Abstract
Despite decades of research, no efficacious chemotherapy exists for the treatment of prostate cancer. Malignant prostate zinc levels are markedly decreased in all cases of prostate cancer compared to normal/benign prostate. ZIP1 zinc transporter down regulation decreases zinc to prevent its cytotoxic effects. Thus, prostate cancer is a “ZIP1-deficient” malignancy. A zinc ionophore (e.g. Clioquinol) treatment to increase malignant zinc levels is a plausible treatment of prostate cancer. However, skepticism within the clinical/biomedical research community impedes significant progress leading to such a zinc treatment. This report reviews the clinical and experimental background, and presents new experimental data showing Clioquinol suppression of prostate malignancy; which provides strong support for a zinc ionophore treatment for prostate cancer. Evaluation of often-raised opposing issues is presented. These considerations lead to the conclusion that the compelling evidence dictates that a zinc-treatment approach for prostate cancer should be pursued with additional research leading to clinical trials.
Keywords: Prostate cancer, Zinc, ZIP1 transporter, Clioquinol, Zinc ionophore, Chemotherapy, ZIP1-deficent malignancy
Introduction
Despite decades of research involving numerous agents and regimens, an efficacious chemotherapeutic approach for the treatment (and perhaps prevention) of prostate cancer does not exist. This is especially relevant for advanced primary site and metastatic malignancy. Moreover, the hormonal treatment approach has a transient effect that results in the development of untreatable hormone resistant prostate cancer within a few years. Consequently, the search for an effective chemotherapeutic approach to prostate cancer remains a high priority. In addition, the diagnosis of low volume and low grade malignancy is often followed by “active surveillance”; during which no treatment is employed until the appearance of malignant progression.
This report focuses on the plausibility that an appropriate zinc treatment regimen would be efficacious against early and advanced stage prostate cancer. Since we first identified in 1999 [1] that exposure of malignant prostate cells to physiological concentrations of zinc inhibits cell growth, many reports have corroborated and extended the cytotoxic effects of zinc on prostate cells. This relationship becomes most relevant when such experimental studies are coupled with the established clinical condition that zinc levels are always decreased in prostate cancer; and that there is no reported confirmed case of prostate cancer with the high zinc levels that exist in normal prostate. Despite such compelling evidence, a zinc-treatment cytotoxic/tumor suppressor approach for prostate cancer has not reached fruition [2].
The purpose of this review is to consolidate the published clinical and experimental evidence with recent unpublished information and data; which, together, demonstrate the cytotoxic/tumor suppressor effects of zinc and support the plausibility of a zinc treatment approach for prostate cancer. We also describe the issues that are often presented in opposition to the employment of zinc for treatment of prostate cancer. In so doing, the reader will be presented with a focused and consolidated assessment of the current status of information that directly impacts the issue of the feasibility of a zinc-treatment approach for prostate cancer. In our view, the evidence will provide a strengthened basis for support of this concept; which, hopefully, will stimulate much-needed research that could lead to an effective chemotherapy for prostate cancer.
In order to maintain this focused presentation, we have omitted citations and results of many important reports of cytotoxic effects of zinc; which the reader can find in our earlier reviews [2-6].
The status of zinc in normal prostate and prostate cancer
It is important to emphasize that prostate malignancy arises and develops predominantly (~90%) in the peripheral zone, and about 10% in the transition zone. The normal peripheral zone occupies ~70% of the prostate gland, with the central zone and transition zone occupying ~25% and 5%, respectively. The peripheral zone is the major source of prostatic fluid composition. Table 1 shows the high zinc levels that typify the normal peripheral zone and the marked decrease (~75-90%) that characterizes malignant peripheral zone. Correspondingly, prostatic fluid from cancer subjects contain ~75%-90% less zinc than normal prostatic fluid. Normal central zone contains ~75%-85% lower zinc than peripheral zone; and in BPH the central zone zinc levels will increase or decrease depending on the glandular/stroma ratio. For extensive reviews of the zinc status in normal prostate and prostate cancer, we refer the reader to [2-6].
Table 1.
Human prostate zinc levels.
| Human prostate zinc levels | (nmol/g) |
|---|---|
| Peripheral zone- normal | 3,000–4,500 |
| Peripheral zone- cancer | 400–800 |
| Prostatic fluid- normal | 8,000–10,000 |
| Prostatic fluid- cancer | 800–2000 |
| Other soft tissues | 200-500 |
| Blood plasma | 150 |
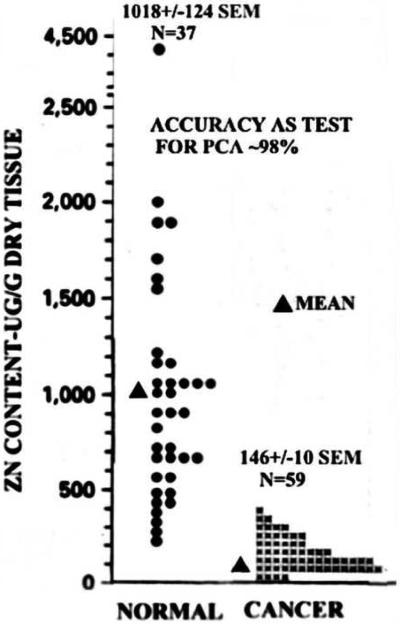
In 1952, Mawson and Fischer [7] first described that zinc was markedly decreased in prostate cancer tissue samples versus normal and hyperplastic tissue samples. Since then, we identified 16 reports, which have confirmed the decrease in zinc in malignant tissue [6]. Compared with normal prostate, the mean decrease in zinc for the 16 reports is ~62%, with a mean standard error of less than 5%. This is an amazing statistical consistency when one considers the variables that exist among these studies; such as different populations, differing stages of cancer, differing composition of tissue components, differing zinc assay methods, and other variables. This is further revealed by figure 1 [8], which shows that all cancers exhibited marked and consistent decreased zinc; and none exhibited a zinc level equivalent to the mean value for normal prostate. Verification is also provided by studies of the in situ zinc levels in prostate tissue sections [9-12], which visibly reveal the major loss of zinc in prostate malignancy as compared to the high zinc levels in the normal/benign prostate acini epithelium (figure 2). It is also important to note that the loss of zinc is evident in highly-differentiated and advancing malignancy; in prostate intraepithelial neoplasia (PIN), and in normal-appearing adjacent cells [11-13]. This demonstrates that the loss of zinc is an early event in the development of prostate cancer, which precedes the histopathological appearance of malignancy. In contrast to this extensive corroborated and consistent zinc relationship, there exists no confirmed or corroborated report of prostate cancer in which zinc is not decreased. These overwhelming data clearly and directly establish that zinc is always decreased in prostate cancer. More importantly the data reveal that prostate cancer that retains the high zinc levels of normal prostate virtually never (or at best rarely) exists. Therefore, it is plausible to apply this relationship to the issue of zinc for the treatment of prostate cancer.
Figure 1.
Zinc levels in normal prostate and prostate cancer. (Modified from [8]).
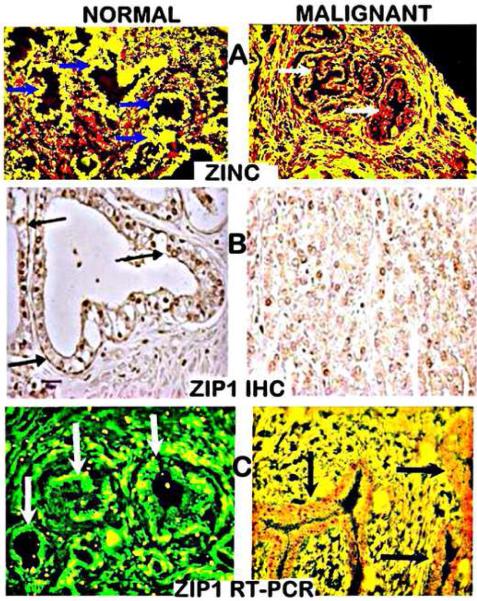
Figure 2.
