Abstract
Health-related quality of life (HRQoL) is frequently impaired in primary hyperparathyroidism (PHPT) but it is unclear if surgery is beneficial. The objective was to prospectively assess HRQoL in PHPT (n=124) with the 15D instrument before and after surgery, to compare it with that of a comparable sample of the general population (n=4295), and search for predictors of HRQoL and its change. HRQoL, and clinical and laboratory parameters were measured before and at 6 and 12 months after surgery. Regression techniques were used to search for predictors of HRQoL and gains from treatment. Before surgery, PHPT patients had significantly lower mean 15D score compared to controls (0.813 vs 0.904, P<0.001). Excretion, mental function, discomfort and symptoms, distress, depression, vitality, and sexual activity were most impaired (all P<0.001). Number of medications (P=0.001) and subjective symptoms (P<0.05) but not calcium or parathyroid hormone (PTH) predicted impaired HRQoL. Serum 25-hydroxyvitamin D (25OHD) was of borderline significance (P=0.051). Compared to baseline, mean 15D score improved significantly 6 months after surgery (0.813 vs 0.865, P<0.001) and the effect sustained at 1 year (0.878, P<0.001). The improvement was clinically important in 77.4% of patients (P<0.001). Educational level independently predicted improvement (P<0.005). HRQoL is severely impaired in PHPT but improves significantly after surgery. The 15D is a sensitive tool for assessing HRQoL and recognizing patients likely to benefit from surgery.
Keywords: primary hyperparathyroidism, health-related quality of life, surgery, 15D
Introduction
The clinical presentation of primary hyperparathyroidism (PHPT) has changed during the last decades. The majority of patients are nowadays asymptomatic with only mild hypercalcaemia (1, 2, 3). Surgery offers the only opportunity for cure of PHPT. There is consensus that patients with markedly increased serum calcium concentrations or signs of skeletal or nephrological complications should undergo parathyroidectomy (4). Neuropsychological symptoms and impaired quality of life are commonly reported in PHPT (5, 6, 7), but whether such symptoms improve after surgery remains to be established (3). According to recent guidelines, the decision to operate should not be based on such criteria as the evidence currently is limited (8). However, symptoms of mild PHPT are difficult to evaluate and so far, no single good predictor of impaired health-related quality of life (HRQoL) in PHPT has been recognized. The value of symptoms as prognostic factors regarding who benefits from surgery has so far been poorly studied. The need for a sensitive tool applicable in the out-patient clinic was recently recognized (3). The 15D instrument (9) has previously been used to study HRQoL in many endocrine (10, 11, 12) and other diseases (13, 14), but not in PHPT. The 15D instrument is a well-validated tool for assessing HRQoL and can be used both as a single, total score and as a profile of 15 different aspects of HRQoL (9). We tested the hypothesis that in patients with PHPT, the 15D instrument might serve as a sensitive tool in assessing diffuse neurocognitive symptoms that might predict which patients benefit from surgery. In this single center study, we prospectively (before the operation, and at 6 and 12 months after surgery) investigated HRQoL as well as clinical and laboratory parameters in 124 PHPT patients referred for surgery to a single centre. The results were compared to those of a large representative sample of the general population (n=4295) standardized for gender and age (15).
Subjects and methods
Subjects
The final study group comprised 124 consecutive PHPT patients referred for parathyroidectomy to the Helsinki University Hospital between October 2010 and May 2013. All patients had first been evaluated by an endocrinologist at the Division of Endocrinology at the Helsinki University Hospital. Possible vitamin D supplementation was prescribed at this visit, i.e. at least 2–3 months before surgery. The preoperative 15D questionnaire was, on average, answered 1–2 weeks before surgery. All patients who were operated on for PHPT and who had answered the first, pre-operative 15D questionnaire were included in the study. The surgical criteria for PHPT were based on the recommendation of the Third International Workshop on the Management of Asymptomatic PHPT in 2008 and were fulfilled by 80.6% of patients (16). The surgical criteria (one or more) were as follows: osteoporosis in 60/124 (48.3%) patients, impaired kidney function in 17/124 (13.7%) patients, kidney stones in 9/124 (7.3%) patients, serum ionized calcium >1.50 mmol/l (reference range, 1.16–1.30 mmol/l) in 36/124 (29.0 %), and age <50 years in 12/124 (9.7%) patients. Twenty-four patients (19.4%) had biochemically mild PHPT and did not fulfill the prevailing surgical criteria for PHPT (16) although they were symptomatic. The mean age of the study cohort was 65 years (range 39–85) and 81.4% were females. Mean serum ionized calcium concentration was 1.47±0.12 mmol/l (reference range 1.16–1.30 mmol/l) and PTH concentration 176.3±155.6 ng/l (reference range 12–47 ng/l). Of the 124 patients, 115 were operated on because of PHPT for the first time, eight for the second, and one for the third time. The patients took on average four regular medications (range 0–11), 41.1% took five or more medications regularly.
