Abstract
Chest tuberculosis (CTB) is a widespread problem, especially in our country where it is one of the leading causes of mortality. The article reviews the imaging findings in CTB on various modalities. We also attempt to categorize the findings into those definitive for active TB, indeterminate for disease activity, and those indicating healed TB. Though various radiological modalities are widely used in evaluation of such patients, no imaging guidelines exist for the use of these modalities in diagnosis and follow-up. Consequently, imaging is not optimally utilized and patients are often unnecessarily subjected to repeated CT examinations, which is undesirable. Based on the available literature and our experience, we propose certain recommendations delineating the role of imaging in the diagnosis and follow-up of such patients. The authors recognize that this is an evolving field and there may be future revisions depending on emergence of new evidence.
Keywords: Chest radiograph, chest tuberculosis (pulmonary, nodal and pleural), computed tomography, imaging recommendations, TB active
Background
The current guidelines for diagnosis of adult chest tuberculosis (TB) are based primarily on the demonstration of acid-fast bacilli (AFB) on sputum microscopy. Chest radiograph (CXR) finds its place in sputum-negative patients not responding to a course of antibiotics. Though computed tomography (CT) is frequently employed in the diagnosis and follow-up of TB, it does not find a place in the national and international guidelines. Literature is lacking and no consensus exists on use of ultrasound (USG), CT, and magnetic resonance imaging (MRI) in such patients. With India having a large burden of TB, it is important to have established imaging criteria and recommendations.
Sputum smear results take several days while culture results need several weeks.[1] This limits the diagnostic efficiency of these conventional approaches and frequently causes delays in isolating infectious patients.[2] These tests also suffer from low sensitivity. Because of these limitations, imaging plays an important role in evaluation of chest TB (CTB) patients and CT is more sensitive than CXR in this regard.[3,4] For optimal management, the radiologists are often expected to deliver important information, while limiting the radiation exposure and costs to the patients.
Epidemiology: Global Scenario and Indian Perspective
TB is a global health problem and the second leading infectious cause of death, after human immunodeficiency virus (HIV). As per the World Health Organization (WHO) reports, 6.1 million cases of TB were notified by national TB programs in 2012, of which 5.4 million were new cases.[5] Of these, 2.5 million had sputum smear-positive pulmonary TB (PTB), 1.9 million had sputum smear-negative PTB, and 0.8 million had extrapulmonary TB (EPTB); case type was unknown in the remaining cases.[5] India accounted for 26% of total cases of TB worldwide in 2012.[5] TB is one of the leading causes of mortality in India, killing two persons every 3 min, nearly 1000 every day.[6] The number of TB deaths is disappointingly large, given that the majority of these are preventable and that curative regimens have been available for a long time now.
Chest TB
TB can affect any organ system, although manifestations are most commonly related to the chest. The lungs are the most common and often the initial site of involvement. Chest involvement is most commonly pulmonary, followed by lymph nodal and pleural disease (latter two are included under EPTB). Chest wall, cardiac, breast, and skeletal involvement can also occur in the thorax; however, these are beyond the scope of the current review. In the current review, we discuss the most common types of CTB, namely PTB and EPTB (pleural/lymph nodal). Cough greater than 2 weeks is the primary criterion to suspect PTB. Patients of PTB/EPTB also present with fever, loss of appetite and loss of weight, chest pain or dyspnea.
Role of imaging in CTB
Diagnosis
Treatment evaluation- response assessment, residual activity
Detection of disease complications/sequelae.
Imaging modalities
CXR – Sputum smear microscopy, culture for AFB, and CXR postero-anterior (PA) view are the initial investigations performed in adults suspected to have TB. CXR is frequently employed as the initial test to evaluate unexplained cough. It is the primary modality for diagnosis and follow-up, and may be the only imaging required in sputum-positive cases. Apicogram/lordotic view (for lung apices) and lateral view are of limited utility and CT is the next investigation in case of equivocal CXR. CXR is useful to look for any evidence of PTB as well as to identify other abnormalities responsible for the symptoms. Table 1 delineates the indications of CXR
USG - Sonography is very useful for pleural effusion detection, characterization, guiding drainage, and follow-up. Differentiating minimal effusion from residual thickening is a common indication. USG can also be used to evaluate associated hepatosplenomegaly, ascites, and abdominal lymphadenopathy
CT chest - Multi-detector CT (MDCT) is an important tool in the detection of radiographically occult disease, differential diagnosis of parenchymal lesions,[7] evaluation of mediastinal lymph nodes (LNs), assessing disease activity, and evaluating complications. It not only enables earlier and more accurate diagnosis of pulmonary lesions, but also can be used to differentiate the etiologies of pneumonia.[7,8] CT enables evaluation of bronchiectasis, cavitation, associated fungal balls, and assessment of necrosis in the LNs, identifying pleural/airway/diaphragmatic pathologies and evaluating visualized bones. Contrast-enhanced CT (CECT) is the investigation of choice for evaluation of mediastinal LNs and also aids in depicting pleural enhancement in empyema. High-resolution CT (HRCT) reconstructions are especially useful to detect miliary and centrilobular nodules, ground-glass opacities, and air-trapping. Table 1 outlines the various situations where CT chest is recommended. The value of CT lies in the fact that it enables one to suggest a diagnosis of TB in patients with negative sputum examination and those without sputum production [as occurs in the follow-up of patients on anti-tuberculosis therapy (ATT) or at presentation] non-invasively. Moreover, CT findings may permit empirical initiation of ATT until the time culture results are obtained[9]
MRI - MRI is a problem-solving modality and conventional sequences (T1 and T2W images) should be combined with diffusion-weighted imaging (DWI) and subtracted contrast-enhanced (CE) imaging for optimal evaluation. It can be used to better evaluate mediastinal nodes and assess disease activity in case of mediastinal nodes/fibrosis. Since it is free from ionizing radiation, MRI can be employed for follow-up of mediastinal nodal disease in young patients to reduce radiation exposure. Presence of diffusion restriction in the LNs and peripheral enhancement suggest active disease. MRI has been proven to be superior to non-contrast CT in the evaluation of mediastinal nodes, pleural abnormalities, and presence of caseation.[10] It may serve as a reasonable alternative to CT for lung parenchymal evaluation in pregnant patients.[10] Cost and availability issues are the main limitations
Positron emission tomography-CT - fluorodeoxyglucose -positron emission tomography (FDG-PET) plays an important role in the work-up of patients with pyrexia of unknown origin (PUO), owing to its high sensitivity in the detection of infection, inflammation, and malignancy.[11] Active TB shows increased uptake with high standardized uptake values (SUVs) and may pose as a cancer mimic.[12] PET may help in assessing the disease activity and response to therapy.[11] Though it is not specific for TB, FDG-PET CT can guide biopsy from active sites, assess complete disease extent, and detect occult distant involvement. The use of PET CT in evaluation of benign diseases is, however, limited due to high radiation exposures involved.
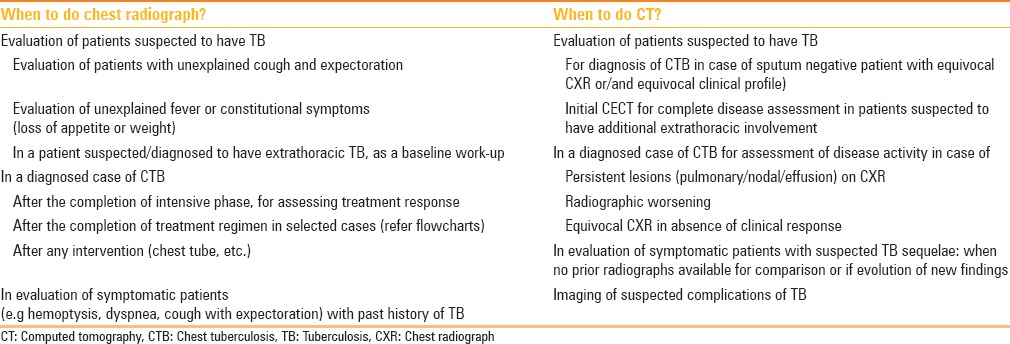
Table 1.
Indications of doing a chest radiograph and CT (in the context of CTB)
Primary and Post-primary TB
CTB is conventionally divided into primary and post-primary (or reactivation) TB (PPT), each with corresponding radiological patterns, albeit with considerable overlap. The radiological features depend on age, underlying immune status, and prior exposure. Figure 1 depicts the natural history and progression of the disease.