In situ zinc staining (dithizone; black stain) of human prostate tissue sections. A Gyorkey et al [9]. B. Costello and Franklin (unpublished). PZ: Peripheral Zone.
The cytotoxic implications of zinc in prostate malignancy
The relevant question is “Why is the zinc level markedly decreased in the development and progression of prostate malignancy?” An understanding of zinc relationships in mammalian cells is required (for reviews [14-17]. The survival, proliferation, metabolism, and functional activities of all cells are dependent upon the cell's maintenance of its total zinc concentration and its cellular distribution. All cells possess zinc regulatory mechanisms to achieve and maintain their required normal zinc status. Under conditions, in which the cellular composition of zinc is not maintained within its normal range, cytotoxic effects will result. However, the normal required zinc status (the cellular concentration and distribution) is not the same for all cells.
This is especially relevant to the normal peripheral zone prostate epithelial cells. These cells evolved for the specialized function and capability of accumulating high concentrations of zinc for secretion into prostatic fluid. As such, these secretory epithelial cells exhibit an intracellular concentration of zinc which is ~3-fold higher than most other mammalian cells [17]. Yet, it is obvious that these cells must possess mechanisms that prevent cytotoxic effects of the high cellular zinc level.
There exists substantial and increasing evidence that malignant prostate cells (and other malignant cells) are susceptible to cytotoxicity by the zinc levels that exists in their corresponding normal cells [18,19]. Moreover, there exists abundant experimental evidence since our initial report [1] that the exposure of malignant prostate cells to physiological zinc treatment under conditions that result in increased cellular zinc will result in cytotoxic effects; including inhibition of cell proliferation, induction of apoptosis, and inhibition of cell migration and invasion [3,20]. These relationships provide the answer to the question posed above. In the development of prostate cancer, the high levels of zinc that exist in the normal epithelial cells are cytotoxic in the malignant cells. Therefore, the development of malignancy requires that the zinc levels are decreased to levels that are not cytotoxic to the malignant cells; but that also provide the appropriate zinc status for the proliferation, metabolism and functional malignant activities of the malignant cells. This “metabolic transformation” is initiated during premalignant cell transition to malignancy.
ZIP1: the functional and clinically important zinc uptake transporter in prostate cells
Now the important issue is the mechanism(s) involved in the decrease in zinc during the development of malignant cells. Cells obtain zinc from their extracellular environment; typically from the interstitial fluid derived from blood plasma. The normal range of zinc in plasma is ~12-16 microM of which ~5-7 microM appears in the interstitial fluid in the form of zinc ligands (such as ZnAlbumin, ZnAmino acids, ZnCitrate). These are relatively loosely-bound ZnLigands that constitutes the pool of exchangeable zinc for transport into the cells. It is important to note that the concentration of free Zn++ is negligible (in the pM range) in extracellular and intracellular fluids [14-17]. Many investigators fail to recognize this important relationship, which offen leads to misinformation regarding the zinc transporters and zinc trafficking. The cellular uptake of zinc requires the presence of a plasma membrane zinc uptake transporter, which is provided by the ZIP-family zinc transporters (SLC39A) [4,21-23]. Once within the cell, zinc is distributed between the cytosol and the organelles or is exported out of the cell by ZnT family transporters (Slc30A). Thus, combinations of zinc transporters are involved in the regulation of the total zinc in cells and its distribution within the cell.
Since the total zinc in the cell is first determined by the cell's uptake of zinc from its extracellular fluid, the identification of the cell's functional ZIP-family zinc uptake transporter is important. We first identified in 1999, and subsequently [24-26] that ZIP1 is a plasma membrane transporter in prostate cells that exhibits functional kinetic zinc uptake properties; which has been corroborated by others [23,27,28].
However, the most important clinical revelation occurred in 2005 [11] when we identified the status of ZIP1 and zinc in human prostate tissue sections, using ZIP1 immunohistochemistry, in situ RT-PCR, and in situ zinc staining. The results (figure 3) reveal that ZIP1 gene expression, ZIP1 transporter protein, and cellular zinc are prominent in normal peripheral zone glandular epithelium. In contrast, ZIP1 gene expression is markedly down-regulated, and ZIP1 transporter protein and zinc are depleted in adenocarcinomatous glands. These changes occur early in malignancy and are sustained during its progression in the peripheral zone. It is important to note that ZIP1 transporter is localized at the plasma membrane of the normal acinar epithelium, which is compelling evidence that ZIP1 is an important functional transporter for the uptake and accumulation of zinc by the epithelial cells. Thus the absence of the transporter in the malignant cells along with the concurrent loss of zinc is evidence of ZIP1 down regulation as the cause of decreased zinc levels in malignancy. These observations were confirmed in similar studies of Johnson et al [12]. Moreover, although several reports exists regarding the expression of ZIP and ZnT transporters in prostate, none has been identified to be functional and clinically relevant transporters associated with the concentration of zinc in normal prostate versus malignant prostate tissues. This brings us to the important clinical recognition that human prostate cancer is a “ZIP1-deficient” malignancy.”
Figure 3.
Human normal prostate peripheral zone and prostate cancer tissue sections. A. Shows in situ zinc staining (yellow) in normal epithelium and loss of zinc (red) in early stage malignant acini cells. Arrows point to the acini glandular epithelium B. ZIP1 IHC shows (arrows) plasma membrane localized transporter in normal epithelium and absence in malignancy. C. In situ RT-PCR shows high gene expression (green stain) of ZIP1 in the normal glandular epithelium (arrows) and ZIP1 downregulation in malignancy. (Modified from [11]).
It is also important that we identified that the cell lines (such as PC-3, LNCaP, DU-145), which were derived from malignant prostate tissues, exhibit constitutive expression of ZIP1 under standard culture conditions [24-26]. This is important evidence that the loss of ZIP1 expression in situ in prostate cancer is not due to gene deletion or fatal mutation. Instead, the loss of ZIP1 in prostate cancer likely results from in situ conditions that promote the epigenetic silencing of ZIP1 gene expression; and such conditions are not included under the cell culture conditions. Although ZIP1 transporter is evident in the malignant cell lines, its kinetic zinc transport activity is not necessarily equivalent to the level of zinc uptake that occurs in situ in the normal prostate acinar epithelial cells.
Because of its relevance to this presentation, we must address the issue of identification of functional zinc transporters; especially ZIP-family zinc uptake transporters. One must recognize that the determination of gene expression and its changes does not establish the functionality of the transporter in the cell; nor does the determination of the transporter protein presence and abundance by Western blot analysis of cell or tissue extracts. The localization of the ZIP transporter in the cell (such as immunohistochemistry) is essential, since cellular zinc uptake transporters must be localized at the plasma membrane in relation to the extracellular fluid that provides the zinc for the cellular uptake. In addition, the determination of the kinetic properties of cell uptake by the transporter (e.g. zinc Km value) under physiological conditions is important. In addition, such studies with cell lines must be substantiated by demonstration of the in situ status of the transporter in its tissue.
