Abstract
Background
Several studies suggested that T-wave normalization (TWN) in exercise ECG indicates the presence of viable myocardium. But the clinical implication of this phenomenon in patients with acute myocardial infarction who received proper revascularization therapy was not determined. Precisely the aim of this study was to investigate the relationship between TWN in exercise ECG and myocardial functional recovery after acute myocardial infarction.
Methods
We studied 30 acute myocardial infarction patients with negative T waves in infarct related electrocardiographic leads and who had received successful revascularization therapy. Exercise ECG was performed 10–14days after infarct onset using Naughton protocol. Patients were divided into 2 groups according to presence (group I; n=14) or not (group II; n=16) of TWN in exercise ECG. Exercise parameters and coronary angiographic findings were compared between groups. Baseline and follow-up (mean 11 months) regional and global left ventricular function was analyzed by echocardiography.
Results
Exercise parameters were similar between groups. There was no difference in baseline ejection fraction and wall motion score between group I and II (EF; 56±12% vs 52±11%, p=ns. WMS; 21±3 vs 23±4, p=ns) and it was improved at the tenth month by similar magnitude (group I/group II, EF % change=12±12% vs 7±6%, p=ns, WMS % change=6±6% vs 7±5%, p=ns). The finding of no relation between TWN and functional recovery was observed also when the patients were analysed according to infarct location and presence or absence of Q-waves.
Conclusion
As the exercise-induced TWN in patients with acute myocardial infarction was not related with better functional recovery of dysfunctional regional wall motion and ejection fraction, TWN does not appear to be an indicator of myocardial viability.
Keywords: Myocardial infarction, Exercise test
INTRODUCTION
Identification of viable myocardium from the left ventricular area of dysfunctional regional wall motion after acute myocardial infarction is very important because proper revascularization therapy may improve the clinical outcome. In the diagnosis of viable myocardium, 24-hour-delayed redistribution imaging by Thallium-201 scintigraphy, reinjection Thallium-201 scintigraphy, myocardial echocardiography or low dose Dobutamine stress echocardiography are currently applied methods1–3, 12). Particularly, Positron Emission Tomography is being used as a standard testing because of it’s high sensitivity4). But these testing methods are complicated and expensive, and they require experience to interpret the acute evaluation of viability. Therefore, as a method to identify the presence of viable myocardium with ease, there have been attempts to use exercise ECG performed after myocardial infarction.
Recently, some studies have reported T-wave normalization (TWN), which means normalization of negative T-waves in rest ECG of infarct-related electrocardiography leads or ST-segment elevation may indicate the presence of viable myocardium. Lombardo et al.3) performed low dose Dobutamine stress echocardography (5–10 μg/kg/min) in Q-wave myocardial infarction patients and found that contractile reserve was higher in the area with T-wave normalization (TWN) or ST-segment elevation than that of no change of ECG. Margonato et al.4) performed Thallium-201 scintigraphy and exercise stress testing and reported that ST-segment elevation and TWN findings in exercise ECG indicate the residual viable myocardium. Also, Mobilia et al.6) reported that exercise induced TWN finding is a marker of viable myocardium by comparing ECG changes and positrom emission tomography. But Bodi et al.7) reported that the ST-segment elevation and TWN findings during exercise testing were not related with functional recovery. It shows that there are still conflicting opinions about the clinical implications of TWN findings and ST-segment elevation induced by exercise stress. Therefore, this study was designed to observe the relation between TWN in exercise ECG and left ventricle functional recovery after acute myocardial infarction to ascertain if T-wave normalization in exercise ECG can detect viable myocardium.
