Abstract
Background
Inflammation has been demonstrated to be an important risk factor for the development of cardiovascular disease (CVD). The relationship of the peripheral leukocyte count to the severity of stable angina remains to be clarified. The present study analyzed the relationship of the peripheral leukocyte count to the severity of stable angina determined by coronary angiography.
Methods
The data from 108 patients with stable angina, and 92 subjects with normal coronary angiograms were reviewed, and the role of the peripheral leukocyte count as a risk factor for stable angina evaluated. In addition, the correlation of the peripheral leukocyte count and the severity of stable angina, as assessed by the Gensini’s score in the stable angina group, were analyzed.
Results
Age, the prevalence of hypertension and diabetes, and the fasting blood sugar were significantly higher, and the HDL was lower in the stable angina than the control group. A multivariate analysis showed that a peripheral leukocyte count over 6,800/mm3 was an independent variable, but with no statistical significance (p=0.067), and diabetes (OR=3.02, 95% CI: 1.29–7.02) and old age (OR=3.62, 95% CI: 1.33–9.87) were independent risk factors for stable angina. A positive correlation between peripheral leukocyte count and Gensini’s score was noted in the stable angina group even after adjusting for age, fasting blood sugar, blood pressure and lipid profiles (R2=0.198, p=0.015).
Conclusion
An increased peripheral leukocyte count is considered not so much an indicator of the pathogenesis of stable angina, but as a predictor for disease progression. Furthermore, it is considered that the above correlation will be helpful in screening high-risk groups that require relatively active interventional therapy.
Keywords: Leukocyte, Inflammation, Angina pectoris, Cardiovascular disease
INTRODUCTION
Many studies have reported that the inflammation is an important causative factor for cardiovascular disease (CVD)1, 2), and the serum markers in inflammatory reaction, including C-reactive protein, fibrinogen and von Willebrand factor, are associated with CVD3–5). In acute coronary syndrome, the peripheral leukocytes increase due to the adrenocortical reaction, via the hypothalamus-hypophysis-adrenal axis and sympathetic activation. Such increases in leukocytes are known to as markers in acute inflammatory reactions and a poor short-term prognostic indicator in acute coronary syndrome6, 7). Stable angina is known to be related with low-grade systemic inflammation8, 9). It has also been reported that the systemic T-cells10), proinflammatory cytokines and neutrophils are activated in stable angina11). Even though peripheral leukocytes in a condition with no acute stress have been reported to be associated with other cardiovascular risk factors, as a non-specific marker for chronic inflammation12, 13) and risk factor and long-term prognostic factor for CVD14–17), there have been few studies on the correlation between peripheral leukocytes and the severity of CVD. Thus, the this study was conducted on patients who had taken coronary angiography for the confirmative diagnosis of stable angina to clarify whether the peripheral leukocyte count is a risk factor for stable angina and associated with disease progression.
MATERIALS AND METHODS
1. Patients
This cross-sectional study was performed on 200 patients (96 males and 104 females) who had been hospitalized under suspicion of angina pectoris. Informed consent was obtained from each patient, and the study protocol, in accordance to the Declaration of Helsinki, was approved by the institutional committee on human research. Patients with myocardial infarction at admission (total creatine kinase>2×N and increased CK-MB isoenzyme mass during the first 24 hours), myocardial infarction within the previous 2 months, unstable angina (angina at rest, recent onset, or crescendo angina within 4 weeks) and a known infectious or inflammatory disease were excluded. The severity of stable angina was evaluated on the basis of the Gensini’s score18). Patients with Gensini’s scores of 0 and over 1 were allocated to the control (92 patients: 45 males and 47 females) and stable angina group (108 patients: 51 males and 57 females), respectively. A comparison of the baseline clinical characteristics and peripheral leukocyte count was conducted. For the patients in the stable angina group, the correlation between peripheral leukocyte count and Gensini’s score was analyzed.