Because of the widespread misrepresentations and misleading translational conclusions resulting from genetic and proteomic studies, we have described these relationships with examples in our review [29]; which has led to the axiom that applies to metabolic enzymes and transporters, “Genetic transformations and proteomic changes have little relevancy if the genetic/proteomic alterations are not manifested as changes in cell metabolism and function. The absence of identified genetic transformations and proteomic changes does not demonstrate the absence of changes in cell metabolism and function.” The fact is that, despite the innumerable reports of genetic and proteomic identification of these transporters, very few have established the cellular functional capability of the transporter. This applies to the status of zinc transporters in prostate cells, and has had an adverse impact regarding the understanding of zinc effects and the role of zinc transporters.
The zinc/ZIP1 relationship in the TRAMP prostate cancer animal model
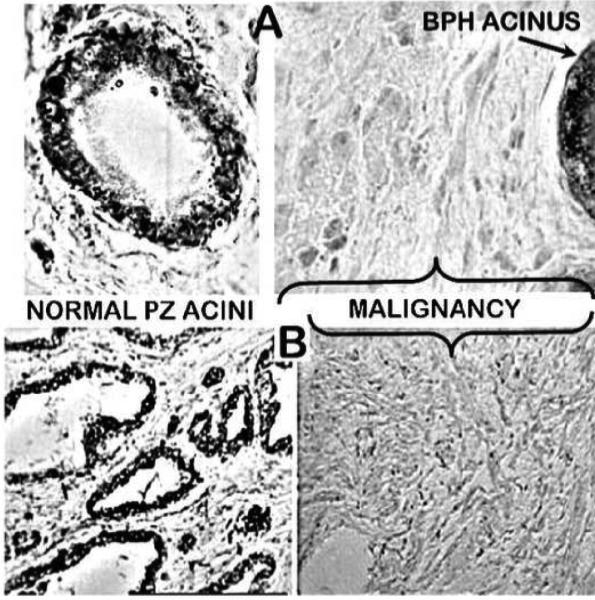
We recently determined the zinc and ZIP1 status in normal and TRAMP mice [30]. TRAMP has been employed as a model for human prostate cancer; but the status of zinc and zinc transporters had not been determined. These studies were conducted in collaboration of Kurhanewicz et al; who established that the clinical citrate relationship in human prostate cancer also exists in TRAMP tumors. Since zinc is responsible for the citrate relationship in human prostate, it was important to determine if the zinc/ZIP1 relationship also exists in TRAMP. As shown in figure 4, the prostate lobe tumors exhibit marked loss of zinc. Also, plasma membrane ZIP1 transporter exists in the normal acini epithelium; and is absent in the TRAMP malignant acini. We also established that the TRAMP C-2 cell line exhibits constitutive ZIP1 transporter; and that exposure of the cells to zinc results in zinc accumulation, inhibition of proliferation and increased apoptosis (figure 5). It is somewhat surprising and extremely relevant to observe the virtually identical zinc/ZIP1 relationship (and also the associated citrate relationship) in both human prostate cancer and TRAMP. It re-enforces the validity that the development of prostate malignancy requires the decrease in zinc in order to prevent zinc cytotoxicity; and that ZIP1 down regulation is essential to prevent the cellular accumulation of high cytotoxic levels of zinc.
Figure 4.
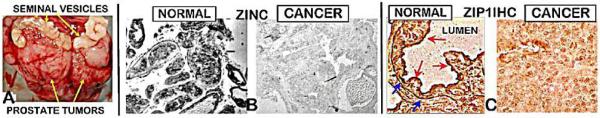
Zinc and ZIP1 status in TRAMP mice prostate tumors. A. Shows prostate tumors in ventral prostate lobes.B. Dithizone staining showing loss of zinc in tumors. C. IHC showing (arrows) prominent basilar and apical membrane staining of the normal glandular epithelium and absence of plasma membrane staining in malignancy. (Modified from [30]).
Figure 5.
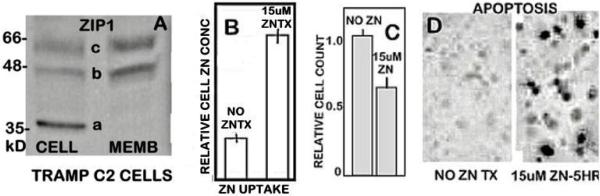
ZIP1 status and zinc effects in TRAMP C-2 cells. A. Western blot shows abundance of ZIP1 transporter in C-2 cell extract and cell membrane fraction. The a-band is free ZIP1; b and c bands are membrane-bound ZIP1.B, C, D show that treatment of C-2 cells with 15 uM zinc results in increased zinc accumulation, which results in decreased proliferation and increased apoptosis (Tunel assay). (Modified from [30]).
Experimental evidence that ZIP1 is the functional transporter for zinc uptake and accumulation
The above clinical identification of the in situ status of ZIP1 and zinc levels does not establish that ZIP1 is responsible for the cellular zinc levels. It is important to determine with corresponding genetic, proteomic and kinetic studies if the uptake, accumulation and effects of zinc under physiological conditions are dependent upon the ZIP1 status in the cells. Our discovery that ZIP1 is an important functional zinc uptake transporter for zinc accumulation and its cytotoxic effects has been based on studies of the effects of altered ZIP1 expression in prostate cells (mainly PC-3 cells) reported in [24-26]. (Figure 6) presents the comparative results obtained with wildtype PC-3 cells (PC3/wt) versus PC-3 cells transfected with ZIP1 expression vector (i.e. ZIP1 upregulated cells, PC3/+ZIP1). As mentioned above, the wildtype PC-3 cells exhibit a constitutive level of ZIP1 transporter, and ZIP1 transfection markedly increased the abundance of ZIP1 transporter. Correspondingly, the PC3/+ZIP1 cells exhibit increased concentration-dependent zinc uptake in the physiological range of 2-10 uM Zn (figure 6B). Notably the Km values demonstrate that ZIP1 is an effective zinc uptake transporter at the exchangeable zinc levels that exists in interstitial fluid. The increased zinc uptake is accompanied by an increase in cellular zinc accumulation, which results in inhibition of cell growth.
Figure 6.
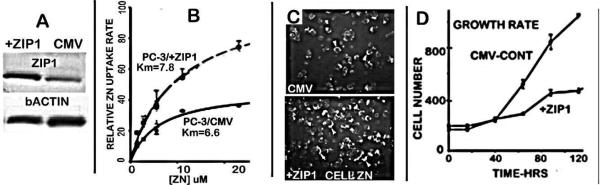
Effects of upregulation of ZIP1 in PC-3 cells. A. shows transfection increased ZIP1 transporter abundance. B, C, D show increased zinc uptake in +ZIP1 cells; which results in increased zinc accumulation and inhibited cell growth. (Compiled and adapted from [25,26]).
Correspondingly, we also developed a PC-3 cell line (PC3/-ZIP1) in which ZIP1 is downregulated to represent the ZIP1-deficient status as exists in the in situ malignant cells in prostate cancer [24-26]. Figure 7 shows the major decrease in expression and transporter protein abundance in the PC3/-ZIP1 cells, which results in decreases in cell uptake and accumulation of zinc. The decrease zinc in the PC3/-ZIP1 cells markedly increases the malignant activities of cell invasion and cell migration. The results demonstrate that other possible ZIP or ZnT plasma membrane zinc transporters, if expressed in the PC-3 cells, do not over-ride the functional role of ZIP1 in the uptake and accumulation of zinc or its cytotoxic effects. We also transfected wild type PC3 cells with mutated ZIP1 [26] and determined the zinc uptake of the PC3/muZIP1 cells. Figure 7F shows that the PC3/muZIP1 cells exhibit minimal zinc uptake, even compared to the PC3/wt cells. This is likely due to competition for the plasma membrane binding sites. The uptake curve is representative of zinc transporter kinetics; so it becomes even more apparent that, in the absence of ZIP1 transport, no other functional zinc uptake transporters are operating in these cells. These results, when coupled with the clinical relationships presented in the preceding section, provide compelling evidence that ZIP1 is the major zinc transporter for the uptake and accumulation of zinc in prostate cells; and that its down regulation is responsible for the decrease in zinc in the malignant cells in prostate cancer.