MATERIALS AND METHODS
1. Patients
30 patients with acute myocardial infarction who visited the Korea University Anam Hospital from Jan. 1998 to May 1999 were included for the study. Among patients with acute myocardial infarction during the same period, the patients with heart failure, severe valvular insufficiency and conduction defect, complications related to reperfusion, were excluded. The patients with ventricular hypertrophy with inverted T-wave in rest ECG, left and right bundle branch blocks, Wolff-Parkinson-White syndrome, serious anemia, electrolyte disorders8) and patients with poor quality of echocardiographic images were also excluded. Acute myocardial infarction was diagnosed by chest pain lasting for more than 30 minutes which was not relieved by sublingual nitroglycerine, ST-segment elevation on ECG and increase of blood creatinine kinase MB over 10 ng/mL. All the patients underwent coronary angiography; 6 were treated with thrombolytic agent, 16 were treated with mechanical revascularization and 4 with both.
2. Exercise Stress Testing
Low grade exercise stress ECG (Naughton method) with an increasing step at 2-minute intervals during mean 10–14 days after myocardial infarction was performed. 12 lead electrocardiography was continuously monitored, blood pressure was measured and ECG was recorded at every step. Also, exercise time, peak heart rate and metabolic equivalents (METs) were observed. Criteria for TWN were normalization of T-wave after exercise, which was inverted over 0.15 mV at more than 2 infarct-related ECG leads9). ST-segment elevation was defined when it was elevated more than 1 mV lasting 0.08 seconds after J-point.
3. Echocardiography
Baseline echocardiography was performed during admission period and a follow-up study was done 11 months later. The changes of left ventricular ejection fraction and regional wall motion were observed for analysis. The ejection fraction was calculated with left ventricular diastolic and systolic volume measured by the modified Simpson’s method from the apical four chamber view. The regional wall motion analysis adopted the method recommended by the American Society of Echocardiography, which divides the left ventricle into 16 segments and gives the scores from 1 to 4 according to the contraction of each segment (1=normal, 2=hypokinesia, 3=akinesia, 4=dyskinesia). All the scores of every segment were summed up to get the wall motion score (WMS).
4. Coronary angiography
The standard method by femoral artery approach was used. When the luminal diameter of the coronary artery was reduced by 70%, it was considered as a significant coronary stenosis. The percent stenosis of infarct -related blood vessel, TIMI grade and presence of collateral circulation vessel were recorded. A successful revascularization was defined when the luminal diameter was expanded over 50% and the chest pain vanished.
5. Statistical analysis
For all the statistical results, SPSSWIN 7.5 program was used. Data was expressed as mean value ± SD. For the difference between groups, Mann-Whitney test as the nonparametric method was used for continuous variables, whereas chi-square method was used for non-continuous variables. Changes of baseline and follow-up ejection fraction and regional wall motion were assessed by using Wilcoxin rank test as the nonparametric method. A value of p<0.05 was considered significant.
RESULTS
1. Clinical features
30 patients were divided into group I (14 patients) with TWN and group II (16 patients) without TWN. Table 1 displays the clinical features of the study patients. There were no differences in sex, age, number of risk factors, infarction area, Q-wave infarction rate and revascularization methods between the two groups.
Table 1.
Comparison of clinical features between group I and group II.
| Group I | Group II | p-value | |
|---|---|---|---|
| Number | 14 | 16 | ns |
| Age (yr) | 57±12 | 62±7 | ns |
| Male | 9 (64%) | 10 (63%) | ns |
| Infarction area | |||
| Anterior | 8 (57%) | 7 (43%) | ns |
| Inferior | 6 (43%) | 7 (43%) | ns |
| Inf-posteror | 0 | 2 (15%) | ns |
| Q-wave infarction | 8 (57%) | 9 (56%) | ns |
| Risk factors | |||
| Diabetes mellitus | 5 (36%) | 2 (13%) | ns |
| Hypertension | 2 (14%) | 2 (13%) | ns |
| Diabetes & hypertension | 1 (7%) | 0 | ns |
| Smoking | 11 (79%) | 12 (75%) | ns |
| Revascularization | ns | ||
| Medical treatment only | 1 (7%) | 3 (19%) | ns |
| PTCA and/or STENT | 7 (50%) | 9 (56%) | ns |
| Thrombolysis | 2 (7%) | 4 (25%) | ns |
| Thrombolysis & PTCA | 4 (29%) | 0 | ns |
2. Exercise ECG test
Figure 1 shows one example of ECG with TWN observed in exercise ECG. During the exercise ECG testing, there was no difference of total exercise time, metabolic equivalents (METs), peak heart rate and rate of combined ST segment elevation between the two groups (Table 2).
