Abstract
Rift Valley fever (RVF) is a mosquito-borne zoonotic disease endemic to the African continent. RVF is characterized by high rate of abortions in ruminants and hemorrhagic fever, encephalitis, or blindness in humans. RVF is caused by the Rift Valley fever virus (RVFV: genus Phlebovirus, family Bunyaviridae). Vaccination is the only known effective strategy to prevent the disease, but there are no licensed RVF vaccines available for humans. A live-attenuated vaccine candidate derived from the wild-type pathogenic Egyptian ZH548 strain, MP-12, has been conditionally licensed for veterinary use in the U.S. MP-12 displays a temperature-sensitive (ts) phenotype and does not replicate at 41°C. The ts mutation limits viral replication at a specific body temperature and may lead to an attenuation of the virus. Here we will review well-characterized ts mutations for RNA viruses, and further discuss the potential in designing novel live-attenuated vaccines for RVF.
Keywords: Rift Valley fever virus, bunyavirus, vaccine, MP-12, temperature sensitivity
Life Cycle for RVFV
Rift Valley fever virus has a tripartite negative-stranded RNA genome designated Small (S)-, Medium (M)-, and Large (L)-segments. The S-segment encodes two open reading frames (ORF) for a nucleoprotein (N) and a non-structural protein (NSs) in an ambi-sense manner. The M-segment encodes a single ORF for a polyprotein precursor. The precursor protein is co-translationally cleaved into four different proteins: Gn, Gc, 78-kD protein, and a non-structural protein (NSm). The L-segment encodes a single ORF for the RNA-dependent RNA polymerase (L) protein.
DC-SIGN, dendritic cell specific intercellular adhesion molecule-3-grabbing non-integrin, is a receptor for RVFV and binds to oligosaccharides attached to virions (Lozach et al., 2011). After viral attachment, viral entry occurs via caveola-mediated endocytosis in a pH-dependent manner (Harmon et al., 2012). Upon uncoating, the L protein, derived from incoming virions begins viral mRNA synthesis (primary transcription). The viral polymerase cleaves a capped host mRNA, near the 5′ terminus, and uses it to prime the synthesis of viral mRNA (cap-snatching) (Schmaljohn and Nichol, 2007). As soon as viral proteins accumulate, the viral RNA genome becomes encapsidated with N protein and forms the ribonucleocapsid (RNP), which is used for RNA genome replication. The viral envelope proteins, Gn and Gc, play a role in viral assembly. Gn encodes a Golgi retention motif (Gerrard and Nichol, 2002), while Gc localizes to the ER, when Gn is not present. The complexes of Gn and Gc localize to the Golgi and trigger the assembly of RNP and L, and then the budding of virions (Piper et al., 2011).
Rift Valley fever virus encodes two non-structural proteins, NSs and NSm. Both proteins are dispensable for viral replication. However, NSs serves as a major virulence factor as it counteracts host antiviral responses. NSs suppresses host general transcription by interrupting the assembly of transcription factor (TF) IIH, which is essential for the function of cellular RNA polymerase I or II (Le May et al., 2004; Kalveram et al., 2011; Kainulainen et al., 2014). RVFV NSs also suppresses the up-regulation of interferon (IFN)-β promoter at a transcriptional level by interacting with cellular transcription repressors (Billecocq et al., 2004; Le May et al., 2008). Furthermore, RVFV NSs promotes the degradation of dsRNA-dependent protein kinase (PKR). PKR is a cellular sensor of dsRNA or the 5′-triphosphate of ssRNA. Upon the binding to RNA, PKR is dimerized. PKR homodimers then undergo autophosphorylation and phosphorylate eukaryotic initiation factor (eIF) 2α, which inhibits the initiation of cellular and viral translation. By promoting the degradation of PKR, RVFV can synthesize viral proteins without inducing significant eIF2α phosphorylation (Habjan et al., 2009; Ikegami et al., 2009). The minor virulence factor, NSm, inhibits the apoptosis of infected cells, yet the lack of NSm expression only moderately affects the RVFV mortality in mice (Won et al., 2006; Terasaki et al., 2013; Kreher et al., 2014). The 78-kD protein and NSm contribute to an efficient dissemination of RVFV in mosquitoes (Crabtree et al., 2012; Kading et al., 2014; Kreher et al., 2014).
RVFV ts Mutants
Rift Valley fever virus is an arbovirus and can replicate in both mosquito and mammalian hosts in nature. RVFV can replicate at 28°C in insect cells (Weingartl et al., 2014), and at 41°C in mammalian cells (Saluzzo and Smith, 1990). Internal body temperatures of RVFV-susceptible hosts are as follows: sheep: 38.3–39.9°C, cattle: 38.0–39.3°C, goats: 38.5–39.7°C, humans: 37°C, mice: 37.5–38.0°C (Talan, 1984; Robertshaw, 2004). RVFV replication initially occurs in the draining lymph nodes, liver, and spleen (Smith et al., 2010; Gommet et al., 2011). It is important to understand the “restrictive temperature” for the ts mutants, because it can allow prediction of viral replication at specific body temperatures in mammalian hosts.