Figure 1.
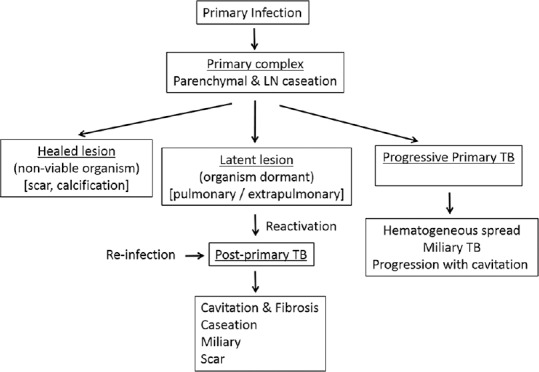
Natural history of chest tuberculosis
Primary TB is acquired by inhalation of airborne organisms and occurs in patients not previously exposed to Mycobacterium tuberculosis. It commonly affects infants and children in endemic areas. However, primary TB is now increasingly encountered in adult patients, accounting for 23-34% of all adult cases and even more in non-endemic areas.[13,14] The primary parenchymal focus is known as the Ghon focus and the combination of Ghon focus and enlarged draining LNs constitutes the primary complex: The Ranke or Ghon complex.[15]
Primary TB may involve lung parenchyma, LNs, tracheobronchial tree, and pleura. Classically, four entities are described: Gangliopulmonary TB, TB pleuritis, miliary TB, and tracheobronchial TB.[15] Only the gangliopulmonary form is characteristic of primary TB and the rest may be seen in post-primary disease as well.
Gangliopulmonary TB is characterized by the presence of mediastinal and/or hilar LN enlargement with associated parenchymal abnormalities. LN enlargement is seen in up to 96% children and 43% adults with primary TB.[16,17,18] Right paratracheal, hilar, and subcarinal regions are the most common sites of nodal involvement, though other sites may also be affected. Bilateral adenopathy occurs in 31% cases.[17] The prevalence of adenopathy decreases with age.[17] CT is better than CXR in detection and characterization of thoracic LN enlargement.[19] On CECT scan, the enlarged LNs show highly characteristic, but not pathogonomic, “rim sign” attributed to low-density center surrounded by a peripheral rim enhancement.[20] This rim sign may also be seen with atypical mycobacteria, histoplasmosis, metastases (from head/neck/testicular malignancy), and lymphoma.[15] Heterogeneous enhancement may also be seen. Homogeneous enhancement is more commonly found in pediatric age group.[19] Associated lung infiltrates are seen on the same side as nodal enlargement in two-thirds of pediatric cases of primary PTB.[17] Parenchymal opacities are usually located in the peripheral subpleural regions. They may be difficult to see on radiographs; thus, CT is often required to detect these subtle parenchymal infiltrates.[21] CXRs may be normal in 15% of cases.[22] Contrary to the age-related decrease in occurrence of lymphadenopathy, the prevalence of radiographically detectable lung involvement is higher in older children and adults,[17,18] so much so that primary infection in adults frequently manifests as parenchymal consolidation without adenopathy. On CT, the air-space consolidation in primary TB is dense, homogeneous, and well-defined. Parenchymal disease in primary TB commonly affects the middle and lower lung zones on CXR, corresponding to the middle lobe, basal segments of lower lobes, and anterior segments of upper lobes.
Generally, the primary disease is self-limiting and immune-competent persons remain asymptomatic. Frequently, the only radiological evidence of primary TB is a combination of parenchymal scar (±calcified) and calcified hilar and/or paratracheal LNs. Complications of gangliopulmonary TB include perforation of an enlarged LN into a bronchus, bronchial compression due to adenopathy leading to retro-obstructive pneumonia, and/or atelectasis. The latter is usually right sided, with obstruction occurring at the level of the right lobar bronchus or bronchus intermedius.[23] In 5-10% patients of primary TB, the infection is progressive and hematogenous dissemination occurs; this is termed progressive primary TB, manifestations of which are identical to PPT.[9]
PPT occurs in previously sensitized patients and results either from re-infection or from reactivation of dormant bacilli in primary infection (90% of cases) owing to immunosuppression, malnutrition, senility, and debilitation.[24,25] Thus, PPT occurs predominantly in adolescents and adults and usually begins with necrotizing consolidation followed by transbronchial spread.[9]
PPT is characterized by: 1. Liquefaction of caseous necrosis, 2. formation of cavities, 3. progressive fibrosis and lung destruction, and 4. bronchogenic spread.[15] Apico-posterior segments of the upper lobes and superior segments of the lower lobes are the usual sites of involvement.[15] Initially, there is liquefaction of regions of caseous necrosis, which then communicate with the tracheobronchial tree to form cavities. Coughing may result in bronchogenic spread to other lung segments and/or may be a source of infection for other patients via inhalation of bacilli-laden droplets. Fibro-atelectasis is common, especially of the upper lobes with retraction of the hilum, mediastinal shift, pulling up of diaphragm, and compensatory hyperinflation of the normal lung segments. Associated pleural thickening, especially of the lung apices, may be evident along with extrapleural fat proliferation. End-stage TB may cause complete destruction of the lung parenchyma resulting from a combination of parenchymal and airway involvement. Contrary to the previous notions, recent studies[26] suggest that children and adolescents are also equally prone to develop destructive lung changes with severe sequelae, similar to PPT. The similar location and morphology of parenchymal changes observed in children blurs the distinction between primary and reactivation TB.
Imaging in PPT often shows extensive abnormalities in predisposed locations.[27] Features of active endobronchial infection - consolidations, alveolar opacities on CXR, clustered nodules, centrilobular nodules on CT - are hallmarks of active PPT. Bronchogenic spread is evident radiographically in 20% of cases and manifests as multiple, ill-defined micronodules, in segmental or lobar distribution, distant from the site of cavitation and usually involving the lower lung zones.[28] On CT scan, it is identified in 95% of cases making HRCT the imaging modality of choice to detect early bronchogenic spread.[3,29] Typical findings include 2- to 4-mm centrilobular nodules and “tree-in-bud” branching opacities (sharply marginated linear branching opacities around terminal and respiratory bronchioles).[3] Cavitation is also characteristic of PPT, radiographically evident in 40% of cases, and walls may be thin and smooth or thick and nodular. Thick-walled cavities and cavities with surrounding consolidation indicate active infection, while thin-walled cavities suggest healed infection.[9] Thin-walled cavities may be difficult to differentiate from bullae, cysts, or pneumatoceles. Air-fluid levels in the cavity occur in 10% of cases and can be due to superimposed bacterial or fungal infection.[16,28] Fibro-parenchymal lesions causing distortion of lung parenchyma and cicatricial bronchiectasis develop with healing of active infection.
Tuberculous cavities can rupture into pleural space, resulting in empyema and even bronchopleural fistula. Erosion into the pulmonary artery branches can lead to massive hemoptysis (Rasmussen pseudoaneurysm). Erosion into systemic vessels or pulmonary veins can lead to hematogenous dissemination and miliary TB. Healing of PPT occurs with fibrosis and calcification.
Radiological patterns encountered in both primary and/or post-primary CTB
Miliary TB
Miliary TB results from hematogenous dissemination of the TB bacilli leading to the development of innumerable small granulomas in lungs and other organs. Though classically encountered in children, the incidence in adults is increasing.[15,26] Early in the course of the disease, CXR may be normal in 25-40% of cases.[30] CT, especially HRCT, can demonstrate miliary disease before it becomes radiographically apparent. Presence of 1-3 mm nodules, both sharply and poorly defined, diffusely spread in random distribution in both lungs, often associated with interstitial septal thickening is characteristic.[25] There may be some basal predominance due to gravity-dependent increased blood flow to the lung bases. Initially, the foci are about 1 mm in diameter. Untreated, they may reach 3-5 mm in size and may become confluent, presenting a “snow-storm” appearance.