Figure 1.
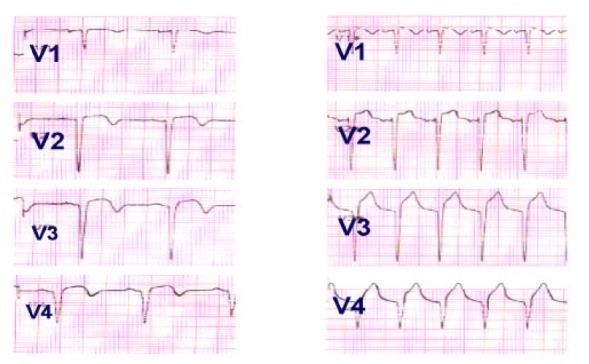
Exercise ECG: Normalization of T-wave was observed in leads from V1 to V4.
Table 2.
Exercise ECG parameters in patients with and without T-wave normalization
| Group I | Group II | p-value | |
|---|---|---|---|
| Exercise time (min) | 8±4 | 11±3 | ns |
| Metabolic equivalents (METs) | 5±2 | 6±1 | ns |
| Peak heart rate (beat/min) | 121±13 | 115±17 | ns |
| Combined ST-segment elevation (%) | 5 (36%) | 5 (31%) | ns |
3. Echocardiography
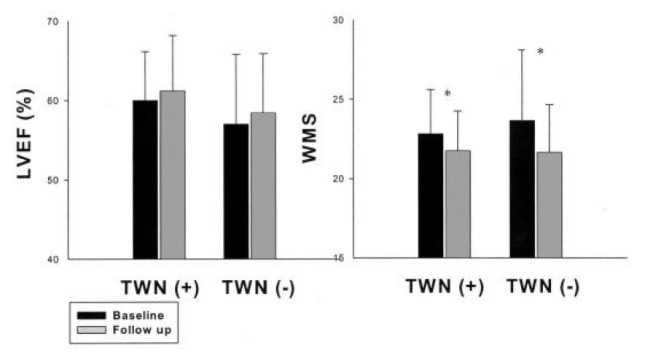
Table 3 indicates baseline and follow-up ejection fraction, wall motion score and it’s percent changes from baseline to follow-up between group I and group II. The ejection fraction and wall motion score were significantly improved in the follow-up test compared to baseline (p<0.05) in each group. There was no difference in percent changes of ejection fraction and wall motion score indicating the degree of improvement (Figure 2, 3) between group I and II. The patients were divided according to the presence or absence of Q wave in ECG and still similar trends between Q wave and non Q wave myocardial infarction patients group were found (Table 4).
Table 3.
Baseline and follow-up ejection fraction, wall motion score and percent changes between groups.
| Group I | Group II | p-value | |
|---|---|---|---|
| Number | 14 | 16 | ns |
| EF: base (%) | 56±12 | 52±11 | ns |
| EF: f/u (%) | 61±7 | 55±9 | ns |
| EF: % change (%) | 13±7 | 15±11 | ns |
| WMS: base | 23±4 | 25±5 | ns |
| WMS: f/u | 21±3 | 23±4 | ns |
| WMS: %change | 11±3 | 12±8 | ns |
EF, ejection fraction; WMS, wall motion score; base, baseline; f/u, follow up.
Figure 2.
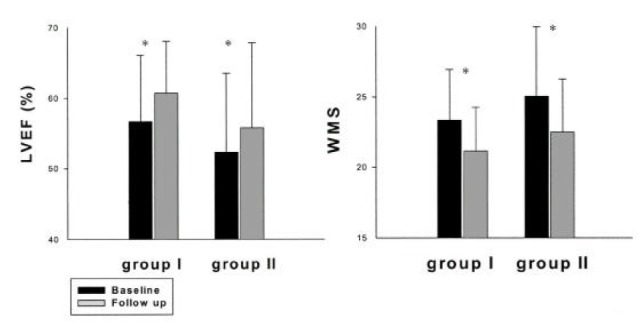
Changes of ejection fraction and wall motion score in each group.
