Abstract
Background
Vascular disease factors like hypertension, diabetes mellitus, dyslipidaemia, and ischaemic heart disease contribute to the development of vascular dementia. As comorbidity of vascular disease factors in vascular dementia is common, we investigated the vascular disease burden in subjects with vascular dementia.
Aims
To investigate the vascular disease burden due to four vascular disease factors: hypertension, diabetes mellitus, dyslipidaemia, and ischaemic heart disease in Indian subjects with vascular dementia.
Methods
In this study, 159 subjects with probable vascular dementia (as per NINDS-AIREN criteria) attending the memory clinic at a tertiary care hospital were assessed for the presence of hypertension, diabetes mellitus, dyslipidaemia, and ischaemic heart disease using standardised operational definitions and for severity of dementia on the Clinical Dementia Rating (CDR) scale. The data obtained was subjected to appropriate statistical analysis.
Results
Dyslipidaemia (79.25 per cent) was the most common vascular disease factor followed by hypertension (73.58 per cent), ischaemic heart disease (58.49 per cent), and diabetes mellitus (40.80 per cent). Most subjects (81.1 per cent) had two or more vascular disease factors. Subjects with more severe dementia had more vascular disease factors (sig 0.001).
Conclusion
People with moderate to severe dementia have a significantly higher vascular disease burden; therefore, higher vascular disease burden may be considered as a poor prognostic marker in vascular dementia. Subjects with vascular dementia and their caregivers must manage cognitive impairment and ADL alongside managing serious comorbid vascular diseases that may worsen the dementia.
Keywords: Vascular dementia, hypertension, diabetes mellitus, dyslipidaemia, ischaemic heart disease, dementia severity, vascular disease burden
What this study adds:
-
What is known about this subject?
Vascular disease risk factors are common in vascular dementia and contribute to its development. These vascular risk factors rarely occur in isolation and hence add to overall disease burden in vascular dementia.
-
What new information is offered in this study?
Subjects with vascular dementia have a high vascular disease burden. The vascular disease burden is significantly greater in subjects with moderate to severe vascular dementia.
-
What are the implications for research, policy, or practice?
The vascular disease burden in people with vascular dementia necessitates revision of treatment strategies and research into pathophysiological mechanisms, preventive approaches, and effective public health approaches.
Background
Vascular dementia is the second most common type of dementia. Hypertension, dyslipidaemia, metabolic syndrome, myocardial infarction, arrhythmias, and cardiovascular disease have been aetiologically implicated in the development of vascular dementia.1–6 These factors rarely occur in isolation and are often comorbid, hence subjects with vascular dementia and their caregivers face the challenge of having to manage impairment in cognition and activities of daily living (ADL) alongside managing serious comorbid conditions that may worsen the dementia.
Currently in India there are about 3.7 million people with dementia and this number is projected to double by 2030.7 India also has a huge burden of vascular disease risk factors. The Indian Council of Medical Research (ICMR)–World Health Organization (WHO) study in 2006 on the burden of disease has given the average prevalence of hypertension to be 16.4 per cent in urban areas and 15.7 per cent in rural areas.8 The same study estimated the average prevalence for ischaemic heart disease to be 6.4 per cent in urban areas and 2.5 per cent in rural areas. The ICMR multi-centric study on risk factors for non-communicable diseases also showed that a high proportion of Indians had substantial vascular risk factors like hypertension, diabetes, and raised cholesterol levels.9
With this background we decided to study the profile of specific comorbid vascular risk factors in Indian subjects with vascular dementia to understand better the vascular disease burden in vascular dementia.
Method
This was a tertiary hospital outpatient-based, cross-sectional cohort study. The study protocol was approved by the Institutional Ethics Committee of our hospital (Reference No. 1- /2013/thesis/IEC/PGIMER/RMLH) in accordance with the Declaration of Helsinki of 1975 (revised 2008) prior to the start of the study.