2. Physical examination and blood test
The mean blood pressure, after measuring 3 times in supine position, was selected and body mass index (kg/m2) calculated. Blood tests were performed with blood sampled from the antecubital vein prior to coronary angiography. The peripheral leukocyte count was measured with by automated hemocytometry (XE-2100, Sysmex, Japanese). The total cholesterol and triglyceride were measured with enzymatic calorimetric tests, high density lipoprotein (HDL) with a selective inhibition method and low density lipoprotein (LDL) with a homogeneous enzymatic calorimetric test. Hypertensive patients were defined as those with a past hypertension history, those with anti-hypertensive medication or those with a systolic pressure over 140 mmHg or a diastolic pressure over 90 mmHg on an outpatient visit. Diabetic patients were defined as those with a past diabetic history insulin or oral hypoglycemic medication and those with a fasting blood sugar over 126 mg/dL or a postprandial 2-h blood sugar over 200 mg/dL.
3. Coronary angiography
Coronary angiography was performed with Judkins technique. A cardiac catheter was percutaneously inserted into the femoral artery, and contrast medium injected into the left/right coronary artery to obtain the anterior view, left anterior oblique 60 degree’s view and right anterior oblique 60 degree’s view for interpretation by a cardiology specialist. To evaluate the degree of coronary stenosis with the Digital Vascular Imaging System (Integris H3000, Philips, Netherlands), the minimum percentile lumen of stenotic lesions to the vascular lumen of normal lesions was obtained. Stenosis of over 25% resulted in referral to the Gensini’s score.
4. Statistical Analysis
All the data was statistically analyzed using the SPSS program (Version 10.0, Inc., Chicago, IL) for MS Windows. The Gensini’s scores were log transformed to normalize the data for analysis. For each group, the mean value was analyzed with the Student’s t-test. Associations between 2 categorical variables were tested by the Chi-squared test. Multivariate analysis was performed on the findings of the univariate analysis. For an intra-group analysis on the CVD group for correlation between the peripheral leukocyte count and Gensini’s score, the Spearman’s correlation coefficient was used. A value of p<0.05 was determined to be significant.
RESULTS
The mean patient age was 59.8±10.8 years, and the mean peripheral leukocyte count and 50 percentile were 6974±1,850/mm3 and 6,800/mm3, respectively. There was no significant difference in the peripheral leukocyte count between smokers and non-smokers. The mean Gensini’s score in the stable angina group was 23.2±28. The peripheral leukocyte count was 7,300±1,500/mm3 in the stable angina group, which was significantly higher than the 6,500±1,500/mm3 in the control group (p<0.01). Age, the prevalence of hypertension and diabetes, and the fasting blood sugar were significantly higher and the HDL cholesterol lower in the stable angina than the control group (Table 1).
Table 1.
Clinical Features of the Control and Stable Angina Groups
| Control (n=92) | Stable angina (n=108) | |
|---|---|---|
| Leukocyte count (1,000/mm3) | 6.5±1.5 | 7.3±1.5† |
| Age (years) | 55.8±11.4 | 63.1±8.9† |
| Male† | 49% | 47% |
| Body mass index (kg/m2) | 25.4±3.3 | 26.2±3.1 |
| Prevalence of hypertension | 39% | 62%† |
| Prevalence of diabetes | 12% | 38%† |
| Current smoking | 23% | 20% |
| Fasting blood sugar (mg/dL) | 100.2±28.6 | 113.8±52.1* |
| Total cholesterol (mg/dL) | 190.5±39.5 | 198±47.2 |
| Triglyceride (mg/dL) | 146.5±72.9 | 168±113.8 |
| LDL (mg/dL) | 119.8±32.6 | 121.0±33.8 |
| HDL (mg/dL) | 48.2±12.1 | 44.7±10.4* |
| Systolic blood pressure | 136.6±16.6 | 138.4±23.1 |
| Diastolic blood pressure | 87.8±12.7 | 86.1±13.3 |
Values are mean±SD or percentage. LDL, low density lipoprotein cholesterol; HDL, high density lipoprotein cholesterol.