LVEF, left ventricular ejection fraction; WMS, wall motion score; TWN, T-wave normalization. *p<0.05
Figure 3.
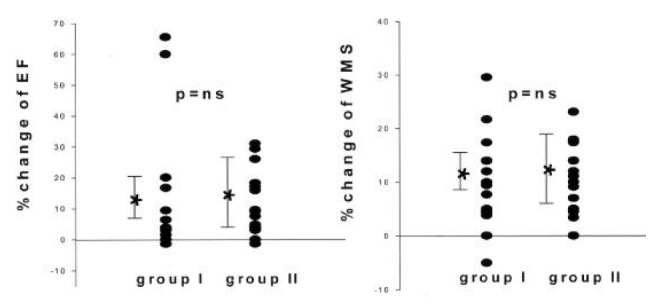
Percent change of ejection fraction and wall motion score
EF, ejection fraction; WMS, wall motion score
Table 4.
Baseline and follow-up ejection fraction, wall motion score and percent changes between groups according to Q-wave.
| Group I | Group II | p-value | |
|---|---|---|---|
| Q wave | |||
| Number | 6 | 7 | ns |
| EF: base (%) | 53±13 | 62±5 | ns |
| EF: f/u (%) | 57±11 | 64±5 | ns |
| EF: % change (%) | 12±12 | 7±6 | ns |
| WMS: base | 24±6 | 22±3 | ns |
| WMS: f/u | 23±4 | 20±2 | ns |
| WMS: % change | 6±6 | 7±5 | ns |
| Non-Q wave | |||
| Number | 8 | 9 | ns |
| EF: base (%) | 51±7 | 51±14 | ns |
| EF: f/u (%) | 56±8 | 58±8 | ns |
| EF: % change (%) | 11±9 | 20±27 | ns |
| WMS: base | 26±4 | 25±4 | ns |
| WMS: f/u | 22±4 | 22±4 | ns |
| WMS: % change | 12±7 | 12±11 | ns |
EF, ejection fraction; WMS, wall motion score; TWN, T-wave normalization; base, baseline; f/u, follow up.
When they were analysed by infarct location, baseline ejection fraction (55±13% vs 43±8%, p=0.06) and follow-up ejection fraction (61±9 vs 52±10, p=0.06) were higher in patients with TWN than without TWN among anterior infarction patients. In the group of anterior wall infarction, the left ventricular function improved significantly in follow-up test in patients without TWN (EF base/follow up: 43±8%/52±10%, p=0.03, WMS base/follow up: 29±4/24±4, p=0.02), whereas patients with TWN did not show a significant improvement (EF base/follow up: 55±14%/61±9%, p=ns, WMS base/follow up: 24±5 / 21±4, p=ns, Table 5).
Table 5.
In anterior myocardial infarction, baseline and follow-up ejection fraction, wall motion score and percent changes between groups.
| Group I | Group II | p-value | |
|---|---|---|---|
| Number | 7 | 7 | ns |
| EF: base | 55±13 | 43±8 | 0.06 |
| EF: f/u | 61±9 | 52±10 | 0.06 |
| EF: % change | 15±4 | 19±10 | ns |
| WMS: base | 24±5 | 29±4 | ns |
| WMS: f/u | 21±4 | 24±4 | ns |
| WMS: % change | 14±7 | 16±9 | ns |
EF, ejection fraction; WMS, wall motion score; TWN, T-wave normalization; base, baseline; f/u, follow up; *p<0.05.
In inferior myocardial infarction patients, the left ventricular function was not different from baseline and follow-up testings in both groups (Table 6).
Table 6.