Sample size calculation
The prevalence of vascular disease factors like hypertension and diabetes in vascular dementia is well known.10–12 Hypertension is considered the most common vascular disease factor in vascular dementia. The sample size was calculated based on the population prevalence of hypertension given by an earlier epidemiological study in a similar population in Delhi.13 Taking Type I error to be 0.05 and Type II error to be 0.1, the sample size was determined to be 152.
Recruitment and data collection
All subjects with dementia aged 55 years and above attending the memory clinic at our tertiary care hospital were assessed for probable vascular dementia as per the National Institute of Neurological Disorders and Stroke and the Association Internationale pour la Recherché et l’Ensignement en Neurosciences (NINDS-AIREN) criteria.14 The memory clinic is a specialised clinic for dementia assessment and management. It has patients referred from the departments of psychiatry, neurology, medicine, and other specialities.
All subjects underwent MRI brain scans that were reported by trained radiologists. The clinical diagnosis of probable vascular dementia was made on detailed clinical evaluation and review of necessary investigations, including MRI brain scans by at least two trained neurologists.
The exclusion criteria for the study were designed to exclude cognitive decline due to any other aetiology. Exclusion criteria were dementia due to any other aetiology (including Alzheimer’s Disease, dementia with Lewy Bodies, fronto-temporal dementia, secondary dementia etc.), current delirium, current major depressive disorder, hepatic, renal or thyroid dysfunction, previous significant head injury, mental retardation, history of psychiatric disorders associated with cognitive deficits such as schizophrenia and bipolar disorder, micronutrient deficiencies known to impair cognition such as B12 and folate, or history of any substance dependence other than nicotine. These factors were ruled out on the basis of history, detailed clinical examination, mental status examination, and appropriate investigations.
Subjects who met the study criteria were enrolled in the study after obtaining written informed consent from the patient and their familial caregivers. After recording their socio-demographic profile, the subjects were assessed for various vascular disease risk factors based on history, past treatment records, clinical examination, and investigations. For the purpose of our research, the standardised operational definition for each vascular factor was identified to ensure validity of assessment of each vascular disease factor. These definitions for the purpose of our study were as follows:
Hypertension
Hypertension is defined as systolic blood pressure of more than 140mmHg or diastolic blood pressure of more than 90mmHg as per the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure VII criteria (JNC VII) on two or more measurements on separate occasions, history of hypertension in previous treatment records, or current use of any antihypertensive agents for treatment of hypertension as per medical records.15
Diabetes mellitus
Fasting blood sugar level of ≥126mg/dl (7.0mmol/l) (fasting is defined as no caloric intake for at least eight hours) or two-hour plasma glucose ≥200mg/dl (11.1mmol/l) during an oral glucose tolerance test using a glucose load containing the equivalent of 75g anhydrous glucose dissolved in water or in a patient with classic symptoms of hyperglycaemia or hyperglycaemic crisis, a random plasma glucose ≥200mg/dl (11.1mmol/l) or A1c levels of 6.5 per cent or above as per the American Diabetes Association (ADA) guidelines, history of diabetes in previous treatment records, or current use of any oral hypoglycaemic agents or insulin.16
Dyslipidaemia
Dyslipidaemia was defined as per the United States National Cholesterol Education Program Adult Treatment Panel (US NCEP ATP) III Guidelines.17 The US NCEP ATP III Guidelines are based on assessment for coronary heart disease (CHD), CHD equivalents (symptomatic carotid artery disease, peripheral artery disease, abdominal aortic aneurysm, or diabetes mellitus) and risk factors (nicotine use, hypertension, low HDL cholesterol less than 40 mg/dl, family history of premature CHD, age more than or equal to 45 years in males and 55 years in females with HDL cholesterol, more than 60mg/dl negating for one risk factor), and evaluation of 10-year CHD risk or subjects with 2+ risk factors as per Framingham Tables.
