women, women with psychiatric illnesses—such as depression, anxiety, PTSD, and schizophrenia—are at increased risk of experiencing partner violence (Moffitt & Caspi, 1999; Trevillion, Oram, Feder, & Howard, 2012). Yet the extent to which childhood ADHD contributes to risk for IPV among young women has not yet been examined.
For a variety of reasons, young women with histories of ADHD might be vulnerable to experiencing IPV. First, they are more likely to have experienced violence and maltreatment in their family of origin (Briscoe-Smith & Hinshaw, 2006; Fuller-Thomson, Mehta, & Valeo, 2014; Guendelman, Owens, Galan, Gard, & Hinshaw, in press), which are well-documented risk factors for subsequent IPV (Tjaden & Thoennes, 2000; Whitfield, Anda, Dube, & Felitti, 2003). Second, other shared risk factors for women with childhood ADHD and women exposed to IPV include coming from a single-parent household (Hjern, Weitoft, & Lindblad, 2009; Moffitt & Caspi, 1999), experiencing chaotic and conflictual family relations (CDC, 2014; Moffitt & Caspi, 1999), and having lower educational achievement and greater rates of school dropout (Loe & Feldman, 2007). Indeed, academic underachievement is associated with problematic behaviors, including aggression, delinquency and association with deviant peer groups, and substance abuse, that may confer increased IPV risk (Frick et al., 1991; Hinshaw, 1992; Magdol et al., 1997).
In addition, women with childhood ADHD are at high risk for developing comorbidities, such as externalizing problems (e.g., conduct disorder, oppositional defiant disorder; Hinshaw et al., 2012) and internalizing problems (e.g., depression, anxiety, and low self-esteem; Babinski et al., 2011; Hinshaw et al., 2012; Magdol et al., 1997), which may function as ‘stepping stones’ for subsequent IPV risk. In a longitudinal, representative birth cohort study, Moffit and Caspi (1999) found that for females, the strongest predictor of physical victimization by an intimate partner was the females’ own aggressive delinquency (e.g., hit a parent, fought in public, used a weapon in a fight). Depression during adolescence is associated with a wide range of functional impairments that might contribute to IPV vulnerability, including diminished self-esteem, interpersonal difficulties, subsequent substance abuse, and decreased likelihood of on-time marriage (e.g., Keenan-Miller, Hammen & Brennan, 2007; Lehrer, Buka, Gortmaker, & Shrier, 2006; Kessler, Walters, & Forthofer, 1998). In a meta-analysis of risk factors for IPV, female physical violence victimization was most strongly predicted by the victim’s use of violence toward her partner, followed by her depression (Stith, Smith, Penn, Ward, & Tritt, 2004). In sum, adolescent internalizing and externalizing behaviors, along with academic underachievement, may represent potential pathways between childhood ADHD and subsequent physical IPV.
A small body of research examining linkages between ADHD and IPV has focused exclusively on perpetration of IPV, particularly by men (Fang, Massetti, Ouyang, Grosse, & Mercy, 2010; Wymbs et al., 2012). Among a sample of young men ages 18 to 25 years, Wymbs et al. (2012) found that ADHD diagnostic status in childhood (but not symptom severity) was associated with increased risk for violence toward romantic partners. Fang and colleagues (2010) found that retrospectively reported childhood symptoms of hyperactivity/impulsivity (HI) and inattention predicted IPV perpetration in a mixed-sex population-based sample (see also Theriault & Holmberg, 2001). Still, the extent to which women with childhood ADHD are at risk for being victimized by an intimate partner by young adulthood has not yet been examined.
In the present study, we draw from a longitudinal sample of girls followed prospectively into young adulthood, comparing those with and without childhood ADHD in terms of their risk for physical IPV by 17–24 years of age. Physical violence is considered the most consistently defined and concretely measured form of IPV in extant research (Jewkes, 2002). We hypothesize that having a childhood diagnosis of ADHD will predict greater physical victimization by an intimate partner. In parallel, we predict that physical IPV-exposed participants will have had significantly greater childhood ADHD symptomatology (e.g., severity). In addition, we examine whether victimization risk is linked to ADHD diagnostic persistence from childhood to young adulthood. We hypothesize that the participants with a persistent diagnosis of ADHD (i.e., during both childhood and young adulthood) will be at greatest risk for physical IPV, followed by those with a transient ADHD diagnosis, and that participants without any history of an ADHD diagnosis will be at lowest risk. Furthermore, the prospective, longitudinal study design allows a preliminary examination of a subset of plausible candidate mediators between ADHD symptomatology in childhood and risk for physical IPV in early adulthood. We focus on three potential mediation domains, measured in adolescence: (1) externalizing behavior; (2) internalizing behavior; and (3) academic achievement.
Because of the limited availability of data regarding participants’ perpetration of physical IPV, we restrict analyses of perpetration status to (a) descriptive statistics and (b) a contrast between ADHD and comparison groups in terms of overall rates of perpetration, as well as bidirectional perpetration and victimization.
Method
Overview of Procedures
Data are drawn from the Berkeley Girls with ADHD Longitudinal Study (BGALS), which has been previously described (e.g., Hinshaw, 2002; Hinshaw, Owens, Sami, & Fargeon, 2006; Hinshaw et al., 2012). In 1997, 1998, and 1999, girls 6–12 years of age were recruited from schools, mental health centers, pediatric practices, and through direct advertisements to participate in research summer camps. The objective was to collect ecologically valid participant data rather than to provide therapeutic intervention. Overall exclusionary criteria included intellectual disability, pervasive developmental disorders, psychosis or overt neurological disorder, English not spoken in the home, and medical problems impeding summer camp participation. Common comorbidities (oppositional defiant disorder [ODD], conduct disorder [CD], anxiety disorders, depression, learning disorders) were allowed.
Following an extensive diagnostic screening process, 140 girls with ADHD (93 combined-type and 47 inattentive-type) and 88 age- and ethnicity-matched comparison girls were enrolled (Hinshaw, 2002). ADHD and comparison participants were mixed and grouped by age in the camps, during which multi-source, multi-informant baseline (Wave 1) data were collected regarding the girls’ demographic characteristics and psychological, social, and behavioral functioning. The participants were invited to partake in follow-up assessments approximately five (Wave 2; Hinshaw et al., 2006) and ten years (Wave 3; Hinshaw et al., 2012) following the summer camps. Follow-up assessments were conducted by trained post-baccalaureate and graduate students in clinical psychology at the University of California, Berkeley campus, or at the participants’ homes if they were unable to travel.
Participants
The Wave 1 sample (N = 228; M age = 9.6 years) was ethnically diverse, with 53% Caucasian, 27% African American, 11% Latina, and 9% Asian American. Mean annual gross household income ranged from $50,000–60,000. Approximately 14% of the participants’ households received some form of public assistance. Mean educational attainment level of participants’ mothers was ‘some college,’ with the majority (57%) of mothers holding a bachelor’s degree or higher. These levels of income and maternal education are reflective of the overall socioeconomic characteristics of the San Francisco Bay Area. Of the 228 participants at Wave 1, 210 (92%; M age = 14.2 years, range = 11 to 18 years) were assessed at the Wave 2 follow-up (Hinshaw et al., 2006); 216 (95%; M age = 19.6 years, range = 17 to 24) were assessed at the Wave 3 follow-up (Hinshaw et al., 2012).