Figure 7.
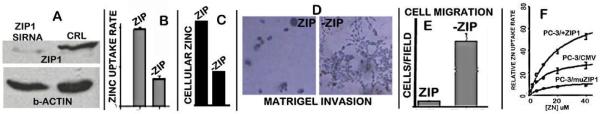
A. Effects of downregulation of ZIP1 in PC-3 cells. A. Shows knockdown of ZIP1 transporter abundance. B, C. Show decrease of zinc uptake and accumulation in PC3/–ZIP cells. D, E. Show increased invasion and migration capability of PC3/–ZIP1 cells. F. Shows the loss of zinc uptake in PC-3 cells that are transfected with mutated ZIP1. (Compiled and adapted from [25,26]).
The above descriptions of the clinical and experimental evidence illustrates the combination of experiments and data, which is required to identify functional zinc transporters in cells; and their involvement in establishing the in situ status of zinc in the cells in their natural tissue environment. This has not been achieved in the vast majority of studies relating to the role of zinc transporters in mammalian tissues. The ZIP1/zinc relationship in prostate is presently the most established functional and clinical zinc transport/zinc status relationship. Genetic/proteomic studies combined with kinetic studies under physiological conditions are required. The identification of the status of zinc and the transporter as exits in the tissue environment cannot be substituted by experimental studies with cells or animal models. Yet, many reports purport to demonstrate and provide conclusions regarding the functional and clinical role of zinc transporters and zinc changes based mainly on genomic and proteomic data; and/or on experimental studies employing unphysiological conditions. We describe these issues in the recent review [29].
The in vivo effects of zinc treatment on tumor growth
The preceding experimental studies demonstrate the cytotoxic effects of zinc under ex vivo conditions. However, it is essential to establish if such effects are manifested in malignant cells under the complex conditions that exist in in vivo tumor growth; and if the effects translate into tumor suppression. We presented the first report in 2003 of in vivo effects of zinc treatment on prostate tumor growth [31]. That study pre-dated the 2005 report [11], in which we identified that ZIP1 is down regulated in prostate cancer malignancy. Until then, we and others assumed that the malignant cell lines, which exhibit constitutive ZIP1 transporter, represented the status that existed in prostate cancer. Consequently, that mouse ectopic xenograff study employed wild type PC-3 cells for tumor development and growth; thereby resulting in “ZIP1 tumors”. The animals were treated with a sustained subcutaneous dosage of zinc sulfate or vehicle (control). The treatment with zinc increased the plasma zinc concentration by ~90%; and resulted in ~50% inhibition (P<0.05) of tumor growth (figure 8). Tumor analyses demonstrated an increase in zinc concentration in the treated tumors, which was accompanied by increased apoptosis, and increased Bax and Bax/BCL2 ratio. These are effects that we established to be direct effects of zinc in malignant prostate cell lines [32,33].
Figure 8.
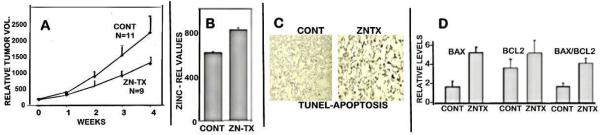
Effect of zinc treatment on wildtype PC-3 tumor growth in the xenograft mouse model. A. Shows inhibition of tumor growth in zinc-treated animals. B. Shows increased tumor zinc in treated animals. C. Shows increased apoptosis (Tunel assay) in zinc treated tumors. D. shows increased Bax and Bax/Bcl2 ratio in treated tumors.(Modified from [31]).
The study demonstrated that zinc treatment of prostate tumors under conditions that permit zinc accumulation in the tumor cells will exhibit its cytotoxic/tumor suppressor effect in vivo. We mistakenly concluded that zinc treatment to increase the plasma concentration of zinc delivered to the tumor site would increase the uptake and accumulation of cytotoxic levels of zinc in the malignant cells; thereby providing an approach for treatment of prostate cancer. We later recognized that the study did not represent the clinical condition in which prostate cancer involves ZIP1-deficient malignancy; and that such an approach would not be plausible. Unfortunately, similar tumor studies by others continue to employ malignant cell lines that do not represent the ZIP1-deficient status that exists in prostate cancer; and this also applies to other cancers (such as pancreatic ductal adenocarcinoma, hepatocellular cancer, and likely other cancers). Such studies lead to questionable and even inappropriate clinical translational application.
The requirements for a zinc treatment approach for ZIP1-deficient prostate cancer
It is now evident that a zinc-treatment approach should address the following issues and conditions:
A treatment regimen that is based on increasing the concentration of zinc delivered to the malignant prostate gland (e.g. increasing the plasma zinc concentration) will not result in zinc uptake and accumulation in the ZIP1-deficient malignant cells; and thereby is not a viable approach for treatment of prostate cancer.
Instead, a vehicle or mechanism is required, which will deliver zinc into the ZIP1-deficient malignant cells; and that the intracellular zinc must be in a mobile, reactive form that manifests the cytotoxic/tumor suppressor effects.
The zinc-treatment regimen must exhibit minimal and acceptable adverse systemic effects and contraindications.
With this in mind, we directed our attention and studies to identify a zinc-treatment approach that would meet these conditions; and would validate the underlying premise.
Evidence that a zinc ionophore (Clioquinol) approach will deliver zinc into ZIP1-deficient prostate cells resulting in cytotoxic effects; and will inhibit the growth of ectopic ZIP1-deficient tumors in mice
For recent studies we elected to employ a cell-permeable zinc ionophore as the approach to deliver zinc into the ZIP1-deficient malignant cells in a mobile reactive form, so as to manifest the cytotoxic effects/tumor-suppressor effects of increased cellular zinc accumulation. Clioquinol (5-chloro-7-iodo-8-quinolinol) is an ionophore with a zinc-binding formation constant logKf~8, which should be an exchangeable reactive ZnLigand. It has been shown [34-37], to deliver zinc and induce cytotoxic effects in some malignant cells. However, none of the studies has demonstrated this in malignant cells that are deficient in their functional zinc uptake transporter, as exists in situ in the respective cancers.
In the following preliminary studies (unpublished) we employed our PC3/-ZIP1 cell line (figure 7) to determine if clioquinol would increase the zinc uptake and accumulation; and if so, would it result in inhibition of proliferation. Figure 9 shows the increased accumulation of zinc in response to clioquinol and physiological concentrations of zinc, which results in the inhibition of cell proliferation. Moreover, clioquinol in the presence of zinc results in phosphorylation of JNK which is a pathway for apoptosis; whereas neither zinc alone nor clioquinol alone has any effect. It becomes evident that the zinc ionophore approach as represented by clioquinol achieves the requirement of delivery of zinc into ZIP1-deficient cells in the form of exchangeable reactive zinc.
Figure 9.