Accordingly, the cut-offs for diagnosing raised LDL cholesterol for subjects with CHD/CHD equivalent/10-year CHD risk more than 20 per cent is 100mg/dl, for subjects with more than two risk factors with 10-year CHD risk more than 10-20 per cent is 130mg/dl, for subjects with more than two risk factors with 10-year CHD risk less than 10 per cent is 160mg/dl, for subjects with either no or one risk factor is 160mg/dl.
Raised triglyceride levels are defined as more than or equal to 150mg/dl. The presence of raised LDL cholesterol or triglyceride levels or documented history of dyslipidaemia in previous treatment records, or current use of any lipid-lowering agent like statins or fenofibrate was considered as dyslipidaemia for the purpose of the study.
Ischaemic cardiovascular disease
Ischaemic cardiovascular disease is based on a history of myocardial infarction, angina with ischaemic changes on graded exercise tests or positive imaging, previous coronary revascularisation procedures like coronary angioplasty or bypass in previous treatment records, or current use of any anti angina agents. 18
The severity of dementia was determined using the CDR scale, which is a widely used measure of severity of dementia with high validity and reliability.19 Mild dementia is given a score of one, moderate dementia a score of two, and severe dementia a score of three.
Data analysis
The data obtained was statistically analysed using descriptive statistics, ANOVA, and Chi-square tests (as appropriate) using SPSS version 17.
Results
A total of 159 subjects with vascular dementia were enrolled in the study between 1 June 2013 and 31 October 2014. The socio-demographic and clinical profile of subjects is given in Table 1. The study subjects were 55 to 88 years in age (mean age of 69.35 ± 7.51 years). There were 87 males and 72 females enrolled in the study. Most subjects were married reflecting the socio-cultural norm. Nearly 30 per cent were widowed. All subjects had received at least primary school education, i.e., five years of formal schooling and no subject was illiterate.
Table 1:Socio-demographic and clinical profile of subjects with vascular dementia.
| n=159 | |
|
Age in years
[Mean ± sd (range)] |
69.35 ±7.51 (55–88) |
| Sex [n(%)] | 87:72 (54.7: 45.3%) |
| Male | 87 (54.7%) |
| Female | 72 (45.3%) |
|
Educational attainment in years
[Mean ± sd (range)] |
11.34±3.76 (5-20) |
| Marital Status [n(%)] | |
| Married | 113 (71.1%) |
| Widowed | 45 (28.3%) |
| Divorced/Separated | 1 (0.6%) |
| Hypertension [n(%)] | 117 (73.58%) |
| Diabetes Mellitus [n(%)] | 65 (40.80%) |
| Dyslipidaemia [n(%)] | 126 (79.25%) |
| Ischaemic Heart Disease [n(%)] | 93 (58.49%) |
| Number of Vascular Disease factors [n(%)] | |
| 0 | 7 (4.4%) |
| 1 | 23 (14.5%) |
| 2 | 51 (32.1%) |
| 3 | 42 (26.4%) |
| 4 | 36 (22.6%) |
The most common vascular risk factor was dyslipidaemia (79.25 per cent), followed by hypertension (73.58 per cent). Ischaemic heart disease was found in 58.49 per cent of subjects, while diabetes mellitus was found in 40.80 per cent subjects.
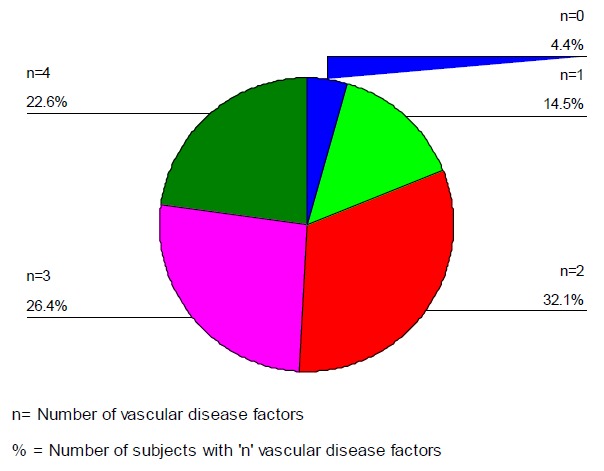
Most subjects had two or more vascular disease factors indicating a trend towards a high comorbid vascular disease burden and less than five per cent had none of the investigated vascular disease factors (Figure 1).