Present study subsample
The present study included 193 (114 with ADHD, 79 comparison) participants with data on physical IPV exposure at Wave 3. Of the 35 (nine comparison, 26 ADHD) participants from the original sample who were not included in the present study, 12 were lost to attrition, 16 lacked data regarding physical IPV exposure at Wave 3, and seven (four ADHD, three comparison) reported that they had never dated or been in a romantic relationship and thus were excluded from the analyses. To evaluate the representativeness of the retained sample, we contrasted the 35 participants excluded from the present study versus those retained with respect to 15 key Wave 1 measures. The non-retained and retained groups did not differ with respect to age, maternal level of education, academic achievement (math and reading), maternal depression, adopted/foster status, family’s welfare status, low birth weight status (< 5 lbs., 8 oz.), ADHD symptom scores at baseline (composite teacher and parent), baseline DISC-IV ODD or CD diagnosis, baseline DISC-IV depression or anxiety disorder diagnosis, or childhood maltreatment status. The non-retained group, however, had lower household income at baseline, t(223) = −2.24, p = .03, d = .41 and lower WISC full scale IQ score, t(224) = −2.15, p = .03, d = .40. The non-retained group was also more likely to be of non-Caucasian ethnicity, 55% vs. 37%, χ2(1, N = 228) = 3.98, OR = 2.11, 95% CI [1.00, 4.42], p = .04.
Measures
Criterion variable: Physical IPV
Physical victimization status was determined via chart review of key project-derived measures administered at Waves 2 and 3. First, the Health and Sexual Behavior Questionnaire (HSBQ; Wave 3) is a self-reported measure that includes a single question related to physical IPV: “In any chosen sexual relationship you’ve had, has there been physical violence (pushing, punching, slapping)?” Participants responded either yes or no; if yes, they specified who caused the violence: (1) participant only; (2) partner only, or (3) both the participant and partner. Coders were instructed to code endorsements of (2) and (3) as positive for victimization. Coders were also instructed to code endorsements of (1) and (3) as positive for perpetration of physical IPV toward a partner (this comprised the key variable used in the brief analyses of perpetration in the sample). Second, the Hot Sheet is an interviewer/clinician post-interview summary of any violence, particularly that which posed a threat to the personal safety of the participant, that participants may have reported. In Waves 1 and 2, the Hot Sheet was utilized by clinicians to document instances of child abuse (e.g., Briscoe-Smith & Hinshaw, 2006; Guendelman et al., in press). Third, the 10-Year Family Information Packet (FIP; Wave 3) is a parent- and participant-reported, comprehensive, year-by-year information sheet regarding significant life events, including participants’ relationship status, between Waves 2 and 3. Because the HSBQ asks specifically about physical IPV in the context of sexual relationships and not intimate relationships more broadly, the FIP and Hot Sheets were used as supplementary sources of victimization data to capture participants who may have experienced physical IPV in a romantic (but not strictly sexual) relational context and to obtain data on the victimization status of participants with missing data on the HSBQ.
Three of the study authors, along with four undergraduate coders blinded to the study hypotheses, reviewed and coded all charts for presence versus absence of physical IPV. All coders relied broadly on the definition of physical IPV victimization used by the CDC, namely, being the target of “intentional…physical force with the potential for causing death, disability, or harm,” caused by a current or former spouse, dating partner, or boyfriend/girlfriend (heterosexual or same sex; Saltzman et al., 1999). The undergraduate coders were instructed to use the codes 1 and 0 for presence or absence of physical IPV for each participant. Three authors coded all charts and resolved disagreements amongst themselves through consensus discussion; their consensus code served as the ‘gold standard’ against which the undergraduate codes were compared. The mean kappa for presence of any physical IPV by Wave 3 was .93, indicating high agreement (Bakeman & Gottman, 1997; Fleiss, 1981). Coding disagreements were resolved by assigning the majority code. A dichotomously coded physical victimization variable (ever/never victimized) served as the key dependent variable for the study.
Predictor variable: Childhood ADHD
We measured ADHD both diagnostically and dimensionally, because of (a) the clinical importance of considering ADHD diagnostic status (and because participants were selected largely on the basis of a diagnostic interview) and (b) the greater statistical power afforded by dimensional scores. Indeed, supplementing analyses of categorical ADHD diagnoses with dimensional symptom scores is consistent with the Research Domain Criteria (RDoC) perspective (National Institute of Mental Health, 2014).
ADHD diagnostic status and symptomatology
ADHD diagnostic status, categorized as present or absent (i.e., comparison participant), was derived from the Diagnostic Interview Schedule for Children (4th ed.; Shaffer et al., 2000) and the Swanson, Nolan, and Pelham Rating Scale (4th ed.; SNAP-IV; Swanson, 1992). See Hinshaw (2002) for details regarding diagnostic procedures. The DISC-IV, which also yielded diagnostic subtype (e.g., ADHD-Combined vs. ADHD-Inattentive), is a well-validated, highly structured diagnostic interview administered to parents at Wave 1; a parallel version was administered to participants and parents at Wave 3 (Young Adult version, DISC-IV-YA; Shaffer et al., 2000).
The SNAP-IV is a dimensionalized checklist that assesses core ADHD symptoms of inattention and hyperactivity/impulsivity, along with symptoms of ODD, each rated 0 (not at all) to 3 (very much), was administered at Wave 1. ADHD total symptom score was derived from a composite of the averaged mother-rated ADHD items and the averaged teacher-rated ADHD items.
Predictor variable: Persistence or Remission of ADHD Diagnosis
Following the procedures of Swanson, Owens, & Hinshaw (2014), we created a dummy variable to reflect the persistence or transience of ADHD diagnosis from Wave 1 to Wave 3. Wave 1 diagnosis was established via the procedures described above; at Wave 3, we used both parent and youth report from the DISC-IV to establish the presence of ADHD via the ‘or’ criterion, symptom by symptom (Piacentini, Cohen, & Cohen, 1992). Young women who did not meet the ADHD criteria at both Wave 1 and Wave 3 were coded as 0; those who met ADHD criteria at Wave 1 or Wave 3 were coded as 1 (transient ADHD); and those who met ADHD criteria at Wave 1 and Wave 3 were coded as 2 (persistent ADHD).
Wave 2 hypothesized mediators
Measures within each mediation domain were administered at the Wave 2 (adolescent) follow-up.
Externalizing behavior
Participants’ primary caregivers completed the Child Behavior Checklist (CBCL; Achenbach, 1991), an extensively used, psychometrically sound questionnaire that assesses behavioral and emotional problems of children and adolescents. We utilized the externalizing broadband scale, which yields a continuous score tapping behaviors such as aggression and noncompliance. In addition, we utilized the DISC-IV Oppositional Defiant Disorder symptom count. The variables (r = .71) were standardized and averaged to create an Externalizing composite variable. The internal consistency of the items comprising the CBCL externalizing scale and the DISC ODD symptom count was very high (α = .90). The mean of this composite was .01, with a standard deviation of .93 and range of −1.29 to 2.53.
Internalizing behavior
An internalizing composite variable was derived from the internalizing broadband scale of the mother-reported CBCL (Achenbach, 1991) and the total score from the Children’s Depression Inventory (CDI; Kovacs, 1992). The CDI is a widely used self-report instrument tapping symptoms of depression in youth; internal consistency ranges from .71–.87 and test-retest reliability figures average .7 (Kovacs, 1992). The internalizing CBCL and CDI total scores (r = .36) were standardized and averaged to create an Internalizing composite variable. The internal consistency of the items across the CBCL internalizing scale and the CDI was very high (α = .95). The mean of this composite was .02, with a standard deviation of .85 and a range of −1.40 to 3.03.