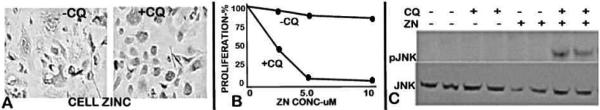
Effects of clioquinol on ZIP1-deficient PC-3 cells. A. Shows increased zinc accumulation in the presence of clioquinol. B. Shows inhibition of cell proliferation in the presence of CQ+Zn. C. Shows increased phosphorylation of JNK in the presence of CQ+Zn. Cells were exposed to 5 uM CQ treatment for 16 hours. A and C treated with 5 uM Zn.
We then determined if clioquinol would suppress ZIP1-deficient tumor growth under the complex conditions that exist in the in vivo environment. No reported studies exist using this ZIP1-deficient tumor model to represent human prostate cancer. For this, we employed PC3/-ZIP1 cells to develop ZIP1-deficent tumors in the ectopic xenograff animals and determined the effects of clioquinol treatment versus vehicle-treatment on tumor growth. (Unpublished information). The animals received 30 mg clioquinol/Kg or vehicle (IP administration) every other day for 5 weeks affer initial tumor development. This dosage regimen approximates the non-toxic dosage in humans [38,39] and in mice [34]. Figure 10 shows that, over the treatment period of 5 weeks, clioquinol suppressed tumor growth by ~85%; and similarly decreased the weight of the tumors by ~78%. These effects are apparent from the photographs that show the marked decrease in size of the tumors in the clioquinol-treated animals compared to the untreated control animals. Zinquin determination of tumor zinc levels showed 9.5 ± 0. 4 and 15.4 ± 3.7 ng/mg tissue for the control versus clioquinol-treated animals; which represents a 62% zinc increase in the clioquinol-treated tumors. Since Zinquin has a zinc-binding affinity of logKf~10, the increase is in the exchangeable reactive pool of zinc, which is responsible for the cellular effects of zinc. We also performed Western blot analysis of the tumors, which revealed that ZIP1 transporter was negligible in the control and clioquinol-treated tumors (figure 10). This demonstrated that the ZIP1-deficient status is retained during tumor development and growth in the animals.
Figure 10.

Effects of clioquinol treatment on growth of ZIP1-deficient tumors. A. Picture showing the size of tumors in the mice following five weeks of clioquinol treatment compared to untreated animals. B. Shows the comparative rates of tumor growth over the five week treatment period. C. Shows the average weights of the resected tumors from the treated versus untreated animals. D. Western blots of ZIP1 transporter abundance in the PC-3/-ZIP1 cells inoculated into the mice; and shows the negligible ZIP1 transporter in the tumors.
The results of these initial experiments coupled with the relationships presented in the preceding sections present compelling experimental and clinical evidence that a zinc-treatment regimen, which permits in situ malignant cell zinc uptake and accumulation can provide an efficacious approach for prostate cancer.
Assessment of issues that give rise to opposition of zinc chemotherapy for prostate cancer
Despite the wealth of supporting clinical and experimental evidence, there exists considerable skepticism in the plausibility of zinc treatment for prostate cancer. Such resistance arises from a number of issues; the validity of which needs to be addressed. Based on the available literature and on our personal experiences, the following are among the most prevalent issues.
The unfounded and adverse impact of epidemiology reports on the issue of zinc treatment and prostate cancer
We believe this to be the most influential detracting issue; which requires special attention and assessment in this review. The prevailing view of most prostate clinicians and biomedical investigators is that zinc consumption poses an increased risk of promoting prostate cancer. This view arose from an NIH-Harvard collaborative epidemiology report in 2003 [40], in which Leitzmann et al concluded that “we found that excessively high supplemental zinc intake was associated with an increased risk of advanced prostate cancer. “The immediate and continued notoriety given to this report is evident from the widespread pronouncements in various news media and notices from health institutions; such as: Health Day News (July 2, 2003) “Men who overdose on zinc supplements more than double their risk of prostate cancer, a government study finds”; the Washington Post (July 1, 2003), “Study Links Zinc, Prostate Cancer-Men who take too much zinc may be raising their prostate cancer risk, U.S. researchers said yesterday”; the Mayo Clinic Health Letter (May, 2004) “Large doses of zinc may increase risk of prostate cancer.”
Prior to 2003, the various epidemiology reports had concluded that zinc intake (diet and supplement) either protects against prostate cancer; or promotes prostate cancer; or has no effect on prostate cancer [41,42]. Despite the fact that the Leitzmann report and conclusion had not been corroborated by any other epidemiology studies, and is not supported by the clinical status of zinc in prostate cancer; contemporary clinicians and investigators continue to cite the Leitzmann et al study as evidence that zinc treatment will exacerbate the development and progression of prostate cancer. Most importantly, two recent major epidemiology studies reached the following conclusion: “In this prospective cohort, long-term supplemental zinc intake was associated with reduced risk of clinically relevant advanced disease” [43] and “These results suggest that high dietary intake of zinc is associated with lower prostate cancer-specific mortality affer diagnosis, particularly in men with localized disease” [44]. In addition, we have published rebuttals and reviews [41,42,45,46]. which describe the questionable results and conclusions inherent in the epidemiology study. Particularly important is our extensive review [46] that analyzes in detail the shortcomings of the Leitzmann et al data and conclusions. In addition, others also raised issue with the Leitzmann et al study and conclusions [47,48].
Relative to the issue of zinc treatment for prostate cancer, the epidemiology conclusions should not be weighed against the overwhelming clinical, physiological, and experimental evidence. If anything, the current assessment of the epidemiology reports would be supportive of a zinc treatment approach for prostate cancer. Unfortunately, we are confronted with the enigma expressed by outstanding epidemiologists [49]. Dr. Trichopoulos who stated that epidemiology studies “studies will inevitably generate false positive and false negative results with disturbing frequency... when people do take us seriously, we may unintentionally do more harm than good” and Dr. Walker who also stated “The first one or two papers about a suspected association spring into the general public consciousness in a way that does not happen in any other field of scientific endeavor. And once a possible link is in the public eye, it can be virtually impossible to discredit”. Affer twelve years of a dominant epidemiological misrepresentation of the zinc relationship in prostate cancer, this dilemma still confronts us.
Concerns regarding the potential toxic effects of zinc treatment in humans
The view of many, and probably most, clinical and biomedical investigators regarding zinc toxicity is not in accord with the physiological and pathophysiological relationships of zinc. It is a mistaken presumption and expectation that a treatment regimen based on increasing the cellular zinc levels that are cytotoxic to malignant cells would also be cytotoxic in normal cells; and thereby would have pathophysiological consequences. There exists little, if any, substantial evidence in support of such a committed outcome from zinc treatment.
The eminent zinc biochemist/physiologist, Dr. Vallee, in the hallmark comprehensive reviews of the physiology and biochemistry of zinc [14,15] states “Clearly, a metal that is known to be essential to the inheritance of the genetic endowment and the induction of development, growth, and differentiation could not easily be intended to be deleterious to the perpetuation and evolution of the species. Instead, one would expect zinc to be regulated carefully to ensure the preservation and continuity of life. In fact, zinc is the only pre-, post-, and transitional element that has proven to be essentially nontoxic.” Several citations and examples are presented as evidence that zinc toxicity in humans rarely occurs, and is only evident under extreme conditions accompanied by exacerbating systemic pathophysiology.
The reviews also present extensive evidence exists that zinc deficiency is the more common pathophysiological consequence. Moreover, it is demonstrated that some zinc-deficient disorders are remedied by the administration of supplemental zinc. In relation to prostate cancer, it is notable that most reports (such as [50-55]) indicate a correlation between a low-zinc status (such as hypozincemia) and prostate cancer, although other reports [56,57] conclude that plasma zinc changes are not associated with prostate cancer. In an individual with premalignant or undetected early stage malignancy, a zinc-deficient condition is likely to promote the development of prostate cancer.