Figure 1: Vascular disease burden in subjects with vascular dementia.
Further analysis was done according to the severity of dementia as per CDR scores (Table 2). The subjects in the mild, moderate, and severe dementia groups were comparable with respect to gender, educational attainment, and marital status. The subjects in the severe dementia group were significantly older than the mild dementia subjects. Significant differences were evident in the three severity groups with respect to rates of hypertension, dyslipidaemia, or ischaemic heart disease individually, and total number of vascular disease factors reflecting the composite vascular disease burden.
Table 2:Analysis of vascular disease burden according to severity of vascular dementia.
| Mild Dementia (n=64) | Moderate Dementia (n=59) | Severe Dementia (n=36) | Sig* (p=0.05) | Post-Hoc Tukey’s Analysis | |
|---|---|---|---|---|---|
|
Age in years
[mean± s.d. (range)] |
67.08 +7.07 (55-82) |
69.93+7.09 (55-87) |
72.42 +7.84 (60-88) |
0.002 * | Mild-Severe =0.002 Mild-Moderate= 0.078 Moderate-Severe=0.241 |
|
Sex
[Male: Female in n(%)] |
32:28 (53.3: 46.7) |
33:25 (56.9: 43.1) |
17:16 (51.5: 48.5) |
0.401 | |
|
Education in years
[mean± s.d. (range)] |
11.77 + 3.77 (5–18) |
11.51 + 3.65 (5–20) |
10.31 + 3.85 (5–17) |
0.161 | |
| Marital Status [n(%)] | |||||
| Married | 42 (65.63) | 42 (71.19) | 29 (80.56) | 0.452 | |
| Widowed | 21 (32.81) | 17(28.81) | 7(19.44) | ||
| Divorced | 1 (1.56) | 0 (0) | 0 (0) | ||
| Vascular disease factors [n(%)] | |||||
| Hypertension | 44 (68.75) | 38 (64.41) | 35 (97.22) | 0.001* | |
| Diabetes mellitus | 19 (29.69) | 28 (47.46) | 18 (50.00) | 0.060 | |
| Dyslipidaemia | 52 ( 81.25) | 41(69.49) | 33 (91.67) | 0.031* | |
| Ischaemic Heart Disease | 28 (43.75) | 38(64.41) | 27 (75.00) | 0.005* | |
| Number of vascular disease factors [n(%)] | |||||
| 0 | 2 (3.13) | 5 (8.47) | 0 (0) | 0.001* | |
| 1 | 12 (18.75) | 8 (13.56) | 3 (8.33) | ||
| 2 | 28 (43.75) | 19 (32.20) | 4 (11.11) | ||
| 3 | 15 (23.44) | 12 (20.34) | 15 (41.67) | ||
| 4 | 7 (10.93) | 15 (25.43) | 14 (38.89) | ||
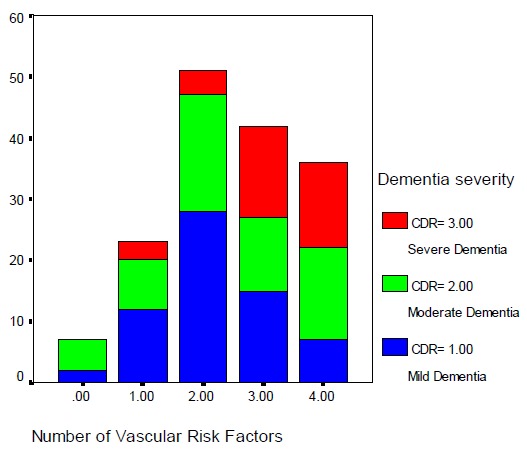
The results showed an inverse relationship between severity of dementia and vascular burden in terms of the number of vascular risk factors (Figure 2 and 3). Subjects with moderate to severe dementia (CDR scores 2 and 3) had proportionately more risk factors (Figure 2). Most subjects in the severe dementia group had 3–4 vascular risk factors, while most subjects with mild dementia had 1–2 vascular risk factors. Similarly, subjects with more vascular risk factors were more likely to have moderate or severe dementia Figure 3). Subjects with one or two vascular risk factors mostly had mild dementia, while most subjects with three or more vascular factors had moderate to severe dementia.