Academic Achievement
We administered the Basic Reading and Math Reasoning subtests of the Wechsler Individual Achievement Test, Second Edition (WIAT-II; Wechsler, 2001), a widely used standardized test of academic achievement; participants were tested while unmedicated (Hinshaw et al., 2006). Established test-retest reliabilities for the Reading and Math scores on the WIAT-II range from .93 to .95 (Wechsler, 2001). Given the correlation of r = .66 between these subtest scores, we summed them to create an Academic Achievement composite variable. The mean of this composite was 203.6, the standard deviation was 27.1, and the range was 126 to 255.
Covariates. Covariates were selected based on previous research showing associations with IPV risk (CDC, 2014; Moffitt & Caspi, 1999; Whitfield et al., 2003). The Background Information Questionnaire, devised for the BGALS study and administered to parents at Wave 1, yielded demographic information including the participants’ date of birth, used to calculate participant age, and four additional covariates including socioeconomic status (SES), a composite of mother’s highest level of education and yearly household income; race/ethnicity, including Caucasian, African-American, Latina, Asian American, or Native American; adopted/foster status (dichotomized as either being raised by foster/adoptive parents or by a biological family member); and single parent status (raised in single vs. two-parent household). Two additional covariates were derived from the DISC-IV: presence or absence of an anxiety disorder or depression/dysthymic disorder (Anx/Dep), and presence or absence of ODD or CD (ODD/CD), each at Wave 1. Full scale IQ (FSIQ) was obtained from the Wechsler Intelligence Scale for Children (3rd ed.; Wechsler, 1991), administered at Wave 1. Childhood maltreatment status (maltreatment) was coded for presence or absence of any exposure to physical, sexual, or verbal/psychological maltreatment by Wave 1 (for details regarding the coding of this variable, see Guendelman et al., in press). Hence, nine sociodemographic, cognitive, and psychiatric covariates were considered: (1) age; (2) SES; (3) race/ethnicity; (4) adopted/foster status; (5) single parent status (6) Anx/Dep; (7) ODD/CD; (8) FSIQ; and (9) maltreatment. Two additional covariates, reading disorder and math disorder, considered present when standard scores were below 85 on the Basic Reading and Math Reasoning subtests, respectively, of the Wave-1 administered Wechsler Individual Achievement Test (WIAT; Hinshaw, 2002; Wechsler, 1992), were included for academic achievement mediation analyses only.
Data analytic plan
Statistical analyses were performed with SPSS for Mac, Version 20 (IBM Corp., 2011).
First, we conducted a chi-square test to assess group differences in Wave 1 diagnostic status (presence or absence of ADHD) regarding Wave 3 victimization status (presence or absence of physical IPV). In parallel, we performed a t-test to determine whether Wave 3 victimization status (presence or absence of physical IPV) was associated with Wave 1 ADHD symptomatology (e.g., severity). Effect sizes were calculated using odds ratios (95% confidence interval) or Cohen’s d values, respectively. We then performed a binary logistic regression and ANCOVA to address the potential effects of the nine covariates.
Second, we conducted a chi-square test and parallel logistic regression to assess group differences among young women with a persistent ADHD diagnosis (P), young women with a transient ADHD diagnosis (T), and a lifetime non-diagnosed comparison group (C; see Swanson et al., 2014).
Third, we tested mediation effects via a bootstrap procedure (Efron & Tibshirani, 1993) utilizing procedures developed by Hayes (2013) for SPSS (see Swanson et al., 2014, for parallel examples with respect to different mediator and criterion measures). We investigated the effects of single mediators, with respect to the Wave 1 ADHD symptomatology-Wave 3 physical IPV criterion association (Preacher & Hayes, 2008; Shrout & Bolger, 2002). Candidate mediators, analyzed separately, were Wave 2 measures of (1) externalizing behavior, (2) internalizing behavior, and (3) academic achievement. The bootstrapping procedure is a statistical simulation that is used to generate an empirically derived representation of the sampling distribution of the indirect effect (Hayes, 2013). After sampling those cases with replacement, a point estimate of the indirect effect (a-prime × b-prime) is determined for the sample and repeated 10,000 times. We formed 95% bias-corrected and accelerated confidence intervals based upon the distribution of these effects and inferred statistical significance, if this interval did not contain 0 (see Preacher & Hayes, 2008; Shrout & Bolger, 2002). All mediation models were tested controlling for sociodemographic, cognitive, and psychiatric covariates. For the criterion variable of academic achievement, we additionally controlled for reading disorder and math disorder. Regression analyses ensured that the predictor-mediator and mediator-outcome pathways were significant and in the hypothesized directions.
Fourth, we conducted a parallel chi-square test (to assess group differences in Wave 1 ADHD diagnostic status regarding Wave 3 physical IPV perpetration status) and t-test (to determine whether Wave 3 perpetration status was associated with Wave 1 ADHD symptomatology). Effect sizes were calculated using odds ratios (95% confidence interval) or Cohen’s d values, respectively. We then performed a binary logistic regression and ANCOVA to address the potential effects of the eight covariates.
Results
Baseline (Wave 1) Sample Characteristics
Participants in the ADHD and comparison groups did not differ significantly at baseline (Wave 1) with respect to age, racial/ethnic status, household income or use of public assistance, maternal level of education and depressive symptoms, single parent status, low birth weight, or childhood maltreatment status1 (Table 1). Relative to comparisons, participants with ADHD had significantly higher SNAP-IV scores, lower full-scale IQ scores, and lower math and reading achievement scores. They were also more likely to have been adopted or placed in foster care, to have a DISC-IV diagnosis of depression or an anxiety disorder, and have a DISC-IV diagnosis of ODD or CD.
Table 1.
Wave 1 Characteristics of Overall Sample plus Comparisons between ADHD and Comparison Groups
| Variable | Overall Sample N = 193 M (SD) |
ADHD Group n = 114 M (SD) |
Comparison Group n = 79 M (SD) |
pa |
|---|---|---|---|---|
|
|
|
|||
| Demographic | ||||
| Age (years) | 9.5 (1.7) | 9.7 (1.7) | 9.4 (1.7) | ns |
| Total annual family incomeb | 6.6 (2.6) | 6.4 (2.7) | 6.9 (2.4) | ns |
| Maternal educationc | 4.8 (0.9) | 4.7 (0.9) | 4.9 (0.9) | ns |
| Caucasian (%) | 55.4 | 59.6 | 49.4 | ns |
| Public Assistance (%) | 13.5 | 14.9 | 11.4 | ns |
| Adopted or in foster care (%) | 14.5 | 21.1 | 5.1 | .001* |
| Single-parent household | 27.5 | 31.6 | 21.5 | .08 |
| Maltreated (%) | 14.0 | 16.7 | 10.1 | ns |
| Prenatal and Cognitive | ||||
| Low birth weight (<2500g) (%) | 8.3 | 10.0 | 8.0 | ns |
| WISC-III Full Scale IQ | 105.3 (14.1) | 100.5 (13.4) | 112.1 (12.1) | <.001* |
| Reading Disorderd (%) | 9.3 | 13.4 | 3.8 | .02* |
| Math Disordere (%) | 11.9 | 16.1 | 6.3 | .03* |
| ADHD-Related | ||||
| SNAP-IV Total Symptom Scoref (0–3) | 1.18 (0.86) | 1.81 (0.48) | 0.27 (0.20) | <.001* |
| Comorbidities | ||||
| DISC-IV ODD/CDg (%) | 42.0 | 65.8 | 7.6 | <.001* |
| DISC-IV Anxiety/Depressionh (%) | 14.0 | 24.6 | 2.5 | <.001* |
Note. WISC-III = Wechsler Intelligence Scale for Children-III; WIAT = Wechsler Individual Achievement Test; SNAP-IV = Swanson, Nolan, and Pelham rating scale (see Swanson, 1992); HI = Hyperactivity/Impulsivity; DISC-IV = Diagnostic Interview Schedule for Children, 4th edition; ns = not significant.