Laboratory measurements
All laboratory tests were performed at the central laboratory of the Helsinki University Hospital, HUSLAB, using in-house methods. Serum ionized calcium was measured by ion-specific electrodes. Serum PTH was measured by a chemiluminometric assay. 25OHD was measured by HPLC, serum creatinine by an enzymatic photometric assay, and serum alkaline phosphatase as well as 24-h urinary calcium by photometric methods.
Study design
A 15D questionnaire including an explanatory letter and an additional questionnaire addressing educational level were sent to PHPT patients along with the date and information for the planned operation. One hundred and twenty eight patients returned the preoperative questionnaire. However, three patients had tertiary PHPT and one had not filled in the questionnaire, thus these patients were excluded from the study. Total response rate to the first questionnaire is unclear because the number of questionnaires sent was not counted. Another set of the 15D questionnaire was sent at 6 and 12 months after surgery to all patients who had returned the first questionnaire. In case of no response to the second or third questionnaire, a new questionnaire with an explanatory letter was sent once. Of the 124 respondents, 117 (94.4%) replied to the questionnaire at six and 116 (93.5%) at 12 months after surgery respectively. Demographic, biochemical and clinical data as well as operative results were collected from the electronic patient record of the Helsinki University Hospital. Possible PHPT-related symptoms (fatigue, depression, loss of memory, abdominal pain or nausea, muscle weakness, and joint pains) as documented by the endocrinologist evaluating the patient before surgery were retrieved from the electronic patient records of the Helsinki University Hospital. Approximately 200–230 patients undergo surgery for PHPT at the Helsinki University Hospital yearly, including reoperations, tertiary PHPT and surgery of MEN patients. The overall complication rate is ∼0.5–1% and is due to laryngeal nerve palsy.
The study was approved by the Ethical Committee of the Helsinki University Hospital. All patients gave their signed informed consent to participate in the study.
HRQoL assessment
The 15D questionnaire is a generic, standardized, well-validated, self-administered measure of HRQoL that can be used both as a profile or a single score measure (9). Each dimension (mobility, vision, hearing, breathing, sleeping, eating, speech, excretion, usual activities, mental function, discomfort and symptoms, depression, distress, vitality, and sexual activity) has five levels and the respondent chooses the level best describing her/his current health status for each dimension. The 15D score and the dimensional level values, both on a 0–1 scale, are calculated from the health state descriptive system by using a set of population-based preference or utility weights. A higher score reflects a better HRQoL. The minimum important change for the 15D score is estimated to be 0.015 for improvement and −0.015 for deterioration and 0.015 can also be regarded as the minimum clinically important cross-sectional difference between groups (13). The HRQoL of the study patients was compared to that of an age- and gender-adjusted sample of the Finnish general population from the Finnish Health 2011 survey (n=4924) (15).
Statistical analysis
The data were analyzed using IBM SPSS Statistics 19 (SPSS, Inc.). Patient characteristics are presented as means and s.d. for continuous variables, and frequencies and proportions for categorical variables. The statistical significance of the difference in the mean 15D score of the general population and study patients was tested by independent samples t-test, and that in the means of continuous variables, including the 15D scores before and after parathyroidectomy with paired samples t-test. As some of the 15D variables were not normally distributed, also corresponding non-parametric tests were applied. Apart from minor differences in the level of statistical significance, the results of parametric and non-parametric tests were quite similar. Therefore, only results of parametric tests are reported.
Linear regression was used to study the association between the baseline 15D score and a set of independent variables (age, gender, education level, serum ionized calcium, PTH and 25OHD concentrations, number of regular medication, and whether one experienced possible PHPT-related symptoms or not). Binary logistic regression was used to explore the association between the previously mentioned factors and baseline 15D score, and whether the patient had experienced at least a minimal clinically important improvement in the 15D score from baseline to 6 months after surgery or not. A P value <0.05 was considered statistically significant.
Results
Clinical and biochemical results of patients with PHPT
Clinical and biochemical characteristics of the study group are reported in Table 1. Compared to baseline concentrations, serum ionized calcium and serum PTH concentrations were significantly lower 1 month after surgery (1.47 mmol/l±0.12 vs 1.25 mmol/l±0.08 and 176.5 ng/l±155.6 vs 35.8 ng/l±33.4, respectively, P<0.001 for both) (Table 1). Parathyroidectomy resulted in normocalcaemia in 111 of 124 (89.5%) patients, while 13 (10.5%) patients did not reach normocalcaemia. Postoperative calcium concentrations decreased also in this subgroup (1.44±0.07 vs 1.36±0.05, P<0.001) indicating partial recovery.