In inferior myocardial infarction, baseline and follow-up ejection fraction, wall motion score and percent changes between groups.
| Group I | group II | p-value | |
|---|---|---|---|
| Number | 7 | 9 | ns |
| EF-base | 56±11 | 57±9 | ns |
| EF-f/u | 60±11 | 58±8 | ns |
| EF-%change | 6±13 | 3±4 | ns |
| WMS-base | 23±3 | 24±4 | ns |
| WMS-f/u | 21±3 | 22±3 | ns |
| WMS-%change | 7±5 | 8±6 | ns |
EF, ejection fraction; WMS, wall motion score; TWN, T-wave normalization; base, baseline; f/u, follow up; *p<0.05.
4. Coronary angiographic finding
There was no difference in number of stenotic coronary vessel, location of infarctor related vessel and grade of collateral circulation between two groups. But after revascularization therapy, the percent of patients with >70% residual stenosis of infarct related coronary artery was higher in the TWN group (Table 7).
Table 7.
Angiographic comparison between patients with and those without TWN
| Group I | Group II | p value | |
|---|---|---|---|
| Diseased vessel (1/2) | 9/5 (64/36%) |
11/5 (69/31%) |
ns |
| IRA (LAD/RCA/LCX) | 7/6/1 (50/43/7%) |
7/7/2 (44/44/12%) |
ns |
| Collateral vessel (grade>1) |
2(14%) | 5(30%) | ns |
| Luminal narrowing >70% in IRA |
0(0%) | 4(16%) | 0.03 |
IRA, infarction related artery;
LAD, left anterior descending artery;
RCA, right coronary artery; LCX, left circumflex artery
DISCUSSION
In This Study, The Association Of Exercise Induced Normaliztion Of T-Wave, Which Was Inverted In Rest ECG In patients after myocardial infarction with late functional recovery, was not found.
Dysfunctional but viable myocardium is generally divided into hibernating myocardium and stunning myocardium. The former is defined as temporary dysfunctional myocardium by the reduction of coronary flow and the latter condition is induced by repeated myocardial ischemia or reversible ischemic myocardial damage10–11). There are several testing methods to detect this viable myocardium. Recently, the finding of T-wave normalization during exercise ECG has been reported as an indicator of viable myocaridum. Previous studies have suggested the relation between viable myocardium and TWN mostly by imaging diagnostic methods1–5). There were a few data comparing left ventricular function recovery with the findings of T-wave normalization but their results are controversial13–15). Therefore, this study was designed to investigate whether TWN on exercise ECG was related with late functional recovery among acute myocardial infarction patients after revascularization therapy. As a result, the left ventricular function was recovered at follow-up in both groups but, regardless of the presence of TWN, the degree of left ventricular functional recovery was similar in both groups and made this result different from previous studies by explaining that positive TWN finding indicates the viable myocardium.
The mechanism of exercise induced T-wave normalization has not been clarified yet, but it can be explained by several reasons. In cases with coronary diseases, exacerbation of myocardial ischemia or passive stretching of the infarct area by the tension being developed by normal contracting myocardium or presence of viable myocardium18) were reported to be related with T-wave normalization. From this study, the mechanism of T-wave normalization on exercise appears to be related with either exaggerated abnormal infarct area wall motion or myocardial ischemia. Every myocardial infarction patient included in this study took a proper revascularization therapy before exercise ECG and showed no ST depression or chest pain during exercise. But 4 patients among group II who did not have TWN exercise ECG showed a significant stenosis (>70%) of infarct related vessel by angiography. But on coronary angiography, all of these patient showed TIMI III coronary flow and exercise ECG showed no ST depression. When the data was analysed after the 4 patients had been excluded, there was no difference in baseline and follow-up left ventricular function and left ventricular functional recovery. Thus, it is unlikely that myocardial ischemia may induce T-wave normalization during exercise test.