p<0.05
p<0.01
In the univariate analysis, the odds ratio of the patients with a peripheral leukocyte count at the 50 percentile level over 6,800/mm3 was 1.79 (95% C.I: 1.02–3.16). The odds ratio of the patients over 45 years in males and over 55 years in females was 3.15 (95% C.I: 1.48–6.68). The odds ratio of the hypertensive and diabetic patients to that of the normal patients were 2.64 (95% C.I: 1.49–4.68) and 4.50 (95% C.I: 2.15–9.44), respectively. Logistic multiple regression analysis on the independent variables, such as significant risk factors from the univariate analysis (peripheral leukocyte count, age, hypertension and diabetes), showed that a peripheral leukocyte count over 6,800/mm3 was an independent variable, but with no statistical significance (p=0.067), and that diabetes (OR=3.02, 95% CI: 1.29–7.02) and old age (OR=3.62, 95% CI: 1.33–9.87) were independent risk factors for CVD (Table 2).
Table 2.
Multivariate Relationship between Risk Factors and Stable Angina Pectoris (n=200)
| OR (95% CI) | p-value | |
|---|---|---|
| Leukocyte count (≥6,800/mm3) | 1.88 (0.95–3.72) | 0.067 |
| Age (M≥45, F≥55 yrs) | 3.62 (1.33–9.87) | 0.012 |
| Presence of diabetes | 3.02 (1.29–7.02) | 0.010 |
| Presence of hypertension | 1.34 (0.66–2.71) | 0.413 |
| LDL (≥130 mg/dL) | 1.00 (0.99–1.01) | 0.973 |
| HDL (<40 mg/dL) | 0.97 (0.94–1.00) | 0.143 |
M, male; F, female; yrs, years; LDL, low density lipoprotein cholesterol; HDL, high density lipoprotein cholesterol.
The variables significantly correlated with Gensini’s score were the peripheral leukocyte count and fasting blood sugar (p=0.028 and 0.001 respectively)(Table 3). The analysis of the correlation between peripheral leukocyte count and Gensini’s score in stable angina group showed that there was a positive correlation, even after adjusting for age, fasting blood sugar, blood pressure and lipid profiles (R2=0.198 and p=0.015)(Figure 1).
Table 3.
Correlation between Gensini’s Score and Variables in Patients with Stable Angina (n=108)
| Coefficient | p-value | |
|---|---|---|
| Leukocyte count | 0.213 | 0.028 |
| Age | 0.060 | 0.121 |
| Body mass index | 0.073 | 0.486 |
| Fasting blood sugar | 0.307 | 0.001 |
| Total cholesterol | 0.155 | 0.114 |
| Triglyceride | 0.002 | 0.987 |
| LDL | 0.184 | 0.076 |
| HDL | −0.161 | 0.121 |
| Systolic blood pressure | 0.112 | 0.247 |
| Diastolic blood pressure | 0.149 | 0.124 |
LDL, low density lipoprotein cholesterol; HDL, high density lipoprotein cholesterol.
Figure 1.
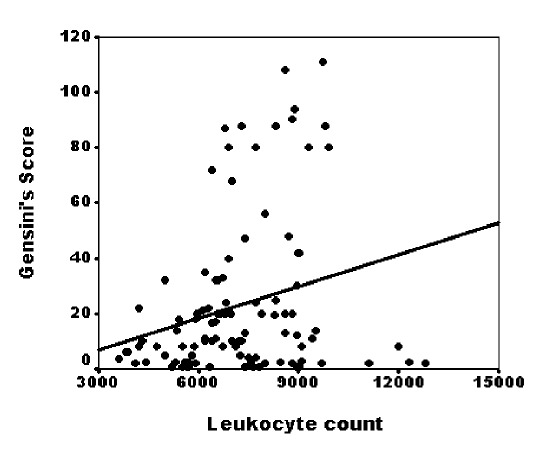
Relationship between leukocyte count and Gensini’s score in 108 patients with stable angina (R2= 0.198, p=0.015).