Figure 2: Vascular disease burden as per severity of vascular dementia.
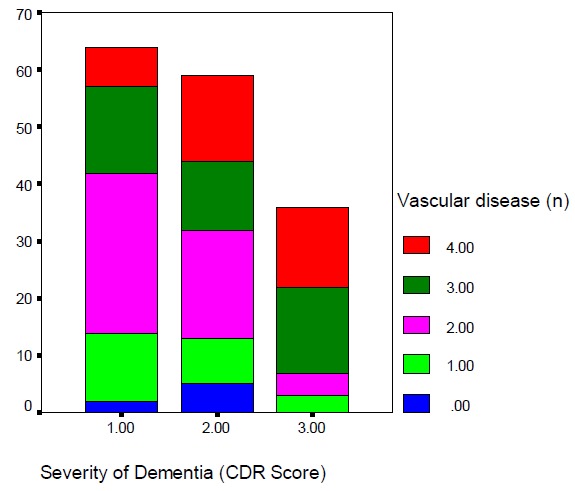
Figure 3: Severity of dementia as per number of vascular disease factors.
Discussion
The presence of vascular risk factors in subjects with vascular dementia has been assessed for different ethnic populations, but how multiple vascular risk factors contribute to more severe dementia has not been established and this was the focus of our research. This study demonstrates that subjects with vascular dementia have a number of vascular risk factors as reported in earlier literature.1–6,20 Subjects with vascular dementia have a high vascular disease burden. Fewer than five per cent of subjects had none of the investigated vascular disease factors and mostly had moderate dementia. This group had high levels of nicotine dependence (results reported in a separate publication).21
Dyslipidaemia, hypertension, and ischaemic heart disease were the most common vascular disease factors. The vascular disease factors investigated in our study are well identified in the literature.20 The most common vascular risk factor in our study was dyslipidaemia, which can be attributed to high rates of lipid abnormalities in both hypertensive and diabetic subjects.22, 23
The rate of hypertension in the study population was very high, far in excess of already high population rates of around 63 per cent in the elderly general population in Delhi as reported in an earlier epidemiological study.13 Similarly, the rates of diabetes, dyslipidaemia, and ischaemic heart disease in the study population are far in excess of population prevalence rates reflecting the contributory role of these vascular disease factors in the development and course of vascular dementia.8,9
Vascular risk factors continue to operate even after the development of vascular dementia. The authors had hypothesised that a higher vascular disease burden would contribute to a more severe state of dementia. The vascular disease burden in our study was significantly more in subjects with moderate to severe vascular dementia reflecting the cumulative impact of different vascular factors on the course and outcome of vascular dementia.
With regard to the severity of dementia, the rates of all investigated vascular disease risk factors were higher in moderate and severe dementia subgroups except for diabetes mellitus. Though the rate of diabetes mellitus was higher in the moderate and severe dementia groups as compared to mild dementia group, the difference was not statistically significant. This must be interpreted in light of the fact that the subjects with severe dementia were significantly older. Therefore, the lack of statistically significant difference in rates of diabetes mellitus between moderate and severe dementia (47.46 per cent versus 50 per cent) may be attributed to decreased survivor rates and the shorter life expectancy by up to 10 years in people with diabetes mellitus.24–28 In other words, people with vascular dementia and diabetes mellitus may succumb to a diabetes-related complication before developing severe dementia.