67% of the patients in this study showed left ventricular ejection fraction over 50%. The mean baseline ejection fraction and wall motion score between group I and II was not different. But in patients with anterior infarction, patients with TWN tended to have higher ejection fraction and wall motion score at baseline. This result was different from previous studies that suggested a relation between TWN finding and viable myocardium. They explained that baseline ejection fraction of patients with TWN was lower than that of patients without TWN and the left ventricular function did not recover or, rather, reduced even after revascularization in the group without TWN16, 22). But the result is the opposite in this study. The explanation for this difference is not clear. All the patients in this study received proper revascularization therapy and did not show inducible ischemia in exercise ECG. Thus the findings of TWN in exercise ECG appear to be related with exaggerated dysfunctional regional wall motion caused by increased myocardial contraction on exercise in normal area.
In diagnosing viable myocardium with exercise ECG, the intensity of exercise stress testing and location of infarction was reported to be important to consider. Mobilia et al.6) presented that detection rate of viable myocardium be higher when a lower intensity of exercise test is used, or when the patient has anterior myocardial infarction. The exercise protocol in this study was the Naughton method which is a low intensity exercise protocol. Also, when compared by infarction areas of anterior and inferior, the left ventricular functional recovery did not show any difference in degree.
Like TWN, there are various opinions about the implication of ST-segment elevation in exercise stress testing in patients with myocardial infarction. Dyskinesia, aneurysm, coronary spasm and serious proximal constriction are known to be related and there are some recent reports that ST-segment elevation indicates viable myocardium17–21). But this has not been clearly explained so far and interaction with TWN is not well known, either. Saito et al.23) performed positron emission tomography and presented that there was viable myocardium in only 10% of patients in case of exercise induced ST-segment elevation without TWN after myocardium infarction, which explained their correlation. But it is considered that TWN finding and combined ST-segment implications require further studies.
This study was subject to some limitations. First, most patients were administered an antianginal drug, except beta blocker, during exercise stress testing, which might mask induction of ischemia. Second, combined ST-segment elevation was seen in 10 patients that may interfere interpretation of the genuine relation between TWN group and viable myocardium. But ST-segment elevation mechanism has not been known so far and there was no difference of frequency between the groups which would affect the study result much. Third, the range of follow-up period was relatively uneven, from 2.2 months, so to 20 months that it can affect the rate of the left ventricular functional recovery. In some patients there could be reocclusion of revascularized infarct related artery.
In conclusion, this study confirmed that exercise stress testing induced TWN finding is not related to the myocardial functional recovery in patients with acute myocardial infarction after revascularization and that TWN finding on exercise stress electrocardiography does not indicate myocardial viability.
Figure 4.
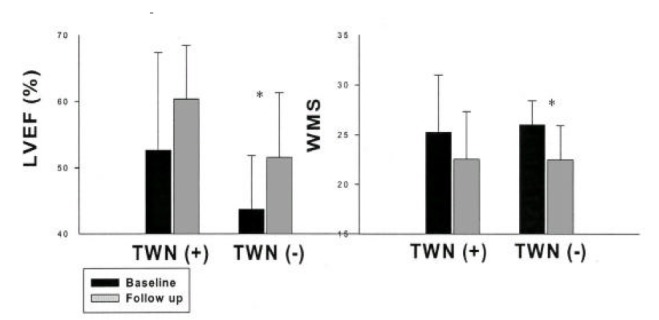
Changes of ejection fraction and wall motion score in anterior myocardial infarction.
LVEF, left ventricular ejection fraction; WMS, wall motion score; TWN, T-wave normalization; *p<0.05.
Figure 5.
Changes of ejection fraction and wall motion score in inferior myocardial infarction.
LVEF, left ventricular ejection fraction; WMS, wall motion score; TWN, T-wave normalization; *p< 0.05.