Table 1.
Clinical and biochemical characteristics of 124 study subjects at baseline and postoperatively.
| Description | Mean±s.d. or number at baseline | Mean±s.d. postoperatively | Normal range |
|---|---|---|---|
| Age (years) | 65±10.2 | ||
| Number of women/men | 101/23 | ||
| BMI (kg/m2) | 27.4±5.1 | ||
| Blood pressure (mmHg) | 145/83±23/14 | ||
| Number of regular medication | 3.9±2.9 | ||
| Educational levela | 56/66/3 | ||
| Serum ionized calcium (mmol/l) | 1.47±0.12 | 1.25±0.08* | 1.16–1.3 |
| PTH (ng/l) | 176.3±155.6 | 35.8±33.4* | 12–47 |
| Creatinine (μmol/l) | 73.3±25.0 | ♀, 50–90; ♂, 60–100 | |
| GFR (ml/min/1.73 m2)b | 82.4±18.6 | >60 | |
| 25-OHD (nmol/l) | 57.2±17.8 | >40 | |
| 24-h urinary calcium (mmol) | 11.5±2.12 | 1.3–6.5 | |
| Alkaline phosphatase (U/l) | 74.8±25.6 | 35–105 |
*P<0.001 for comparison with preoperative concentrations.
Less than high school/high school or more/not known.
Calculated with CKD-EPI – equation.
Symptoms according to the electronic patient record
Fifty-one of the 124 (41.4%) patients suffered from possible PHPT-related symptoms, i.e. fatigue, depression, loss of memory, abdominal pain or nausea, muscle weakness, and joint pain.
HRQoL in patients with PHPT compared to general population controls
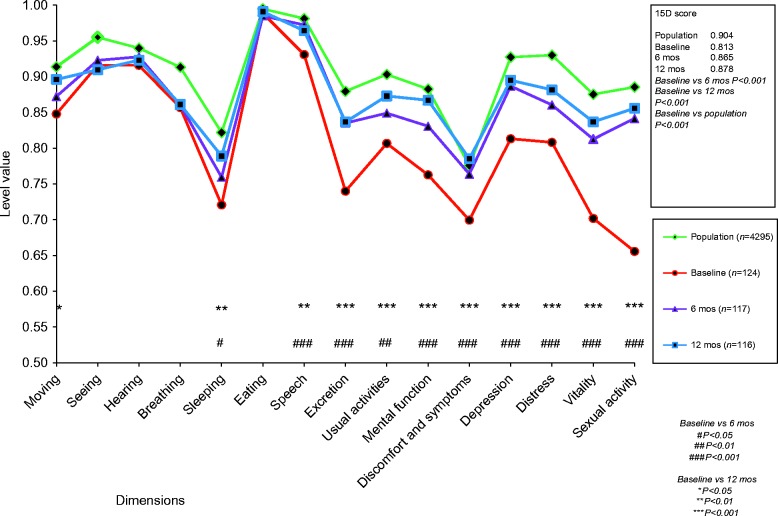
The mean 15D profiles for PHPT patients before parathyroidectomy and for the age- and gender-adjusted general population are presented in Fig. 1. Mean total preoperative 15D score of PHPT patients (n=124) was significantly lower (0.813±0.110 vs 0.904±0.091, P<0.001) compared to that of the general population (n=4295). PHPT patients were worse off on 13 of 15 dimensions of the HRQoL instrument (P<0.001 for 11 dimensions, P<0.01 for two dimensions). All five dimensions (mental function, discomfort and symptoms, depression, distress, vitality) measuring cognitive and psychiatric well-being were severely impaired compared to controls (all P<0.001). Excretion, usual activities and sexual activity were also severely impaired (all P<0.001). The dimensions of eating and hearing did not differ between patients and controls (Fig. 1).
Figure 1.
Mean 15D dimension profiles of PHPT patients before, at 6 months, and 12 months after parathyroidectomy compared to an age- and gender-adjusted sample of the general population.