Pleural involvement
Involvement of the pleura is one of the most common forms of EPTB and is more common in the primary disease. In case of primary TB, it manifests as unilateral free large effusion, without loculations. It occurs 3-6 months after infection, as a result of delayed hypersensitivity response to mycobacterial antigens.[15] It is often asymptomatic and microbiological analyses are often negative. Though rare in children, it is common in adolescents and young adults. Pleural involvement can be seen in up to 38% cases of primary TB and up to 18% cases of PPT.[16] In PPT, effusion is usually small, loculated, and associated with parenchymal lesions. Since it originates from rupture of a cavity into the pleural space, cultures are usually positive because a larger number of bacilli are found in the pleural space.[31] The exudative effusion in PPT develops in three phases. The first phase is the exudative phase where CECT typically shows smooth thickening and enhancement of the visceral and parietal pleura with loculated effusion within (split pleura sign).[15] There may be septations and echogenic debris within, which are better appreciated on USG. The latter are more characteristic of the second phase, the fibrino-purulent stage. At this time, the effusion may consist entirely of pus (empyema) when there may be associated rib crowding on imaging and volume loss as well. This empyema may break through the parietal pleura to form a subcutaneous abscess (empyema necessitans). Appearance of air-fluid level in empyema suggests communication with the bronchial tree (bronchopleural fistula). The latter presents as increasing expectoration, air in the pleural space, and changing air-fluid level. CT is the investigation of choice and may demonstrate the exact site of communication between the pleural space and the bronchial tree or lung parenchyma.[32]
The final phase is the organizing phase and includes chronic empyema and fibrothorax. Chronic empyemas appear as persistent focal fluid collections with pleural thickening and calcification with extrapleural fat proliferation. Fibrothorax manifests as diffuse pleural thickening with volume loss, but without effusion, and suggests inactivity. Pleural thickening and calcifications are the frequently encountered features of healed TB.
When CXR suggests pleural effusion, thoracocentesis and pleural fluid analysis (biochemical, cytological, and microscopic examination) should be done. In addition, sputum induction for AFB and culture is recommended in all patients suspected to have TB pleurisy.[33] Straw-colored fluid with large number of cells (in hundreds; predominantly mononuclear), high protein level (>3 g/dl), and elevated adenosine deaminase (ADA) levels suggest TB.[34] ADA levels greater than 40 U/l in the pleural fluid have a high predictive value in areas with high TB prevalence, and the specificity of this enzyme increases if the exudate is predominantly lymphocytic.[33] Pleural biopsy may be performed when the thoracocentesis findings are inconclusive.
Tracheobronchial TB
Tracheobronchial involvement occurs in 2-4% of patients with PTB.[35] It usually occurs as a complication of primary TB, originating from perforation of an involved LN into a bronchus, though it may occur in PPT as well by ascending endobronchial spread.[15] Lymphatic submucosal spread and hematogenous infection may also be responsible. CT in acute tracheobronchitis may reveal circumferential narrowing of the involved segment associated with smooth or irregular wall thickening.[36,37] Abnormal enhancement and adjacent adenopathy may also be seen. Less commonly, ulcerated polypoid mass or peribronchial soft tissue cuff may be seen.[37] Involvement of the small airways is in the form of acute bronchiolitis with centrilobular “tree-in-bud” nodules.
This granulomatous involvement of the tracheobronchial tree can ulcerate, which on healing produces fibrotic bronchostenosis and post-obstructive bronchiectasis. Long segment involvement is common and left main bronchus is most frequently involved.[35] These bronchial strictures can lead to lobar or segmental collapse which may be evident on CXR. However, the more common cause of bronchiectasis in TB is cicatricial bronchiectasis as a result of destruction–fibrosis of lung parenchyma. Calcified peribronchial LNs can erode into or cause distortion of adjacent bronchus (more common on the right side), producing broncholiths. Presence of calcium near an area of lung collapse may be a subtle indicator of broncholithiasis.[38] Secondary amyloidosis may also develop in this background of chronic inflammation.
Tuberculoma
Tuberculomas are persistent nodules or mass-like lesions which can be seen in both primary TB and PPT. Pulmonary tuberculomas can range in size from being subcentimetric to 5 cm in diameter, and may be solitary or multiple. They are most often the result of healed primary TB and are usually smooth-walled and sharply defined. The majority of these lesions remain stable in size and may calcify. Nodular or diffuse calcification can be seen in 20-30% of tuberculomas.[39] Cavitation is seen in 10-50% of cases. In 80% of cases, small round opacities (satellite lesions) may be observed in the immediate vicinity of the main lesion.[15]
Complications of CTB
Various complications can occur. These include
Parenchymal complications
Aspergilloma colonization in pre-existing tuberculous cavities. Such patients may also present with hemoptysis as the dominant symptom
Destructive lung changes
Scar carcinoma - co-existence or secondary development of malignancy
Airway complications - tracheobronchial involvement (including broncholithiasis and secondary amyloidosis)
Vascular complications (pseudoaneurysms, hypertrophied bronchial arteries, and systemic collaterals), which present with hemoptysis
Pleural complications (chronic empyema, fibrothorax, bronchopleural fistula, and pneumothorax)
Mediastinal complications: Mediastinal fibrosis, esophageal involvement (in the form of strictures, traction diverticulae, or fistulae), pericarditis, pneumothorax, and spondylodiskitis.
Imaging findings of active CTB
The imaging findings of active CTB are presented in Table 2 and Figures 2 and 3.
Table 2.
Indicators of CTB disease activity on CXR and CT
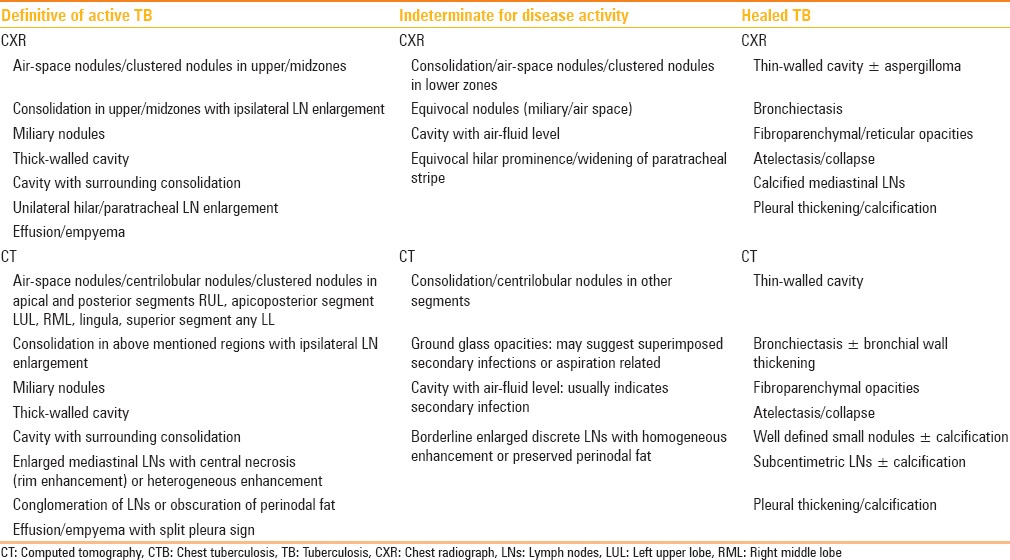
Figure 2 (A-E).
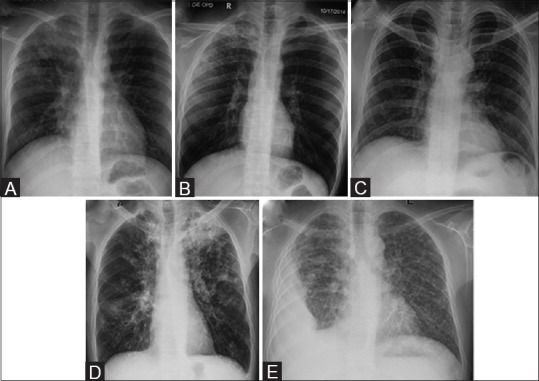
Chest radiographs in active TB. (A) CXR depicts RT upper zone consolidation with prominent RT hilum. (B) CXR in a different patient shows multiple coalescent air-space nodules in RT upper zone. (C) CXR in a different patient shows multiple ill-defined reticulo-nodular lesions in both lungs with basal predominance, suggestive of miliary TB. (D) CXR in a different patient shows active post-primary TB. Cavity with surrounding consolidation is seen in LT upper zone. Scattered air-space nodules are seen in both lungs with left hilar adenopathy. (E) There is RT-sided loculated pleural effusion with multiple air-space nodules scattered in both lungs
Figure 3 (A-G).