It becomes evident that normal and also malignant mammalian cells evolved with mechanisms and conditions that provide and maintain a zinc concentration and status as required for their survival, proliferation, metabolism, and functional activities. However, the required concentration and status of zinc is different for the malignant cells compared to their corresponding normal cells; and the zinc levels that exist in the normal cells can be cytotoxic in malignant cells. Therefore, the malignant cells evolved with mechanisms that prevent the accumulation of the cytotoxic high zinc levels; and this event occurs during the oncogenic transformation of the normal cells to malignant cells [2,58]. Under such relationships, a zinc treatment regimen that increases the cellular zinc to a cytotoxic level in the malignant cells can be achieved in the absence of cytotoxic effects in the normal cells; and in the absence of systemic pathophysiological consequences.
The issue of zinc ionophore toxicity as represented by clioquinol
It is not the intent of this review to promote the use of clioquinol as a preferable agent for zinc treatment of prostate cancer. We employed clioquinol in our studies to demonstrate the plausibility of a zinc ionophore approach for increasing zinc uptake, accumulation and cytotoxicity in ZIP1-deficent malignant cells and tumors as exists in prostate cancer. Clioquinol had been employed as a zinc treatment for diarrhea and skin infections, and in clinical trials for the treatment of Alzheimer diseases. At effective therapeutic concentrations, clioquinol exhibits minimal or no adverse effects [38,39]. In animal studies clioquinol has been shown to exhibit anticancer effects with minimal side effects [34,35]. However, clioquinol was withdrawn from the market due to an incident of purported potential toxic effects of subacute myelo-optic neuropathy, despite the evidence of its relatively safe use in conditions described above. Rather than imposing this issue as a deterrent to the potential use of a zinc ionophore approach for prostate cancer, it would seem to be more prudent to be supportive of the necessary studies to validate the zinc-treatment approach. If studies are successful, the issue of contraindications at an effective therapeutic regimen in humans should be addressed.
The clinical application of zinc treatment for prostate cancer
The xenograff model reflects the effects of zinc treatment on primary site tumor growth of established human malignant cells. The model does not permit the determination of zinc effects on the development of malignancy, nor generally on metastases and metastatic cells; the latter being the major untreatable condition leading to death. Studies of such effects are essential to the practicality of the application of zinc treatment for prostate cancer. As described above, clinical evidence exists for the expectation that the cytotoxic effects of zinc will be manifested during the initiation and early development of prostate malignancy, Our studies [11] and those of Johnson et al [12] have shown that the down regulation of ZIP1 and the decrease in zinc are evident in PIN and in well-differentiated malignancy. Cortesi et al [13] employing in situ zinc levels in peripheral zone similarly described that “the zinc depletion occurs not only in the cancerous tissue segments but also... in the non-cancer components surrounding the lesion.” Horn et al [59] with in situ MRS imaging showed that PIN lesions exhibit decreased citrate, which would be due to loss of zinc. Such clinical observations are consistent with our view that the events of down regulation of ZIP1 and loss of zinc occur in pre-malignancy, and prior to the histopathological identification of malignancy. Such relationships make it plausible to suggest that the zinc treatment regimen described above could prevent the development of malignancy in at-risk individuals, such as individuals with elevated PSA and no histopathological confirmation of malignancy. Since the zinc treatment would likely be somewhat innocuous, its employment to abort potential early development and progression of malignancy would be advantageous over the absence of any mitigating interventions in an “active surveillance” protocol.
Regarding metastatic and advanced hormone-independent prostate cancer, the determination of the zinc status has not been established. However, some existing evidence is indicative of the likelihood that the loss of zinc persists in the advanced stages of malignancy. Heijmink et al [60] showed with magnetic resonance spectroscopy that the citrate is absent in lymph node metastasis; and this would be indicative of decreased zinc. Kim et al [61] reported that promotion of prostate cancer invasion and metastasis occurs by decreasing intracellular zinc levels. Compelling evidence is also provided by identification of the loss of citrate, zinc, and ZIP1 in the metastatic lymph nodes in TRAMP. Based on such evidence, it is reasonable to expect that clioquinol treatment will increase zinc accumulation and cytotoxic effects in metastatic cells.
Conclusions
Studies of cytotoxic/tumor suppressor effects of zinc in support of a potential zinc treatment approach for prostate cancer is scattered among many published reports. This places a burden on clinical and biomedical researchers in extracting and assimilating the existing supporting evidence for zinc chemotherapy. This is compounded by the complexity of zinc and zinc transport physiology, biochemistry, and molecular biology; which, if not well understood, offen leads to misinterpretation and misapplication of zinc relationships in mammalian systems. This comprehensive report provides the reader with some of the most relevant background and data of published reports, along with important recent unpublished information, as evidence in support of a zinc treatment approach for prostate cancer. Over the ~15 years since elevated cellular zinc levels were first identified as an inhibitor of malignant cell growth, many reports have extended and corroborated the cytotoxic effects of zinc. Animal model studies have confirmed that zinc treatment that results in increased zinc accumulation in malignant cells inhibits tumor growth; thereby identifying the potential of zinc as a tumor-suppressor agent,
However, the success of a zinc treatment regimen must consider the important identification of human prostate cancer as a ZIP1-deficient malignancy; which requires a mechanism or factor that will facilitate zinc uptake into the cell and its availability as exchangeable reactive zinc. In vitro studies demonstrate that the zinc ionophore, clioquinol, facilitates zinc uptake and accumulation which exhibits cytotoxic effects in ZIP1-deficient malignant cells. In support of this, the zinc ionophore approach with clioquinol treatment has been shown to markedly suppress the growth of ZIP1-deficient tumors in the xenograff animal model.
Thus, the collective experimental and clinical evidence provides compelling support for the plausibility of an appropriate zinc treatment regimen for prostate cancer. Such an approach could be efficacious for primary site malignancy and for metastatic malignancy; and also for prevention of development of malignancy in at-risk individuals. We hope that the relationships and data provided in this presentation will lead to additional supporting experimental studies and to clinical trials of a zinc treatment regimen for prostate cancer. We look forward to responses to this presentation; especially clinical and scientifically-credible comments that might be in support or in opposition to the plausibility of a zinc-treatment approach for prostate cancer.
Acknowledgement
The studies of LC Costello and RB Franklin cited herein were supported by NIH grants CA79903, DK076783 and DK42839.
