Abstract
Background
Bevacizumab plus chemotherapy is a widely used therapeutic option for first-line treatment of metastatic colorectal cancer (mCRC). However, molecular predictors of bevacizumab efficacy have not yet been identified. We analyzed vascular endothelial growth factor (VEGF) and endothelial nitric oxide synthase (eNOS) polymorphisms in relation to response to bevacizumab.
Methods
Two hundred and thirty-seven patients with mCRC enrolled onto the phase III prospective multicentre randomized “Italian Trial in Advanced Colorectal Cancer (ITACa)” trial were evaluated. One hundred fourteen patients received chemotherapy plus bevacizumab (CT + B) and 123 received chemotherapy (CT) alone. Five single nucleotide polymorphisms (SNPs) (−2578, −1498, −1154, −634 and +936) for VEGF and 2 SNPs (−786, +894) and one variable number tandem repeat in intron 4 for eNOS were analyzed for each patient. The polymorphisms were assessed in relation to progression-free survival (PFS), objective response rate (ORR) and overall survival (OS).
Results
VEGF 936C/T, eNOS +894 G/T and VNTR were significantly correlated with outcome in CT + B patients, but not in CT-only patients. In particular, patients with a specific haplotype combination of the 2 eNOS polymorphisms (defined eNOS Haplo1/Haplo1 and eNOS Haplo 2/Haplo2) showed significantly longer PFS (15.0 vs 9.1 months, P = 0.001) and OS (34.5 vs 20.5 months P = 0.002), and a higher ORR (71 vs 45.9%, P = 0.013) than those with the other genotypes, respectively.
Conclusions
Specific eNOS polymorphisms may be capable of identifying a subset of mCRC patients who are more responsive to bevacizumab-based chemotherapy. If confirmed, these results would permit individually tailored treatment with bevacizumab.
Electronic supplementary material
The online version of this article (doi:10.1186/s12967-015-0619-5) contains supplementary material, which is available to authorized users.
Keywords: Advanced colorectal cancer, Bevacizumab, eNOS, VEGF, SNPs
Background
The therapeutic approach to metastatic colorectal cancer (mCRC) has changed in recent years, mainly thanks to the introduction of biologic drugs such as cetuximab, a monoclonal antibody (MoAb) directed against the epidermal growth factor receptor (EGFR), or bevacizumab, a MoAb that blocks the vascular endothelial growth factor (VEGF) [1]. As RAS-mutated patients show no benefit from anti-EGFR therapy, RAS mutations are used as a marker to select candidates for cetuximab treatment [2, 3]. However, they are not predictive of the efficacy of bevacizumab [4, 5], for which there are still no known biomarkers that are capable of distinguishing between responsive and non responsive patients. The correct selection of patients to be treated with bevacizumab-based chemotherapy could allow for the drug only to be given to those patients who will really benefit from it and for a reduction in the number of adverse effects.
Some studies have reported that specific VEGF single nucleotide polymorphisms (SNPs) would seem to affect gene transcription, with a consequent variation in VEGF expression [6, 7]. Other studies have evaluated the role of VEGF SNPs in relation to response to bevacizumab [8–12], the contradictory results reported possibly due to different study designs. In a retrospective study by Loupakis and colleagues, VEGF −1498 C/T variants proved capable of predicting response to bevacizumab plus FOLFIRI [11]. Similarly, in a more recent study [10], the same variants together with VEGF −2578 C/A were shown to predict response to bevacizumab treatment. A prospective study by Koutras and colleagues reported that only the VEGF −1154 G/A variants were associated with response and overall survival (OS) in patients treated with bevacizumab plus FOLFIRI or XELIRI [9]. The same VEGF SNPs were associated with progression-free survival (PFS) in another study [8] in which VEGF −634 G/C was associated with response. These SNPs have also been associated with cardiovascular adverse effects induced by bevacizumab, in particular, hypertension [10], and a correlation has been reported between response and bevacizumab-induced hypertension [13]. Recently, another study found that VEGF and endothelial nitric oxide synthase (eNOS) polymorphisms were associated with sunitinib-induced hypertension in patients with metastatic renal cancer, with grade three hypertension identified as an independent predictor of OS [14].
In the present study, we analyzed VEGF and eNOS polymorphisms in relation to clinical outcome (PFS, overall response rate [ORR] and OS) in mCRC patients undergoing bevacizumab-based chemotherapy in the phase III prospective multicentre randomized “Italian Trial in Advanced Colorectal Cancer (ITACa)” (EudraCT no. 2007-004539-44 and on ClinicalTrials.gov (NCT01878422).
Methods
Case series
The study was approved by the Local Ethics Committee (Comitato Etico Area Vasta Romagna e IRST) and informed consent was obtained from all patients before blood samples were obtained for genotype testing. Participation in the ITACa biological study was not mandatory for those taking part in the clinical trial. Of the 376 patients with mCRC enrolled onto the ITACa trial, 237 had sufficient biological material archived to be considered for this planned secondary analysis.
Inclusion criteria, patient characteristics, randomization strategy and the clinical results of the ITACa study are reported elsewhere [15]. Patients were randomized to receive first-line chemotherapy (CT) (FOLFOX4 or FOLFIRI) only or CT plus bevacizumab (B). FOLFOX4 consisted of oxaliplatin 85 mg/m2 as a 2-h infusion on day one and leucovorin 100 mg/m2 as a 2-h infusion followed by bolus 5-FU 400 mg/m2 and a 22-h infusion of 5-FU 600 mg/m2 on days 1–2 every 2 weeks. FOLFIRI consisted of the same 5-FU +leucovorin regimen with the addition of irinotecan 180 mg/m2 as a 90-min infusion on day one. B was administered as a 30- to 90-min intravenous infusion at a dose of 5 mg/kg on day 1 of each 2-week cycle. Treatment was to be continued until progressive disease (PD), withdrawal of consent or unacceptable toxicity, whichever came first. Tumor assessment tests were performed within 28 days of starting the study treatment and repeated every 8 weeks during treatment until PD.
The clinical characteristics of patients are represented in Table 1. One hundred and fourteen patients received CT + B and 123 patients received CT only (control group). We considered KRAS status as an independent variable because it was a stratification factor in the clinical study. Furthermore, to our knowledge, there are no significant data in the literature that attest to the fact that KRAS plays a role in response to bevacizumab.
Table 1.