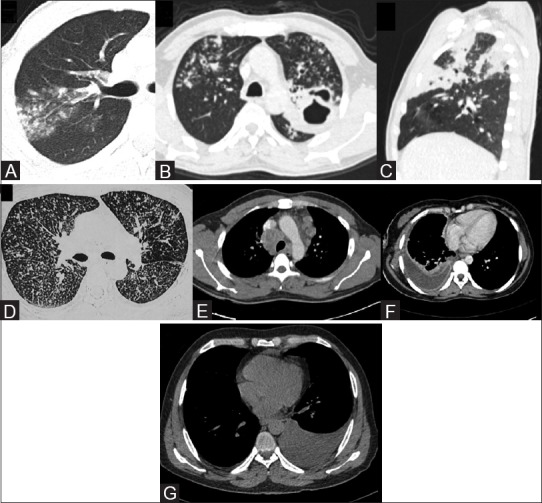
Chest CT in active TB. (A) Lung window (window center -600 HU, width 1200 HU) of chest CT depicts centrilobular and clustered nodules in posterior segment of RT upper lobe, suggesting active endobronchial infection. (B) Lung window of chest CT in a different patient shows cavity with surrounding consolidation in apicoposterior segment of LT upper lobe. Multiple centrilobular nodules with tree-in-bud branching pattern are also seen. (C) Sagittal multiplanar CT reformat lung window shows segmental consolidations in RT upper lobe. (D) Axial CT section lung window (in the same patient as in Figure 1c) in miliary TB shows multiple tiny discrete nodules randomly distributed in both lungs. (E) Axial CECT mediastinal window (window center 40 HU, width 400 HU) shows conglomerate rim-enhancing lymphadenopathy in paratracheal locations and multiple enlarged lymph nodes in prevascular location as well showing central necrosis. (F) Axial CECT mediastinal window shows RT-sided effusion with enhancing layers of pleura (split pleura sign) and rib crowding suggestive of empyema. (G) Axial non-contrast CT mediastinal window shows LT-sided free effusion
A normal CXR has a high negative predictive value for the presence of active TB. On the other hand, presence of characteristic radiographic findings in appropriate clinical setting may be sufficient to diagnose TB even in the absence of sputum positivity; and no further investigation is required. Even then, disease activity may not be accurately assessed by radiographs and the frequency of false-negatives is higher in HIV-positive patients.[24,25,26] Temporal change over serial radiographs is frequently employed to assess response to ATT and evolution of new lesions may suggest reactivation in the proper clinical setting. No significant radiographic change over 4- to 6-month interval is termed “radiographically stable” disease and generally indicates disease inactivity.[9]
Following are the imaging findings which suggest active TB:
Consolidation: usually located in lung apices and/or superior segments of lower lobes.[40] CT is more sensitive and can detect subtle and smaller consolidations. Presence of consolidation is non-specific for the etiology of infection; nevertheless, consolidation with ipsilateral hilar/paratracheal LN enlargement is strongly suggestive of TB. On CT, the majority of consolidations are peribronchial or subpleural in location. Consolidations involving multiple lung segments are more likely to have positive AFB smear results.[41] Consolidations in the basal segments of lower lobes are unlikely to be associated with TB, though they may be seen in elderly patients.[42] Lobular consolidations favor TB, while other bacterial infections are more likely to present with segmental consolidation[43]
Thick-walled cavity: thick-walled cavities are frequently seen in patients with early active TB and represent necrotizing consolidation in the early stage. Cavities, consolidations, and nodules in the upper lung fields suggest active TB in several prediction models[41,44]
Cavity with air-fluid levels: air-fluid levels in tuberculous cavities have been reported to be an indicator of superimposed bacterial or fungal infection[9]
Acinar/centrilobular nodules (bronchogenic spread): ill-defined fluffy air-space nodular opacities (5-10 mm) are indicators of active disease on CXRs.[3] These nodules may coalesce, resulting in focal area of bronchopneumonia. CT features of endobronchially disseminated TB include centrilobular nodules and sharply marginated linear branching opacities (tree-in-bud sign) along with bronchial wall thickening and narrowing. These indicate active disease and correspond to bronchitis of the small airways. Presence of centrilobular nodules and tree-in-bud appearance on CT is more sensitive than radiographs in detection of active endobronchial disease.[45] Other causes of tree-in-bud nodules include infections (bacterial, fungal, viral, or parasitic), bronchiolitis, aspiration or inhalation of foreign substances, connective tissue disorders, and neoplastic pulmonary emboli
Clustered nodules: Large nodular opacities (1-4 cm) may result due to coalescence of smaller nodules. These usually have irregular margins and are surrounded by tiny satellite nodules. These may appear as nodular patches or masses on CXR. Such nodule clusters, especially in a peribronchial distribution are an indicator of active disease.[40,41] Larger nodules (>1 cm) are seen in Kaposi's sarcoma (in HIV) and lymphoma.[46] Large nodules with surrounding ground-glass and internal cavitation favor a diagnosis of fungal infections[46]
Miliary nodules: Small (1-3 mm), well-defined, randomly distributed nodules that indicate hematogenous spread of infection. These may be inconspicuous on radiographs and evident only on HRCT, which may also show associated septal thickening[47]
Rim-enhancing LNs: Enlarged LNs (short axis dimension >1 cm) with peripheral rim enhancement and central low attenuation suggest active disease, while homogeneous and calcified nodes represent inactive disease.[48] Low attenuation areas have a pathological correspondence to caseous necrosis and are thus a reliable indicator of disease activity. Conglomeration of LNs and obscuration of perinodal fat are also associated with active disease.[19] Homogeneously enhancing lymphadenopathy without calcification poses a diagnostic dilemma. Viral and fungal infections are less likely to be associated with lymphadenopathy, thus presence of enlarged LNs favors TB[49,50]
Pleural effusion or empyema: Unilateral free effusion and empyema suggest active disease, while isolated pleural thickening with or without calcification indicates healed TB.
It may be borne in mind that imaging modalities like CXR and CT serve to detect and localize the disease,[34] and based on site and morphology of findings, diagnosis of active TB may be suggested. Definitive diagnosis of active TB still requires isolation and identification of M. tuberculosis, especially if the clinical/laboratory profile is equivocal.
Table 2 delineates features which are definitive of active TB [Figures 2 and 3], definitive for healed TB (sequelae) [Figure 4], and features indeterminate for disease activity [Figure 5]. Figure 6 demonstrates examples of complications in CTB. When CT features indicate TB but are indeterminate for disease activity, then other criteria like bronchoalveolar lavage [BAL] (in case of parenchymal involvement), laboratory parameters (erythrocyte sedimentation rate ESR, C-reactive protein CRP, total and differential leukocyte counts TLC, DLC respectively, and Mantoux test), sampling for LNs, thoracocentesis for effusion, clinical response, and follow-up may be employed to resolve the ambiguity.
Figure 4(A-F).
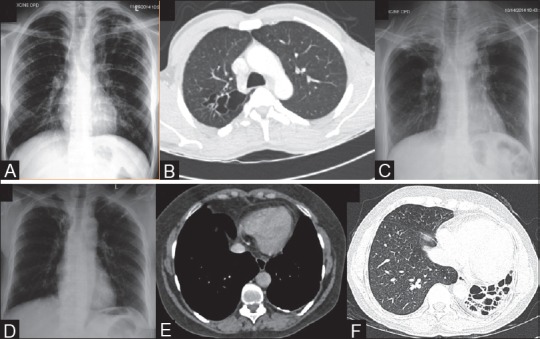
Imaging features of healed TB. (A) CXR shows thin-walled cavity in left upper zone. Areas of fibro-bronchiectasis and fibrocalcific lesions are seen in left upper zone, RT upper and mid zones. (B) Axial CT lung window (window center -600 HU, width 1200 HU) shows clustered thin-walled cavities in superior segment RT lower lobe. (C) CXR shows volume loss in both upper zones with apical pleural thickening, pulled hila, fibro-bronchiectasis, and calcific foci. (D) CXR shows fibro-bronchiectasis both upper zones. (E) CECT mediastinal window (window center 40 HU, width 400 HU) shows left-sided pleural thickening and focal plaque-like calcifications. (F) CT lung window section in end-stage lung disease shows collapse and bronchiectasis involving the left lung with ipsilateral mediastinal shift and rib crowding
Figure 5 (A-C).