Footnotes
Citation: Costello LC, Franklin RB, Zou J, Naslund MJ (2015) Evidence that Human Prostate Cancer is a ZIP1-Deficient Malignancy that could be Effectively Treated with a Zinc Ionophore (Clioquinol) Approach. Chemotherapy 4: 152. doi:10.4172/2167-7700.1000152
References
- 1.Liang JY, Liu YY, Zou J, Franklin RB, Costello LC, et al. Inhibitory effect of zinc on human prostatic carcinoma cell growth. Prostate. 1999;40:200–207. doi: 10.1002/(sici)1097-0045(19990801)40:3<200::aid-pros8>3.0.co;2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costello LC, Franklin RB. Cytotoxic/tumor suppressor role of zinc for the treatment of cancer: an enigma and an opportunity. Expert Rev Anticancer Ther. 2012;12:121–128. doi: 10.1586/era.11.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Franklin RB, Costello LC. The important role of the apoptotic effects of zinc in the development of cancers. J Cell Biochem. 2009;106:750–757. doi: 10.1002/jcb.22049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Franklin RB, Milon B, Feng P, Costello LC. Zinc and zinc transporter in normal prostate function and the pathogenesis of prostate cancer. Front Biosci. 2005;10:2230–2239. doi: 10.2741/1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costello LC, Franklin RB. The clinical relevance of the metabolism of prostate cancer; zinc and tumor suppression: connecting the dots. Mol Cancer. 2006;5:17. doi: 10.1186/1476-4598-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Costello LC, Franklin RB. Zinc is decreased in prostate cancer: an established relationship of prostate cancer! J Biol Inorg Chem. 2011;16:3–8. doi: 10.1007/s00775-010-0736-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MAWSON CA, FISCHER MI. The occurrence of zinc in the human prostate gland. Can J Med Sci. 1952;30:336–339. doi: 10.1139/cjms52-043. [DOI] [PubMed] [Google Scholar]
- 8.Zaichick VYe, Sviridova TV, Zaichick SV. Zinc in the human prostate gland: normal, hyperplastic and cancerous. Int Urol Nephrol. 1997;29:565–574. doi: 10.1007/BF02552202. [DOI] [PubMed] [Google Scholar]
- 9.Györkey F, Min KW, Huff JA, Györkey P. Zinc and magnesium in human prostate gland: normal, hyperplastic, and neoplastic. Cancer Res. 1967;27:1348–1353. [PubMed] [Google Scholar]
- 10.SCHRODT GR, HALL T, WHITMORE WF., Jr THE CONCENTRATION OF ZINC IN DISEASED HUMAN PROSTATE GLANDS. Cancer. 1964;17:1555–1566. doi: 10.1002/1097-0142(196412)17:12<1555::aid-cncr2820171207>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 11.Franklin RB, Feng P, Milon B, Desouki MM, Singh KK, et al. hZIP1 zinc uptake transporter down regulation and zinc depletion in prostate cancer. Mol Cancer. 2005;4:32. doi: 10.1186/1476-4598-4-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson LA, Kanak MA, Kajdacsy-Balla A, Pestaner JP, Bagasra O. Differential zinc accumulation and expression of human zinc transporter 1 (hZIP1) in prostate glands. Methods. 2010;52:316–321. doi: 10.1016/j.ymeth.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Cortesi M, Fridman E, Volkov A, Shilstein SSh, Chechik R, et al. Clinical assessment of the cancer diagnostic value of prostatic zinc: a comprehensive needle-biopsy study. Prostate. 2008;68:994–1006. doi: 10.1002/pros.20766. [DOI] [PubMed] [Google Scholar]
- 14.VALLEE BL. Biochemistry, physiology and pathology of zinc. Physiol Rev. 1959;39:443–490. doi: 10.1152/physrev.1959.39.3.443. [DOI] [PubMed] [Google Scholar]
- 15.Vallee BL, Falchuk KH. The biochemical basis of zinc physiology. Physiol Rev. 1993;73:79–118. doi: 10.1152/physrev.1993.73.1.79. [DOI] [PubMed] [Google Scholar]
- 16.Maret W, Li Y. Coordination dynamics of zinc in proteins. Chem Rev. 2009;109:4682–4707. doi: 10.1021/cr800556u. [DOI] [PubMed] [Google Scholar]
- 17.Costello LC, Fenselau CC, Franklin RB. Evidence for operation of the direct zinc ligand exchange mechanism for trafficking, transport, and reactivity of zinc in mammalian cells. J Inorg Biochem. 2011;105:589–599. doi: 10.1016/j.jinorgbio.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sliwinski T, Czechowska A, Kolodziejczak M, Jajte J, Wisniewska-Jarosinska M, et al. Zinc salts differentially modulate DNA damage in normal and cancer cells. Cell Biol Int. 2009;33:542–547. doi: 10.1016/j.cellbi.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 19.Park SE, Park JW, Cho YS, Ryu JH, Paick JS, et al. HIF-1alpha promotes survival of prostate cells at a high zinc environment. Prostate. 2007;67:1514–1523. doi: 10.1002/pros.20641. [DOI] [PubMed] [Google Scholar]
- 20.Franklin RB, Costello LC. Zinc as an anti-tumor agent in prostate cancer and in other cancers. Arch Biochem Biophys. 2007;463:211–217. doi: 10.1016/j.abb.2007.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lichten LA, Cousins RJ. Mammalian zinc transporters: nutritional and physiologic regulation. Annu Rev Nutr. 2009;29:153–176. doi: 10.1146/annurev-nutr-033009-083312. [DOI] [PubMed] [Google Scholar]
- 22.Eide DJ. Zinc transporters and the cellular trafficking of zinc. Biochim Biophys Acta. 2006;1763:711–722. doi: 10.1016/j.bbamcr.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 23.Franz MC, Anderle P, Bürzle M, Suzuki Y, Freeman MR, et al. Zinc transporters in prostate cancer. Mol Aspects Med. 2013;34:735–741. doi: 10.1016/j.mam.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Costello LC, Liu Y, Zou J, Franklin RB. Evidence for a zinc uptake transporter in human prostate cancer cells which is regulated by prolactin and testosterone. J Biol Chem. 1999;274:17499–17504. doi: 10.1074/jbc.274.25.17499. [DOI] [PubMed] [Google Scholar]
- 25.Franklin RB, Ma J, Zou J, Guan Z, Kukoyi BI, et al. Human ZIP1 is a major zinc uptake transporter for the accumulation of zinc in prostate cells. J Inorg Biochem. 2003;96:435–442. doi: 10.1016/s0162-0134(03)00249-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Milon B, Wu Q, Zou J, Costello LC, Franklin RB. Histidine residues in the region between transmembrane domains III and IV of hZip1 are required for zinc transport across the plasma membrane in PC-3 cells. Biochim Biophys Acta. 2006;1758:1696–1701. doi: 10.1016/j.bbamem.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 27.Kolenko V, Teper E, Kutikov A, Uzzo R. Zinc and zinc transporters in prostate carcinogenesis. Nat Rev Urol. 2013;10:219–226. doi: 10.1038/nrurol.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang L, Kirschke CP, Zhang Y. Decreased intracellular zinc in human tumorigenic prostate epithelial cells: a possible role in prostate cancer progression. Cancer Cell Int. 2006;6:10. doi: 10.1186/1475-2867-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Costello LC, Franklin RB. Integration of molecular genetics and proteomics with cell metabolism: how to proceed; how not to proceed! Gene. 2011;486:88–93. doi: 10.1016/j.gene.2011.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Costello LC, Franklin RB, Zou J, Feng P, Bok R, et al. Human prostate cancer ZIP1/zinc/citrate genetic/metabolic relationship in the TRAMP prostate cancer animal model. Cancer Biol Ther. 2011;12:1078–1084. doi: 10.4161/cbt.12.12.18367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feng P, Li TL, Guan ZX, Franklin RB, Costello LC. Effect of zinc on prostatic tumorigenicity in nude mice. Ann N Y Acad Sci. 2003;1010:316–320. doi: 10.1196/annals.1299.056. [DOI] [PubMed] [Google Scholar]