Patient Characteristics
| Variable | CT + B (n = 114) n (%) | CT (n = 123) n (%) |
|---|---|---|
| Median age, years (range) | 66 (34–83) | 67 (37–82) |
| Gender | ||
| Male | 70 (61.4) | 74 (60.2) |
| Female | 44 (38.6) | 49 (39.8) |
| Performance status (ECOG) | ||
| 0 | 97 (85.1) | 102 (82.9) |
| 1 | 17 (14.9) | 21 (17.1) |
| Tumor localization | ||
| Rectum | 31 (27.2) | 34 (27.6) |
| Colon | 83 (72.8) | 89 (72.4) |
| Histology | ||
| Adenocarcinoma | 104 (91.2) | 119 (96.8) |
| Mucinous adenocarcinoma | 10 (8.8) | 4 (3.2) |
| Grade | ||
| 1 | 0 | 0 |
| 2 | 56 (64.4) | 67 (65.1) |
| 3 | 31 (35.6) | 36 (34.9) |
| Unknown | 27 | 20 |
| Stage at diagnosis | ||
| I–III | 29 (26.4) | 31 (27.2) |
| IV | 81 (73.4) | 83 (72.8) |
| Unknown | 4 | 9 |
| Chemotherapy regimen planned | ||
| FOLFOX4 | 69 (60.5) | 73 (59.4) |
| FOLFIRI | 45 (39.5) | 50 (40.6) |
| KRAS statusa | ||
| Wild type | 67 (59.8) | 69 (58.5) |
| Mutated | 45 (40.2) | 49 (41.5) |
| Unknown | 2 | 5 |
| Prior cancer therapy | ||
| Surgery | 88 (77.2) | 91 (74.0) |
| Radiotherapy | 11 (9.6) | 11 (8.9) |
| Adjuvant chemotherapy | 18 (15.8) | 17 (13.8) |
aMandatory as consequence of amendment n.1 of 3 May 2009.
All patients were evaluated for response [according to Response Evaluation Criteria in Solid Tumors (RECIST) guidelines], PFS and OS. In particular, response was classified as complete response (CR), partial response (PR), stable disease (SD) or PD, and patients with CR or PR were defined as responsive.
Genomic DNA extraction
Peripheral blood samples were available for polymorphism analysis in 153 patients, whereas only paraffin-embedded tumor samples were available for 84 patients.
Genomic DNA was extracted from whole blood using QIAamp DNA Minikit (Qiagen SPA, Milan, Italy) following the manufacturer’s protocol. DNA was extracted from formalin-fixed paraffin- embedded (FFPE) tumor tissue starting from 5-μM FFPE tissue sections. Tissue was lysed in 50 mM of KCl, 10 mM of Tris–HCl pH 8.0, 2.5 mM of MgCl2 and Tween-20 0.45%, supplemented with Proteinase K at a concentration of 1.25 mg/ml, overnight at 56°C. Proteinase K was inactivated at 95°C for 10 min, after which samples were centrifuged twice to eliminate debris. Supernatant was assessed for DNA quality and quantity by Nanodrop (Celbio Spa, Milan, Italy) and then underwent molecular analysis.
Genotyping analyses
Genotyping was performed for five VEGF SNPs (VEGF −2578C>A, −1498C>T, −1154G>A, −634C>G, +936C>T) and for two SNPs (eNOS −786T>C, +894G>T) and one variable number tandem repeat (VNTR) of 27 nucleotides for eNOS. The localizations and refSNP (rs) numbers of the different polymorphisms are shown in Fig. 1. All but eNOS −786 were analyzed by direct sequencing. The primer sequences and PCR conditions are reported in an Additional file 1. PCRs were performed starting from 50 ng of genomic DNA. eNOS-786 was analyzed by Real-Time PCR using a TaqMan SNP Genotyping assay (Assay ID C_15903863_10, Applied Biosystems, Foster City, CA, USA) and starting from 10 ng of DNA.
Fig. 1.
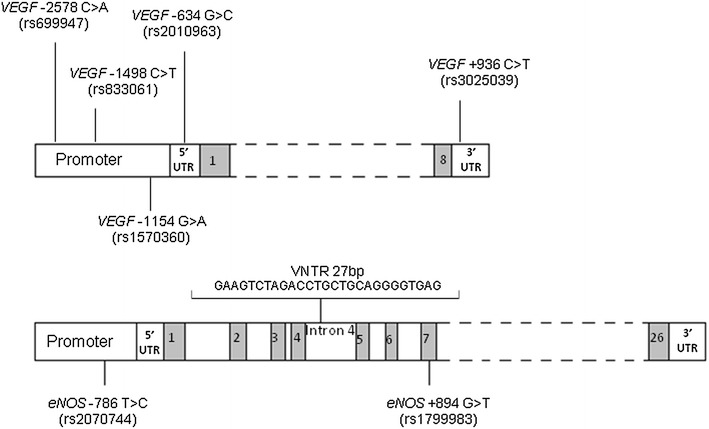
VEGF and eNOS polymorphisms (with rs reference numbers) analyzed in the study.
Statistical analysis
All polymorphisms were examined for deviation from Hardy–Weinberg equilibrium (HWE) by comparing actual allelic distributions with those expected from HWE using a χ2 test. Lewontin’s standardised disequilibrium coefficient (D′) among investigated polymorphisms was assessed using the HaploView programme [16]. The software provides the D′ coefficient as a measure of the non-random association of alleles at different loci. D′ coefficient is equal to one only if two SNPs have not been separated by recombination (or recurrent mutation) during the history of the sample [complete degree of linkage disequilibrium (LD)]. The same software was used to perform haplotype analysis.
The primary aim of the ITACa study was PFS. Secondary efficacy endpoints were ORR and OS. PFS was calculated from the date of randomization to the date of the first observation of disease progression or last follow-up or death in the absence of progressive disease. OS was calculated from the date of randomization to the date of death from any cause, or last follow-up. PFS, OS and their 95% confidence intervals (95% CI) were estimated using the Kaplan–Meier method.
SNPs and haplotypes and clinical outcomes were analyzed separately in each treatment group (CT + B and CT). Adjusted HRs by baseline characteristics (gender, age, performance status, KRAS status, tumor localization (rectum/colon) and chemotherapy regimen (FOLFOX4/FOLFIRI) were calculated using the Cox proportional-hazard model. Two-sided 95% CIs for each HR were provided. Covariate selection was based on a list of probable prognostic factors from the ITACa study [15]. Associations between polymorphisms or haplotypes and ORR (CR + PR) were analyzed by logistic regression models. Odds ratios (OR) and 95% CI were adjusted for gender, age, performance status, KRAS status, tumor localization (rectum/colon) and chemotherapy regimen (FOLFOX4/FOLFIRI).
All P values were based on two-sided testing; to mitigate the issue of multiple testing, a false discovery rate (FDR) of less than 10% was used to determine polymorphisms or haplotypes associated with PFS, OS and ORR. FDR was controlled using the Benjamini-Hochberg step-up procedure [17]. The effect of the interaction between SNPs or haplotypes and treatment on PFS was evaluated using Cox regression models of the entire population (CT + B and CT arms) that included SNPs or haplotypes, treatment and treatment-by-SNPs or -haplotypes. Statistical analyses were performed using SAS Statistical software version 9.3 (SAS Inc., Cary, NC, USA).