HRQoL in patients with PHPT before and after surgery
The 15D results before and at 6 and 12 months after surgery are presented in Fig. 1. Six months after surgery, the mean 15D score (n=117) had increased significantly from baseline (0.813±0.105–0.865±0.108, P<0.001). The proportion of patients that experienced at least a minimum clinically important change in HRQoL after surgery was 77.4% for improvement and 13.7% for deterioration, respectively (Table 2). Regarding the different dimensions, a significant improvement was seen in ten of 15 dimensions. The most significant improvements were observed in speech, excretion, mental function, discomfort and symptoms, depression, distress, vitality, and sexual activity (all P<0.001). Usual activities (P<0.01) and sleeping also improved (P<0.05, Fig. 1). The 15D scores before surgery did not differ between the small subgroup of uncured (n=12) and cured (n=113) patients (0.778±0.095 vs 0.818±0.106, P=0.195), neither did the changes in 15D score 6 months after surgery (0.052±0.074 vs 0.061±0.083, P=0.695).
Table 2.
Classification of the changes in 15D scores from baseline to 6 months into global assessment scale categories and the distribution of the patients into these categories.
| Global assessment category | Limits for change in 15D scorea | Distribution of patients (%) |
|---|---|---|
| Much better | >0.035 | 60.5 |
| Slightly better | 0.015–0.035 | 16.9 |
| Much the same (no change) | >−0.015 and <0.015 | 8.9 |
| Slightly worse | −0.015 to −0.035 | 3.2 |
| Much worse | <−0.035 | 10.5 |
For the limits, see (13).
Compared to baseline, also mean 15D score 12 months after surgery (n=116) was significantly higher (0.813±0.105 vs 0.878±0.105, P<0.001) and similar to that of 6 months after surgery (Fig. 1). The most marked sustained improvements were noted on the dimensions of excretion, mental function, discomfort and symptoms, depression, distress, vitality, and sexual activity (all P<0.001). Usual activities (P<0.001), sleep, mobility, and speech also improved (P<0.01, Fig. 1).
Comparison of patients fulfilling and not fulfilling current criteria for surgery of PHPT
The difference in changes of total 15D scores from baseline to 6 months after surgery for those PHPT patients who fulfilled (n=100, 80.6%) and did not fulfill (n=24, 19.4%) the prevailing recommended surgical criteria (16) was not statistically significant (0.052±0.074 vs 0.060±0.101, respectively, P=0.643). Neither were there any statistically significant differences between these subgroups regarding the changes in the single 15 dimension scores.
Predictors of impaired HRQoL in PHPT
Of several possible independent variables (age, gender, educational level, serum ionized calcium and PTH concentrations, number of regular medications (range 0–11, mean 4), whether one experienced possibly PHPT-related symptoms or not), only the number of regular medications (β=−0.012, P=0.001) and whether one experienced subjective symptoms (β=−0.038, P=0.049) reached statistical significance as predictors of impaired HRQoL in PHPT patients before surgery (adjusted R2=0.175, F=3.948, P<0.001). Serum 25OHD level had a borderline significance in predicting impaired HRQoL (β=0.001, P=0.051).
Predictors of improved HRQoL after surgery in PHPT
Among different patient-related factors, higher educational level predicted improved HRQoL after surgery and low preoperative 15D score was of borderline significance (P=0.057) (Table 3).
Table 3.
The results of binary logistic regression model predicting whether the patient had experienced at least a minimum clinically important improvement in the 15D score from baseline to 6 months after operation.
| Variable | Regression coefficient | Significance |
|---|---|---|
| Constant | 9.506 | 0.112 |
| Age (years) | −0.037 | 0.217 |
| Gender (0=female, 1=male) | −0.480 | 0.481 |
| Educational levela | 1.858 | 0.003 |
| Preoperative serum calcium | −2.112 | 0.555 |
| Preoperative serum PTH | 0.001 | 0.817 |
| Preoperative serum 25OHD | 0.028 | 0.156 |
| No. of regular medication | 0.084 | 0.410 |
| Preoperative 15D score | −6.180 | 0.057 |
| Presence of self-reported symptoms | −0.959 | 0.100 |
High school or more=1, less than high school=0.
Discussion
The main findings of this prospective study are that PHPT patients scheduled for surgery because of the disease have significantly impaired HRQoL compared to the age- and gender-adjusted general population as assessed by the 15D, that HRQoL significantly improves after surgery in the patients, and that the improvements are sustained 1 year after surgery.
Previous studies have reported impaired HRQoL using the SF-36 (17, 18, 19, 20), the Pasieka Assessment Scale (21), both (5, 7) or the SF-12 (22) in PHPT patients compared to healthy or thyroid-operated controls. These and other authors (6, 23, 24) reported improved HRQoL after surgery, but have been criticized regarding insufficient patients numbers, lack of control population and insufficient assessment of cognitive parameters, i.e. lack of validated tools (3). Another difficulty relates to the time point for assessing HRQoL. In some studies, HRQoL has within the study group been assessed at differing time points after surgery, or only short-term outcome has been assessed, which does not allow for the exclusion of a possible placebo effect induced by the surgical procedure itself.