The study has several strengths. First, it was a well-planned systematic investigation into vascular disease burden in vascular dementia. The study was designed using nosologically valid diagnosis for vascular dementia by using NINDS-AIREN criteria.14 Standardised operational definitions for various vascular disease risk factors allowed for reliable assessment of vascular disease burden.15–18 The CDR scale was used to determine severity of dementia.19 The study population comprised Indian subjects who are at increased risk for high vascular disease burden as per different epidemiological studies8,9 and hence may be at increased risk for more severe states of vascular dementia.
The major limitation is the site of the study. It was a hospital-based study at a tertiary care centre attending to subjects referred from other specialities. The patient load does not reflect a community-based sample. The actual vascular disease burden can be better determined by appropriately designed community-based epidemiological studies incorporating other vascular factors like arrhythmia, hypotension, etc., in addition to the ones investigated in our study.
The NINDS-AIREN criteria for vascular dementia employed in our study have been reported to have issues of low sensitivity and moderate inter-rater reliability. Further, a diagnosis of probable vascular dementia was used in the study because a diagnosis of definite vascular dementia, which requires histopathological correlation from biopsy or autopsy, was beyond the scope of the study.
On the other hand, the NINDS-AIREN criteria have the advantage of high specificity Further, they take into consideration evidence of vascular lesions on neuroimaging, a wide range of neurological symptoms consistent with vascular dementia (and not just focal neurological deficits), many etiopathological causes of vascular dementia (unlike other diagnostic criteria). Hence, the NINDS-AIREN criteria are able to capture the broad rubric of vascular insufficiency contributing to development of dementia.29 Since the research focussed on the role of vascular disease burden, the NINDS-AIREN criteria were considered appropriate for the study.
Conclusion
Vascular dementia is the second most common type of dementia and is associated with an enormous vascular disease burden. Subjects with vascular dementia and their caregivers must manage cognitive impairment and ADL alongside managing serious comorbid vascular diseases that have the potential to worsen the dementia.
Vascular risk factors are known to contribute to the development of incident vascular dementia in different ethnic populations and continue to operate even after the development of vascular dementia. This study demonstrates that vascular risk factors also have a prognostic significance with higher vascular disease burden being a poor prognostic marker and contributing to a more severe dementia state.
Information on vascular burden in vascular dementia necessitates revision of pharmacological and non-pharmacological treatment strategies. Further research is also needed to elucidate the pathophysiological mechanisms of vascular dementia and to determine an evidence base for various preventive approaches. As most vascular disease factors are amenable to pharmacological and non-pharmacological interventions, a more comprehensive public health policy must be devised to address primary and secondary prevention of vascular dementia.
ACKNOWLEDGEMENTS
This paper was written as a part of PhD research carried out at the Post-Graduate Institute of Medical Education and Research and Dr. Ram Manohar Lohia Hospital under Guru Gobind Singh Indra Prastha University, New Delhi.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
ETHICS COMMITTEE APPROVAL
Institutional Ethics Committee, Dr Ram Manohar Lohia Hospital, New Delhi. Approval Reference No. 1- /2013/thesis/IEC/PGIMER/RMLH dated 21 May 2013.