Significant at p < .05.
ADHD Group vs. Comparison Group. Significance: t-test for continuous variables; Pearson chi-square statistic for categorical variables.
For total annual family income, 1 ≤ $10,000; 9 ≥ $75,000.
For maternal education, 1 = less than 8th grade; 6 = advanced or professional degree.
Reading Disorder defined as standard score <85 on Basic Reading subtest of Wave 1-administered WIAT.
Math Disorder defined as standard score <85 on Math Reasoning subtest of Wave 1-administered WIAT.
SNAP-IV Total Symptom Score defined as composite of the averaged mother-rated ADHD items and the averaged teacher-rated ADHD items
Diagnosis of Oppositional Defiant Disorder and/or Conduct Disorder.
Diagnosis of Anxiety Disorder and/or Major Depressive Episode and/or Dysthymia.
Wave 3 Physical IPV Victimization
Unadjusted analyses
Forty participants (20.7%) were positive for IPV by the Wave 3 assessment. Relative to comparisons, participants with ADHD were more likely to have been victimized, 30.7% vs. 6.3%, χ2(1, N = 193) = 16.87, OR = 6.56, 95% CI [2.44, 17.63], p < .001.2 In parallel, relative to participants not exposed to IPV, IPV-exposed participants had significantly greater Wave 1 ADHD symptomatology, M = 1.68 (SD = 0.72) vs. M = 1.05 (SD = 0.84), t(191) = 7.30, p < .001, d = 0.73).
Covariate-adjusted analyses
Logistic regression and ANCOVA analyses revealed that Wave 1 ADHD diagnostic status and SNAP-IV symptomatology each remained significantly associated with Wave 3 victimization status, p = .01 and p = .03, respectively, when covarying sociodemographic, cognitive, and psychiatric covariates.
Prediction of Wave 3 IPV (Victimization) from Diagnostic Persistence of ADHD Over Time
Table 2 presents differences in young women’s IPV status across the persistent ADHD, transient ADHD, and lifetime non-diagnosed comparison groups. Results indicated a step-wise relation, whereby young women with persistent ADHD had significantly greater IPV exposure (37.3%) relative to the transient ADHD group3 (OR = 2.54), who in turn had significantly greater IPV exposure (19.0%) relative to the lifetime comparison group (5.9%; OR = 3.74). The odds ratio for the persistent ADHD versus the lifetime comparison group was 9.52. These findings withstood adjustment of sociodemographic, cognitive, and psychiatric covariates.
Table 2.
Wave 3 Victimization Risk by ADHD Diagnostic Persistence
| Comparison n = 68 |
Transient ADHD n = 58 |
Persistent ADHD n = 67 |
ESb and Post Hoc | |||||
|---|---|---|---|---|---|---|---|---|
| W3 IPV Status | % | % | % | p-valuea | C-T | C-P | T-P | p-valuec |
|
|
|
|
|
|
|
|||
| Victimized | 5.9 | 19.0 | 37.3 | <.001 | 3.74* | 9.52* | 2.54* | <.05 |
Note. ADHD = Attention-Deficit/Hyperactivity Disorder; Victimized = physically victimized by an intimate partner; C = lifetime non-diagnosed comparison group; T = transient ADHD (includes 47 with ADHD at Wave 1 only and 11 with ADHD at Wave 3 only); P = persistent ADHD.
Significant at p < .05.
Significance: chi-squared.
Odds ratios, reflecting subgroup contrasts.
Significance: logistic regression.
Mediational Analyses
Bootstrap analyses were used to test the association between Wave 1 SNAP-IV symptomatology and Wave 3 IPV status with respect to candidate mediators measured at Wave 2, with inclusion of the covariates listed in the Data Analytic Plan.
Externalizing
The Wave 2 externalizing composite variable was not a significant mediator of the relation between Wave 1 SNAP-IV severity and Wave 3 IPV status, IE = .28, SE = .21, 95% CI [−0.12, 0.69]. There was a significant and positive relation between Wave 1 SNAP-IV severity and Wave 2 externalizing, b = .59, standard error [SE] = .09, t(178) = −6.83, p < .001, R2 = .46. However, the relation between Wave 2 externalizing and Wave 3 IPV status was not significant, b = .48, standard error [SE] = .29, z = 1.66, p = .10. When we omitted the associated baseline covariate, ODD/CD, to avoid overcontrol, the model remained non-significant, IE = .32, SE = .23, 95% CI [−0.17, 0.76].
Internalizing
The Wave 2 internalizing composite variable was not a significant mediator of the relation between Wave 1 SNAP-IV severity and Wave 3 IPV status, IE = −.04, SE = .08, 95% CI [−0.25, 0.09]. There was a significant and positive relation between Wave 1 SNAP-IV severity and Wave 2 internalizing, b = .21, standard error [SE] = .10, t(178) = 2.21, p < .05, R2 = .21. However, the relation between Wave 2 internalizing and Wave 3 IPV status was not significant, b = −.20, standard error [SE] = .30, z = −.66, p = .51. When we omitted the associated baseline covariate, Anx/Dep, to avoid overcontrol, the model remained non-significant, IE = −.02, SE = .08, 95% CI [−0.20, 0.11].
Academic Achievement
The Wave 2 academic achievement composite variable was a significant partial mediator of the relation between Wave 1 SNAP-IV severity and Wave 3 IPV status, IE = .23, SE = .16, 95% CI [0.01, 0.61]. There was a significant and negative relation between Wave 1 SNAP-IV severity and Wave 2 academic achievement, b = −7.18, standard error [SE] = 1.99, t(174) = −3.61, p < .001, R2 = .67. A similar pattern emerged for the relation between Wave 2 academic achievement and Wave 3 IPV status, b = −.03, standard error [SE] = .01, z = −2.27, p < .05. See Figure 1.
Fig. 1.
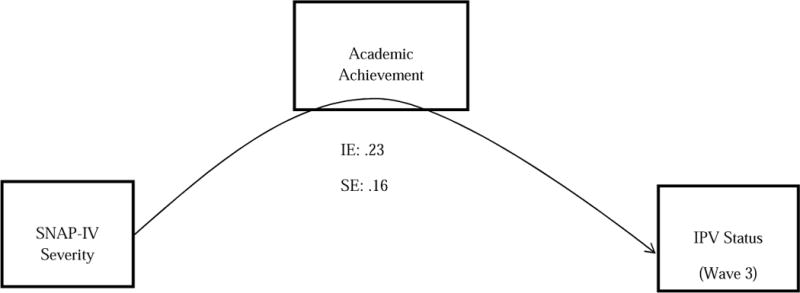
The relation between Wave 1 ADHD and Wave 3 Intimate Partner Violence (IPV) physical victimization status (presence vs. absence) was partially mediated by Academic Achievement, controlling for: (1) age; (2) SES; (3) race/ethnicity; (4) adopted/foster status; (5) single parent status; (6) Anx/Dep; (7) ODD/CD; (8) FSIQ; (9) maltreatment, (10) reading disorder, and (11) math disorder; data represent indirect effect and standard errors using 10,000 bootstrap samples to obtain bias-corrected and accelerated 95% confidence intervals.