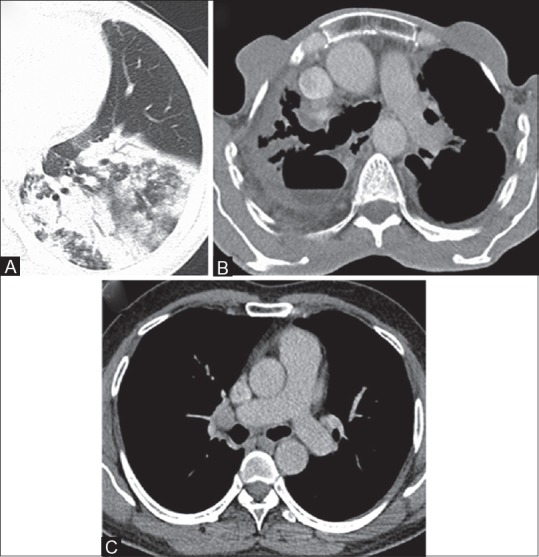
Imaging features indeterminate for disease activity in CTB. (A) Axial CT lung window (window center -600 HU, width 1200 HU) shows consolidation in basal segments of left lower lobe. No ipsilateral adenopathy, no cavitation was seen. (B) CECT mediastinal window (window center 40 HU, width 400 HU) shows cavity with air-fluid level in RT upper lobe. Note is also made of bronchiectasis and apical pleural thickening. (C) Axial CECT mediastinal window shows small discrete homogeneous lymph node in RT hilar location, measuring ~10 mm in short axis dimension (SAD). This node was unchanged in size and morphology after complete course of ATT
Figure 6(A-E).
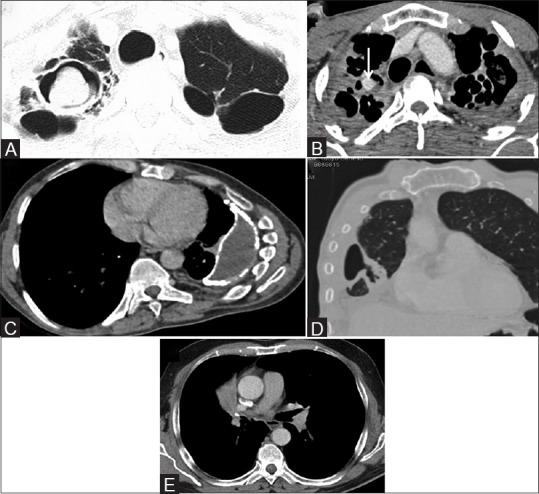
Imaging findings in tuberculous complications. (A) Axial CT lung window (window center -600 HU, width 1200 HU) shows thin-walled cavities in both upper lobes and presence of aspergilloma in RT upper lobe cavity. (B) Axial CECT mediastinal window (window center 40 HU, width 400 HU) shows contrast-filled pseudoaneurym (arrow) arising from the superior division of RT pulmonary artery (Rasmussen aneurysm) in the background of fibro-cavitary lesions in both upper lobes. (C) Axial CECT mediastinal window shows chronic empyema LT side with volume loss and pleural calcifications. (D) Coronal CT lung window depicts abnormal communication of pleural space with bronchial tree suggesting a bronchopleural fistula. (E) Axial CECT mediastinal window shows calcified LN in RT hilum causing post-obstructive atelectasis of RT middle lobe
Following features are not specific for TB and further work-up to exclude other diagnoses like non-tubercular infections, non-infectious diseases (like sarcoidosis, serositis), and even malignancies (lymphoma, carcinoma) should be undertaken:
Consolidation without ipsilateral lymphadenopathy
Imaging features of active endobronchial infection in the non-typical locations
Imaging features of active endobronchial infection in the presence of TB sequelae. These may represent superimposed secondary infection (usually pyogenic) or reactivation TB
Thick-walled cavity may be seen in malignancy
Bilateral hilar lymphadenopathy. Commonly seen in sarcoidosis and lymphoma
Necrotic mediastinal LNs may also occur in malignancies and fungal infections
Bilateral free effusion is more likely to be non-infective in etiology (serositis/underlying heart, liver, or renal disease).
Imaging Signs of Healing (TB Sequelae)
The imaging signs of healing (TB sequelae) are presented in Table 2 and Figures 4 and 7.
Figure 7.
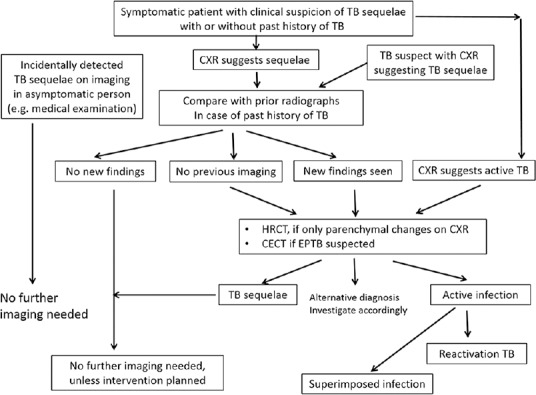
Imaging work-up of symptomatic patients suspected/detected to have TB sequelae
Imaging findings in patients with TB sequelae include bronchovascular distortion, fibro-parenchymal lesions, bronchiectasis, emphysema, and fibro-atelectatic bands indicative of prior infection with scarring.[9] Thin-walled cavities and well-defined nodules may persist for a long time after completion of ATT. The former may get colonized by saprophytic fungi (aspergilloma) and the latter may get calcified. Calcified mediastinal LNs and pleural thickening (with/without calcification) are also imaging features of healed TB. Tuberculomas and small calcified lung nodules also suggest prior infection.
Imaging features of healed TB may be detected incidentally or patients may only have some minor symptoms. In such cases, no further imaging is required, especially if a comparison with prior imaging suggests stability of findings, and symptomatic management is done. However, if the symptoms are severe and refractory, then an initial CT is usually done for comprehensive assessment of lungs, LNs, and pleura. Based on this, definitive management (surgery for localized fibro-bronchiectatic disease) or palliative measures may be undertaken [bronchial artery embolization (BAE) for hemoptysis, bronchoscopy-guided or percutaneous antifungal instillation for persistent fungal ball in pre-existing tuberculous cavities]. The initial CT also serves to rule out any reactivation or to detect any superimposed bacterial infection.
Persistent lesions at the end of treatment
Persistent lesions on CXR at the end of treatment indicate residual lesions in which case activity needs to be resolved using imaging and/or laboratory parameters. The residual inactive lesions do not require any treatment, whereas in case of partial or no response, treatment is prolonged and follow-up is repeated after extension of intensive phase/continuation phase (IP/CP) as per the revised national tuberculosis control program (RNTCP) guidelines. No further imaging/treatment is required when CXR or CT is definitive for healed TB. Secondly, persistent lesions may represent drug-resistant TB, in which case sampling and drug susceptibility testing is recommended. Appearance of new lesions or reappearance of radio-opacities may represent reactivation TB or superimposed bacterial infections. Thirdly, persistent lesions may suggest the possibility of alternative diagnoses and additional work-up may be undertaken to investigate the patient for the same.
Recommendations
Imaging algorithm for diagnosis of CTB
Figure 8 depicts the proposed algorithm. As per the RNTCP, any person with cough for 2 or more weeks is a PTB suspect.[51] Presence of fever, unexplained loss of appetite/weight, and recent contact with an infectious patient further raise the suspicion. In addition to sputum smear examination, all such patients should be subjected to a CXR, wherever feasible. CXR has been justified as an initial investigation in the evaluation of childhood TB as well.[34] CXR is also desirable in a patient suspected/diagnosed to have extrathoracic TB, as a baseline work-up.
Figure 8.
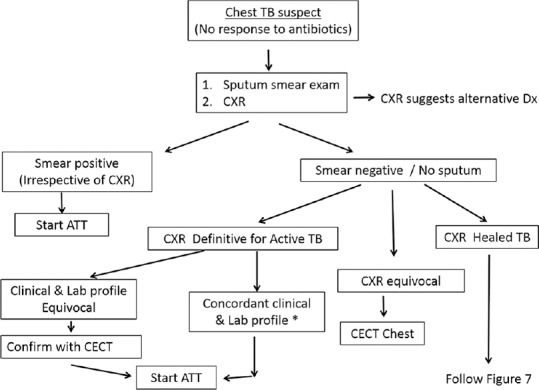
Flowchart depicting the role of imaging in diagnosis of CTB (*lab profile includes hematological parameters like ESR, CRP, TLC, DLC, and Mantoux test)
If the patient is sputum smear positive, ATT can be started irrespective of the CXR findings. Though CXR is likely to be abnormal in majority of such cases, up to 9% patients with culture-confirmed PTB can have normal radiographs, more so in case of HIV-infected population.[52] Even then, initial CXR serves as a reference standard for comparison with future studies.