Results
We previously demonstrated that VEGF and eNOS polymorphism analysis showed concordant results regardless of starting material used (FFPE or blood sample) in all but the VEGF −1154G>A SNP [18]. On the basis of this observation, VEGF −1154G>A was only analyzed in patients for whom peripheral blood samples were available (153 patients).
The observed allele distributions of VEGF −2578, −1498, −1154, −634, +936 polymorphisms and eNOS +894, −786, VNTR 4a/b are shown in an Additional file 2; all were in HWE (P = 0.95; P = 0.95, P = 0.12, P = 0.30, P = 0.91, P = 0.50, P = 0.85, P = 0.26 respectively).
In accordance with the primary endpoint of the ITACA trial, we analyzed the association between the different polymorphisms and PFS in the CT + B and CT only groups. At a median follow-up of 36 months (range 1–65), there had been 103 (90.4%) and 115 (93.5%) progressions and 82 (71.9%) and 91 (74.0) deaths in the CT + B and CT groups, respectively.
In the CT + B group, only the VEGF +936 T/C polymorphism was significantly associated with PFS; in particular, the VEGF +936 TT genotype was associated with a shorter median PFS compared with other genotypes (7.8 months, 95% CI 1.7–9.1 vs. 10.2 months, 95% CI 9.0–12.4, P = 0.036) (Table 2). No statistically significant differences were observed in the CT-only group (Table 2). Of note, the p value did not reach the P value threshold adjusted for multiple testing, possibly due to the small number of patients (3) with a VEGF +936 TT genotype. eNOS +894 G/T was also associated with PFS, and patients with eNOS +894 G/T showed a shorter PFS (8.9 months, range 6.8–10.2 months) than those with eNOS +894 GG/TT (11.9 months, range 9.6–14.1 months, P = 0.013) in the CT + B arm (Table 2; Additional file 3: Figure S1, panel A). This polymorphism was statistically significant after FDR correction. Conversely, no differences were observed in the control group (Table 2, Additional file 3: Figure S1, panel B). Moreover, eNOS VNTR 4a/b was associated with PFS in the CT + B arm. Patients homozygous for the five repetitions (VNTR 4bb) showed a longer PFS (10.9 months, range 9.1–12.9 months) than those with other genotypes (9.1 months, range 6.2–11.3 months, P = 0.034) (Table 2; Additional file 3: Figure S1, panel C). No statistically significant differences were observed in the control group (Table 2, Additional file 3: Figure S1, panel D).
Table 2.
Association between VEGF and eNOS polymorphisms and progression–free survival (PFS)
| Polymorphisms | CT + B | CT | ||||
|---|---|---|---|---|---|---|
| Median PFS (95% CI) | HR (95% CI) | P* | Median PFS (95% CI) | HR (95% CI) | P* | |
| VEGF −2578 | ||||||
| AA | 9.3 (3.1–12.5) | 1.18 (0.72–1.93) | 9.1 (7.8–11.4) | 1.27 (0.81–1.99) | ||
| CC/CA | 10.4 (8.9–12.4) | 1.00 | 0.515 | 9.0 (7.8–10.3) | 1.00 | 0.304 |
| VEGF −1498 | ||||||
| CC | 9.1 (6.4–12.5) | 1.30 (0.81–2.11) | 9.1 (7.8–11.4) | 1.21 (0.77–1.90) | ||
| TT/CT | 10.7 (9.1–12.4) | 1.00 | 0.277 | 9.0 (7.8–10.3) | 1.00 | 0.406 |
| VEGF −1154 | ||||||
| AA | 11.5 (2.3–18.5) | 1.09 (0.54–2.21) | 9.1 (3.1–12.2) | 1.74 (0.89–3.38) | ||
| GA/GG | 10.3 (8.3–12.9) | 1.00 | 0.808 | 9.6 (8.9–11.3) | 1.00 | 0.105 |
| VEGF −634 | ||||||
| GC | 9.1 (7.5–11.3) | 1.21 (0.81–1.82) | 9.0 (7.0–10.3) | 1.14 (0.77–1.68) | ||
| GG/CC | 11.7 (9.1–12.9) | 1.00 | 0.356 | 9.1 (8.0–11.3) | 1.00 | 0.513 |
| VEGF +936 | ||||||
| TT | 7.8 (1.7–9.1) | 3.63 (1.09–12.14) | 28.0 (–) | 0.34 (0.04–2.76) | ||
| CT/CC | 10.2 (9.0–12.4) | 1.00 | 0.036 | 9.1 (8.3–10.2) | 1.00 | 0.311 |
| eNOS +894 | ||||||
| GT | 8.9 (6.8–10.2) | 1.70 (1.12–2.60) | 9.0 (7.4–9.6) | 1.06 (0.73–1.54) | ||
| GG/TT | 11.9 (9.6–14.1) | 1.00 | 0.013 | 10.0 (8.3–11.4) | 1.00 | 0.773 |
| eNOS VNTR | ||||||
| 4bb | 10.9 (9.1–12.9) | 0.63 (0.41–0.96) | 9.1 (8.3–10.3) | 1.09 (0.69–1.74) | ||
| 4ab/4aa | 9.1 (6.2–11.3) | 1.00 | 0.034 | 8.9 (6.1–11.6) | 1.00 | 0.708 |
| eNOS −786 | ||||||
| CC | 12.7 (4.7–14.3) | 0.90 (0.52–1.56) | 8.9 (4.2–11.5) | 1.17 (0.68–2.03) | ||
| CT/TT | 9.6 (8.5–11.3) | 1.00 | 0.709 | 9.1 (8.6–10.3) | 1.00 | 0.572 |
*Adjusted for CT (FOLFOX4/FOLFIRI), gender, age, KRAS status, tumor localization (rectum/colon).
Formal tests of interaction between SNPs and treatment were not significant.
Polymorphisms were also investigated in relation to ORR and OS. For VEGF SNPs, only VEGF −634 G/C was associated with ORR, a lower rate seen in heterozygous patients compared to the other genotypes (P = 0.017) (see Additional file 4). With regard to eNOS, eNOS +894 G/T was significantly associated with ORR, heterozygous patients showing a lower ORR (42.5%) than the other genotypes (63.1%) (P = 0.030) (see Additional file 4). No polymorphism reached the P value threshold adjusted for multiple testing. No significant associations were observed between VEGF and eNOS polymorphisms and ORR in the control group (data not shown).