DISCUSSION
Even though most studies on the correlation between peripheral leukocytes and CVD have been performed in the field of epidemiology, none have presented consistent results. Gillum et al.19) stated that the peripheral leukocytes are not an independent cardiovascular risk factor but a mediator and indicator of smoking. In a study on patients who had undergone coronary angiography, Kostis et al.20) reported that non-smokers had a weak or insignificant correlation between leukocyte and prevalence of CVD, and an increased leukocyte count was mainly due to smoking in the CVD compared to the control group. There have been some studies on the role of peripheral leukocytes aside from smoking in the pathogenesis of CVD. Some cohort studies have reported that peripheral leukocytes have significant correlation with mortality of CVD, even after adjusting for smoking13, 21). Also, some prospective studies on patients with a past medical history of myocardial infarction have reported that peripheral leukocytes are a prognostic factor for mortality of coronary heart disease15, 16). In the present study, there was no significant difference observed in the peripheral leukocyte count between smokers and non-smokers, which was considered to be due to the exclusion of the amount of a patients’ past smoking, and females with a relatively lower smoking rate accounted for a higher proportion of the patients than males.
Several hypotheses have been proposed to explain the effect of leukocytes on the pathogenesis and progression of CVD. Overall, with atherosclerotic steps, inflammatory cells were observed within the lesions22, 23), and monocytes and lymphocytes were present in not only fatty streaks, but also in atheroma, progressing enough to accompany symptoms22, 24). Cytokines, including TNF-α and IL-1, induce atherosclerotic progression by elevating the LDL cholesterol receptors in endothelial cells25). Activation of the inflammatory marker and circulating T cell, including CRP, in unstable angina has been reported26–28). Stable angina is known to be related with low-grade systemic inflammation8, 9) and have activated systemic T-cells, proinflammatory cytokines and neutrophils10, 11).
In the present study, a multiple regression analysis, with a cut-off value of 6,800/mm3, the 50 percentile peripheral leukocyte count, showed that an increased peripheral leukocyte count tended to be an independent risk factor for stable angina, but with no statistical significance. However, there was a positive correlation between the Gensini’s score and the peripheral leukocyte count, even after adjusting for age, fasting blood sugar, blood pressure and lipid profiles, indicating that an increased peripheral leukocyte count may be related not so much to the incidence of stable angina, as to its severity and progression, which supports the hypothesis that inflammation plays a key role in the pathogenesis of stable angina.
There is a limitation in this cross-sectional study, as it was impossible to determine the causal relationship between the peripheral leukocyte count and the Gensini’s score. Therefore, it is considered that a further prospective study will be required to verify the above causal relationship. Also, an inter-group analysis was performed on the basis of the 50 percentile as an arbitrary cut-off value, as the normal variations in the peripheral leukocyte count are unknown in normal adult populations. In this study, the deviation of the peripheral leukocyte count was within the normal range; therefore, more research is needed. The mean age of the patients was 59.8±10.8 years, somewhat high, and the patients unevenly allocated to the control and coronary disease groups. The amount of Patients’ past smoking was not considered in the present study. The total cholesterol, triglyceride and LDL cholesterol showed no significant differences between the two groups, and were not risk factors for stable angina, which was considered to be due to the negligence in administration of HMG CoA reductase inhibitor prior to coronary angiography.
In conclusion, an increased peripheral leukocyte count is considered not so much an indicator for the pathogenesis of stable angina, but more as a predictor for disease progression. Furthermore, it is considered that the above correlation will be helpful in screening high-risk stable angina that requires relatively active interventional therapy.