REFERENCE
- 1.Khaw BA, Strauss HW, Pohost GM, Fallon JT, Kattus HA, Haber E. Relation of immediate and delayed thallium-201 distribution to localization of iodine-125 antimyosin antibody in acute experimental myocardial infarction. Am J Cardiol. 1983;51:1428–1432. doi: 10.1016/0002-9149(83)90324-7. [DOI] [PubMed] [Google Scholar]
- 2.Pie’rard LA, Lancellotti PL, Kulbertus HE, Liege FF. ST-segment elevation during dobutamine stress testing predicts functional recovery after acute myocardial infarction. Am Heart J. 1999;137:500–511. doi: 10.1016/s0002-8703(99)70499-0. [DOI] [PubMed] [Google Scholar]
- 3.Lombardo A, Loperfido F, Pennestri F, Rossi E, Patrizi R, Cristinziani G, Catapano G, Maseri A. Significance of transient ST- segment changes during dobutamine testing in Q-wave myocardial infarction. J Am Coll Cardiol. 1996;27:599–605. doi: 10.1016/0735-1097(95)00499-8. [DOI] [PubMed] [Google Scholar]
- 4.Margonata A, Chierchia SL, Xuereb RG, Xuereb M, Fragasso G, Cappelletti A, Landoni C, Lucignani G, Fazio F. Specificity and sensitivity of exercise induced ST-segment elevation for detection of residual viability: comparison with fluorodeoxyglucose and positron emission tomography. J Am Coll Cardiol. 1995;25:1032–1038. doi: 10.1016/0735-1097(94)00539-3. [DOI] [PubMed] [Google Scholar]
- 5.Margonata A, Ballarotto C, Bonetti F, Cappelletti A, Sciammarella M, Cianflone D, Chierchia LS. Assessment of residual tissue viability by exercise testing in recent myocardial infarction:comparison of the electrocardiogram and myocardial perfusion scintigraphy. J Am Coll Cardiol. 1992;19:948–952. doi: 10.1016/0735-1097(92)90276-s. [DOI] [PubMed] [Google Scholar]
- 6.Mobilia G, Zanco P, Desiseri A, Neri G, Alitto F, Suzzi G, Chierichetti F, Celegon L, Ferlin G, Buchberger T-wave normalization in infarct-related electrocardiographic leads during exercise testing for detection of residual viability. J Am Coll Cardiol. 1998;32:75–82. doi: 10.1016/s0735-1097(98)00205-8. [DOI] [PubMed] [Google Scholar]
- 7.Salustri A, Garyfallidis P, Elhendy A, Ciavatti JH, Cornel JH, Gemelli A. T-wave normalization during dobutamine echocardiography for diagnosis of viable myocardium. Am J Cardiol. 1995;75:505–507. doi: 10.1016/s0002-9149(99)80591-8. [DOI] [PubMed] [Google Scholar]
- 8.Haines DE, Beller GA, Watson DD, Kaise DL, Sayre SL, Gibson RS. Exercise induced ST-segment elevation 2 weeks after uncomplicated myocardial infarction : contributing factors and prognostic significance. J Am Coll Cardiol. 1987;9:996–1003. doi: 10.1016/s0735-1097(87)80299-1. [DOI] [PubMed] [Google Scholar]
- 9.Master AM. The Master two-step test. Am Heart J. 1968;75:809. doi: 10.1016/0002-8703(68)90042-2. [DOI] [PubMed] [Google Scholar]
- 10.Rahiumtoola SH. The hibernating myocardium. Am Heart J. 1989;117:211–221. doi: 10.1016/0002-8703(89)90685-6. [DOI] [PubMed] [Google Scholar]
- 11.Patel B, Kloner RA, Przyklenk K, Braunwald E. Postischemic myocardial stunning. A clinically relevant phenomenon. Ann Intern Med. 1988;108:626. doi: 10.7326/0003-4819-108-4-626. [DOI] [PubMed] [Google Scholar]
- 12.Zimmermann R, Mall G, Raueh B, Zimmer G, Gabel M, Zehelein J, Bubeck B, Tillmanns H, Hagl S, Kuber W. Residual 201 TI activity in irreversible defects as a marker of myocardial viability. Clinicopathological Study Circulation. 1995;91:1016–1021. doi: 10.1161/01.cir.91.4.1016. [DOI] [PubMed] [Google Scholar]