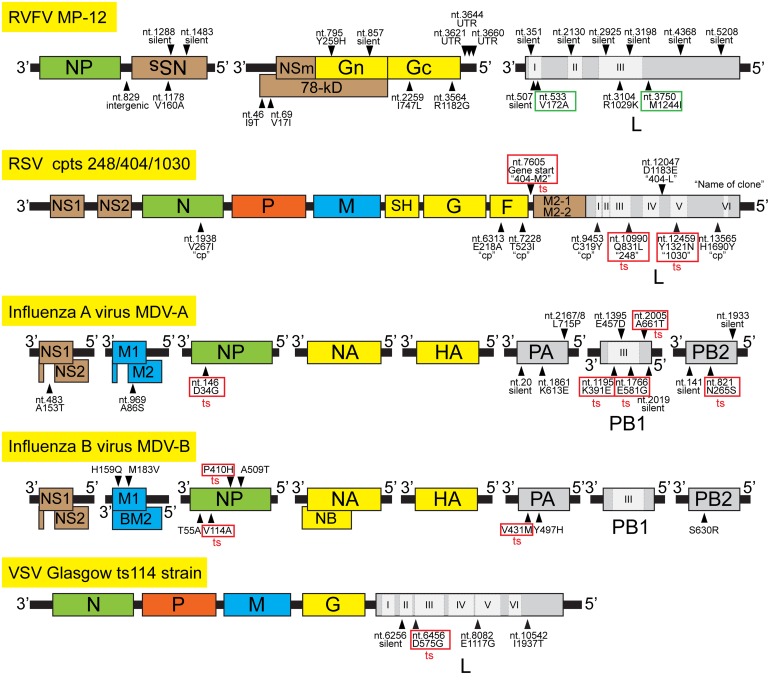
Currently, little is known about ts mutations for RVF vaccine candidates. The RVFV MP-12 strain was developed by 12 serial plaque isolations in human lung diploid (MRC-5) cells in the presence of a chemical mutagen, 5-fluorouracil (Caplen et al., 1985). As a result, a total of 23 mutations are encoded in the genome: four mutations in the S-segment, nine mutations in the M-segment, and 10 mutations in the L-segment (Figure 1). The MP-12 vaccine does not replicate efficiently in vivo, though the S-segment encodes a functional NSs gene. Saluzzo and Smith (1990) previously characterized reassortant RVFV strains between the pathogenic Senegal ArD38661 strain and the MP-12 vaccine strain or the intermediate passage levels of MP-12 (MP-4, MP-6, or MP-9). Their study identified that MP-12 M- and L-segment produce the ts phenotype. Ts mutations on the M-segment were introduced during the MP-12 development (from 7 to 9 passages). On the other hand, ts mutation on the L-segment occurred during the earlier stages of development (the passage 4 or earlier). Since the U533C (V172A) and G3750A (M1244I) mutations were introduced in the L-segment at the passage 3, these two specific mutations may be responsible for the ts phenotype of L-segment (Vialat et al., 1997). However, no further characterization of ts mutations has been reported for MP-12 vaccine.
FIGURE 1.
Mapping of temperature-sensitive (ts) mutations for selected negative-stranded RNA viruses. The genome structures of RVFV MP-12 strain, Respiratory syncytial virus (RSV) cpts 248/404/1030, Influenza A virus (MDV-A), Influenza B virus (MDV-B), and Vesicular stomatitis virus (VSV) ts114 strain are shown. Viral genes are shown in different colors: Nucleocapsid protein (green), phosphoprotein (orange), RNA-dependent RNA polymerase (gray), envelope protein (yellow), matrix proteins (blue), and accessory or non-structural proteins (brown). Conserved six functional regions of RNA-dependent RNA polymerase (RdRp) among non-segmented negative-stranded RNA viruses are shown as I, II, III, IV, V, and VI, and those aligned to RdRp of bunyavirus and influenza virus are also indicated. Location of representative mutations and ts mutations (red square) are indicated by arrowheads. Putative ts mutations in the L-segment of MP-12 are shown in green squares. For RSV mutations, the name of clone, which encodes the mutation, is also shown in quotation.
Currently, the MP-12 vaccine is conditionally licensed in the U.S., and the master seed is available for the production of vaccine lots. A number of safety and efficacy tests were performed for the MP-12 vaccine using pregnant and newborn ruminants (Morrill et al., 1987, 1991, 1997a,b, 2013a; Morrill and Peters, 2003, 2011a,b). To understand the mechanism of attenuation for the MP-12 vaccine, virulent recombinant ZH501 (rZH501) strains encoding the MP-12 S-, M-, or L-segment, or a single mutation of the MP-12 M- or L-segment were analyzed in an outbred CD1 mouse model (1 × 103 pfu, i.p) (Ikegami et al., 2015). The study revealed that an incorporation of a MP-12 S-, M-, or L-segment confers partial attenuation to pathogenic ZH501. Two amino acid changes in Gn (Y259H) and Gc (R1182G) were identified as major attenuation mutations for the M-segment. A combination of Y259H and R1182G only partially attenuates rZH501, while a combination of Y259H, R1182G, plus an L-segment mutation, G3104A (R1029K), could fully attenuate rZH501. Importantly, MP-12 encoding reversion mutations in these three amino acids (H259Y, G1182R, and K1029R) still retained attenuation in mice, indicating that the attenuation of MP-12 vaccine is supported by multiple attenuation mutations, and MP-12 does not revert into virulent phenotype by a few reversion mutations. Further characterization of ts mutations of MP-12 vaccine will help the understanding of the mechanism behind attenuation.
Meanwhile, Rossi and Turell (1988) isolated another ts strain of RVFV. RVFV T1 strain was isolated from female Culex pipiens, which fed on hamsters infected with the pathogenic ZH501 strain. T1 strain displayed a ts phenotype at 41°C, and produced uniformly small plaques. The T1 strain is also highly attenuated in hamsters, and the LD50 is >6.3 × 105 pfu (i.p). On the other hand, the RVFV T46 strain, which was isolated from Aedes taeniorhynchus that fed on ZH501-infected gerbils, also predominantly produced small plaques, but was pathogenic in hamsters, without showing a ts phenotype. As the full genome sequences are available (T1 strain: GenBank Accession DQ375407, DQ380201, and DQ380150, T46 strain: DQ375405, DQ380147, and DQ380199), we analyzed the mutations that occurred in the T1 and T46 strains compared to the parental ZH501 strain. The T1 strain encodes two mutations in the N gene: the G144U (G to V) mutation and a deletion of A at nt.640, which causes a frame-shift and a premature termination of N protein synthesis. T1 strain also encodes a mutation in the 5′-M-untranslated region (C3818U), and two silent mutations in the L-segment (C282U and A2691G). On the other hand, T46 strain encodes only one mutation in the M-segment (U1174A: M to K). The T1 strain has not been further evaluated for vaccine development.