The randomized controlled trial by Bollerslev et al. (25), including 191 PHPT patients not fulfilling surgical criteria for the disease, half of which were randomized for surgery and half of which were not, reported no clear improvements in HRQoL 2 years after surgery. This was despite impaired HRQoL, as measured by the SF-36 and the Comprehensive Psychopathological Rating Scale in patients compared to controls at baseline. This study included subjects with very mild PHPT, as none fulfilled the prevailing surgical criteria (25). Several patients initially withdrew from the study, as they could not accept adherence to their randomization group, which could have caused a selection bias (25). In contrast, Ambrogini et al. (26) and Rao et al. (27) reported that reduced baseline HRQoL improved with surgery in randomized trials of 50 and 53 PHPT patients not fulfilling surgical criteria, as assessed by the SF-36. Other studies on mild PHPT reported similar findings (28, 29). Of note, in the present study, total 15D scores significantly improved at 6 and 12 months after surgery compared to baseline in the patients, but were still slightly lower than those observed in controls (Fig. 1). Only longer follow-up can tell whether surgically cured patients eventually will have identical scores compared to controls or not.
The question remains whether the observed improvements in HRQoL are significant enough to expose patients to surgical intervention, and how to assess the neuropsychological symptoms and HRQoL in PHPT in the out-patient setting.
In the present study, independent predictors of impaired HRQoL in the patient group before surgery were whether one experienced possible PHPT-related symptoms and a number of regular medications. It is perhaps not surprising that PHPT patients with a mean age of 65±10 years are ordered quite a large number of medications (mean 4, range 0–11). This might in part reflect an attempt to treat diffuse disease-related symptoms. Melck et al. (30) reported that patients undergoing surgery because of PHPT have a significantly higher mean number of regular pre-operative medications compared to patients referred for thyroidectomy (4 vs 2.8, P<0.001). Number of medications or dosage decreased significantly after surgery in PHPT patients, which was mainly explained by symptom improvement (30). Number of medications has previously been associated with lower HRQoL (31). In the present study, number of medications after surgery was not studied.
Neither serum calcium nor PTH was able to predict the impairment, while serum 25OHD was of borderline significance. A recent study did not find any correlation between serum 25OHD and preoperative HRQoL (20). As seasonal variation can influence HRQoL (32), we investigated whether this could have influenced our results. We divided the patients into three categories according to whether they answered the preoperative 15D questionnaire in October to January, February to May, or June to September (data not shown). The results of the present study were not explained by seasonal variation.
Educational level predicted an improvement in HRQoL after surgery, while baseline 15D score was borderline significant. Previous studies in the general population and in patients with single diseases demonstrate educational level associates with HRQoL (14, 33). In the present study, patients with the lowest baseline 15D score demonstrated the most significant improvements in HRQoL after surgery, and the result was sustained at 1 year. Despite a wide range in serum calcium concentrations in our cohort (range 1.33–2.18 mmol/l), neither serum calcium nor PTH concentrations correlated with improvement of HRQoL. Previous results regarding HRQoL and serum calcium have been discordant (7, 17, 20, 24, 28). In the present study, using the 15D instrument, PHPT patients also demonstrated a distinct profile of impaired HRQoL including the dimensions of vitality, distress, depression, discomfort and symptoms, mental function, sexual activity and excretion. The results indicate that in the future it might be possible to recommend surgery because of HRQoL-related symptoms directly based on a preoperative 15D score and this distinct profile. Further studies with the 15D including larger numbers of PHPT patients with impaired HRQoL but not fulfilling the prevailing surgical criteria are needed.
Although not used in PHPT before, the 15D has been extensively used in other diseases (13). When indirectly compared to patients groups operated on because of coronary artery disease, morbid obesity or arthrosis of the knee, the improvement in HRQoL observed after surgery in PHPT patients is among the largest described (34, 35, 36). Converted to the GAS scale, our results show that 60.5% of PHPT patients did much better and 16.9% slightly better at 6 months after surgery.
The lack of a control group of unoperated PHPT patients can be regarded as a weakness of the study. As 80% fulfilled the criteria for surgery, such a setting seems unethical and patient recruitment would have been difficult. Strengths of the study are its prospective nature, that HRQoL was measured both before and at 6 and 12 months after surgery, the well-validated HRQoL assessment tool, large control population, and assessment of a large number of possible predictors of impaired HRQoL in PHPT.