Wave 3 IPV Perpetration and Bidirectional Physical IPV
Perpetration data were available for 78.8% (n = 152; 92 ADHD, 60 comparison) of the sample. Overall, 16 of these participants had perpetrated IPV by Wave 3 (14.1% of ADHD group vs. 5.0% of comparison group, χ2(1, N = 152) = 3.21, OR = 3.13, 95% CI [0.85, 11.48], p = .07). In addition, compared to non-perpetrators, dimensional analyses revealed that participants who had perpetrated IPV had significantly higher SNAP-IV scores, M = 1.69 (SD = 0.88) vs. M = 1.15 (SD = 0.84), t(150) = −2.44, p = .02, d = 0.46. ANCOVA analysis revealed that after controlling for sociodemographic, cognitive, and psychiatric covariates, SNAP-IV symptomatology was no longer significantly associated with Wave 3 perpetration status.
Of the 16 participants with any perpetration, 12 (11 ADHD, 1 comparison) had bidirectional physical IPV (i.e., status as both a victim and perpetrator) whereas 4 (2 ADHD, 2 comparison) had perpetration only (i.e., without victimization).
Discussion
First, whether measured diagnostically (i.e., dichotomously) or dimensionally (i.e., continuously), ADHD in childhood predicted increased risk for physical IPV victimization by young adulthood. Indeed, approximately 30% of young women with childhood ADHD had experienced physical IPV victimization compared to only 6% in the comparison group. Furthermore, dimensional analyses revealed that greater ADHD symptom severity in childhood was associated with increased risk for physical IPV victimization, with an effect size approaching large (d = .73). These associations remained significant when controlling for multiple covariates, suggesting that the core characteristics of childhood ADHD predict risk for victimization independently of other sociodemographic, cognitive, and psychiatric factors (e.g., poverty, maltreatment, depression, conduct problems). In short, for females, childhood ADHD is specifically associated with a substantially increased risk for being physically abused by a romantic partner by young adulthood.
We also found a significant step-wise relation between ADHD diagnostic persistence and physical IPV victimization risk. Participants with a persistent diagnosis of ADHD were twice as likely to experience IPV relative to those with transient diagnoses, and nine times more likely to experience IPV than those without any history of an ADHD diagnosis. Thus, when ADHD diagnostically remits, the longitudinal association lessens. These findings add ADHD to the set of mental disorders (e.g., anxiety, mood, and substance use disorders, PTSD) previously shown to be associated with women’s risk for being abused by their partners (e.g., Moffitt & Caspi, 1999; Rees et al., 2011). In addition, they also extend existing research by showing that, far from being a time-limited, male-dominated disorder, childhood ADHD has disadvantageous long-term implications for women’s young adult relationships.
Second, adolescent academic achievement (i.e., WIAT-II Basic Reading plus Math Reasoning scores) was a significant partial mediator of the relation between childhood ADHD symptomatology and young adulthood physical IPV victimization. Given our control of Wave 1 reading and math disorders, assessed using the same instrument used to measure Wave 2 academic achievement, we can argue that achievement during adolescence – not childhood –was the key agent in the causal pathway. Previous research has shown that lower educational attainment (e.g., younger age at leaving secondary school in Moffitt & Caspi, 1999; less than high-school diploma in Thompson et al., 2006) is associated with victimization in women. Educational attainment is strongly and negatively correlated with income (Sirin, 2005); poorer women tend to be at greater risk for IPV (Jewkes, 2002; Vest, Catlin, Chen, & Brownson, 2002). Additionally, lower educational performance is associated with having partners who are unemployed (Kyriacou et al., 1999) and with single parenthood (Thompson et al., 2006), both of which have been linked to higher IPV risk. Overall, higher levels of female empowerment – for instance, in the form of strong academic achievement, which tends to confer social empowerment via social networks, self-confidence, and social enfranchisement – have generally been found to be protective against IPV (Jewkes, 2002). Notably, we found partial mediation for academic achievement even when controlling for key covariates including baseline IQ, family SES, and reading and math disorders. Thus, low academic achievement during adolescence may function as a sieve of sorts, constituting a pathway that partially differentiates between females who subsequently become romantically involved with violence-prone partners and those who do not.
Contrary to our hypotheses, adolescent externalizing behavior was not a significant mediator of the ADHD symptomatology-physical IPV victimization linkage. This null finding was unexpected given the large literature implicating youth aggressive and delinquent behavior in both victimization (e.g., in the Dunedin Multi-disciplinary Health and Development Study; Magdol et al., 1997; Moffitt & Caspi, 1999) and perpetration of IPV in general samples (e.g., Ehrensaft et al., 2003; Fang et al., 2010) and samples of males with ADHD (Wymbs et al., 2012) — along with evidence pointing to high rates of externalizing problems in females with ADHD (e.g., Hinshaw, 2002; Hinshaw et al., 2006; Hinshaw et al., 2012). Findings from the Dunedin study revealed substantial assortative mating for antisocial behaviors (Krueger, Moffitt, Caspi, Bleske, & Silva, 1998), suggesting that a girl’s history of externalizing and delinquent behavior increases the likelihood that she will become involved with a partner for whom aggression and violence is both acceptable and common (Ehrensaft et al., 2003). Intriguingly, in exploratory analyses we found that externalizing behavior did partially mediate the ADHD-IPV linkage when only a subset of covariates were included in the model (i.e., participant age, SES, race/ethnicity, single parent household, FSIQ). Yet when the other covariates (i.e., adopted/foster, maltreatment, Anx/Dep, CD/ODD) were included, the finding no longer attained significance. Externalizing behavior is embedded in a web of early-life and comorbidity-related features, which together explain some of the risk for partner violence.
Also in contrast to our hypotheses, adolescent internalizing behavior did not mediate the association between ADHD symptomatology and physical IPV victimization status. Depressive symptomatology has been found in population-based samples to be associated with increased risk of subsequent physical IPV (Lehrer et al., 2006). However, internalizing behavior during adolescence was quite common across our entire sample, and our measure of this construct may not have been sufficiently sensitive to distinguish between those who did versus did not subsequently become vulnerable to IPV.
Our findings were in line with prior research showing a positive association between ADHD and IPV perpetration (e.g., Fang et al., 2010; Wymbs et al., 2012). Indeed, although perpetration data were available for only a subset of the sample, participants with histories of perpetration had higher baseline ADHD symptoms, and were marginally more likely to have been diagnosed with ADHD in childhood.
Results should be interpreted in light of several study limitations, which can be considered as a springboard for future research. First, although physical IPV victimization data were available for a large proportion (87.3%) of the original BGALS sample, a subset was excluded from present analyses due to attrition, missing data, or lack of prior romantic relationship or dating experience. The excluded participants were more likely to be of minority ethnicity, and to have lower household income and IQ scores, compared to retained participants.
Second, we determined physical IPV victimization status via a single self-report question plus chart review (i.e., rather than a standardized IPV instrument), which may have led to unreliability of measurement as well as false negatives (i.e., an underestimate of the actual IPV frequency). The single question probing physical violence did so in the context of a narrowly sexual, rather than more broadly intimate, relationship. Also, it is plausible that participants may not have felt comfortable disclosing their IPV history, out of a desire (for instance) to protect their partner, because of recall bias, or related to trauma-related psychological processes such as dissociation. Nonetheless, the chart review comprised multi-informant data, which provided some degree of protection against false negatives.