Studies of ts Phenotype in Other RNA Viruses
It is difficult to predict viral attenuation, as a result of mutagenesis, without using animal models. However, a ts phenotype indicates attenuation in vivo and can be screened for using culture cells. Ts phenotypes have been characterized for many viruses (Richman and Murphy, 1979), using different approaches. In Table 1, we have summarized the ts mutants of selected RNA viruses. The ts phenotype depends on host cell types for the Poliovirus Sabin Type2 strain or Dengue virus NS5 gene mutants. For other RNA viruses, the majority of ts mutants were determined by using just one or a few cell types. Thus, it is important to broadly test different cell types to determine a ts phenotype. The location of ts mutations results in a unique ts phenotype. If the viral polymerase encodes a ts mutation, the syntheses of viral genomic RNA or mRNA, or both can be affected at a restricted temperature. If envelope proteins encode a ts mutation, the production of infectious progeny can be inefficient at a restricted temperature. A lack of viral replication or viral RNA synthesis can be an indicator for ts screening when a ts mutation is encoded in the viral polymerase. On the other hand, when the ts mutation is encoded in envelope proteins, the reduction of viral titers may be more remarkable than the decrease in viral RNA accumulation.
Table 1.
Determination of temperature-sensitive (ts) phenotypes for RNA viruses.
| Classification | Species | ts strains | Location of ts mutation | Restrictive Temp for ts (Permissive) | Cell type | Reference |
|---|---|---|---|---|---|---|
| Family Bunyaviridae | ||||||
| Genus Phlebovirus | RVFV | MP-12 | M- and L-segments | 41°C (35°C) | Vero | Rossi and Turell (1988) |
| T1 | Unknown | 41°C (35°C) | Vero | Rossi and Turell (1988) | ||
| UUKV | S23 ts6, 7, 8, 11, 12 | Unknown | 39°C (33°C) | CEF | Gahmberg (1984) | |
| Genus Orthobunyavirus | MAGV | MAG ts8 | M-segment | 38°C (33°C) | BHK-21 | Pollitt et al. (2006) |
| LACV | RFC/25B.5 | Unknown | 39.8°C (37°C) | BHK-21 | Endres et al. (1990) | |
| BUNV | rBUNdelNSs with N mutation | N protein | 38°C (33°C) | VeroE6 | Eifan and Elliott (2009) | |
| SSHV | ts1, 2, 3 | Unknown | 39.5°C (33°C) | BHK-21 | Gentsch and Bishop (1976) | |
| AKV | OBE-1 strain mutants | M- and/or L-segments | 40°C (33°C) | HmLu-1 | Ogawa et al. (2007) | |
| Family Paramixoviridae | ||||||
| Genus Pneumovirus | RSV | rA2 cpts 248/404 | M2 and L | 37°C (32°C) | Hep-2 | Whitehead et al. (1998) |
| rA2 cpts 248/404/1030 | M2 and L | 36°C (32°C) | Hep-2 | Whitehead et al. (1998) | ||
| Genus Respirovirus | HPIV3 | rHPIV3 JS cp45 | L | 38°C (32°C) | LLC-MK2 | Skiadopoulos et al. (1998) |
| HPIV1 | rHPIV1 L:F456L | L | 38°C (32°C) | LLC-MK2 | Newman et al. (2004) | |
| BPIV3 | rBPIV L:I1103V | L | 40°C (37°C) | Vero | Haller et al. (2001) | |
| Family Orthomyxoviridae | ||||||
| Genus Influenza virus A | Flu A | MDV-A | NP, PB1, PB2 | 39°C (33°C) | MDCK | Jin et al. (2003) |
| Genus Influenza virus B | Flu B | MDV-B | M1, NP, PA | 37°C (33°C) | MDCK or PCK | Hoffmann et al. (2005) |
| Family Rhabdoviridae | ||||||
| Genus Vesiculovirus | VSV | Indiana ts11, 13, 114, 22, 33, 41, 45 | L (ts114) | 38.5°C (31°C) | L | Rettenmier et al. (1975) |
| Family Picornaviridae | ||||||
| Genus Enterovirus | PV | Sabin Type3 | VP3 | 40°C (35°C) | Hep-2c | Minor et al. (1989) |
| Sabin Type2 | 5′-UTR | 39.9°C (35°C) | Hep-2c | Macadam et al. (1991) | ||
| 5′-UTR | 38.4°C (35°C) | BGM | ||||
| 5′-UTR | 38.3°C (35°C) | Vero F | ||||
| Sabin Type1 | VP1, VP3, VP4, 3Dpol, 3′-UTR | 40°C (37°C) | HeLa S3 | Bouchard et al. (1995) | ||
| EV A | EV71 (BrCr-ts) | VP1 | 39°C (36°C) | Vero | Arita et al. (2005) | |
| Family Flaviviridae | ||||||
| Genus Flavivirus | DENV | rDEN4 NS5 E645A-K646A | NS5 | 39°C (35°C) | Vero | Hanley et al. (2002) |
| Not ts | HuH-7 | |||||
| WNV | rWNV NS4B C102S | NS4B | 41°C (37°C) | Vero | Wicker et al. (2006) | |
| JEV | M1/311 ts104 | Unknown | 39°C (35°C) | CF | Halle and Zebovitz (1977) | |
| LGV | E5-104 | NS3, E | 37°C (32°C) | Vero | Rumyantsev et al. (2006) | |
RVFV, Rift Valley fever virus; UUKV, Uukuniemi virus; MAGV, Maguari virus; LACV, La Crosse virus; BUNV, Bunyamwera virus; SSHV, Snowshow hare virus; AKV, Akabane virus; RSV, Respiratory syncytial virus; HPIV, Human parainfluenza virus; VSV, Vesicular stomatitis virus; PV, Poliovirus; EV, Enterovirus; DENV, Dengue virus; WNV, West Nile virus; JEV, Japanese encephalitis virus; LGV, Langat virus.