Please cite this paper as: Chandra M, Anand KS. Vascular disease burden in Indian subjects with vascular dementia. AMJ 2015;8(7): 227–234. http//dx.doi.org/10.4066/AMJ.2015.2390
References
- 1.Kalmijn S, Foley D, White L. et al. Metabolic Cardiovascular Syndrome and Risk of Dementia in Japanese-American Elderly Men-The Honolulu-Asia Aging Study. Arterioscler Thromb Vasc Biology. 2000;20:2255–60. doi: 10.1161/01.atv.20.10.2255. PMID:11031212. [DOI] [PubMed] [Google Scholar]
- 2.Whitmer RA, Selby SJ, Johnston SC. et al. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology. 2005;64:277–81. doi: 10.1212/01.WNL.0000149519.47454.F2. doi: 10.1212/01.WNL.0000149519.47454.F2. [DOI] [PubMed] [Google Scholar]
- 3.Reitz C, Tang MX, Schupf N. et al. A Summary Risk Score for the Prediction of Alzheimer Disease in Elderly Persons. Archives of Neurology. 2010;67(7):835–41. doi: 10.1001/archneurol.2010.136. DOI: 10.1001/archneurol.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solfrizzi V, Solfrizzi E, Capurso C. et al. Italian Longitudinal Study on Ageing Working Group Metabolic syndrome and the risk of vascular dementia: the Italian Longitudinal Study on Ageing. J Neurol Neurosur Ps. 2010;81(4):433–40. doi: 10.1136/jnnp.2009.181743. doi: 10.1136/jnnp.2009.181743. [DOI] [PubMed] [Google Scholar]
- 5.Kaffashian S, Dugravot A, Nabi H. et al. Predictive utility of the Framingham general cardiovascular disease risk profile for cognitive function: evidence from the Whitehall II study. Eur Heart J. 2011;32:2326–32. doi: 10.1093/eurheartj/ehr133. DOI: http://dx.doi.org/10.1093/eurheartj/ehr133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rönnemaa E, Zethelius B, Lannfelt L. et al. Vascular risk factors and dementia: 40-year follow-up of a population-based cohort. Dement Geriatr Cogn Disord. 2011;31(6):460–6. doi: 10.1159/000330020. doi: 10.1159/000330020. [DOI] [PubMed] [Google Scholar]
- 7.Shaji KS, Jotheeswaran AT, Girish N. et al. The dementia India report 2010 – prevalence, impact, costs and services for dementia – a report prepared for The Alzheimer’s and Related Disorders Society of India. 2010:13–4. [Google Scholar]
- 8.Mathur P, Shah B. Research priorities for prevention and control of Non Communicable Diseases in India. Indian J Community Med. 2011;36(Suppl S1):72–7. doi: 10.4103/0970-0218.94713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah B, Mathur P. Surveillance of cardiovascular disease risk factors in India: The need & scope’. Indian J Med Res. 2010;132:634–42. doi: 10.4103/0971-5916.73420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hébert R, Lindsay J, Verreault R. et al. Vascular Dementia: Incidence and Risk Factors in the Canadian Study of Health and Aging. Stroke. 2000;31:1487–93. doi: 10.1161/01.str.31.7.1487. [DOI] [PubMed] [Google Scholar]
- 11.Welsh TJ, Gladman JR, Gordon AL. The treatment of hypertension in people with dementia: a systematic review of observational studies. BMC Geriatrics. 2014;14:19. doi: 10.1186/1471-2318-14-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindsay J, Hébert R, Rockwood K. The Canadian Study of Health and Aging - Risk Factors for Vascular Dementia. Stroke. 1997;28:526–30. doi: 10.1161/01.str.28.3.526. [DOI] [PubMed] [Google Scholar]
- 13.Chaturvedi S, Pant M, Neelam. et al. Hypertension in Delhi: prevalence, awareness, treatment and control. Trop Doct. 2007;37(3):142–5. doi: 10.1258/004947507781524593. PMID:17716496. [DOI] [PubMed] [Google Scholar]