Third, we were not able to reliably code certain dimensions of IPV, such as its exact timing, severity, frequency, or the context in which it occurred (e.g., whether it was reciprocal, or provoked, or used in self-defense). Indeed, mounting evidence suggests that IPV is often co-instigated and perpetrated mutually (Whitaker, Haileyesus, Swahn, & Saltzman, 2007). Individuals with ADHD demonstrate not only the core characteristics of the disorder but also marked social skills deficits (e.g., Bagwell et al., 2001). These could undermine individuals’ ability to effectively negotiate conflict, increase the likelihood they would unwittingly provoke their partners, and plausibly make them vulnerable to attracting partners with similarly poor or aggressive problem-solving strategies. In short, future studies should examine the bidirectional nature of IPV in the partnerships of women with ADHD.
In addition, we focused solely on physical violence and were not able to reliably examine other types of IPV such as sexual, verbal, and psychological victimization. We were also unable to reliably assess adolescent peer victimization/bullying, a conceptually plausible pathway to physical IPV in females with ADHD. Indeed, within a developmental victimology framework (Finkelhor, 2007), prior victimization (e.g., by peers) functions as a ‘gateway’ for subsequent victimization of other kinds, including IPV (see Connolly, Pepler, Craig, & Taradesh, 2000; Espelage & Holt, 2007; but see Chiodo et al., 2012). We were unable, as well, to examine the role of participants’ exposure to parental battering, a well-documented risk factor for subsequent IPV (Bensley, Van Eenwyk, & Wynkoop Simmons, 2003; Ehrensaft et al., 2003). It is also possible that in a small number of cases, assessments of the mediator variables did not temporally precede the IPV. In general, additional research is needed to investigate whether aspects of interpersonal violence during adolescence (e.g., maltreatment, peer victimization/bullying, harsh parenting and family conflict) mediate the ADHD-IPV relation.
Nonetheless, this study has several important strengths. First, it is among the first to prospectively examine young adult romantic relationship outcomes in women with childhood-diagnosed ADHD. It also utilized a rigorously diagnosed, well-characterized and well-retained, ethnically and socioeconomically diverse sample. Findings extend previous research by showing that the increased levels of interpersonal dysfunction and victimization among children and adolescents with ADHD (e.g., Blachman & Hinshaw, 2002; Sciberras et al., 2012; Zalecki & Hinshaw, 2004) persist in the form of physical violence in intimate relationships by early adulthood. In addition, to our knowledge, findings comprise the first evidence regarding physical IPV victimization in women with childhood ADHD, as previous studies examining the IPV-ADHD linkage have focused strictly on IPV perpetration, mostly in males (Fang et al., 2010; Theriault & Holmberg, 2001; Wymbs et al., 2012). Furthermore, results from the diagnostic persistence analyses as well as the inclusion of comprehensive covariate control in all analyses provide novel evidence that childhood ADHD specifically, rather than confounding variables, is an important predictor of subsequent physical IPV victimization risk. Finally, mediational analyses suggest one developmental pathway for the longitudinal association, namely, through academic achievement in adolescence. However, future studies, especially those utilizing path analyses, are needed to further probe the complex pathways linking early ADHD and IPV risk and to examine whether the associations are similar in comparable samples of males.
Our findings have several clinical and public health implications for girls and women with childhood ADHD. In terms of prevention efforts, given that ADHD is specifically associated with relationship violence, provision of empirically supported treatment targeting the core symptoms and characteristics of the disorder may have downstream effects of preventing IPV and its associated consequences (e.g., revictimization, physical and mental health problems). In conjunction, females with ADHD might be well-served by developmentally-appropriate interventions targeting social skills (e.g., nonviolent communication and conflict resolution) and IPV psychoeducation, as well as academic skill training. Finally, findings also suggest that increasing the level of educational support for girls with ADHD, especially during adolescence, may not only have proximal benefits for their academic achievement but also may correlate distally with decrements in their IPV risk. Academic achievement and scholastic competence may be particularly protective for girls with ADHD, who experience significant school difficulties (Hinshaw, 1992; Mikami & Hinshaw, 2006).
Taken together, findings highlight that for women, childhood ADHD is specifically associated with lasting, adverse consequences for relationship functioning in the form of physical violence in their young adult intimate relationships. Improved prevention and intervention efforts, especially those focused on reducing core symptoms of ADHD and increasing academic support for females with ADHD, are critical to reducing the burden of IPV in this vulnerable population. Given the devastating impact of intimate partner violence, additional research on how to empower females with ADHD in their social and romantic relationships is greatly needed.
Acknowledgments
This research was supported by funding from National Institute of Mental Health Grant 45064 (to S.P.H.). We gratefully acknowledge the young women who have participated in this longitudinal investigation, along with their caregivers and the large number of graduate students and staff who have made this research possible. We also thank Fred Loya, Ph.D., Orly Perlstein, Lisa Post Tornes, Leslie Ho, and Esther Rah.
Footnotes
The authors declare that they have no conflict of interest.
The Guendelman et al. (in press) investigation focused almost exclusively on maltreatment in the ADHD sample only, and examined outcomes related to maltreatment in Waves 1 and 2 combined.
Among the 114 participants with ADHD, victimization risk did not differ by Wave 1 ADHD subtype (Combined: 31.6% vs. Inattentive: 28.9%, χ2(1, N = 114) = 0.08, OR = 1.13, 95% CI [0.48, 2.66], p = 0.48).
Within the transient ADHD group (n = 58), 47 participants had a diagnosis of ADHD at Wave 1 only, whereas 11 had ADHD at Wave 3 only. Ten (21.3%) of the participants with ADHD at Wave 1 only had physical IPV victimization, whereas one (9.1%) of the participants with ADHD at Wave 3 only had physical IPV victimization, χ2(1, N = 58) = 0.86, p = .33.