In conclusion, patients with PHPT demonstrate significantly impaired HRQoL compared to controls, which significantly improves after surgery. The 15D instrument appears to be a good tool for the assessment of HRQoL in PHPT and for evaluating which patients might benefit from surgery.
Author contribution statement
All authors have contributed to the study concept and design, were involved in drafting the manuscript and approved the final manuscript. The preliminary data of this study has been presented as a poster at the Endocrine Society meeting in June 2013 in San Francisco, CA, USA.
Acknowledgements
We wish to thank Mika Väisänen, Endocrinology, Abdominal Center, and Heli Sarpila and Tarja Vainiola from Group Administration of the Helsinki and Uusimaa Hospital District, as well as Viveca Gustavsson, Kirsi Kilpeläinen, Saana Lautala, Pirkko-Liisa Nyman, Anne Villman and Päivi Wirtanen from the Department of Surgery, Helsinki University Central Hospital for their assistance.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
E M Ryhänen received grants from the Helsinki University Central Hospital Research Foundation, Jalmari and Rauha Ahokas Foundation and the Emil Aaltonen Foundation. C Schalin-Jäntti received a grant from the Finska Läkaresällskapet.
References
- 1.Silverberg SJ, Shane E, Jacobs TP, Siris E, Bilezikian JP. A 10-year prospective study of primary hyperparathyroidism with or without parathyroid surgery. New England Journal of Medicine. 1999;341:1249–1255. doi: 10.1056/NEJM199910213411701. [DOI] [PubMed] [Google Scholar]
- 2.Leese PT. The natural history of treated and untreated primary hyperparathyroidism: the parathyroid epidemiology and audit research study. QJM. 2011;104:513–521. doi: 10.1093/qjmed/hcq261. [DOI] [PubMed] [Google Scholar]
- 3.Grant P, Velusamy A. What is the best way of assessing neurocognitive dysfunction in patients with primary hyperparathyroidism? Journal of Clinical Endocrinology and Metabolism. 2014;99:49–55. doi: 10.1210/jc.2013-3115. [DOI] [PubMed] [Google Scholar]
- 4.Bilezikian JP, Brandi ML, Eastell R, Silverberg SJ, Udelsman R, Marcocci C, Potts JT., Jr Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the fourth international workshop. Journal of Clinical Endocrinology and Metabolism. 2014;99:3561–3569. doi: 10.1210/jc.2014-1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pasieka JL, Parsons LL, Demeure MJ, Wilson S, Malycha P, Jones J, Krzywda B. Patient-based surgical outcome tool demonstrating alleviation of symptoms following parathyroidectomy in patients with primary hyperparathyroidism. World Journal of Surgery. 2002;26:942–949. doi: 10.1007/s00268-002-6623-y. [DOI] [PubMed] [Google Scholar]
- 6.Caillard C, Sebag F, Mathonnet M, Gibelin H, Brunaud L, Loudot C, Kraimps JL, Hamy A, Bresler L, Charbonnel B, et al. Prospective evaluation of quality of life (SF-36v2) and nonspecific symptoms before and after cure of primary hyperparathyroidism (1-year follow-up) Surgery. 2007;141:153–159; discussion 159-160. doi: 10.1016/j.surg.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Weber T, Eberle J, Messelhäuser U, Schiffmann L, Nies C, Schabram J, Zielke A, Holzer K, Rottler E, Henne-Bruns D, et al. Parathyroidectomy, elevated depression scores, and suicidal ideation in patients with primary hyperparathyroidism: results of a prospective multicenter study. JAMA Surgery. 2013;148:109–115. doi: 10.1001/2013.jamasurg.316. [DOI] [PubMed] [Google Scholar]
- 8.Silverberg SJ, Clarke BL, Peacock M, Bandeira F, Boutroy S, Cusano NE, Dempster D, Lewiecki EM, Liu JM, Minisola S, et al. Current issues in the presentation of asymptomatic primary hyperparathyroidism: proceedings of the fourth international workshop. Journal of Clinical Endocrinology and Metabolism. 2014;99:3580–3594. doi: 10.1210/jc.2014-1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Annals of Medicine. 2001;33:328–336. doi: 10.3109/07853890109002086. [DOI] [PubMed] [Google Scholar]