RNA-Dependent RNA Polymerase and ts Phenotypes
Temperature-sensitive mutations have been identified in the RNA-dependent RNA polymerases of many RNA viruses (Table 1). Non-segmented negative-stranded RNA viruses encode six conserved regions (Region I, II, III, IV, V, and VI) in the RNA-dependent RNA polymerase (Rahmeh et al., 2010). The region III (Premotif A, and Motif A, B, C, D, and E) serves in RNA polymerization, and V and VI function in cap addition and cap methylation, respectively. There is also an endonuclease domain at the N-terminus of some of segmented negative-stranded RNA viruses (Reguera et al., 2010). As described above, V172A and M1244I mutations may be involved in the ts phenotype for MP-12 L protein. The V172A mutation is located in Region I, while M1244I is located downstream of Region III Motif E (Muller et al., 1994). Though no studies have been performed for the ts phenotype of RVFV L mutants, mutagenesis of the L protein may identify ts mutations useful for the future rational design of RVF vaccines. Several studies have indicated that ts phenotypes occur from amino acid change(s) in the viral polymerase. Figure 1 illustrates the locations of ts mutations for selected negative-stranded RNA viruses.
The vesicular stomatitis virus (VSV) ts114 mutant encodes three amino changes (D575G, E1117G, and I1937T) in the L-segment compared to the non-ts parental strain. The ts phenotype occurs from D575G, which is located between PreMotif A and Motif A in Region III (Galloway and Wertz, 2009). The ts114 mutant displayed a ts phenotype at 39°C. The ts114 mutant also showed a selected inhibition of viral mRNA synthesis, while maintaining active viral RNA genome replication. However, the selected inhibition of viral transcription only occurred with the combination of all three mutations of ts114, and the single D575G mutant abolished both viral genome replication and transcription at 39°C.
The respiratory syncytial virus (RSV) cold-adapted, temperature-sensitive (cpts) 248/404/1030 is a live-attenuated vaccine strain (Polack and Karron, 2004). It encodes two ts mutations (Q831L and Y1321N) in the L region, in addition to a nucleotide substitution in the M2 transcription start sequence. Q831L is located between Motif C and D in Region III, while Y1321N is located in Region V. In another study, an alanine scan of charged amino acid residues in the RSV L protein was performed to identify ts mutants (Tang et al., 2002). Alanine scanning identified three types of L phenotypes: (1) Abolished L activity, (2) Little change in L activities, and (3) a ts phenotype at 39°C: K157A-D158A (Upstream of Region I), E510A-R511A, R520A, L587A-R588A, R588A-D589A (Region II and upstream) or E1208A-R1209A (Region V).
The live-attenuated FluMist vaccine consists of master donor virus for influenza virus A (MDV-A) and influenza virus B (MDV-B). MDV-A has been developed by serial passages of the wt A/Ann Arbor/6/60 strain in primary chicken kidney tissue culture at successively low temperatures down to 25°C (Jin et al., 2003). MDV-A encodes five ts mutations in NP, PB1, and PB2. A study showed that the MDV-A virus has an impaired synthesis of anti-viral-sense genomic RNA, but not mRNA, at 39°C (Chan et al., 2008). MDV-A also decreases the nuclear export of RNP and the incorporation of the M1 protein into virions at 39°C. Furthermore, MDV-A virions become heterogeneous in size and shape at 39°C. Meanwhile, MDV-B is derived from a cold-adapted B/Ann Arbor/a/66 strain, and encodes ts mutations in the PA and NP segments (Hoffmann et al., 2005).
Temperature-sensitive mutants have been successfully developed as licensed vaccines, or candidate vaccines, in particular, for respiratory diseases: e.g., FluMist (influenza A and B viruses), FluAvert (equine influenza virus) (Paillot et al., 2006), and MEDI-559 (recombinant human RSV A2 cp248/404/1030/ΔSH) (Empey et al., 2010). Most ts mutants have been identified by random mutagenesis. Rational design of ts mutations by reverse genetics will require further understanding of temperature-susceptible domains.
Efficacy of MP-12 Vaccine against Aerosol Challenge of Pathogenic RVFV
A vaccine protection from an exposure via aerosols or powders must be considered in the case of bioterrorism. Little is known about the efficacy of RVF vaccines against aerosol challenge of pathogenic RVFV. Efficacy of the MP-12 vaccine in a pathogenic RVFV challenge via the respiratory route has been studied. Aerosol (~1 × 105 pfu) or intranasal vaccination (~1 × 104 pfu in 1.0 ml volume) of rhesus macaques with MP-12 induced serum neutralizing IgG (Morrill and Peters, 2011a). Intramuscular vaccination of rhesus macaques with MP-12 vaccine also led to neutralizing antibody titers of 1:320 to 1:1,280 (Plaque Reduction Neutralization Test 80: PRNT80), which was maintained for 6 years. The vaccinated rhesus macaques were protected from an aerosol challenge of the pathogenic ZH501 strain (Morrill and Peters, 2011b). These results clearly indicate that the MP-12 vaccine is efficacious for aerosol RVFV challenge, regardless of vaccination routes. Meanwhile, further characterization of viral replications in upper and lower respiratory tract will be important to evaluate the risk of available live-attenuated RVF vaccine candidates: e.g., MP-12, or rMP12-ΔNSm21/384 (Morrill et al., 2013a,b), Clone 13 vaccine (Dungu et al., 2010), or rZH501ΔNSsΔNSm (Bird et al., 2011).
Concluding Remarks
Outbreak of RVF causes decreased animal productivities and viral persistence in mosquito vectors for unknown periods of time, thus significantly impacting the animal industry. In the U.S., the live-attenuated MP-12 vaccine is conditionally licensed, but the vaccine will still require an improvement in terms of safety considering reported side effects: e.g., abortions in pregnant ewes, necrosis in calf liver. Further studies should design additional attenuation mutations rationally, including gene deletion(s) or ts mutations, to fully attenuate the S-, M-, and L-segments, toward the development of highly safe and efficacious RVF vaccines (Grobbelaar et al., 2011; Ikegami, 2012; Lihoradova and Ikegami, 2012).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Ms. Hoai J. Ly and Ms. Inaia Phoenix for their proofreading of this manuscript. This work was partly supported by NIH grant R01 AI08764301, and by the Sealy Center for Vaccine Development at The University of Texas Medical Branch at Galveston.