- 14.Roman GC, Tatemichi TK, Erkinjuntti T. et al. Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology. 1993;43(2):250–60. doi: 10.1212/wnl.43.2.250. [DOI] [PubMed] [Google Scholar]
- 15.Chobanian AA, Bakris GL, Black HR. et al. The National High Blood Pressure Education Program Coordinating Committee. JNC 7: Complete Report-Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 16.American Diabetes Association. Standards of Medical Care in Diabetes-2013. Diabetes Care. 2013;36(Supplement 1):S11–S66. doi: 10.2337/dc13-S011. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Expert Panel on the Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. PMID:11368702. [DOI] [PubMed] [Google Scholar]
- 18.Fihn SD, Gardin JM, Abrams J. et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60(24):e44–e164. doi: 10.1016/j.jacc.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 19.Morris JC. Clinical Dementia Rating: A Reliable and Valid Diagnostic and Staging Measure for Dementia of the Alzheimer Type. Int Psychogeriatr. 1997;9(suppl.1):173–6. doi: 10.1017/s1041610297004870. [DOI] [PubMed] [Google Scholar]
- 20.Gorelick PB. Risk Factors for Vascular Dementia and Alzheimer Disease. Stroke. 2004;35:2620–22. doi: 10.1161/01.STR.0000143318.70292.47. DOI: 10.1161/01.STR.0000143318.70292.47. [DOI] [PubMed] [Google Scholar]
- 21.Chandra M, Anand KS. Assessment of nicotine dependence in subjects with vascular dementia. Int J Res Med Sci. 2015;3:711–4. doi: 10.5455/2320-6012.ijrms20150335. [Google Scholar]
- 22.Chehade JM, Gladysz M, Mooradian AD. Dyslipidaemia in type 2 diabetes: prevalence, pathophysiology, and management. Drugs. 2013 Mar;73(4):327–39. doi: 10.1007/s40265-013-0023-5. doi: 10.1007/s40265-013-0023-5. [DOI] [PubMed] [Google Scholar]
- 23.Yadav D, Mishra M, Tiwari A. et al. Prevalence of Dyslipidemia and Hypertension in Indian Type 2 Diabetic Patients with Metabolic Syndrome and its Clinical Significance. Osong Public Health Res Perspect. 2014;5(3):169–75. doi: 10.1016/j.phrp.2014.04.009. doi: 10.1016/j.phrp.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leal J, Gray AM, Clarke PM. Development of life-expectancy tables for people with type 2 diabetes. Eur Heart J. 2009;30(7):834–39. doi: 10.1093/eurheartj/ehn567. doi:10.1093/eurheartj/ehn567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dale AC, Nilsen TI, Vatten L. et al. Diabetes mellitus and risk of fatal ischaemic heart disease by gender: 18 years follow up of 74 914 individuals in the HUNT 1 Study. Eur Heart J. 2007;28:2924–9. doi: 10.1093/eurheartj/ehm447. PMID:17947212. [DOI] [PubMed] [Google Scholar]
- 26.Gu K, Cowie CC, Harris MI. Mortality in adults with and without diabetes in a national cohort of the U. S. population, 1971–1993. Diabetes Care. 1998;21:1138–45. doi: 10.2337/diacare.21.7.1138. PMID:9653609. [DOI] [PubMed] [Google Scholar]
- 27.Roper NA, Bilous RW, Kelly WF. et al. Excess mortality in a population with diabetes and the impact of material deprivation: longitudinal, population based study. BMJ. 2001;322:1389–83. doi: 10.1136/bmj.322.7299.1389. PMCID: PMC32252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Conway BN, May ME, Blot WJ. Mortality Among Low-Income African Americans and Whites With Diabetes. Diabetes Care. 2012;35(11):2293–9. doi: 10.2337/dc11-2495. doi:10.2337/dc11-2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wetterling T, Kanitz R-D, Borgis K-J. Comparison of Different Diagnostic Criteria for Vascular Dementia (ADDTC, DSM-IV, ICD-10, NINDS-AIREN) Stroke. 1996;1996(27):30–36. doi: 10.1161/01.str.27.1.30. doi: 10.1161/01.STR.27.1.30. [DOI] [PubMed] [Google Scholar]