- 13.Bodi V, Sanchis J, Llacer A, Insa L, Chorro FJ, Lopez-Merino V. ST-segment elevation on Q leads at rest and during exercise:relation with myocardial viability and left ventricular remodeling within the first 6 months after infarction. Am Heart J. 1999;137:1107–1115. doi: 10.1016/s0002-8703(99)70370-4. [DOI] [PubMed] [Google Scholar]
- 14.Schneider CA, Helmig AK, Horst M, Erdman E, Sechtem U. Significance of exercise induced ST-segment elevation and T-wave normalization for improvement of function in healed Q-wave myocardial infaction. Am J Cardiol. 1998;82:148–153. doi: 10.1016/s0002-9149(98)00312-9. [DOI] [PubMed] [Google Scholar]
- 15.Marin JJ, Heng MK, Sevrin R, Udhoji VN. Significance of T-wave normalization in the electrocardiogram during exercise stress test. Am Heart J. 1987;114:1342–1348. doi: 10.1016/0002-8703(87)90535-7. [DOI] [PubMed] [Google Scholar]
- 16.Ajisaka R, Watanabe S, Masuoka T, Yamanouchi T, Saitoh T, Toyama M, Takeda Y, Itai Y, Sugishita Y. Relationship between normalization of negative T-waves on exercise ECG and residual myocardial viability in patients with previous myocardial infarction and no postinfarction angina. Jpn Circ J. 1998;62:153–159. doi: 10.1253/jcj.62.153. [DOI] [PubMed] [Google Scholar]
- 17.Waters DD, Chaitman BR, Bourassa MG, Tubau JF. Clinical and angiographic correlates of exercise induced ST-segment elevation:Increased detection with multiple ECG leads. Circulation. 1980;61:286–296. doi: 10.1161/01.cir.61.2.286. [DOI] [PubMed] [Google Scholar]
- 18.Lahiri A, Subramanian B, Millar-Craig M, Crawley J, Raftery EB. Exercise induced ST-elevation in variant angina. Am J Cardiol. 1980;45:887–894. doi: 10.1016/0002-9149(80)90136-8. [DOI] [PubMed] [Google Scholar]
- 19.Lahiri A, Balasubramanian V, Millar Craig MW, Crawley J, Raftery EB. Exercise induced ST segment elevation. Electrocardiographic, angiographic and scintigraphic evaluation. Br Heart J. 1980;43:582–588. doi: 10.1136/hrt.43.5.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chahine RA, Raizner AE, Ishimori T. The clinical significance of exercise induced ST-segment elevation. Circulation. 1976;54:209–213. doi: 10.1161/01.cir.54.2.209. [DOI] [PubMed] [Google Scholar]
- 21.Gewirtz H, Sullivan M, Oreilly G, Winter S, Most AS. Role of myocardial ischemia in the genesis of stress induced ST-segment elevation in previous anterior myocardial infarction. Am J Cardiol. 1983;51:1289–1293. doi: 10.1016/0002-9149(83)90300-4. [DOI] [PubMed] [Google Scholar]
- 22.Elhendy A, Geleijnse ML, Salustri A, van Domburg RT, Cornel JH, Arnese M, Roelandt JR, Fioretti PM. Evaluation by quantitative 99m-technetium MIBI SPECT and echocardiography of myocardial perfusion and wall motion abnormalities in patients with dobutamine-induced ST-segment elevation. Eur H J. 1996;17:526–531. doi: 10.1016/s0002-9149(99)80127-1. [DOI] [PubMed] [Google Scholar]
- 23.Saito M, Asonuma H, Tomita M, Sumiyoshi T, Haze K, Fukami K. Differentiation of myocardial ischemia and left ventricular aneurysm in the genesis of exercise induced ST-T changes in previous anterior myocardial infarction. Jpn Circ J. 1987;51:503–510. doi: 10.1253/jcj.51.503. [DOI] [PubMed] [Google Scholar]