With regard to OS, patients bearing the VEGF −634 GC genotype showed a shorter OS (19.3 months, 95% CI 13.1–22.0) than those with the VEGF −634 GG/CC genotype (29.1 months, 95% CI 20.9–33.5), although the difference was not statistically significant (P = 0.064) (Table 3). No statistically significant differences were observed in the control group (Table 3). Moreover, patients bearing the VEGF +936 TT genotype showed a significantly shorter median OS than VEGF +936 TC/CC patients (8.6 months, 95% CI 7.9–13.9 vs 22.7 months, 95% CI 20.5–27.5, respectively, P = 0.007; these data remained statistically significant after FDR correction) (Table 3). With regard to eNOS polymorphisms and OS, eNOS +894 G/T was again found to be associated with outcome. In particular, patients bearing the eNOS +894 GT genotype showed a shorter OS (20.1 months, 95% CI 12.0–23.2) compared to eNOS +894 GG/TT patients (26.1 months, 95% CI 21.0–33.5, P = 0.014) (Table 3). These data remained statistically significant after FDR correction. No statistically significant differences were observed in the control group (Table 3). Finally, eNOS VNTR 4a/b was also associated with OS, and patients with a VNTR 4bb genotype showed a longer OS (24.8 months, 95% CI 20.1–34.5) compared to those with the eNOS VNTR 4ab/aa genotype (20.6 months, 95% CI 13.7–24.7, P = 0.015; not significant after FDR correction) (Table 3). No differences were observed in the control group (Table 3).
Table 3.
Association between VEGF and eNOS polymorphisms and overall survival (OS)
| Polymorphisms | CT + B | CT | ||||
|---|---|---|---|---|---|---|
| Median OS (95% CI) | HR (95% CI) | P* | Median OS (95% CI) | HR (95% CI) | P* | |
| VEGF −2578 | ||||||
| AA | 26.1 (9.0–34.5) | 1.05 (0.61–1.81) | 24.0 (14.4–36.7) | 1.11 (0.67–1.85) | ||
| CC/CA | 21.4 (19.3–27.2) | 1.00 | 0.854 | 20.8 (19.2–24.5) | 1.00 | 0.671 |
| VEGF −1498 | ||||||
| CC | 26.1 (10.4–33.1) | 1.12 (0.66–1.91) | 26.6 (14.4–36.7) | 0.95 (0.56–1.59) | ||
| TT/CT | 21.8 (19.3-27.2) | 1.00 | 0.664 | 20.8 (18.8–24.3) | 1.00 | 0.834 |
| VEGF −1154 | ||||||
| AA | 21.8 (2.3–30.4) | 1.18 (0.53–2.63) | 20.2 (11.1–29.2) | 1.92 (0.96–3.85) | ||
| GA/GG | 21.4 (14.6–28.8) | 1.00 | 0.686 | 25.2 (19.2–29.1) | 1.00 | 0.066 |
| VEGF −634 | ||||||
| GC | 19.3 (13.1–22.0) | 1.54 (0.98–2.44) | 20.2 (16.8–24.3) | 1.18 (0.76–1.82) | ||
| GG/CC | 29.1 (20.9–33.5) | 1.00 | 0.064 | 24.3 (20.2–29.2) | 1.00 | 0.456 |
| VEGF +936 | ||||||
| TT | 8.6 (7.9–13.9) | 5.48 (1.60–18.8) | 28.0 (–) | 0.96 (0.11–7.98) | ||
| CT/CC | 22.7 (20.5–27.5) | 1.00 | 0.007 | 21.3 (19.2–25.2) | 1.00 | 0.967 |
| eNOS +894 | ||||||
| GT | 20.1 (12.0–23.2) | 1.80 (1.12–2.89) | 24.3 (17.9–28.6) | 0.82 (0.53–1.25) | ||
| GG/TT | 26.1 (21.0–33.5) | 1.00 | 0.014 | 21.3 (19.2–26.4) | 1.00 | 0.356 |
| eNOS VNTR | ||||||
| 4bb | 24.8 (20.1–34.5) | 0.54 (0.33–0.89) | 23.6 (19.9–28.0) | 0.76 (0.46–1.23) | ||
| 4ab/4aa | 20.6 (13.7–24.7) | 1.00 | 0.015 | 20.1 (15.0–23.3) | 1.00 | 0.259 |
| eNOS −786 | ||||||
| CC | 27.2 (14.6–33.5) | 0.97 (0.53–1.80) | 20.4 (16.0–21.7) | 1.40 (0.77–2.55) | ||
| CT/TT | 21.3 (16.4–27.4) | 1.00 | 0.931 | 23.6 (19.9–28.0) | 1.00 | 0.270 |
*Adjusted for CT (FOLFOX4/FOLFIRI), gender, age, KRAS status, tumor localization (rectum/colon).
Haplotype analysis
Haplotype analysis was performed to evaluate the combined effect of SNPs in the promoter, 5′UTR and 3′UTR of the VEGF gene on treatment response. Analysis showed a single block of high linkage disequilibrium formed by three VEGF polymorphisms upstream of the coding sequence (promoter and 5′ UTR). Three haplotypes based on VEGF −2578 C/A, −1498 C/T and −634 G/C were defined on the basis of the population frequencies of the three SNPs (VEGF Haplo1: A–C–G 46.6%; VEGF Haplo 2: C–T–C 34%; and VEGF Haplo 3: C–T–G 16.5%). None of these haplotypes were significantly associated with clinical outcome. Haplotype analysis of eNOS polymorphisms showed a strong linkage disequilibrium between eNOS VNTR4a/b and eNOS +894 G/T (correlation coefficient, r2 = 0.084; Lewontin’s D′ = 0.926) and eNOS VNTR 4a/b and eNOS −786 T/C (r2 = 0.217, D′ = 0.903). Moreover, a weak correlation was found between eNOS +894 G/T and eNOS −786 T/C polymorphisms (r2 = 0.156, D′ = 0.456). Three haplotypes based on eNOS VNTR 4a/b and eNOS +894 G/T were defined: eNOS Haplo 1 (4b-G, 50.2%), eNOS Haplo 2 (4b-T, 34.1%) and eNOS Haplo 3 (4a-G, 15.3%).