In case of sputum negativity or inability of the patient to produce sputum, CXR serves a pivotal role in guiding management. If the radiographic findings suggest active TB, ATT may be started if the clinical/laboratory profile is also concordant. In case the latter is equivocal and not specific for TB, confirmation with CECT is needed. CECT is also indicated when the CXR is indeterminate for disease activity. If the CXR suggests healed TB, then as delineated in Figure 7, comparison with prior imaging is desirable to document stability, failing which a CT is usually done to confirm absence of active infection. It may be noted that the initial CT evaluation in a CTB suspect should be a contrast-enhanced study. In addition to being more sensitive, CECT is especially useful to characterize mediastinal LNs, effusion, and to confirm the parenchymal findings. In the unusual scenario of negative sputum and normal CXR in a CTB suspect, CECT may still be undertaken if the clinical suspicion is strong; however, other investigations may also be done depending on the dominant symptom (bronchoscopy/USG abdomen).
Based on the CECT findings, the radiologist should categorize the patient into one of the three categories [Figure 9]. CT may be definitive for active TB, wherein ATT can be started. Presence of even a single imaging criterion of activity in a suspected case of TB is sufficient to diagnose active disease and warrants ATT. Demonstration of AFB is desirable and adds supportive evidence, but is not mandatory. However, if clinically TB is not the most likely possibility, then single criterion of activity needs to be confirmed bacteriologically or other supportive evidence may be sought (blood/pleural fluid parameters, pathological confirmation). If the CT features suggest healed TB (and there is no evidence of active infection), then based on symptoms, palliative/definitive treatment is undertaken. In case CECT is indeterminate for disease activity, other parameters like BAL, lab parameters, or sampling come to rescue. Patient is worked up for alternative diagnosis if CECT findings do not suggest TB.
Figure 9.
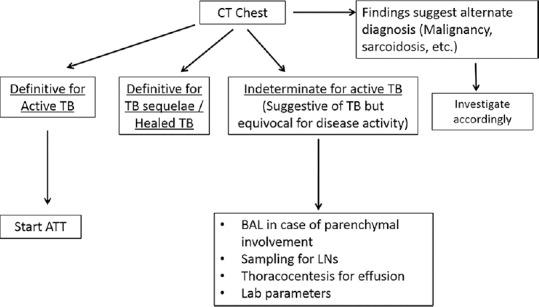
Flowchart demonstrating the stratification of patients after CT. Based on CT findings, the patient should be categorized into either active TB, healed TB, or indeterminate for disease activity
Imaging indicators of active TB, healed TB, and features indeterminate for disease activity
Table 2 enumerates the imaging features of disease activity on CXR and CT.
In a diagnosed case of CTB, these features help in assessing the disease activity at the time of presentation and during follow-up. Imaging features indeterminate for disease activity include equivocal radiographic findings, signs of active endobronchial infection in non-predisposed locations, and non-specific evidence of active infection (which may suggest superimposed secondary infections).
Protocol for follow-up
Figures 10 and 11 show the protocol for follow-up of CTB patients.
Figure 10.
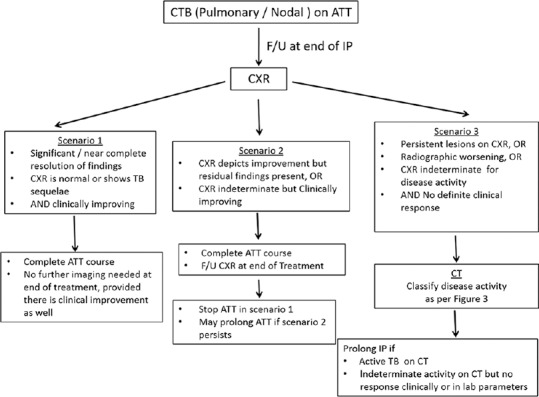
Imaging protocol for follow-up of PTB and mediastinal nodal TB (IP = Intensive phase)
Figure 11.
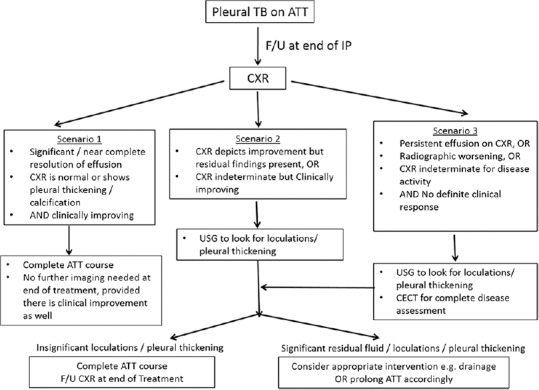
Imaging protocol for follow-up of pleural TB (IP = Intensive phase)
With compliant treatment, clinical improvement is expected within 2-4 weeks. Follow-up is done at the end of IP and CP. In case of no response, follow-up is repeated after extension of IP/CP as per the RNTCP guidelines/institute protocol. If the patient was sputum-smear positive to begin with, then follow-up is usually done with sputum-smear examination. However, problems arise when such patients become unable to produce sputum but other symptoms persist. Also, if sputum becomes negative but clinical improvement is discordant, then imaging provides a viable option for response assessment.
Figure 10 depicts the imaging protocol for follow-up of pulmonary and nodal types of CTB. CXR is done at the completion of IP of the treatment regimen. If there is significant resolution of findings or CXR depicts only sequelae of prior infection, then no further imaging is needed even at the end of treatment regimen, provided there is clinical improvement as well. This is even applicable to those cases where initial disease was evident only on CT. Scenario 2 (partial response) merits a CXR at the completion of ATT course. If at the end of treatment, CXR is consistent with scenario 1, then ATT can be stopped. However, if there is scenario 2 at the end of treatment, then the CP may be prolonged depending on clinical and laboratory parameters. In case of no definite response on CXR and absence of clinical improvement (scenario 3), CT may be done to assess disease activity. Non-contrast CT (with HRCT reconstructions) is sufficient for follow-up of solely parenchymal lesions, but contrast administration is required for follow-up of nodal disease. IP of ATT may be prolonged in case CT suggests residual active disease or if CT is indeterminate but clinical and laboratory parameters do not suggest any response.
If the nodes persist at the completion of treatment regimen, or CECT is equivocal for disease activity, then multiparametric MRI may help. The latter, being a radiation-free alternative, can be employed instead of CT for follow-up in young patients. It may be noted that residual nodes do not necessarily indicate active disease.[19] If there is good clinical response after the completion of treatment regimen with significant reduction in LN size compared with the initial scan, then few persistent LNs may not suggest active disease and can be kept on follow-up.
Figure 11 demonstrates the imaging follow-up in case of pleural TB. The main difference from follow-up of PTB/nodal TB is that USG is recommended to look for loculations/thickening in case of no response or partial response at the end of IP, so that further management can be decided accordingly.
Symptomatic TB sequelae
The imaging features of TB sequelae/healed TB are presented in Table 2.
Patients presenting with refractory respiratory symptoms (persistent/recurrent cough, expectoration, hemoptysis, dyspnea), with or without prior history of ATT, need evaluation using CXR. Figure 7 demonstrates the imaging approach to such patients. The same flowchart should be followed for patients incidentally detected to have TB sequelae on imaging and for those clinically suspected to have active TB but were found to have sequelae on CXR.
A comparison with previous radiographs or CT examinations (if available) is very important. If CXR suggests TB sequelae and there are no new lesions compared with previous imaging, then no further imaging is indicated unless some intervention like BAE is planned. However, if no prior imaging is available, then an initial CECT is usually done to confirm the radiographic findings. CT findings of active infection may suggest a superimposed infection, usually bacterial or reactivation TB. If the patient presents with significant hemoptysis, then CT thoracic angiography may be done to map out the abnormal arteries in order to plan for BAE.