References
- Abu-Elyazeed R., El-Sharkawy S., Olson J., Botros B., Soliman A., Salib A., et al. (1996). Prevalence of anti-Rift-Valley-fever IgM antibody in abattoir workers in the Nile delta during the 1993 outbreak in Egypt. Bull. World Health Organ. 74 155–158. [PMC free article] [PubMed] [Google Scholar]
- Arita M., Shimizu H., Nagata N., Ami Y., Suzaki Y., Sata T., et al. (2005). Temperature-sensitive mutants of enterovirus 71 show attenuation in cynomolgus monkeys. J. Gen. Virol. 86 1391–1401. 10.1099/vir.0.807840 [DOI] [PubMed] [Google Scholar]
- Billecocq A., Spiegel M., Vialat P., Kohl A., Weber F., Bouloy M., et al. (2004). NSs protein of Rift Valley fever virus blocks interferon production by inhibiting host gene transcription. J. Virol. 78 9798–9806. 10.1128/JVI.78.18.9798-9806.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird B. H., Ksiazek T. G., Nichol S. T., Maclachlan N. J. (2009). Rift Valley fever virus. J. Am. Vet. Med. Assoc. 234 883–893. 10.2460/javma.234.7.883 [DOI] [PubMed] [Google Scholar]
- Bird B. H., Maartens L. H., Campbell S., Erasmus B. J., Erickson B. R., Dodd K. A., et al. (2011). Rift Valley fever virus vaccine lacking the NSs and NSm genes is safe, nonteratogenic, and confers protection from viremia, pyrexia, and abortion following challenge in adult and pregnant sheep. J. Virol. 85 12901–12909. 10.1128/JVI.06046-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botros B., Omar A., Elian K., Mohamed G., Soliman A., Salib A., et al. (2006). Adverse response of non-indigenous cattle of European breeds to live attenuated Smithburn Rift Valley fever vaccine. J. Med. Virol. 78 787–791. 10.1002/jmv.20624 [DOI] [PubMed] [Google Scholar]
- Bouchard M. J., Lam D. H., Racaniello V. R. (1995). Determinants of attenuation and temperature sensitivity in the type 1 poliovirus Sabin vaccine. J. Virol. 69 4972–4978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caplen H., Peters C. J., Bishop D. H. (1985). Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J. Gen. Virol. 66(Pt 10), 2271–2277. 10.1099/0022-1317-66-10-2271 [DOI] [PubMed] [Google Scholar]
- CDC. (2007). Rift Valley fever outbreak–Kenya, November 2006-January 2007. MMWR Morb. Mortal. Wkly. Rep. 56 73–76. [PubMed] [Google Scholar]
- Chambers P. G., Swanepoel R. (1980). Rift valley fever in abattoir workers. Cent. Afr. J. Med. 26 122–126. [PubMed] [Google Scholar]
- Chan W., Zhou H., Kemble G., Jin H. (2008). The cold adapted and temperature sensitive influenza A/Ann Arbor/6/60 virus, the master donor virus for live attenuated influenza vaccines, has multiple defects in replication at the restrictive temperature. Virology 380 304–311. 10.1016/j.virol.2008.07.027 [DOI] [PubMed] [Google Scholar]
- Crabtree M. B., Kent Crockett R. J., Bird B. H., Nichol S. T., Erickson B. R., Biggerstaff B. J., et al. (2012). Infection and transmission of Rift Valley fever viruses lacking the NSs and/or NSm genes in mosquitoes: potential role for NSm in mosquito infection. PLoS Negl. Trop. Dis. 6:e1639 10.1371/journal.pntd.0001639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daubney R., Hudson J. R. (1931). Enzootic hepatitis or Rift Valley fever: an undescribed virus disease of sheep cattle and man from east Africa. J. Pathol. Bacteriol. 34 545–579. 10.1002/path.1700340418 [DOI] [Google Scholar]
- Dungu B., Louw I., Lubisi A., Hunter P., Von Teichman B. F., Bouloy M. (2010). Evaluation of the efficacy and safety of the Rift Valley Fever Clone 13 vaccine in sheep. Vaccine 28 4581–4587. 10.1016/j.vaccine.2010.04.085 [DOI] [PubMed] [Google Scholar]
- Eifan S. A., Elliott R. M. (2009). Mutational analysis of the Bunyamwera Orthobunyavirus nucleocapsid protein gene. J. Virol. 83 11307–11317. 10.1128/JVI.01460-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Empey K. M., Peebles R. S., Jr., Kolls J. K. (2010). Pharmacologic advances in the treatment and prevention of respiratory syncytial virus. Clin. Infect. Dis. 50 1258–1267. 10.1086/651603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endres M. J., Valsamakis A., Gonzalez-Scarano F., Nathanson N. (1990). Neuroattenuated bunyavirus variant: derivation, characterization, and revertant clones. J. Virol. 64 1927–1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gahmberg N. (1984). Characterization of two recombination-complementation groups of Uukuniemi virus temperature-sensitive mutants. J. Gen. Virol. 65(Pt 6), 1079–1090. 10.1099/0022-1317-65-6-1079 [DOI] [PubMed] [Google Scholar]
- Galloway S. E., Wertz G. W. (2009). A temperature sensitive VSV identifies L protein residues that affect transcription but not replication. Virology 388 286–293. 10.1016/j.virol.2009.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentsch J., Bishop D. H. (1976). Recombination and complementation between temperature-sensitive mutants of a Bunyavirus, snowshoe hare virus. J. Virol. 20 351–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerrard S. R., Nichol S. T. (2002). Characterization of the Golgi retention motif of Rift Valley fever virus G(N) glycoprotein. J. Virol. 76 12200–12210. 10.1128/JVI.76.23.12200-12210.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gommet C., Billecocq A., Jouvion G., Hasan M., Zaverucha Do Valle T., Guillemot L., et al. (2011). Tissue tropism and target cells of NSs-deleted rift valley fever virus in live immunodeficient mice. PLoS Negl. Trop. Dis. 5:e1421 10.1371/journal.pntd.0001421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grobbelaar A. A., Weyer J., Leman P. A., Kemp A., Paweska J. T., Swanepoel R. (2011). Molecular epidemiology of Rift Valley fever virus. Emerg. Infect. Dis. 17 2270–2276. 10.3201/eid1712.111035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habjan M., Pichlmair A., Elliott R. M., Overby A. K., Glatter T., Gstaiger M., et al. (2009). NSs protein of rift valley fever virus induces the specific degradation of the double-stranded RNA-dependent protein kinase. J. Virol. 83 4365–4375. 10.1128/JVI.02148-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halle S., Zebovitz E. (1977). A spontaneous temperature sensitive mutant of Japanese encephalitis virus: preliminary characterization. Arch. Virol. 54 165–176. 10.1007/BF01314783 [DOI] [PubMed] [Google Scholar]