- 32.Feng P, Li TL, Guan ZX, Franklin RB, Costello LC. Direct effect of zinc on mitochondrial apoptogenesis in prostate cells. Prostate. 2002;52:311–318. doi: 10.1002/pros.10128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Feng P, Li T, Guan Z, Franklin RB, Costello LC. The involvement of Bax in zinc-induced mitochondrial apoptogenesis in malignant prostate cells. Mol Cancer. 2008;7:25. doi: 10.1186/1476-4598-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ding WQ, Liu B, Vaught JL, Yamauchi H, Lind SE. Anticancer activity of the antibiotic clioquinol. Cancer Res. 2005;65:3389–3395. doi: 10.1158/0008-5472.CAN-04-3577. [DOI] [PubMed] [Google Scholar]
- 35.Ding WQ, Lind SE. Metal ionophores - an emerging class of anticancer drugs. IUBMB Life. 2009;61:1013–1018. doi: 10.1002/iub.253. [DOI] [PubMed] [Google Scholar]
- 36.Yu H, Lou JR, Ding WQ. Clioquinol independently targets NF-kappaB and lysosome pathways in human cancer cells. Anticancer Res. 2010;30:2087–2092. [PubMed] [Google Scholar]
- 37.Chen D, Cui QC, Yang H, Barrea RA, Sarkar FH, et al. Clioquinol, a therapeutic agent for Alzheimer's disease, has proteasome-inhibitory, androgen receptor-suppressing, apoptosis-inducing, and antitumor activities in human prostate cancer cells and xenografts. Cancer Res. 2007;67:1636–1644. doi: 10.1158/0008-5472.CAN-06-3546. [DOI] [PubMed] [Google Scholar]
- 38.Mao X, Schimmer AD. The toxicology of Clioquinol. Toxicol Lett. 2008;182:1–6. doi: 10.1016/j.toxlet.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 39.Bareggi SR, Cornelli U. Clioquinol: review of its mechanisms of action and clinical uses in neurodegenerative disorders. CNS Neurosci Ther. 2012;18:41–46. doi: 10.1111/j.1755-5949.2010.00231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leitzmann MF, Stampfer MJ, Wu K, Colditz GA, Willett WC, et al. Zinc supplement use and risk of prostate cancer. J Natl Cancer Inst. 2003;95:1004–1007. doi: 10.1093/jnci/95.13.1004. [DOI] [PubMed] [Google Scholar]
- 41.Costello LC, Feng P, Milon B, Tan M, Franklin RB. Role of zinc in the pathogenesis and treatment of prostate cancer: critical issues to resolve. Prostate Cancer Prostatic Dis. 2004;7:111–117. doi: 10.1038/sj.pcan.4500712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Costello LC, Franklin RB, Feng P, Tan M, Bagasra O. Zinc and prostate cancer: a critical scientific, medical, and public interest issue (United States). Cancer Causes Control. 2005;16:901–915. doi: 10.1007/s10552-005-2367-y. [DOI] [PubMed] [Google Scholar]
- 43.Gonzalez A, Peters U, Lampe JW, White E. Zinc intake from supplements and diet and prostate cancer. Nutr Cancer. 2009;61:206–215. doi: 10.1080/01635580802419749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Epstein MM, Kasperzyk JL, Andrén O, Giovannucci EL, Wolk A, et al. Dietary zinc and prostate cancer survival in a Swedish cohort. Am J Clin Nutr. 2011;93:586–593. doi: 10.3945/ajcn.110.004804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Costello LC, Franklin RB, Feng P, Tan M. Re: Zinc supplement use and risk of prostate cancer. J Natl Cancer Inst. 2004;96:239–240. doi: 10.1093/jnci/djh045. [DOI] [PubMed] [Google Scholar]
- 46.Costello LC, Franklin RB, Tan MT. A Critical Assessment of Epidemiology Studies Regarding Dietary/Supplemental Zinc and Prostate Cancer Risk. Open Urol Nephrol J . 2008 doi: 10.2174/1874303X00801010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Krone CA, Harms LC. Re: Zinc supplement use and risk of prostate cancer. J Natl Cancer Inst. 2003;95:1556. doi: 10.1093/jnci/djg088. [DOI] [PubMed] [Google Scholar]
- 48.Chang ET, Hedelin M, Adami HO, Grönberg H, Bälter KA. Re: Zinc supplement use and risk of prostate cancer. J Natl Cancer Inst. 2004;96:1108. doi: 10.1093/jnci/djh206. [DOI] [PubMed] [Google Scholar]
- 49.Taubes G. Epidemiology faces its limits. Science. 1995;269:164–169. doi: 10.1126/science.7618077. [DOI] [PubMed] [Google Scholar]
- 50.Gumulec J, Masarik M, Adam V, Eckschlager T, Provaznik I, et al. Serum and tissue zinc in epithelial malignancies: a meta-analysis. PLoS One. 2014;9:e99790. doi: 10.1371/journal.pone.0099790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Whelan P, Walker BE, Kelleher J. Zinc, vitamin A and prostatic cancer. Br J Urol. 1983;55:525–528. doi: 10.1111/j.1464-410x.1983.tb03362.x. [DOI] [PubMed] [Google Scholar]
- 52.Chirulescu Z, Chiriloiu C, Suciu A, Pîrvulescu R. Variations of zinc, calcium and magnesium in normal subjects and in patients with neoplasias. Med Interne. 1987;25:257–261. [PubMed] [Google Scholar]
- 53.Ogunlewe JO, Osegbe DN. Zinc and cadmium concentrations in indigenous blacks with normal, hypertrophic, and malignant prostate. Cancer. 1989;63:1388–1392. doi: 10.1002/1097-0142(19890401)63:7<1388::aid-cncr2820630725>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 54.Lekili M, Ergen A, Celebi I. Zinc plasma levels in prostatic carcinoma and BPH. Int Urol Nephrol. 1991;23:151–154. doi: 10.1007/BF02549712. [DOI] [PubMed] [Google Scholar]
- 55.Goel T, Sankhwar SN. Comparative study of zinc levels in benign and malignant lesions of the prostate. Scand J Urol Nephrol. 2006;40:108–112. doi: 10.1080/00365590500368922. [DOI] [PubMed] [Google Scholar]
- 56.Habib FK, Dembinski TC, Stitch SR. The zinc and copper content of blood leucocytes and plasma from patients with benign and malignant prostates. Clin Chim Acta. 1980;104:329–335. doi: 10.1016/0009-8981(80)90390-3. [DOI] [PubMed] [Google Scholar]
- 57.Feustel A, Wennrich R. Zinc and cadmium plasma and erythrocyte levels in prostatic carcinoma, BPH, urological malignancies, and inflammations. Prostate. 1986;8:75–79. doi: 10.1002/pros.2990080109. [DOI] [PubMed] [Google Scholar]
- 58.Costello LC, Franklin RB. The genetic/metabolic transformation concept of carcinogenesis. Cancer Metastasis Rev. 2012;31:123–130. doi: 10.1007/s10555-011-9334-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hom JJ, Coakley FV, Simko JP, Lu Y, Qayyum A, et al. High-grade prostatic intraepithelial neoplasia in patients with prostate cancer: MR and MR spectroscopic imaging features--initial experience. Radiology. 2007;242:483–489. doi: 10.1148/radiol.2422051828. [DOI] [PubMed] [Google Scholar]
- 60.Heijmink SW, Scheenen TW, Fütterer JJ, Klomp DW, Heesakkers RA, et al. Prostate and lymph node proton magnetic resonance (MR) spectroscopic imaging with external array coils at 3 T to detect recurrent prostate cancer after radiation therapy. Invest Radiol. 2007;42:420–427. doi: 10.1097/01.rli.0000262759.46364.50. [DOI] [PubMed] [Google Scholar]
- 61.Kim YR, Kim IJ, Kang TW, Choi C, Kim KK, et al. HOXB13 downregulates intracellular zinc and increases NF-κB signaling to promote prostate cancer metastasis. Oncogene. 2014;33:4558–4567. doi: 10.1038/onc.2013.404. [DOI] [PubMed] [Google Scholar]