References
- Achenbach TM. Manual for the child behavior checklist and revised child behavior profile. Burlington, VT: University Associates in Psychiatry; 1991. [Google Scholar]
- Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55:469–480. [PubMed] [Google Scholar]
- Arnett JJ. Conceptions of the transition to adulthood: Perspectives from adolescence through midlife. Journal of Adult Development. 2001;8:133–143. [Google Scholar]
- Babinski DE, Pelham WE, Molina BS, Gnagy EM, Waschbusch DA, Yu J, Karch KM. Late adolescent and young adult outcomes of girls diagnosed with ADHD in childhood: An exploratory investigation. Journal of Attention Disorders. 2011;15:204–214. doi: 10.1177/1087054710361586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagwell CL, Molina BSG, Pelham WE, Hoza B. Attention-deficit hyperactivity disorder and problems in peer relations: Predictions from childhood to adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:1285–1292. doi: 10.1097/00004583-200111000-00008. [DOI] [PubMed] [Google Scholar]
- Bakeman R, Gottman JM. Observing interaction: An introduction to sequential analysis. 2. New York: Cambridge University Press; 1997. Assessing observer agreement; pp. 56–80. [Google Scholar]
- Barkley RA, Murphy KR, Fisher M. ADHD in adults: What the science says. New York: Guilford; 2008. [Google Scholar]
- Bensley L, Van Eenwyk J, Wynkoop Simmons K. Childhood family violence history and women’s risk for intimate partner violence and poor health. American Journal of Preventive Medicine. 2003;25:38–44. doi: 10.1016/s0749-3797(03)00094-1. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Monuteaux MC, Fried R, Byrne D, Mirto T, Faraone SV. Adult psychiatric outcomes of girls with attention deficit hyperactivity disorder: 11-year follow-up in a longitudinal case-control study. American Journal of Psychiatry. 2010;167:409–417. doi: 10.1176/appi.ajp.2009.09050736. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, O’Connor KB, Hyder LL, Faraone SV. Predictors of persistence in girls with attention-deficit/hyperactivity disorder: Results from an 11- year controlled follow-up study. Acta Psychiatrica Scandinavica. 2012;125:147–156. doi: 10.1111/j.1600-0447.2011.01797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blachman DR, Hinshaw SP. Patterns of friendship among girls with and without attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology. 2002;30:625–640. doi: 10.1023/a:1020815814973. [DOI] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Stevens MR. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- Briscoe-Smith AM, Hinshaw SP. Linkages between child abuse and attention-deficit/hyperactivity disorder in girls: Behavioral and social correlates. Child Abuse & Neglect. 2006;30:1239–1255. doi: 10.1016/j.chiabu.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capaldi DM, Knoble NB, Shortt JW, Kim HK. A systematic review of risk factors for intimate partner violence. Partner Abuse. 2012;3:231–280. doi: 10.1891/1946-6560.3.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Costs of intimate partner violence against women in the United States. Atlanta, GA: National Center for Injury Prevention and Control; 2003. [Google Scholar]
- Centers for Disease Control and Prevention. Intimate partner violence. 2014 Mar; Retrieved from http://www.cdc.gov/ViolencePrevention/intimatepartnerviolence/index.html.
- Chiodo D, Crooks CV, Wolfe DA, McIsaac C, Hughes R, Jaffe PG. Longitudinal prediction and concurrent functioning of adolescent girls demonstrating various profiles of dating violence and victimization. Prevention Science. 2012;13:350–359. doi: 10.1007/s11121-011-0236-3. [DOI] [PubMed] [Google Scholar]
- Connolly J, Pepler D, Craig W, Taradash A. Dating experiences of bullies in early adolescence. Child Maltreatment. 2000;5:299–310. doi: 10.1177/1077559500005004002. [DOI] [PubMed] [Google Scholar]
- Efron B, Tibshirani RJ. An introduction to the bootstrap. New York: Chapman & Hall; 1993. [Google Scholar]
- Ehrensaft MK, Cohen P, Brown J, Smailes E, Chen H, Johnson JG. Intergenerational transmission of partner violence: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2003;71:741–753. doi: 10.1037/0022-006x.71.4.741. [DOI] [PubMed] [Google Scholar]
- Erikson E. Identity: Youth and crisis. New York: Norton; 1968. [Google Scholar]
- Espelage DL, Holt MK. Dating violence and sexual harassment across the bully- victim continuum among middle and high school students. Journal of Youth and Adolescence. 2007;36:799–811. [Google Scholar]
- Fang X, Massetti GM, Ouyang L, Grosse SD, Mercy JA. Attention-deficit/hyperactivity disorder, conduct disorder, and young adult intimate partner violence. Archives of General Psychiatry. 2010;67:1179–1186. doi: 10.1001/archgenpsychiatry.2010.137. [DOI] [PubMed] [Google Scholar]
- Finkelhor D. Developmental victimology: The comprehensive study of childhood victimizations. In: Davis RC, Luirigio AJ, Herman S, editors. Victims of crime. 3. Thousand Oaks, CA: Sage Publications; 2007. pp. 9–34. [Google Scholar]
- Fleiss JL. Statistical methods for rates and proportions. New York: Wiley; 1981. [Google Scholar]
- Flory K, Molina BS, Pelham WE, Gnagy E, Smith B. Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child & Adolescent Psychology. 2006;35:571–577. doi: 10.1207/s15374424jccp3504_8. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Kamphaus RW, Lahey BB, Loeber R, Christ MAG, Hart EL, Tannenbaum LE. Academic underachievement and the disruptive behavior disorders. Journal of Consulting and Clinical Psychology. 1991;59:289–294. doi: 10.1037/0022-006X.59.2.289. [DOI] [PubMed] [Google Scholar]
- Fuller-Thomson E, Mehta R, Valeo A. Establishing a link between attention deficit disorder/attention deficit hyperactivity disorder and childhood physical abuse. Journal of Aggression, Maltreatment and Trauma. 2014;23:188–198. [Google Scholar]
- Greene RW, Biederman J, Faraone SV, Monuteaux MC, Mick E, DuPre EP, Goring JC. Social impairment in girls with ADHD: Patterns, gender comparisons, and correlates. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:704–710. doi: 10.1097/00004583-200106000-00016. [DOI] [PubMed] [Google Scholar]
- Guendelman MD, Owens EB, Galan C, Gard A, Hinshaw SP. Early- adult correlates of maltreatment in girls with attention-deficit/hyperactivity disorder: Increased risk for internalizing symptoms and suicidality. Development and Psychopathology. doi: 10.1017/S0954579414001485. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- Hinshaw SP. Academic underachievement, attention deficits, and aggression: Comorbidity and implications for intervention. Journal of Consulting & Clinical Psychology. 1992;60:893–903. doi: 10.1037//0022-006x.60.6.893. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP. Preadolescent girls with attention-deficit/hyperactivity disorder: I. Background characteristics, comorbidity, cognitive and social functioning, and parenting practices. Journal of Consulting and Clinical Psychology. 2002;70:1086–1098. doi: 10.1037//0022-006x.70.5.1086. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Sami N, Fargeon S. Prospective follow-up of girls with attention- deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. Journal of Consulting and Clinical Psychology. 2006;74:489–499. doi: 10.1037/0022-006X.74.3.489. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, Swanson EN. Prospective follow-up of girls with attention- deficit/hyperactivity disorder into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self-injury. Journal of Consulting and Clinical Psychology. 2012;80:1041–1051. doi: 10.1037/a0029451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjern A, Weitoft GR, Lindblad F. Social adversity predicts ADHD-medication in school children – a national cohort study. Acta Paediatrica. 2010;99:920–924. doi: 10.1111/j.1651-2227.2009.01638.x. [DOI] [PubMed] [Google Scholar]
- Hoza B. Peer functioning in children with ADHD. Journal of Pediatric Psychology. 2007;32:655–663. doi: 10.1093/jpepsy/jsm024. [DOI] [PubMed] [Google Scholar]
- Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA, Arnold LE. What aspects of peer relationships are impaired in children with attention deficit/hyperactivity disorder? Journal of Consulting and Clinical Psychology. 2005;73:411–423. doi: 10.1037/0022-006X.73.3.411. [DOI] [PubMed] [Google Scholar]