- Haller A. A., Macphail M., Mitiku M., Tang R. S. (2001). A single amino acid substitution in the viral polymerase creates a temperature-sensitive and attenuated recombinant bovine parainfluenza virus type 3. Virology 288 342–350. 10.1006/viro.2001.1106 [DOI] [PubMed] [Google Scholar]
- Hanley K. A., Lee J. J., Blaney J. E., Jr., Murphy B. R., Whitehead S. S. (2002). Paired charge-to-alanine mutagenesis of dengue virus type 4 NS5 generates mutants with temperature-sensitive, host range, and mouse attenuation phenotypes. J. Virol. 76 525–531. 10.1128/JVI.76.2.525-531.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmon B., Schudel B. R., Maar D., Kozina C., Ikegami T., Tseng C. T., et al. (2012). Rift Valley fever virus strain MP-12 enters mammalian host cells via caveolae-mediated endocytosis. J. Virol. 86 12954–12970. 10.1128/JVI.02242-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann E., Mahmood K., Chen Z., Yang C. F., Spaete J., Greenberg H. B., et al. (2005). Multiple gene segments control the temperature sensitivity and attenuation phenotypes of ca B/Ann Arbor/1/66. J. Virol. 79 11014–11021. 10.1128/JVI.79.17.11014-11021.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter P., Erasmus B. J., Vorster J. H. (2002). Teratogenicity of a mutagenised Rift Valley fever virus (MVP 12) in sheep. Onderstepoort J. Vet. Res. 69 95–98. [PubMed] [Google Scholar]
- Ikegami T. (2012). Molecular biology and genetic diversity of Rift Valley fever virus. Antiviral Res. 95 293–310. 10.1016/j.antiviral.2012.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T., Hill T. E., Smith J. K., Zhang L., Juelich T. L., Gong B., et al. (2015). Rift Valley fever virus MP-12 vaccine is fully attenuated by a combination of partial attenuations in the S-, M- and L-segments. J. Virol. 89 7262–7276. 10.1128/JVI.00135-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T., Makino S. (2009). Rift valley fever vaccines. Vaccine 27(Suppl. 4), D69–D72. 10.1016/j.vaccine.2009.07.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T., Makino S. (2011). The pathogenesis of rift valley fever. Viruses 3 493–519. 10.3390/v3050493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T., Narayanan K., Won S., Kamitani W., Peters C. J., Makino S. (2009). Rift Valley fever virus NSs protein promotes post-transcriptional downregulation of protein kinase PKR and inhibits eIF2alpha phosphorylation. PLoS Pathog. 5:e1000287 10.1371/journal.ppat.1000287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin H., Lu B., Zhou H., Ma C., Zhao J., Yang C. F., et al. (2003). Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology 306 18–24. 10.1016/S0042-6822(02)00035-1 [DOI] [PubMed] [Google Scholar]
- Kading R. C., Crabtree M. B., Bird B. H., Nichol S. T., Erickson B. R., Horiuchi K., et al. (2014). Deletion of the NSm virulence gene of Rift Valley fever virus inhibits virus replication in and dissemination from the midgut of Aedes aegypti mosquitoes. PLoS Negl. Trop. Dis. 8:e2670 10.1371/journal.pntd.0002670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kainulainen M., Habjan M., Hubel P., Busch L., Lau S., Colinge J., et al. (2014). Virulence factor NSs of rift valley fever virus recruits the F-box protein FBXO3 to degrade subunit p62 of general transcription factor TFIIH. J. Virol. 88 3464–3473. 10.1128/JVI.02914-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalveram B., Lihoradova O., Ikegami T. (2011). NSs protein of rift valley fever virus promotes post-translational downregulation of the TFIIH subunit p62. J. Virol. 85 6234–6243. 10.1128/JVI.02255-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreher F., Tamietti C., Gommet C., Guillemot L., Ermonval M., Failloux A. B., et al. (2014). The Rift Valley fever accessory proteins NSm and P78/NSm-Gn are determinants of virus propagation in vertebrate and invertebrate hosts. Emerg. Microbe Infect. 3 e71. 10.1038/emi.2014.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le May N., Dubaele S., Proietti De Santis L., Billecocq A., Bouloy M., Egly J. M. (2004). TFIIH transcription factor, a target for the Rift Valley hemorrhagic fever virus. Cell 116 541–550. 10.1016/S0092-8674(04)00132-1 [DOI] [PubMed] [Google Scholar]
- Le May N., Mansuroglu Z., Leger P., Josse T., Blot G., Billecocq A., et al. (2008). A SAP30 complex inhibits IFN-beta expression in Rift Valley fever virus infected cells. PLoS Pathog. 4:e13 10.1371/journal.ppat.0040013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lihoradova O., Ikegami T. (2012). Modifying the NSs gene to improve live-attenuated vaccine for Rift Valley fever. Expert Rev. Vaccines 11 1283–1285. 10.1586/erv.12.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozach P. Y., Kuhbacher A., Meier R., Mancini R., Bitto D., Bouloy M., et al. (2011). DC-SIGN as a receptor for phleboviruses. Cell Host Microbe 10 75–88. 10.1016/j.chom.2011.06.007 [DOI] [PubMed] [Google Scholar]