REFERENCES
- 1.Ross R. Atherosclerosis: an inflammatory disease. N Engl J Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 2.Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CM. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973–979. doi: 10.1056/NEJM199704033361401. [DOI] [PubMed] [Google Scholar]
- 3.Ridker PM, Buring JE, Shin J, Matias M, Hennekens CH. Prospective study of C-reactive protein and the risk of future cardiovascular events among apparently healthy women. Circulation. 1998;98:731–733. doi: 10.1161/01.cir.98.8.731. [DOI] [PubMed] [Google Scholar]
- 4.Woodward M, Lowe GD, Rumley A, Tunstall-Pedoe H. Fibrinogen as a risk factor for coronary heart disease and mortality in middle-aged men and women. Eur Heart J. 1998;19:55–62. doi: 10.1053/euhj.1997.0573. [DOI] [PubMed] [Google Scholar]
- 5.Silveira AM, Elgue G, Hamsten A, Blomback M. von Willebrand factor in plasma and urine of men with premature coronary artery disease. Thromb Haemost. 1992;67:161–165. [PubMed] [Google Scholar]
- 6.Barron HV, Cannon CP, Murphy SA, Braunwald E, Gibson CM. Association between white blood cell count, epicardial blood flow, myocardial perfusion, and clinical outcomes in the setting of acute myocardial infarction: a thrombolysis in myocardial infarction 10 substudy. Circulation. 2000;102:2329–2334. doi: 10.1161/01.cir.102.19.2329. [DOI] [PubMed] [Google Scholar]
- 7.Furman MI, Becker RC, Yarzebski J, Savegeau J, Gore JM, Goldberg RJ. Effect of elevated leukocyte count on in-hospital mortality following acute myocardial infarction. Am J Cardiol. 1996;78:945–948. doi: 10.1016/s0002-9149(96)00473-0. [DOI] [PubMed] [Google Scholar]
- 8.Ikonomidis I, Andreotti F, Economou E, Stefanadis C, Toutouzas P, Nihoyannopoulos P. Increased proinflammatory cytokines in patients with chronic stable angina and their reduction by aspirin. Circulation. 1999;100:793–798. doi: 10.1161/01.cir.100.8.793. [DOI] [PubMed] [Google Scholar]
- 9.Abdelmouttaleb I, Danchin N, Ilardo C, Aimone-Gastin I, Angioi M, Lozniewski A, Loubinoux J, Ie Faou A, Gueant JL. C-reactive protein and coronary artery disease: additional evidence of the implication of an inflammatory process in acute coronary syndrome. Am Heart J. 1999;137:346–351. doi: 10.1053/hj.1999.v137.92052. [DOI] [PubMed] [Google Scholar]
- 10.Jonasson L, Linderfalk C, Olsson J, Wikby A, Olsson AG. Systemic T-cell activation in stable angina pectoris. Am J Cardiol. 2002;89:754–756. doi: 10.1016/s0002-9149(01)02348-7. [DOI] [PubMed] [Google Scholar]
- 11.Johnny N, Anders W, Lena J. Proinflammatory cytokines and neutrophil activation in stable angina. J Am Coll Cardiol. 2003;41:359. [Google Scholar]
- 12.Ingram DD, Gillum RF. Leukocyte count and cardiovascular risk factors. J Natl Med Assoc. 1992;84:1041–1043. [PMC free article] [PubMed] [Google Scholar]
- 13.Hansen LK, Grimm RH, Jr, Neaton JD. The relationship of white blood cell count to other cardiovascular risk factors. Int J Epidemiol. 1990;19:881–888. doi: 10.1093/ije/19.4.881. [DOI] [PubMed] [Google Scholar]
- 14.Phillips AN, Neaton JD, Cook DG, Grimm RH, Shaper AG. Leukocyte count and risk of major coronary heart disease events. Am J Epidemiol. 1992;136:59–70. doi: 10.1093/oxfordjournals.aje.a116421. [DOI] [PubMed] [Google Scholar]
- 15.Ernst E, Hammerschmidt DE, Bagge U, Matrai A, Dormandy JA. Leukocytes and the risk of ischemic disease. JAMA. 1987;257:2318–2324. [PubMed] [Google Scholar]