- Humphrey JL, Storch EA, Geffken GR. Peer victimization in children with attention-deficit hyperactivity disorder. Journal of Child Health Care. 2007;11:248–260. doi: 10.1177/1367493507079571. [DOI] [PubMed] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Mac OS, Microsoft Windows (Version 20.0) Armonk, NY: IBM Corp; 2011. [Google Scholar]
- Jewkes R. Intimate partner violence: Causes and prevention. The Lancet. 2002;359:1423–1429. doi: 10.1016/S0140-6736(02)08357-5. [DOI] [PubMed] [Google Scholar]
- Keenan-Miller D, Hammen CL, Brennan PA. Health outcomes related to early adolescent depression. Journal of Adolescent Health. 2007;41:256–262. doi: 10.1016/j.jadohealth.2007.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Walters EE, Forthofer MS. The social consequences of psychiatric disorders, III: Probability of marital stability. American Journal of Psychiatry. 1998;155:1092–1096. doi: 10.1176/ajp.155.8.1092. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory (CDI) manual. Toronto, Ontario, Canada: Multi-Health Systems; 1992. [Google Scholar]
- Krueger RF, Moffitt TE, Caspi A, Bleske A, Silva PA. Assortative mating for antisocial behavior: Developmental and methodological implications. Behavior Genetics. 1998;28:173–186. doi: 10.1023/a:1021419013124. [DOI] [PubMed] [Google Scholar]
- Kyriacou DN, Anglin D, Taliaferro E, Stone S, Tubb T, Linden JA, Kraus JF. Risk factors for injury to women from domestic violence. New England Journal of Medicine. 1999;341:1892–1898. doi: 10.1056/NEJM199912163412505. [DOI] [PubMed] [Google Scholar]
- Lehrer JA, Buka S, Gortmaker S, Shrier LA. Depressive symptomatology as a predictor of exposure to intimate partner violence among US female adolescents and young adults. Archives of Pediatrics & Adolescent Medicine. 2006;160:270–276. doi: 10.1001/archpedi.160.3.270. [DOI] [PubMed] [Google Scholar]
- Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. Journal of Pediatric Psychology. 2007;32:643–654. doi: 10.1093/jpepsy/jsl054. [DOI] [PubMed] [Google Scholar]
- Magdol L, Moffitt TE, Caspi A, Newman DL, Fagan J, Silva PA. Gender differences in partner violence in a birth cohort of 21-year-olds: Bridging the gap between clinical and epidemiological approaches. Journal of Consulting and Clinical Psychology. 1997;65:68–78. doi: 10.1037//0022-006x.65.1.68. [DOI] [PubMed] [Google Scholar]
- Max W, Rice DP, Finkelstein E, Bardwell RA, Leadbetter S. The economic toll of intimate partner violence against women in the United States. Violence and Victims. 2004;19:259–272. doi: 10.1891/vivi.19.3.259.65767. [DOI] [PubMed] [Google Scholar]
- Mikami AY, Hinshaw SP. Resilient adolescent adjustment among girls: Buffers of childhood peer rejection and attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology. 2006;34:825–839. doi: 10.1007/s10802-006-9062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikami AY, Lorenzi J. Gender and conduct problems predict peer functioning among children with attention-deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology. 2011;40:777–786. doi: 10.1080/15374416.2011.597089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A. Findings about partner violence from the Dunedin Multidisciplinary Health and Development Study. US Department of Justice, Office of Justice Programs, National Institute of Justice; 1999. [Google Scholar]
- National Institute of Mental Health. Research domain criteria project. 2014 Retrieved from http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml.
- Piacentini JC, Cohen P, Cohen J. Combining discrepant diagnostic information from multiple sources: Are complex algorithms better than simple ones? Journal of Abnormal Child Psychology. 1992;20:51–63. doi: 10.1007/BF00927116. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rees S, Silove D, Chey T, Ivancic L, Steel Z, Creamer M, Forbes D. Lifetime prevalence of gender-based violence in women and the relationship with mental disorders and psychosocial function. Journal of the American Medical Association. 2011;306:513–521. doi: 10.1001/jama.2011.1098. [DOI] [PubMed] [Google Scholar]
- Saltzman LE, Fanslow JL, McMahon PM, Shelley GA. Intimate partner violence surveillance: Uniform definitions and recommended data elements, Version 1.0. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 1999. [Google Scholar]
- Sciberras E, Ohan J, Anderson V. Bullying and peer victimization in adolescent girls with attention-deficit/hyperactivity disorder. Child Psychiatry & Human Development. 2012;43:254–270. doi: 10.1007/s10578-011-0264-z. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children, Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Sirin SR. Socioeconomic status and academic achievement: A meta-analytic review of research. Review of Educational Research. 2005;75:417–453. [Google Scholar]
- Stith SM, Smith DB, Penn CE, Ward DB, Tritt D. Intimate partner physical abuse perpetration and victimization risk factors: A meta-analytic review. Aggression and Violent Behavior. 2004;10:65–98. [Google Scholar]
- Swanson JM. School-based assessments and interventions for ADD students. Irvine, CA: K. C. Press; 1992. [Google Scholar]
- Swanson EN, Owens EB, Hinshaw SP. Pathways to self-harmful behaviors in young women with and without ADHD: A longitudinal investigation of mediating factors. Journal of Child Psychology and Psychiatry. 2014;55:505–515. doi: 10.1111/jcpp.12193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theriault SW, Holmberg D. Impulsive, but violent? Are components of the attention-deficit hyperactivity syndrome associated with aggression in relationships? Violence Against Women. 2001;7:1464–1489. [Google Scholar]
- Thompson RS, Bonomi AE, Anderson M, Reid RJ, Dimer JA, Carrell D, Rivara FP. Intimate partner violence: Prevalence, types, and chronicity in adult women. American Journal of Preventive Medicine. 2006;30:447–457. doi: 10.1016/j.amepre.2006.01.016. [DOI] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Extent, nature, and consequences of intimate partner violence: Findings from the National Violence Against Women Survey. Washington, DC: US Department of Justice, Office of Justice Programs, National Institute of Justice; 2000. [Google Scholar]
- Trevillion K, Oram S, Feder G, Howard LM. Experiences of domestic violence and mental disorders: A systematic review and meta-analysis. PloS One. 2012;7 doi: 10.1371/journal.pone.0051740. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vest JR, Catlin TK, Chen JJ, Brownson RC. Multistate analysis of factors with intimate partner violence. American Journal of Preventive Medicine. 2002;22:156–164. doi: 10.1016/s0749-3797(01)00431-7. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Intelligence Scales for Children. 3. New York: Psychological Corporation; 1991. [Google Scholar]
- Wechsler D. Wechsler Individual Achievement Test. New York: Psychological Corporation; 1992. [Google Scholar]
- Wechsler D. Wechsler Individual Achievement Test. 2. New York, NY: Psychological Corporation; 2001. [Google Scholar]
- Whitaker DJ, Haileyesus T, Swahn M, Saltzman LS. Differences in frequency of violence and reported injury between relationships with reciprocal and nonreciprocal intimate partner violence. American Journal of Public Health. 2007;97:941–947. doi: 10.2105/AJPH.2005.079020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitfield CL, Anda RF, Dube SR, Felitti VJ. Violent childhood experiences and the risk of intimate partner violence in adults: Assessment in a large health maintenance organization. Journal of Interpersonal Violence. 2003;18:166–185. [Google Scholar]
- Wiener J, Mak M. Peer victimization in children with attention-deficit/hyperactivity disorder. Psychology in the Schools. 2009;46:116–131. [Google Scholar]
- Wymbs B, Molina B, Pelham W, Cheong J, Gnagy E, Belendiuk K, Waschbusch D. Risk of intimate partner violence among young adult males with childhood ADHD. Journal of Attention Disorders. 2012;16:373–383. doi: 10.1177/1087054710389987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalecki CA, Hinshaw SP. Overt and relational aggression in girls with attention deficit hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology. 2004;33:125–137. doi: 10.1207/S15374424JCCP3301_12. [DOI] [PubMed] [Google Scholar]