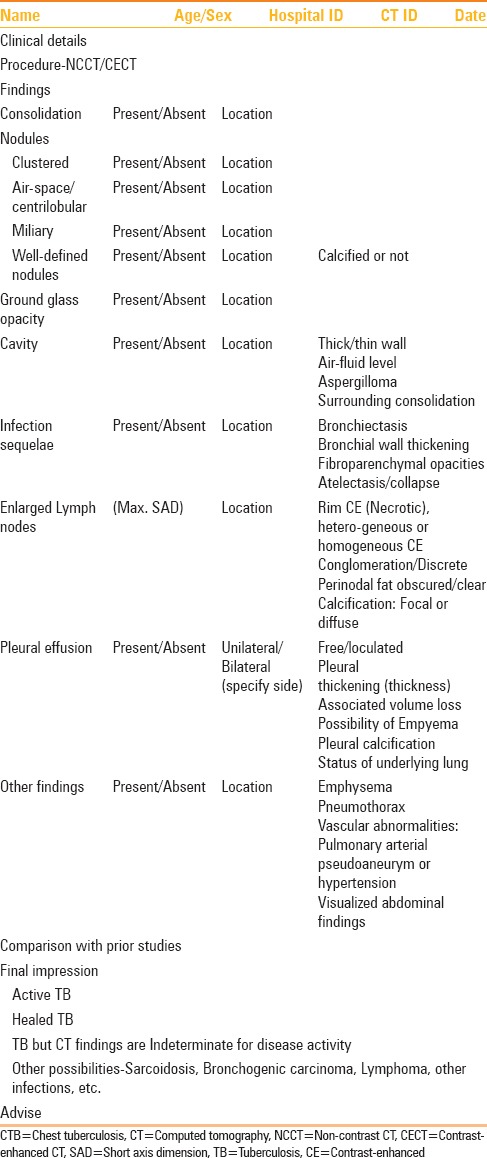
Reporting template
A structured reporting format for reporting chest CT in a suspected/follow-up case of CTB is proposed in Table 3.
Table 3.
Structured reporting format for reporting chest CT in a suspected/follow-up case of CTB
Conclusion
In this review, we have attempted to summarize the criteria to differentiate active TB from sequelae and acknowledge that in conditions where imaging is indeterminate, other parameters be taken into consideration. However, a discussion of non-radiological parameters is beyond the scope of the current review. We have attempted to formulate algorithms for imaging recommendations in the diagnosis and follow-up of patients with suspected/proven CTB. Further research is, however, required for validation of these recommendations and the same may be revised subject to emergence of new information. The proposed recommendations are not intended for application in national programs/at primary health care level, but are more applicable to secondary and tertiary care centers. In fact, we expect that these algorithms would enable judicious use of imaging and reduce the number of unnecessary CT examinations in the diagnosis and follow-up of these cases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Foulds J, O’Brien R. New tools for the diagnosis of tuberculosis: The perspective of developing countries. Int J Tuberc Lung Dis. 1998;2:778–83. [PubMed] [Google Scholar]
- 2.Okur E, Yilmaz A, Saygi A, Selvi A, Süngün F, Oztürk E, et al. Patterns of delays in diagnosis amongst patients with smear-positive pulmonary tuberculosis at a teaching hospital in Turkey. Clin Microbiol Infect. 2006;12:90–2. doi: 10.1111/j.1469-0691.2005.01302.x. [DOI] [PubMed] [Google Scholar]
- 3.Im JG, Itoh H, Shim YS, Lee JH, Ahn J, Han MC, et al. Pulmonary tuberculosis: CT findings- early active disease and sequential change with antituberculous therapy. Radiology. 1993;186:653–60. doi: 10.1148/radiology.186.3.8430169. [DOI] [PubMed] [Google Scholar]
- 4.Jeong YJ, Lee KS. Pulmonary tuberculosis: Up-to-date imaging and management. AJR Am J Roentgenol. 2008;191:834–44. doi: 10.2214/AJR.07.3896. [DOI] [PubMed] [Google Scholar]
- 5.WHO Global tuberculosis report. 2013. [Last accessed on 2014 Aug 06]. Available from: http://www.who.int/tb .
- 6.TBC India: Tuberculosis Key Facts. [Last accessed on 2014 Aug 16]. Available from: http://www.tbcindia.nic.in/key.html .
- 7.Ito I, Ishida T, Togashi K, Niimi A, Koyama H, Ishimori T, et al. Differentiation of bacterial and non-bacterial community-acquired pneumonia by thin-section computed tomography. Eur J Radiol. 2009;72:388–95. doi: 10.1016/j.ejrad.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heussel CP, Kauczor HU, Heussel G, Fischer B, Mildenberger P, Thelen M. Early detection of pneumonia in febrile neutropenic patients: Use of thin-section CT. AJR Am J Roentgenol. 1997;169:1347–53. doi: 10.2214/ajr.169.5.9353456. [DOI] [PubMed] [Google Scholar]
- 9.Raniga S, Parikh N, Arora A. Is HRCT reliable in determining disease activity in pulmonary tuberculosis. Ind J Radiol Imag. 2006;16:221–8. [Google Scholar]
- 10.Rizzi EB, Schinina’ V, Cristofaro M, Goletti D, Palmieri F, Bevilacqua N, et al. Detection of Pulmonary tuberculosis: Comparing MR imaging with HRCT. BMC Infect Dis. 2011;11:243. doi: 10.1186/1471-2334-11-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harkirat S, Anand SS, Indrajit IK, Dash AK. Pictorial essay: PET/CT in tuberculosis. Indian J Radiol Imaging. 2008;18:141–7. [Google Scholar]
- 12.Yang CM, Hsu CH, Lee CM, Wang FC. Intense uptake of [F-18]-fluoro-2 deoxy-D-glucose in active pulmonary tuberculosis. Ann Nucl Med. 2003;17:407–10. doi: 10.1007/BF03006610. [DOI] [PubMed] [Google Scholar]
- 13.McAdams HP, Erasmus J, Winter JA. Radiologic manifestations of pulmonary tuberculosis. Radiol Clin North Am. 1995;33:655–78. [PubMed] [Google Scholar]
- 14.Harisinghani MG, McLoud TC, Shepard JA, Ko JP, Shroff MM, Mueller PR. Tuberculosis from head to toe. Radiographics. 2000;20:449. doi: 10.1148/radiographics.20.2.g00mc12449. quiz 528-9, 532. [DOI] [PubMed] [Google Scholar]
- 15.Van Dyck P, Vanhoenacker FM, Van den Brande P, De Schepper AM. Imaging of pulmonary tuberculosis. Eur Radiol. 2003;13:1771–85. doi: 10.1007/s00330-002-1612-y. [DOI] [PubMed] [Google Scholar]
- 16.Woodring JH, Vandiviere HM, Fried AM, Dillon ML, Williams TD, Melvin IG. Update: The radiographic features of pulmonary tuberculosis. AJR Am J Roentgenol. 1986;146:497–506. doi: 10.2214/ajr.146.3.497. [DOI] [PubMed] [Google Scholar]
- 17.Leung AN, Müller NL, Pineda PR, FitzGerald JM. Primary tuberculosis in childhood: Radiographic manifestations. Radiology. 1992;182:87–91. doi: 10.1148/radiology.182.1.1727316. [DOI] [PubMed] [Google Scholar]
- 18.Choyke PL, Sostman HD, Curtis AM, Ravin CE, Chen JT, Godwin JD, et al. Adult-onset pulmonary tuberculosis. Radiology. 1983;148:357–62. doi: 10.1148/radiology.148.2.6867325. [DOI] [PubMed] [Google Scholar]
- 19.Mukund A, Khurana R, Bhalla AS, Gupta AK, Kabra SK. CT patterns of nodal disease in pediatric chest tuberculosis. World J Radiol. 2011;3:17–23. doi: 10.4329/wjr.v3.i1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim WS, Moon WK, Kim IO, Lee HJ, Im JG, Yeon KM, et al. Pulmonary tuberculosis in children: Evaluation with CT. AJR Am J Roentgenol. 1997;168:1005–9. doi: 10.2214/ajr.168.4.9124105. [DOI] [PubMed] [Google Scholar]
- 21.Naidich DP, McCauley DI, Leitman BS, Genieser NB, Hulnick DH. CT of pulmonary tuberculosis. In: Siegelmann SS, editor. Computed Tomography of the Chest. New York: Churchill Livingstone; 1984. pp. 175–217. [Google Scholar]
- 22.Miller WT, Miller WT., Jr Tuberculosis in the normal host: Radiological findings. Semin Roentgenol. 1993;28:109–18. doi: 10.1016/s0037-198x(05)80100-2. [DOI] [PubMed] [Google Scholar]
- 23.Weber AL, Bird KT, Janower ML. Primary tuberculosis in childhood with particular emphasis on changes affecting the tracheobronchial tree. Am J Roentgenol Radium Ther Nucl Med. 1968;103:123–32. doi: 10.2214/ajr.103.1.123. [DOI] [PubMed] [Google Scholar]