In the CT + B arm, patients homozygous for eNOS Haplo 1 (eNOS Haplo 1/Haplo 1) and the group composed of eNOS Haplo 1/Haplo 1 patients and individuals homozygous for Haplo 2 (eNOS Haplo 2/Haplo 2) showed a significantly improved outcome compared to the other patients. In particular, a longer median PFS was observed in eNOS Haplo1/Haplo1 patients compared to the others in the CT + B group [17.8 months (95% CI 8.1–22.3) vs 9.6 (95% CI 8.3–10.9) (P = 0.004)]; this was not observed in the CT only arm (10.3, 95% CI 8.0–15.0, vs. 9.0, 95% CI 7.8–9.6, P = 0.123) (Table 4; Fig. 2a, b). More significant results were observed in the CT + B group when eNOS Haplo1/Haplo1 and eNOS Haplo 2/Haplo 2 patients were combined, with a median PFS of 15.0 months (95% CI 10.6–18.7) compared to 9.1 (95% CI 7.4–10.1) months for those with other genotypes (P = 0.001). Both eNOS haplotyes reached the P value threshold adjusted for FDR correction. No significant differences were observed in the control group (10.3, 95% CI 8.3–11.5, vs 9.0, 95% CI 7.2–9.6, months, P = 0.542) (Table 4; Fig. 2c, d).
Table 4.
Association between eNOS Haplotypes and PFS and OS
| eNOS haplotypes | CT + B | CT | ||||||
|---|---|---|---|---|---|---|---|---|
| n | Median PFS (95% CI) | HR (95% CI) | P* | n | Median PFS (95% CI) | HR (95% CI) | P* | |
| Haplo1/Haplo1 | 24 | 17.8 (8.1–22.3) | 0.46 (0.27–0.78) | 33 | 10.3 (8.0–15.0) | 0.71 (0.46–1.10) | ||
| Other | 90 | 9.6 (8.3–10.9) | 1.00 | 0.004 | 86 | 9.0 (7.8–9.6) | 1.00 | 0.123 |
| Haplo2/Haplo2 | 15 | 13.1 (7.2–15.7) | 0.82 (0.46–1.46) | 16 | 9.9 (5.9–11.5) | 1.44 (0.82–2.51) | ||
| Other | 99 | 9.6 (8.3–11.3) | 1.00 | 0.501 | 107 | 9.0 (8.3–10.2) | 1.00 | 0.199 |
| Haplo1/Haplo1 + Haplo2/Haplo2 | 39 | 15.0 (10.6–18.7) | 0.48 (0.30–0.75) | 49 | 10.3 (8.3–11.5) | 0.88 (0.60–1.31) | ||
| Other | 75 | 9.1 (7.4–10.1) | 1.00 | 0.001 | 70 | 9.0 (7.2–9.6) | 1.00 | 0.542 |
| eNOS haplotypes | CT + B | CT | ||||||
|---|---|---|---|---|---|---|---|---|
| n | Median OS (95% CI) | HR (95% CI) | P* | n | Median OS (95% CI) | HR (95% CI) | P* | |
| Haplo1/Haplo1 | 24 | 31.6 (19.3–nr) | 0.46 (0.24–0.86) | 33 | 23.2 (16.8–39.7) | 0.80 (0.49–1.31) | ||
| Other | 90 | 21.3 (15.9–25.2) | 1.00 | 0.016 | 86 | 20.8 (18.2–24.5) | 1.00 | 0.379 |
| Haplo2/Haplo2 | 15 | 34.5 (13.1–42.9) | 0.70 (0.37–1.31) | 16 | 21.3 (14.4–26.4) | 1.35 (0.73–2.50) | ||
| Other | 99 | 21.3 (16.4–24.7) | 1.00 | 0.260 | 107 | 21.6 (19.2–27.1) | 1.00 | 0.331 |
| Haplo1/Haplo1 + Haplo2/Haplo2 | 39 | 34.5 (23.4–38.4) | 0.42 (0.25–0.72) | 49 | 21.7 (18.8–29.6) | 0.95 (0.61–1.48) | ||
| Other | 75 | 20.5 (14.4–22.7) | 1.00 | 0.002 | 70 | 20.8 (18.2–27.1) | 1.00 | 0.829 |
*Adjusted for CT (FOLFOX4/FOLFIRI), gender, age, KRAS status, tumor localization (rectum/colon).
Fig. 2.
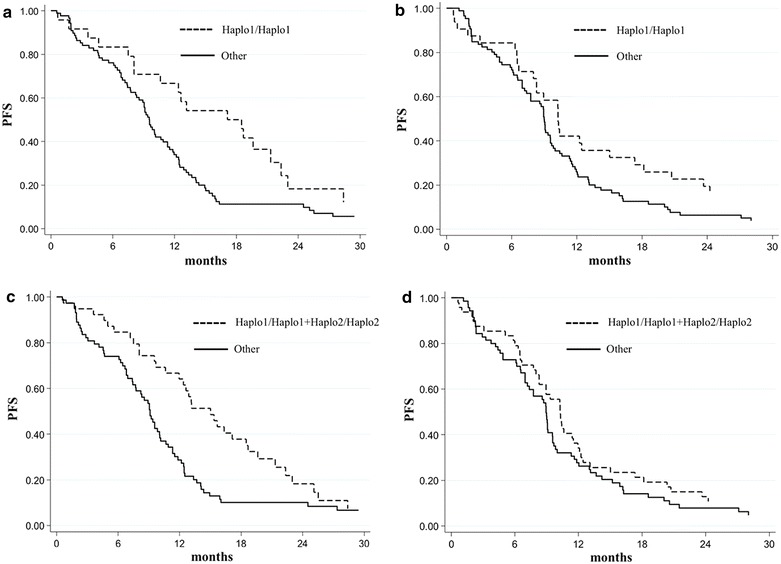
PFS in relation to Haplo1/Haplo1 (top panels) or Haplo1/Haplo1 plus Haplo2/Haplo2 (bottom panels) genotypes in patients treated with CT + B (a, c) or CT (b, d).
Formal tests of interaction between haplotypes and treatment were not significant.
Moreover, a 71% ORR was observed in Haplo1/Haplo1 and Haplo2/Haplo2 patients compared to 45.9% in patients with other genotypes (P = 0.013) (see Additional file 5). We also analyzed eNOS haplotypes in relation to OS. Patients with eNOS Haplo1/Haplo1 showed a longer median OS (31.6 months, 95% CI 19.3-not reached) than those with other genotypes (21.3, 95% CI 15.9–25.2) (P = 0.016), the statistical significance was more evident for eNOS Haplo1/Haplo1 and eNOS Haplo2/Haplo2 patients (34.5, 95% CI 23.4–38.4, vs 20.5, 95% CI 14.4–22.7, respectively, P = 0.002) (Table 4). This latter eNOS haplotype passed the FDR correction. No differences were observed within the control group in relation to these different genotypes (Table 4). The results obtained were independent of KRAS status.
Interestingly, with regard to the other genotypes, no differences in PFS or OS were observed between patients who were treated or not with B (median PFS 9.1 vs 9.0 months and median OS 20.5 vs 20.8 months, respectively). Conversely, the benefit of B was clearly visible in patients carrying the identified haplotype combination (Table 4).