- Macadam A. J., Pollard S. R., Ferguson G., Dunn G., Skuce R., Almond J. W., et al. (1991). The 5’ noncoding region of the type 2 poliovirus vaccine strain contains determinants of attenuation and temperature sensitivity. Virology 181 451–458. 10.1016/0042-6822(91)90877-E [DOI] [PubMed] [Google Scholar]
- Madani T. A., Al-Mazrou Y. Y., Al-Jeffri M. H., Mishkhas A. A., Al-Rabeah A. M., Turkistani A. M., et al. (2003). Rift Valley fever epidemic in Saudi Arabia: epidemiological, clinical, and laboratory characteristics. Clin. Infect. Dis. 37 1084–1092. 10.1086/378747 [DOI] [PubMed] [Google Scholar]
- Miller M. M., Bennett K. E., Drolet B. S., Lindsay R., Mecham J. O., Reeves W. K., et al. (2015). Evaluation of the efficacy, potential for vector transmission, and duration of immunity of MP-12, an attenuated Rift Valley fever virus vaccine candidate, in sheep. Clin. Vaccine Immunol. 10.1128/CVI.00114-15 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minor P. D., Dunn G., Evans D. M., Magrath D. I., John A., Howlett J., et al. (1989). The temperature sensitivity of the Sabin type 3 vaccine strain of poliovirus: molecular and structural effects of a mutation in the capsid protein VP3. J. Gen. Virol. 70(Pt 5), 1117–1123. 10.1099/0022-1317-70-5-1117 [DOI] [PubMed] [Google Scholar]
- Morrill J. C., Carpenter L., Taylor D., Ramsburg H. H., Quance J., Peters C. J. (1991). Further evaluation of a mutagen-attenuated Rift Valley fever vaccine in sheep. Vaccine 9 35–41. 10.1016/0264-410X(91)90314-V [DOI] [PubMed] [Google Scholar]
- Morrill J. C., Jennings G. B., Caplen H., Turell M. J., Johnson A. J., Peters C. J. (1987). Pathogenicity and immunogenicity of a mutagen-attenuated Rift Valley fever virus immunogen in pregnant ewes. Am. J. Vet. Res. 48 1042–1047. [PubMed] [Google Scholar]
- Morrill J. C., Laughlin R. C., Lokugamage N., Pugh R., Sbrana E., Weise W. J., et al. (2013a). Safety and immunogenicity of recombinant Rift Valley fever MP-12 vaccine candidates in sheep. Vaccine 31 559–565. 10.1016/j.vaccine.2012.10.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrill J. C., Laughlin R. C., Lokugamage N., Wu J., Pugh R., Kanani P., et al. (2013b). Immunogenicity of a recombinant Rift Valley fever MP-12-NSm deletion vaccine candidate in calves. Vaccine 31 4988–4994. 10.1016/j.vaccine.2013.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrill J. C., Mebus C. A., Peters C. J. (1997a). Safety and efficacy of a mutagen-attenuated Rift Valley fever virus vaccine in cattle. Am. J. Vet. Res. 58 1104–1109. [PubMed] [Google Scholar]
- Morrill J. C., Mebus C. A., Peters C. J. (1997b). Safety of a mutagen-attenuated Rift Valley fever virus vaccine in fetal and neonatal bovids. Am. J. Vet. Res. 58 1110–1114. [PubMed] [Google Scholar]
- Morrill J. C., Peters C. J. (2003). Pathogenicity and neurovirulence of a mutagen-attenuated Rift Valley fever vaccine in rhesus monkeys. Vaccine 21 2994–3002. 10.1016/S0264-410X(03)00131-2 [DOI] [PubMed] [Google Scholar]
- Morrill J. C., Peters C. J. (2011a). Mucosal immunization of rhesus macaques with Rift Valley Fever MP-12 vaccine. J. Infect. Dis. 204 617–625. 10.1093/infdis/jir354 [DOI] [PubMed] [Google Scholar]
- Morrill J. C., Peters C. J. (2011b). Protection of MP-12-vaccinated rhesus macaques against parenteral and aerosol challenge with virulent rift valley fever virus. J. Infect. Dis. 204 229–236. 10.1093/infdis/jir249 [DOI] [PubMed] [Google Scholar]
- Muller R., Poch O., Delarue M., Bishop D. H., Bouloy M. (1994). Rift Valley fever virus L segment: correction of the sequence and possible functional role of newly identified regions conserved in RNA-dependent polymerases. J. Gen. Virol. 75 1345–1352. 10.1099/0022-1317-75-6-1345 [DOI] [PubMed] [Google Scholar]
- Newman J. T., Riggs J. M., Surman S. R., Mcauliffe J. M., Mulaikal T. A., Collins P. L., et al. (2004). Generation of recombinant human parainfluenza virus type 1 vaccine candidates by importation of temperature-sensitive and attenuating mutations from heterologous paramyxoviruses. J. Virol. 78 2017–2028. 10.1128/JVI.78.4.2017-2028.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogawa Y., Kato K., Tohya Y., Akashi H. (2007). Characterization of temperature-sensitive Akabane virus mutants and their roles in attenuation. Arch. Virol. 152 1679–1686. 10.1007/s00705-007-0991-4 [DOI] [PubMed] [Google Scholar]
- Olaleye O. D., Tomori O., Ladipo M. A., Schmitz H. (1996). Rift Valley fever in Nigeria: infections in humans. Rev. Sci. Tech. 15 923–935. [DOI] [PubMed] [Google Scholar]
- Paillot R., Hannant D., Kydd J. H., Daly J. M. (2006). Vaccination against equine influenza: quid novi? Vaccine 24 4047–4061. 10.1016/j.vaccine.2006.02.030 [DOI] [PubMed] [Google Scholar]
- Pepin M., Bouloy M., Bird B. H., Kemp A., Paweska J. (2010). Rift Valley fever virus (Bunyaviridae: Phlebovirus): an update on pathogenesis, molecular epidemiology, vectors, diagnostics and prevention. Vet. Res. 41 61 10.1051/vetres/2010033v100009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper M. E., Sorenson D. R., Gerrard S. R. (2011). Efficient cellular release of Rift Valley fever virus requires genomic RNA. PLoS ONE 6:e18070 10.1371/journal.pone.0018070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polack F. P., Karron R. A. (2004). The future of respiratory syncytial virus vaccine development. Pediatr. Infect. Dis. J. 23 S65–S73. 10.1097/01.inf.0000108194.71892.95 [DOI] [PubMed] [Google Scholar]