- 24.Haque AK. The pathology and pathophysiology of mycobacterial infections. J Thorac Imaging. 1990;5:8–16. doi: 10.1097/00005382-199004000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Leung AN. Pulmonary tuberculosis: The essentials. Radiology. 1999;210:307–22. doi: 10.1148/radiology.210.2.r99ja34307. [DOI] [PubMed] [Google Scholar]
- 26.Veedu PT, Bhalla AS, Vishnubhatla S, Kabra SK, Arora A, Singh D, et al. Pediatric vs adult pulmonary tuberculosis: A retrospective computed tomography study. World J Clin Pediatr. 2013;2:70–6. doi: 10.5409/wjcp.v2.i4.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Palmer PE. Pulmonary tuberculosis-usual and unusual radiographic presentations. Semin Roentgenol. 1979;14:204–43. doi: 10.1016/0037-198x(79)90007-5. [DOI] [PubMed] [Google Scholar]
- 28.Hadlock FP, Park SK, Awe RJ, Rivera M. Unusual radiographic findings in adult pulmonary tuberculosis. AJR Am J Roentgenol. 1980;134:1015–8. doi: 10.2214/ajr.134.5.1015. [DOI] [PubMed] [Google Scholar]
- 29.Im JG, Itoh H, Han MC. CT of pulmonary tuberculosis. Semin Ultrasound CT MR. 1995;16:420–34. doi: 10.1016/0887-2171(95)90029-2. [DOI] [PubMed] [Google Scholar]
- 30.Kwong JS, Carignan S, Kang EY, Müller NL, Fitz Gerald JM. Miliary tuberculosis. Diagnostic accuracy of chest radiography. Chest. 1996;110:339–42. doi: 10.1378/chest.110.2.339. [DOI] [PubMed] [Google Scholar]
- 31.Hopewell PC. A clinical view of tuberculosis. Radiol Clin North Am. 1995;33:641–53. [PubMed] [Google Scholar]
- 32.Westcott JL, Volpe JP. Peripheral bronchopleural fistula: CT evaluation in 20 patients with pneumonia, empyema, or postoperative air leak. Radiology. 1995;196:175–81. doi: 10.1148/radiology.196.1.7784563. [DOI] [PubMed] [Google Scholar]
- 33.Porcel JM. Tuberculous pleural effusion. Lung. 2009;187:263–70. doi: 10.1007/s00408-009-9165-3. [DOI] [PubMed] [Google Scholar]
- 34.Working Group on Tuberculosis, Indian Academy of Pediatrics (IAP). Consensus statement on childhood tuberculosis. Indian Pediatr. 2010;47:41–55. doi: 10.1007/s13312-010-0008-3. [DOI] [PubMed] [Google Scholar]
- 35.Lee KS, Kim YH, Kim WS, Hwang SH, Kim PN, Lee BH. Endobronchial tuberculosis: CT features. J Comput Assist Tomogr. 1991;15:424–8. doi: 10.1097/00004728-199105000-00014. [DOI] [PubMed] [Google Scholar]
- 36.Moon WK, Im JG, Yeon KM, Han MC. Tuberculosis of the central airways: CT findings of active and fibrotic disease. AJR Am J Roentgenol. 1997;169:649–53. doi: 10.2214/ajr.169.3.9275870. [DOI] [PubMed] [Google Scholar]
- 37.Arora A, Bhalla AS, Jana M, Sharma R. Overview of airway involvement in tuberculosis. J Med Imaging Radiat Oncol. 2013;57:576–81. doi: 10.1111/1754-9485.12017. [DOI] [PubMed] [Google Scholar]
- 38.Conces DJ, Jr, Tarver RD, Vix VA. Broncholithiasis: CT features in 15 patients. AJR Am J Roentgenol. 1991;157:249–53. doi: 10.2214/ajr.157.2.1853800. [DOI] [PubMed] [Google Scholar]
- 39.Lee KS, Song KS, Lim TH, Kim PN, Kim IY, Lee BH. Adult-onset pulmonary tuberculosis: Findings on chest radiographs and CT scans. AJR Am J Roentgenol. 1993;160:753–8. doi: 10.2214/ajr.160.4.8456658. [DOI] [PubMed] [Google Scholar]
- 40.Yeh JJ, Yu JK, Teng WB, Chou CH, Hsieh SP, Lee TL, et al. High-resolution CT for identify patients with smear-positive, active pulmonary tuberculosis. Eur J Radiol. 2012;81:195–201. doi: 10.1016/j.ejrad.2010.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yeh JJ, Chen SC, Teng WB, Chou CH, Hsieh SP, Lee TL, et al. Identifying the most infectious lesions in pulmonary tuberculosis by high-resolution multi-detector computed tomography. Eur Radiol. 2010;20:2135–45. doi: 10.1007/s00330-010-1796-5. [DOI] [PubMed] [Google Scholar]
- 42.Yeh JJ, Chen SC, Chen CR, Yeh TC, Lin HK, Hong JB, et al. A high-resolution computed tomography-based scoring system to differentiate the most infectious active pulmonary tuberculosis from community-acquired pneumonia in elderly and non-elderly patients. Eur Radiol. 2014;24:2372–84. doi: 10.1007/s00330-014-3279-6. [DOI] [PubMed] [Google Scholar]
- 43.McGuinness G, Gruden JF, Bhalla M, Harkin TJ, Jagirdar JS, Naidich DP. AIDS-related airway disease. AJR Am J Roentgenol. 1997;168:67–77. doi: 10.2214/ajr.168.1.8976923. [DOI] [PubMed] [Google Scholar]
- 44.El-Solh AA, Hsiao CB, Goodnough S, Serghani J, Grant BJ. Predicting active pulmonary tuberculosis using an artificial neural network. Chest. 1999;116:968–73. doi: 10.1378/chest.116.4.968. [DOI] [PubMed] [Google Scholar]
- 45.Lee KS, Im JG. CT in adults with tuberculosis of the chest: Characteristic findings and role in management. AJR Am J Roentgenol. 1995;164:1361–7. doi: 10.2214/ajr.164.6.7754873. [DOI] [PubMed] [Google Scholar]
- 46.Edinburgh KJ, Jasmer RM, Huang L, Reddy GP, Chung MH, Thompson A, et al. Multiple pulmonary nodules in AIDS: Usefulness of CT in distinguishing among potential causes. Radiology. 2000;214:427–32. doi: 10.1148/radiology.214.2.r00fe22427. [DOI] [PubMed] [Google Scholar]
- 47.Oh YW, Kim YH, Lee NJ, Kim JH, Chung KB, Suh WH, et al. High-resolution CT appearance of miliary tuberculosis. J Comput Assist Tomogr. 1994;18:862–6. doi: 10.1097/00004728-199411000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Moon WK, Im JG, Yeon KM, Han MC. Mediastinal tuberculous lymphadenitis: CT findings of active and inactive disease. AJR Am J Roentgenol. 1998;170:715–8. doi: 10.2214/ajr.170.3.9490959. [DOI] [PubMed] [Google Scholar]
- 49.Castañer E, Gallardo X, Mata JM, Esteba L. Radiologic approach to the diagnosis of infectious pulmonary diseases in patients infected with the human immunodeficiency virus. Eur J Radiol. 2004;51:114–29. doi: 10.1016/j.ejrad.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 50.Feng F, Shi YX, Xia GL, Zhu Y, Lu HZ, Zhang ZY. Computed tomography in predicting smear-negative pulmonary tuberculosis in AIDS patients. Chin Med J (Engl) 2013;126:3228–33. [PubMed] [Google Scholar]
- 51.Revised guidelines for diagnosis of pulmonary TB. [Last accessed on 2014 Aug 16]. Available from: http://www.tbcindia.nic.in/pdfs/1b-Diagnosis of smear positive pulmonary TB.pdf .
- 52.Pepper T, Joseph P, Mwenya C, McKee GS, Haushalter A, Carter A, et al. Normal chest radiography in pulmonary tuberculosis: Implications for obtaining respiratory specimen cultures. Int J Tuberc Lung Dis. 2008;12:397–403. [PubMed] [Google Scholar]