Discussion
The present study analyzed VEGF and eNOS polymorphisms in relation to clinical outcome in patients with metastatic colorectal cancer receiving bevacizumab-based chemotherapy. Although numerous studies have reported significant results regarding VEGF polymorphisms, others have failed to show such associations, perhaps because of different study designs. A retrospective study by Loupakis and colleagues [11], hypothesized a role of the VEGF −1498 C/T polymorphism as a predictive biomarker of bevacizumab efficacy, showing that patients with a VEGF −1498 TT genotype had a worse prognosis. However, the same authors did not confirm this hypothesis in a subsequent prospective study [12] in which only another SNP, VEGFR2 rs12505758, was found to be significantly correlated with PFS. In another retrospective study, VEGF −1498 C/T and −2578 A/C were found to be correlated with outcome. In particular, the VEGF −2578 CC and −1498 CC genotypes were associated with lower response and hypertension [10]. In other prospective studies, VEGF −1154 G/A [9] and VEGF −634 G/C [8] were significantly correlated with patient outcome. However, neither study had a chemotherapy only (control) group, making it impossible to reach definitive conclusions.
One strength of our study was the fact that molecular analyses were performed on patients enrolled onto a randomized, prospective phase III multicentre study (ITACa trial) in which two treatment arms were analyzed: chemotherapy plus bevacizumab vs chemotherapy only (highest level of evidence). Our results did not confirm the predictive value of VEGF −2578, −1498 and −1154 polymorphisms, whereas VEGF −634 was found to be associated with OS. In particular, patients with a heterozygous genotype showed a significantly lower ORR and a lower OS with a trend toward statistical significance. The poorer outcome observed with the heterozygous genotype suggests that the presence of both alleles enhance their negative effect. Moreover, in our case series, the three patients with a VEGF +936 TT showed a shorter PFS and a substantially shorter OS. This finding, albeit based on a small number of patients, remained statistically significant after multiple testing corrections and might be worth validating in a larger case series.
The novelty of our work lies in its analysis of eNOS polymorphisms in relation to the clinical outcome of patients treated with bevacizumab. Our results show that eNOS +894 G/T and eNOS VNTR 4a/b were the most interesting polymorphisms. In particular, we identified a specific haplotype (eNOS Haplo1/Haplo1, characterised by eNOS +894GG and eNOS VNTR 4bb) that was significantly associated with improved PFS and OS. Moreover, the combination of eNOS Haplo1/Haplo1 and eNOS Haplo 2/Haplo2 (characterised by eNOS +894TT and eNOS VNTR 4bb) accurately identified patients with a better ORR, PFS and OS. Interestingly, no significant associations were found in the group of patients treated with chemotherapy only, reinforcing the predictive value of the haplotypes in relation to bevacizumab efficacy.
eNOS is a constitutively expressed gene in endothelium involved in the production of nitric oxide (NO), which plays a central role in maintaining endothelial cell functional integrity, regulating hemodynamics, and establishing collateral circulation [19]. Adequate NO production, consequent to adequate eNOS expression and activity, is essential for preventing thrombotic and atherogenic processes [20]. It has been shown that VEGF inhibition induces a decrease in eNOS expression and thus in NO production [21], and that this phenomenon is linked to the induction of hypertension, one of the most common dose-limiting toxicities of VEGF inhibitors [22]. Previous studies have demonstrated an association between specific eNOS polymorphisms and hypertension [14, 23]. A positive correlation between the induction of hypertension and the clinical benefit of bevacizumab has also been observed [13]. Although we did not observe a statistical significance between eNOS polymorphisms and hypertension (data not shown), we did find that eNOS genotypes associated with a better outcome were also associated with a trend towards higher grade hypertension. Intron 4 eNOS VNTR polymorphism plays a role in regulating eNOS expression by acting as an enhancer/repressor and by coding for a 27-nt small RNA which appears to inhibit eNOS expression at the transcriptional level [24–27]. The higher the number of 27-nt repeats, the more 27nt sir-RNA is produced, inhibiting eNOS expression. However, the association between eNOS VNTR in intron 4 and eNOS expression is still a much debated issue [28–30]. Our results showed that patients homozygous for the five repetitions (4bb), who presumably had a lower eNOS expression, showed a better response to bevacizumab. With respect to eNOS +894, it has been demonstrated that the +894 TT genotype is associated with lower eNOS activity [31–33]. In our study, the haplotype most frequently associated with better PFS and OS was the one homozygous for eNOS VNTR 4bb and eNOS +894 TT. However, the association with the haplotype homozygous for eNOS VNTR 4bb and eNOS +894 GG was also significantly associated with outcome. These results suggest that eNOS VNTR 4bb is the genotype most strongly correlated with response to bevacizumab. It also implies that, as eNOS is not the direct target of bevacizumab, other factors may be involved in the relation between eNOS activity and bevacizumab efficacy. In particular, it is possible that the variants are in linkage disequilibrium with other functional variants in the regulatory regions of the eNOS gene.
Our study was carried out on 63% (237/376) of the patients enrolled onto the ITACa study, a much higher percentage than those reported by other authors (26% for the AViTA trial and 17% for the AVOREN trial) [34]. This relatively low number of patients did not allow us to reach a sufficient statistical power to test the formal interaction between SNPs and clinical outcome or to consider our results definitively validated. Thus, although the work was based on patients from a randomized clinical trial with a control arm and SNP determinations were prospectively planned and centrally performed, our findings require further validation in independent and larger case series before they can be implemented into clinical practice.
Conclusions
In conclusion, we identified a haplotype combination of eNOS polymorphisms capable of identifying patients who may/will probably benefit from bevacizumab-based chemotherapy. No advantage was observed from the use of bevacizumab in patients not harboring the identified haplotype combination, whereas those carrying the specific genotype showed a significant improvement in ORR, PFS and OS. If confirmed in future studies, this haplotype combination could represent a valid criterion for selecting candidates for treatment with bevacizumab.
Authors’ contributions
PU, ES, AP, GM, DC, WZ, MDR, GLF, DT, ST, BV and DA wrote the manuscript. PU, ES, AP, DC, WZ and DA designed the research. AP, WZ, GLF, DT, ST, BV, PU, ES and GM performed the research. PU, ES, AP, DC, MDR and GLF analyzed the data. All authors read and approved the final manuscript.
Acknowledgements
The authors thank Ursula Elbling for editing the manuscript. Collaborating authors: Manuela Fantini, Department of Oncology, Per gli Infermi Hospital, Rimini; Antonio Polselli, Oncology Unit, Cervesi Hospital, Cattolica; Eva Freier, Oncology Unit, Degli Infermi Hospital, Faenza; Alberto Verlicchi, Oncology Unit, S. Maria delle Croci Hospital, Ravenna; Francesca Fabbri and Oriana Nanni, Unit of Biostatistics and Clinical Trials, IRST IRCCS, Meldola, Italy.