- 16.Lowe GD, Machado SG, Krol WF, Barton BA, Forbes CD. White blood cell count and haematocrit as predictors of coronary recurrence after myocardial intarction. Thromb Haemost. 1985;54:700–703. [PubMed] [Google Scholar]
- 17.Hajj-Ali R, Zareba W, Ezzeddine R, Moss AJ. Relation of the leukocyte count to recurrent cardiac events in stable patients after acute myocardial infarction. Am J Cardiol. 2001;88:1221–1224. doi: 10.1016/s0002-9149(01)02080-x. [DOI] [PubMed] [Google Scholar]
- 18.Gensini GG. A more meaningful scoring system lor determining the severity of coronary heart disease. Am J Cardiol. 1983;51:606. doi: 10.1016/s0002-9149(83)80105-2. [DOI] [PubMed] [Google Scholar]
- 19.Gillum RF, Ingram DD, Makuc DM. White blood cell count and stroke incidence and death. Am J Epidemiol. 1994;139:894–902. doi: 10.1093/oxfordjournals.aje.a117095. [DOI] [PubMed] [Google Scholar]
- 20.Kostis JB, Turkevich D, Sharp J. Association between leukocyte count and extent of coronary atherosclerosis as determined by coronary arteriography. Am J Cardiol. 1984;53:997–999. doi: 10.1016/0002-9149(84)90624-6. [DOI] [PubMed] [Google Scholar]
- 21.Brown DW, Giles WH, Croft JB. White blood cell count: an independent predictor of coronary heart disease mortality among a national cohort. J Clin Epidemiol. 2001;54:316–322. doi: 10.1016/s0895-4356(00)00296-1. [DOI] [PubMed] [Google Scholar]
- 22.Stay HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W, Jr, Rosenfeld ME, Schwartz CJ, Wagner WD, Wissler RW. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. Circulation. 1995;92:1355–1374. doi: 10.1161/01.cir.92.5.1355. [DOI] [PubMed] [Google Scholar]
- 23.Stay HC, Chandler AB, Glagov S, Guyton JR, Insull W, Jr, Rosenfeld ME, Schaffer SA, Schwartz CJ, Wagner WD, Wissler RW. A definition of initial, fatty streak, and intermediate lesions of atherosclerosis. Circulation. 1994;89:2462–2478. doi: 10.1161/01.cir.89.5.2462. [DOI] [PubMed] [Google Scholar]
- 24.Napoli C, D’Armiento FP, Mancini FP, Postiglione A, Witztum JL, Palumbo G, Palinski W. Fatty streak formation occurs in human fetal aortas and is greatly enhanced by maternal hypercholesterolemia: intimal accumulation of low density lipoprotein and its oxidation precede monocyte recruitment into early atherosclerotic lesions. J Clin Invest. 1997;100:2680–2690. doi: 10.1172/JCI119813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hajjar DP, Haberland ME. Lipoprotein trafficking in vascular cells: molecular trojan horses and cellular saboteurs. J Biol Chem. 1997;272:22975–22978. doi: 10.1074/jbc.272.37.22975. [DOI] [PubMed] [Google Scholar]
- 26.Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, Rebuzzi AG, Pepys MB, Maseri A. The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med. 1994;331:417–424. doi: 10.1056/NEJM199408183310701. [DOI] [PubMed] [Google Scholar]
- 27.Neri Serneri GG, Prisco D, Martini F, Gori AM, Brunelli T, Poggesi L, Rostagno C, Gensini GF, Abbate R. Acute T cell activation is detectable in unstable angina. Circulation. 1997;95:1806–1812. doi: 10.1161/01.cir.95.7.1806. [DOI] [PubMed] [Google Scholar]
- 28.Caligiuri C, Liuzzo G, Biasucci LM, Maseri A. Immune system activation follows inflammation in unstable angina: pathogenic implications. J Am Coll Cradiol. 1998;32:1295–1304. doi: 10.1016/s0735-1097(98)00410-0. [DOI] [PubMed] [Google Scholar]