- 10.Pelttari H, Sintonen H, Schalin-Jäntti C, Välimäki MJ. Health-related quality of life in long-term follow-up of patients with cured TNM Stage I or II differentiated thyroid carcinoma. Clinical Endocrinology. 2009;70:493–497. doi: 10.1111/j.1365-2265.2008.03366.x. [DOI] [PubMed] [Google Scholar]
- 11.Ritvonen E, Karppinen A, Sintonen H, Vehkavaara S, Kivipelto L, Roine RP, Niemelä M, Schalin-Jäntti C. Normal long-term health-related quality of life can be achieved in patients with functional pituitary adenomas having surgery as primary treatment. Clinical Endocrinology. 2015;82:412–421. doi: 10.1111/cen.12550. [DOI] [PubMed] [Google Scholar]
- 12.Kluger N, Matikainen N, Sintonen H, Ranki A, Roine RP, Schalin-Jäntti C. Impaired health-related quality of life in Addison's disease – impact of replacement therapy, comorbidities and socio-economic factors. Clinical Endocrinology. 2014;81:511–518. doi: 10.1111/cen.12484. [DOI] [PubMed] [Google Scholar]
- 13.Alanne S, Roine RP, Räsänen P, Vainiola T, Sintonen H. Estimating the minimum important change in the 15D scores. Quality of Life Research. 2015;24:599–606. doi: 10.1007/s11136-014-0787-4. [DOI] [PubMed] [Google Scholar]
- 14.Saarni SI, Härkänen T, Sintonen H, Suvisaari J, Koskinen S, Aromaa A, Lönnqvist J. The impact of 29 chronic conditions on health-related quality of life: a general population survey in Finland using 15D and EQ-5D. Quality of Life Research. 2006;15:1403–1414. doi: 10.1007/s11136-006-0020-1. [DOI] [PubMed] [Google Scholar]
- 15.Saarni SI, Luoma M-L & Koskinen S. Elämänlaatu. In Health, Functional Capacity and Welfare in Finland in 2011, pp 159-162. Eds S Koskinen, A Lundqvist & R Ristiluoma, National Institute for Health and Welfare (THL), Report 68/2012. Helsinki 2012.
- 16.Bilezikian JP, Khan AA, Potts JT., Jr Third International Workshop on the Management of Asymptomatic Primary Hyperthyroidism Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. Journal of Clinical Endocrinology and Metabolism. 2009;94:335–339. doi: 10.1210/jc.2008-1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burney RE, Jones KR, Christy B, Thompson NW. Health status improvement after surgical correction of primary hyperparathyroidism in patients with high and low preoperative calcium levels. Surgery. 1999;125:608–614. doi: 10.1016/S0039-6060(99)70224-2. [DOI] [PubMed] [Google Scholar]
- 18.Sheldon DG, Lee FT, Neil NJ, Ryan JA., Jr Surgical treatment of hyperparathyroidism improves health-related quality of life. Archives of Surgery. 2002;137:1022–1026, discussion 1026-1028. doi: 10.1001/archsurg.137.9.1022. [DOI] [PubMed] [Google Scholar]
- 19.Siilin H, Rastad J, Ljunggren O, Lundgren E. Disturbances of calcium homeostasis consistent with mild primary hyperparathyroidism in premenopausal women and associated morbidity. Journal of Clinical Endocrinology and Metabolism. 2008;93:47–53. doi: 10.1210/jc.2007-0600. [DOI] [PubMed] [Google Scholar]
- 20.Åberg V, Norenstedt S, Zedenius J, Sääf M, Nordenström J, Pernow Y, Nilsson I-L. Health-related quality of life after successful surgery for primary hyperparathyroidism: no additive effect from vitamin D supplementation: results of a double-blind randomized study. European Journal of Endocrinology. 2015;172:181–187. doi: 10.1530/EJE-14-0757. [DOI] [PubMed] [Google Scholar]
- 21.Pasieka JL, Parsons L, Jones J. The long-term benefit of parathyroidectomy in primary hyperparathyroidism: a 10-year prospective surgical outcome study. Surgery. 2009;146:1006–1013. doi: 10.1016/j.surg.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 22.Weber T, Keller M, Hense I, Pietsch A, Hinz U, Schilling T, Nawroth P, Klar E, Büchler MW. Effect of parathyroidectomy on quality of life and neuropsychological symptoms in primary hyperparathyroidism. World Journal of Surgery. 2007;31:1202–1209. doi: 10.1007/s00268-007-9006-6. [DOI] [PubMed] [Google Scholar]
- 23.Blanchard C, Mathonnet M, Sebag F, Caillard C, Hamy A, Volteau C, Heymann MF, Wyart V, Drui D, Roy M, et al. Surgery for ‘asymptomatic’ mild primary hyperparathyroidism improves some clinical symptoms postoperatively. European Journal of Endocrinology. 2013;169:665–672. doi: 10.1530/EJE-13-0502. [DOI] [PubMed] [Google Scholar]
