Abstract
Background
The effects of antihypertensive agents on endothelial function have not been fully evaluated in human hypertension and data on the forearm circulation of humans are controversial. The aim of this study was (1) to evaluate the endothelial function in hypertensive patients (2) to investigate whether vitamin C administration has any benefit on the endothelial function and (3) to determine whether treatment with calcium antagonist improves endothelial dysfunction in hypertensive patients.
Methods
The endothelial function was estimated using venous occlusion plethysmography (VOP) in 8 hypertensive patients and 8 healthy volunteers. The patients in the hypertension group were treated with amlodipine, then examined again. The change of forearm blood flow (FBF) was measured with acetylcholine infusion through brachial artery and also with intra-arterial vitamin C.
Results
Forearm blood flow response to acetylcholine was significantly enhanced with intra-arterial infusion of vitamin C in hypertensive group before antihypertensive treatment. Co-infusion of L-NMMA, an inhibitor of nitric oxide synthase, blunted forearm blood flow response to acetylcholine. After treatment with amlodipine for 2 months in hypertensive group, endothelium-dependent vasorelaxation to acetylcholine was significantly improved compared to pretreatment, and vitamin C did not affect the improved endothelial function by amlodipine treatment.
Conclusion
Vitamin C (acutely) and amlodipine (chronically) improved endothelial function in hypertensive patients. These results suggest that increased oxidative stress, at least in part, may be involved in the decreased endothelial function in hypertension.
Keywords: Plethysmography, Endothelium, Hypertension, Ascorbic acid, Amlodipine
INTRODUCTION
The endothelium plays an important role in maintaining vascular tone and function. The main endothelium derived factor is nitric oxide (NO) which is not only a potent vasodilator but also inhibits platelet aggregation, smooth muscle cell migration and proliferation, monocyte adhesion and adhesion molecule expression, thus protecting the vessel wall against the development of atherosclerosis and thrombosis.
Essential hypertension is associated with alterations in endothelial function. Endothelium-dependent vasodilation in response to substances, such as acetylcholine, bradykinin and substance P and reactive hyperemia, was reduced in brachial1–3), coronary4), renal arteries5, 6) and femoral areteries7) in patients with essential hypertension. Impairment of endothelial function has been shown to play an important role in the development and maintenance of hypertension8). Therefore, an important aim of antihypertensive therapy would be not only to normalize blood pressure values but also to reverse endothelial dysfunction by restoring NO availability.
Several studies have demonstrated the restoration of endothelial function in essential hypertensive patients through the administration of antihypertensive agents8–10), while others have shown that effective antihypertensive therapy did not restore impaired endothelium-dependent vasodilation in the forearm circulation of hypertensive patients11, 12).
The effects of antihypertensive agents on endothelial function have not been fully evaluated in human hypertension and data on the forearm circulation of humans are controversial. It may be clinically important to select an appropriate antihypertensive agent that is effective in improving endothelial dysfunction in patients with established essential hypertension.
Recently, the role of superoxide anion and its interaction with nitric oxide has been investigated13). Under physiological conditions, these oxygen-free radicals are potent chemical inactivators of NO14, 15) and the balance between NO and superoxide is more important than the absolute levels of either alone16).
Vitamin C is an important antioxidant in human plasma, capable of scavenging oxygen-free radicals and sparing other endogenous antioxidants from consumption17).
Therefore, the aim of this study was (1) to evaluate the endothelial function in hypertensive patients (2) to investigate whether vitamin C administration has any benefit on the endothelial function and (3) to determine whether treatment with calcium antagonist improves endothelial dysfunction in hypertensive patients.
METHODS
Subjects
Eight hypertensive patients (age range 35 to 73 years) were recruited. They had a clinical blood pressure reading (the average of 3 different sphygmomanometric measurements, each performed on 3 separate days) of >140/90 mmHg. The possibility of secondary causes of hypertension was excluded by standard clinical and laboratory tests. Exclusion criteria were 1) evidence of overt atherosclerotic disease, i.e., coronary artery disease, peripheral vascular disease, stroke, etc. 2) having other risk factors of atherosclerosis, i.e., current smoking and smoking within 1year, severe hypercholesterolemia (> 240 mg/dL) and diabetes mellitus 3) advanced organ failure 4) malignancy. In all patients, a noninvasive 24-hour blood pressure monitoring was performed at baseline and after treatment. Eight normal volunteers were enrolled who had normal blood pressure. Exclusion criteria were the same as hypertensive group.
Study design
Subjects were randomized to receive amlodipine 5–10 mg daily for at least 2 months. It was only the hypertensives that underwent the treatments. Clinical profiles of the subjects are shown in Table 1. Forearm vascular function was studied before and after antihypertensive treatment. Subjects were required to refrain from drinking alcohol or caffeine-containing beverage for 12 hours before the study.
Table 1.
Clinical characteristics of normal control and hypertensive patients
| NC | HT | |
|---|---|---|
| Number | 8 | 8 |
| Age | 50±4 | 56±3 |
| Sex (m:f) | 2:6 | 3:5 |
| Cholesterol | 182±20 | 191±14 |
| SBP* | 115±4 | 169±8 |
| DBP* | 65±3 | 98±3 |
Values are mean ±SEM,
p<0.05 (NC vs HT) NC, normal control; HT, hypertensive patients group
The protocol of the study was approved by the ethics committee of our institution and informed consent was obtained from each participant. The procedures followed were in accordance with institutional guidelines.