Grant support
This study was partially funded by Roche S.p.A. and the Italian Medicines Agency (AIFA).
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Abbreviations
- mCRC
metastatic colorectal cancer
- VEGF
vascular endothelial growth factor
- eNOS
endothelial nitric oxide synthase
- SNPs
single nucleotide polymorphisms
- VNTR
variable number tandem repeat
- PFS
progression-free survival
- ORR
objective response rate
- OS
overall survival
- mCRC
metastatic colorectal cancer
- MoAb
monoclonal antibody
- EGFR
epidermal growth factor receptor
- PD
progression disease
- CR
complete response
- PR
partial response
- SD
stable disease
- FFPE
formalin-fixed paraffin- embedded
- rs
refSNP
- LD
linkage disequilibrium
- FDR
false discovery rate
Additional files
Primer sequences for VEGF and eNOS SNPs.
Genotype distribution of VEGF and eNOS polymorphisms.
Figure S1. PFS in relation to eNOS +894 (top panels) and VNTR 4ab (bottom panels) polymorphisms in patients treated with CT + B (A, C) or CT alone (B, D).
Correlations between VEGF and eNOS polymorphisms and overall response rate (ORR) in CT+B arm.
Correlation between eNOS haplotypes and ORR.
Footnotes
Paola Ulivi and Emanuela Scarpi contributed equally to this work
Contributor Information
Paola Ulivi, Email: paola.ulivi@irst.emr.it.
Emanuela Scarpi, Email: emanuela.scarpi@irst.emr.it.
Alessandro Passardi, Email: alessandro.passardi@irst.emr.it.
Giorgia Marisi, Email: giorgia.marisi@irst.emr.it.
Daniele Calistri, Email: daniele.calistri@irst.emr.it.
Wainer Zoli, Email: wainer.zoli@irst.emr.it.
Marzia Del Re, Email: marzia.delre@gmail.com.
Giovanni Luca Frassineti, Email: luca.frassineti@irst.emr.it.
Davide Tassinari, Email: dtassinari@rimini.com.
Stefano Tamberi, Email: s.tamberi@ausl.ra.it.
Bernadette Vertogen, Email: bernadette.vertogen@irst.emr.it.
Dino Amadori, Email: direzione.scientifica@irst.emr.it.
References
- 1.Banerjee S, Flores-Rozas H. Monoclonal antibodies for targeted therapy in colorectal cancer. Cancer Biol Ther. 2010;9:563–571. doi: 10.4161/cbt.9.8.11403. [DOI] [PubMed] [Google Scholar]
- 2.Lievre A, Bachet JB, Le Corre D, Boige V, Landi B, Emile JF, et al. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 2006;66:3992–3995. doi: 10.1158/0008-5472.CAN-06-0191. [DOI] [PubMed] [Google Scholar]
- 3.Van Cutsem E, Kohne CH, Hitre E, Zaluski J, Chang Chien CR, Makhson A, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360:1407–1408. doi: 10.1056/NEJMoa0805019. [DOI] [PubMed] [Google Scholar]
- 4.Price TJ, Bruhn MA, Lee CK, Hardingham JE, Townsend AR, Mann KP, et al. Correlation of extended RAS and PIK3CA gene mutation status with outcomes from the phase III AGITG MAX STUDY involving capecitabine alone or in combination with bevacizumab plus or minus mitomycin C in advanced colorectal cancer. Br J Cancer. 2015;112:963–970. doi: 10.1038/bjc.2015.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hurwitz HI, Yi J, Ince W, Novotny WF, Rosen O. The clinical benefit of bevacizumab in metastatic colorectal cancer is independent of K-ras mutation status: analysis of a phase III study of bevacizumab with chemotherapy in previously untreated metastatic colorectal cancer. Oncologist. 2009;14:22–28. doi: 10.1634/theoncologist.2008-0213. [DOI] [PubMed] [Google Scholar]
- 6.Renner W, Kotschan S, Hoffmann C, Obermayer-Pietsch B, Pilger E. A common 936 C/T mutation in the gene for vascular endothelial growth factor is associated with vascular endothelial growth factor plasma levels. J Vasc Res. 2000;37:443–448. doi: 10.1159/000054076. [DOI] [PubMed] [Google Scholar]
- 7.Watson CJ, Webb NJ, Bottomley MJ, Brenchley PE. Identification of polymorphisms within the vascular endothelial growth factor (VEGF) gene: correlation with variation in VEGF protein production. Cytokine. 2000;12:1232–1235. doi: 10.1006/cyto.2000.0692. [DOI] [PubMed] [Google Scholar]
- 8.Formica V, Palmirotta R, Del Monte G, Savonarola A, Ludovici G, De Marchis ML, et al. Predictive value of VEGF gene polymorphisms for metastatic colorectal cancer patients receiving first-line treatment including fluorouracil, irinotecan, and bevacizumab. Int J Colorectal Dis. 2011;26:143–151. doi: 10.1007/s00384-010-1108-1. [DOI] [PubMed] [Google Scholar]
- 9.Koutras AK, Antonacopoulou AG, Eleftheraki AG, Dimitrakopoulos FI, Koumarianou A, Varthalitis I, et al. Vascular endothelial growth factor polymorphisms and clinical outcome in colorectal cancer patients treated with irinotecan-based chemotherapy and bevacizumab. Pharmacogenomics J. 2012;12:468–475. doi: 10.1038/tpj.2011.37. [DOI] [PubMed] [Google Scholar]
- 10.Morita S, Uehara K, Nakayama G, Shibata T, Oguri T, Inada-Inoue M, et al. Association between bevacizumab-related hypertension and vascular endothelial growth factor (VEGF) gene polymorphisms in Japanese patients with metastatic colorectal cancer. Cancer Chemother Pharmacol. 2013;71:405–411. doi: 10.1007/s00280-012-2028-2. [DOI] [PubMed] [Google Scholar]
- 11.Loupakis F, Ruzzo A, Salvatore L, Cremolini C, Masi G, Frumento P, et al. Retrospective exploratory analysis of VEGF polymorphisms in the prediction of benefit from first-line FOLFIRI plus bevacizumab in metastatic colorectal cancer. BMC Cancer. 2011;11:247. doi: 10.1186/1471-2407-11-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loupakis F, Cremolini C, Yang D, Salvatore L, Zhang W, Wakatsuki T, et al. Prospective validation of candidate SNPs of VEGF/VEGFR pathway in metastatic colorectal cancer patients treated with first-line FOLFIRI plus bevacizumab. PLoS One. 2013;8:e66774. doi: 10.1371/journal.pone.0066774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tahover E, Uziely B, Salah A, Temper M, Peretz T, Hubert A. Hypertension as a predictive biomarker in bevacizumab treatment for colorectal cancer patients. Med Oncol. 2013;30:327. doi: 10.1007/s12032-012-0327-4. [DOI] [PubMed] [Google Scholar]