- Pollitt E., Zhao J., Muscat P., Elliott R. M. (2006). Characterization of Maguari orthobunyavirus mutants suggests the nonstructural protein NSm is not essential for growth in tissue culture. Virology 348 224–232. 10.1016/j.virol.2005.12.026 [DOI] [PubMed] [Google Scholar]
- Rahmeh A. A., Schenk A. D., Danek E. I., Kranzusch P. J., Liang B., Walz T., et al. (2010). Molecular architecture of the vesicular stomatitis virus RNA polymerase. Proc. Natl. Acad. Sci. U.S.A. 107 20075–20080. 10.1073/pnas.1013559107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reguera J., Weber F., Cusack S. (2010). Bunyaviridae RNA polymerases (L-protein) have an N-terminal, influenza-like endonuclease domain, essential for viral cap-dependent transcription. PLoS Pathog. 6:e1001101 10.1371/journal.ppat.1001101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rettenmier C. W., Dumont R., Baltimore D. (1975). Screening procedure for complementation-dependent mutants of vesicular stomatitis virus. J. Virol. 15 41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richman D. D., Murphy B. R. (1979). The association of the temperature-sensitive phenotype with viral attenuation in animals and humans: implications for the development and use of live virus vaccines. Rev. Infect. Dis. 1 413–433. 10.1093/clinids/1.3.413 [DOI] [PubMed] [Google Scholar]
- Robertshaw D. (2004). “Temperature regulation and thermal environment,” in Duke’s Physiology of Domestic Animals, 12th Edn, ed. Reece W. O. (Ithaca, NY: Cornell University Press; ). [Google Scholar]
- Rossi C. A., Turell M. J. (1988). Characterization of attenuated strains of Rift Valley fever virus. J. Gen. Virol. 69(Pt 4), 817–823. 10.1099/0022-1317-69-4-817 [DOI] [PubMed] [Google Scholar]
- Rumyantsev A. A., Murphy B. R., Pletnev A. G. (2006). A tick-borne Langat virus mutant that is temperature sensitive and host range restricted in neuroblastoma cells and lacks neuroinvasiveness for immunodeficient mice. J. Virol. 80 1427–1439. 10.1128/JVI.80.3.1427-1439.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saluzzo J. F., Smith J. F. (1990). Use of reassortant viruses to map attenuating and temperature-sensitive mutations of the Rift Valley fever virus MP-12 vaccine. Vaccine 8 369–375. 10.1016/0264-410X(90)90096-5 [DOI] [PubMed] [Google Scholar]
- Schmaljohn C., Nichol S.T. (2007). “Bunyaviridae,” in Fields Virology, 5th Edn, eds Knipe D. M., Howley P. M., Griffin D. E., Lamb R. A., Martin M. A., Roizman B., et al. (Philadelphia, PA: Lippincott, Williams & Wilkins; ), 1741–1789. [Google Scholar]
- Skiadopoulos M. H., Durbin A. P., Tatem J. M., Wu S. L., Paschalis M., Tao T., et al. (1998). Three amino acid substitutions in the L protein of the human parainfluenza virus type 3 cp45 live attenuated vaccine candidate contribute to its temperature-sensitive and attenuation phenotypes. J. Virol. 72 1762–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith D. R., Steele K. E., Shamblin J., Honko A., Johnson J., Reed C., et al. (2010). The pathogenesis of Rift Valley fever virus in the mouse model. Virology 407 256–267. 10.1016/j.virol.2010.08.016 [DOI] [PubMed] [Google Scholar]
- Swanepoel R., Coetzer J. A. W. (2004). “Rift Valley fever,” in Infectious Diseases of Livestock with Special Reference to Southern Africa, 2nd edn, eds Coetzer J. A. W., Tustin R. C. (Cape Town: Oxford University Press; ), 1037–1070. [Google Scholar]
- Talan M. (1984). Body temperature of C57BL/6J mice with age. Exp. Gerontol. 19 25–29. 10.1016/0531-5565(84)90028-7 [DOI] [PubMed] [Google Scholar]
- Tang R. S., Nguyen N., Zhou H., Jin H. (2002). Clustered charge-to-alanine mutagenesis of human respiratory syncytial virus L polymerase generates temperature-sensitive viruses. Virology 302 207–216. 10.1006/viro.2002.1596 [DOI] [PubMed] [Google Scholar]
- Terasaki K., Won S., Makino S. (2013). The C-terminal region of Rift Valley fever virus NSm protein targets the protein to the mitochondrial outer membrane and exerts anti-apoptotic function. J. Virol. 87 676–682. 10.1128/JVI.02192-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vialat P., Muller R., Vu T. H., Prehaud C., Bouloy M. (1997). Mapping of the mutations present in the genome of the Rift Valley fever virus attenuated MP12 strain and their putative role in attenuation. Virus Res. 52 43–50. 10.1016/S0168-1702(97)00097-X [DOI] [PubMed] [Google Scholar]
- Weingartl H. M., Zhang S., Marszal P., Mcgreevy A., Burton L., Wilson W. C. (2014). Rift Valley fever virus incorporates the 78 kDa glycoprotein into virions matured in mosquito C6/36 cells. PLoS ONE 9:e87385 10.1371/journal.pone.0087385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead S. S., Firestone C. Y., Collins P. L., Murphy B. R. (1998). A single nucleotide substitution in the transcription start signal of the M2 gene of respiratory syncytial virus vaccine candidate cpts248/404 is the major determinant of the temperature-sensitive and attenuation phenotypes. Virology 247 232–239. 10.1006/viro.1998.9248 [DOI] [PubMed] [Google Scholar]
- Wicker J. A., Whiteman M. C., Beasley D. W., Davis C. T., Zhang S., Schneider B. S., et al. (2006). A single amino acid substitution in the central portion of the West Nile virus NS4B protein confers a highly attenuated phenotype in mice. Virology 349 245–253. 10.1016/j.virol.2006.03.007 [DOI] [PubMed] [Google Scholar]
- Won S., Ikegami T., Peters C. J., Makino S. (2006). NSm and 78-kilodalton proteins of Rift Valley fever virus are nonessential for viral replication in cell culture. J. Virol. 80 8274–8278. 10.1128/JVI.00476-06 [DOI] [PMC free article] [PubMed] [Google Scholar]