- 24.Gopinath P, Sadler GP, Mihai R. Persistent symptomatic improvement in the majority of patients undergoing parathyroidectomy for primary hyperparathyroidism. Langenbeck's Archives of Surgery. 2010;395:941–946. doi: 10.1007/s00423-010-0689-z. [DOI] [PubMed] [Google Scholar]
- 25.Bollerslev J, Jansson S, Mollerup CL, Nordenström J, Lundgren E, Tørring O, Varhaug JE, Baranowski M, Aanderud S, Franco C, et al. Medical observation, compared with parathyroidectomy, for asymptomatic primary hyperparathyroidism: a prospective, randomized trial. Journal of Clinical Endocrinology and Metabolism. 2007;92:1687–1692. doi: 10.1210/jc.2006-1836. [DOI] [PubMed] [Google Scholar]
- 26.Ambrogini E, Cetani F, Cianferotti L, Vignali E, Banti C, Viccica G, Oppo A, Miccoli P, Berti P, Bilezikian JP, et al. Surgery or surveillance for mild asymptomatic primary hyperparathyroidism: a prospective, randomized clinical trial. Journal of Clinical Endocrinology and Metabolism. 2007;92:3114–3121. doi: 10.1210/jc.2007-0219. [DOI] [PubMed] [Google Scholar]
- 27.Rao DS, Phillips ER, Divine GW, Talpos GB. Randomized controlled clinical trial of surgery versus no surgery in patients with mild asymptomatic primary hyperparathyroidism. Journal of Clinical Endocrinology and Metabolism. 2004;89:5415–5422. doi: 10.1210/jc.2004-0028. [DOI] [PubMed] [Google Scholar]
- 28.Blanchard C, Mathonnet M, Sebag F, Caillard C, Kubis C, Drui D, van Nuvel E, Ansquer C, Henry JF, Masson D, et al. Quality of life is modestly improved in older patients with mild primary hyperparathyroidism postoperatively: results of a prospective multicenter study. Annals of Surgical Oncology. 2014;21:3534–3540. doi: 10.1245/s10434-014-3731-5. [DOI] [PubMed] [Google Scholar]
- 29.Talpos GB, Bone HG, III, Kleerekoper M, Phillips ER, Alam M, Honasoge M, Divine GW, Rao DS. Randomized trial of parathyroidectomy in mild asymptomatic primary hyperparathyroidism: patient description and effects on the SF-36 health survey. Surgery. 2000;128:1013–1020, discussion 1020-1021. doi: 10.1067/msy.2000.110844. [DOI] [PubMed] [Google Scholar]
- 30.Melck AL, Armstrong MJ, Stang MT, Carty SE, Yip L. Medication discontinuation after curative surgery for sporadic primary hyperparathyroidism. Surgery. 2010;148:113–1118, discussion 1118-1119. doi: 10.1016/j.surg.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 31.Andersson LB, Marcusson J, Wressle E. Health-related quality of life and activities of daily living in 85-year-olds in Sweden. Health & Social Care in the Community. 2014;22:368–374. doi: 10.1111/hsc.12088. [DOI] [PubMed] [Google Scholar]
- 32.Jia H, Lubetkin EI. Time trends and seasonal patterns of health-related quality of life amoung U.S. adults. Public Health Reports. 2009;124:692–701. doi: 10.1177/003335490912400511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Torvinen S, Färkkilä N, Sintonen H, Saarto T, Roine RP, Taari K. Health-related quality of life in prostate cancer. Acta Oncologica. 2013;52:1094–1101. doi: 10.3109/0284186X.2012.760848. [DOI] [PubMed] [Google Scholar]
- 34.Loponen P, Luther M, Korpilahti K, Wistbacka JO, Huhtala H, Laurikka J, Tarkka MR. HRQoL after coronary artery bypass grafting and percutaneous coronary intervention for stable angina. Scandinavian Cardiovascular Journal. 2009;43:94–99. doi: 10.1080/14017430802395450. [DOI] [PubMed] [Google Scholar]
- 35.Helmiö M, Salminen P, Sintonen H, Ovaska J, Victorzon M. A 5-year prospective quality of life analysis following laparoscopic adjustable gastric banding for morbid obesity. Obesity Surgery. 2011;21:1585–1591. doi: 10.1007/s11695-011-0425-y. [DOI] [PubMed] [Google Scholar]
- 36.Räsänen P, Paavolainen P, Sintonen H, Koivisto AM, Blom M, Ryynänen OP, Roine RP. Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthopaedica. 2007;78:108–115. doi: 10.1080/17453670610013501. [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a