- 14.Eechoute K, van der Veldt AA, Oosting S, Kappers MH, Wessels JA, Gelderblom H, et al. Polymorphisms in endothelial nitric oxide synthase (eNOS) and vascular endothelial growth factor (VEGF) predict sunitinib-induced hypertension. Clin Pharmacol Ther. 2012;92:503–510. doi: 10.1038/clpt.2012.136. [DOI] [PubMed] [Google Scholar]
- 15.Passardi A, Nanni O, Tassinari D, Turci D, Cavanna L, Fontana A, et al. Effectiveness of bevacizumab added to standard chemotherapy in metastatic colorectal cancer: final results for first-line treatment from the ITACa randomized clinical trial. Ann Oncol. 2015;26:1201–1207. doi: 10.1093/annonc/mdv130. [DOI] [PubMed] [Google Scholar]
- 16.Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–265. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- 17.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B (Methodological) 1995;57:289–300. [Google Scholar]
- 18.Marisi G, Passardi A, Calistri D, Zoli W, Amadori D, Ulivi P. Discrepancies between VEGF −1154G>A polymorphism analysis performed in peripheral blood samples and FFPE tissue. Int J Mol Sci. 2014;15:13333–13343. doi: 10.3390/ijms150813333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gibbons GH, Dzau VJ. The emerging concept of vascular remodeling. N Engl J Med. 1994;330:1431–1438. doi: 10.1056/NEJM199405193302008. [DOI] [PubMed] [Google Scholar]
- 20.Oemar BS, Tschudi MR, Godoy N, Brovkovich V, Malinski T, Luscher TF. Reduced endothelial nitric oxide synthase expression and production in human atherosclerosis. Circulation. 1998;97:2494–2498. doi: 10.1161/01.CIR.97.25.2494. [DOI] [PubMed] [Google Scholar]
- 21.Winnik S, Lohmann C, Siciliani G, von Lukowicz T, Kuschnerus K, Kraenkel N, et al. Systemic VEGF inhibition accelerates experimental atherosclerosis and disrupts endothelial homeostasis—implications for cardiovascular safety. Int J Cardiol. 2013;168:2453–2461. doi: 10.1016/j.ijcard.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 22.Facemire CS, Nixon AB, Griffiths R, Hurwitz H, Coffman TM. Vascular endothelial growth factor receptor 2 controls blood pressure by regulating nitric oxide synthase expression. Hypertension. 2009;54:652–658. doi: 10.1161/HYPERTENSIONAHA.109.129973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang B, Xu JR, Liu XM, Yang Y, Na XF, Li M, et al. Polymorphisms of rs1799983 (G > T) and rs1800780 (A > G) of the eNOS gene associated with susceptibility to essential hypertension in the Chinese Hui ethnic population. Genet Mol Res. 2013;12:3821–3829. doi: 10.4238/2013.March.26.2. [DOI] [PubMed] [Google Scholar]
- 24.Wang J, Dudley D, Wang XL. Haplotype-specific effects on endothelial NO synthase promoter efficiency: modifiable by cigarette smoking. Arterioscler Thromb Vasc Biol. 2002;22:e1–e4. doi: 10.1161/01.ATV.0000016248.51577.1F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Senthil D, Raveendran M, Shen YH, Utama B, Dudley D, Wang J, et al. Genotype-dependent expression of endothelial nitric oxide synthase (eNOS) and its regulatory proteins in cultured endothelial cells. DNA Cell Biol. 2005;24:218–224. doi: 10.1089/dna.2005.24.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang MX, Ou H, Shen YH, Wang J, Wang J, Coselli J, et al. Regulation of endothelial nitric oxide synthase by small RNA. Proc Natl Acad Sci USA. 2005;102:16967–16972. doi: 10.1073/pnas.0503853102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ou H, Shen YH, Utama B, Wang J, Wang X, Coselli J, et al. Effect of nuclear actin on endothelial nitric oxide synthase expression. Arterioscler Thromb Vasc Biol. 2005;25:2509–2514. doi: 10.1161/01.ATV.0000189306.99112.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsukada T, Yokoyama K, Arai T, Takemoto F, Hara S, Yamada A, et al. Evidence of association of the ecNOS gene polymorphism with plasma NO metabolite levels in humans. Biochem Biophys Res Commun. 1998;245:190–193. doi: 10.1006/bbrc.1998.8267. [DOI] [PubMed] [Google Scholar]
- 29.Wang XL, Sim AS, Wang MX, Murrell GA, Trudinger B, Wang J. Genotype dependent and cigarette specific effects on endothelial nitric oxide synthase gene expression and enzyme activity. FEBS Lett. 2000;471:45–50. doi: 10.1016/S0014-5793(00)01356-9. [DOI] [PubMed] [Google Scholar]
- 30.Yoon Y, Song J, Hong SH, Kim JQ. Plasma nitric oxide concentrations and nitric oxide synthase gene polymorphisms in coronary artery disease. Clin Chem. 2000;46:1626–1630. [PubMed] [Google Scholar]
- 31.Jachymova M, Horky K, Bultas J, Kozich V, Jindra A, Peleska J, et al. Association of the Glu298Asp polymorphism in the endothelial nitric oxide synthase gene with essential hypertension resistant to conventional therapy. Biochem Biophys Res Commun. 2001;284:426–430. doi: 10.1006/bbrc.2001.5007. [DOI] [PubMed] [Google Scholar]
- 32.Hingorani AD. Endothelial nitric oxide synthase polymorphisms and hypertension. Curr Hypertens Rep. 2003;5:19–25. doi: 10.1007/s11906-003-0006-0. [DOI] [PubMed] [Google Scholar]
- 33.Tesauro M, Thompson WC, Rogliani P, Qi L, Chaudhary PP, Moss J. Intracellular processing of endothelial nitric oxide synthase isoforms associated with differences in severity of cardiopulmonary diseases: cleavage of proteins with aspartate vs. glutamate at position 298. Proc Natl Acad Sci USA. 2000;97:2832–2835. doi: 10.1073/pnas.97.6.2832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lambrechts D, Claes B, Delmar P, Reumers J, Mazzone M, Yesilyurt BT, et al. VEGF pathway genetic variants as biomarkers of treatment outcome with bevacizumab: an analysis of data from the AViTA and AVOREN randomised trials. Lancet Oncol. 2012;13:724–733. doi: 10.1016/S1470-2045(12)70231-0. [DOI] [PubMed] [Google Scholar]