Venous occlusion plethysmography
The examination was done at supine position. The brachial artery of the nondominant arm was cannulated with 20 gauge cannula. A mercury-filled silastic strain gauge was placed around the thickest part of the forearm. The size of the strain gauge was selected to be about 2 cm less than the maximal forearm circumference. The strain gauge was connected to plethysmograph (Hokanson EC-R5, Issaquah, Washington) to record the forearm volume change. A rapid cuff inflator (Hokanson E-10) was used to inflate the arm cuff to 40 mmHg instantaneously, thus occluding venous return from the forearm. A wrist cuff was inflated to 20 mmHg above the systolic pressure to cut off the arterial flow to hand. Intra-arterial pressure was measured continuously (Transpac; Abbot Laboratories) throughout the study. Drug infusions were administered using a constant rate infusion pump. The measurement of forearm volume change was repeated 7 times for each stage. Between infusions, the cuffs were deflated, allowing at least 15 min for forearm blood flow to recover from the preceding infusion and before further baseline measures were recorded. All solutions were prepared aseptically from sterile stock solutions or ampoules immediately before infusion into brachial artery. Acetylcholine and L-NMMA had been diluted in distilled water and filtered through 0.22 m filter.
Evaluation of endothelium-dependent vasodilation and effect of vitamin C
An intra-arterial infusion of 5% dextrose solution was begun at 1 mL/min and continued throughout drug infusion. Basal measurement was obtained during the infusion of dextrose solution. Acetylcholine (Sigma chemical) was infused intra-arterially at 7.5, 15 and 30 g/min. Acetylcholine was infused for 5 minutes for each dose level and forearm blood flow was measured during the last 2 minutes of each dose. After 15 minutes of wash-out period, intra-arterial infusion of vitamin C at 24 mg/min was done for 10 minutes. With continued infusion of vitamin C at the same rate, acetylcholine was infused at the same incremental doses as the previous stage and measurement of forearm blood flow was made during the last 2 minutes of each dose. After another 15 minutes of rest period, intra-arterial infusion of vitamin C at the same rate, plus infusion of L-NMMA (NG-monomethyl-L-arginine, Sigma chemical), an inhibitor of nitric oxide synthesis, was begun at 100 g/min and continued for 5 minutes. Then infusion of acetylcholine at incremental dose and measurement of forearm blood flow were done as in previous stages. (Figure 1).
Figure 1.
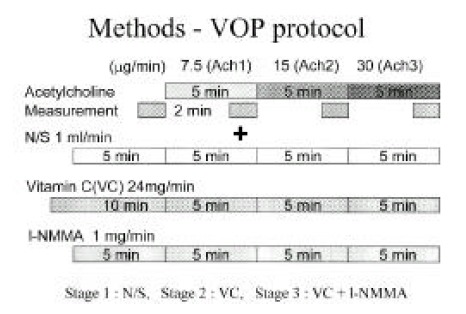
Methods; venous occlusion plethysmography Acetylcholine was infused intra-arterially at 7.5, 15 and 30 g/min for 5 minutes for each dose level and forearm blood flow was measured during the last 2 minutes of each dose. Forearm blood flow response to acetylcholine was assessed during the infusion of dextrose solution (stage 1), intra-arterial infusion of vitamin C (stage 2) and intra-arterial co-infusion of vitamin C and L-NMMA (NG-monomethyl-L-arginine (stage 3).
Statistical analysis
Forearm blood flow was measured and forearm blood flow changes during acetylcholine infusion were expressed as percentage changes from the baseline immediately preceding each drug administration. Forearm blood flow changes were compared between normal and hypertensive groups with and without vitamin C infusion. Comparison was also made between before and after antihypertensive treatment in hypertensive group and forearm blood flow was compared in hypertensive group with and without vitamin C infusion. Repeated measures ANOVA were used in comparison with SAS ver. 6.12 All values were expressed in mean standard error of mean and p<0.05 was considered significant.
RESULTS
Eight hypertensive patients and eight normotensive controls (age range 35 to 73 years) were recruited. There were not any significant differences in cholesterol levels between normotensive controls and hypertensive patients. Only systolic and diastolic blood pressure differed in the two groups (Table 1). After 2-month antihypertensive treatment, there were significant decreases in systolic and diastolic blood pressure (mean blood pressure; 169/98 mmHg → 131/74 mmHg, p<0.05).
Absolute FBF data recorded in the infused limbs at baseline and during the infusion of acetylcholine at three dose levels before and after antihypertensive treatment are presented in Table 2.
Table 2.
Absolute forearm blood flow responses in normal control and hypertensive patients
| NC | HT | post-treatment | |
|---|---|---|---|
| Basal | 4.2±0.6 | 5.7±0.4 | 4.9±0.3 |
| Ach1 | 9.2±1.8 | 7.2±0.6 | 9.7±3.0 |
| Ach2 | 12.9±1.9 | 12.1±1.2 | 13.8±3.2 |
| Ach3 | 17.6±1.9 | 15.9±1.6 | 26.1±4.3 |
Values are means ±SEM in ml/100 ml forearm/min.
NC, normal control; HT, hypertensive patients group;
Ach1, acetylcholine infusion with 7.5 μg/min;
Ach2, acetylcholine infusion with 15 μg/min;
Ach3, acetylcholine infusion with 30 μg/min
FBF in HT and NC groups
Endothelium-dependent vasorelaxation (vasodilatory response to acetylcholine) was significantly greater in normal control group compared to hypertensive group before antihypertensive treatment (maximum forearm blood flow in NC: 448±63%, HT: 302±58%, p<0.05, Figure 2).
Figure 2.
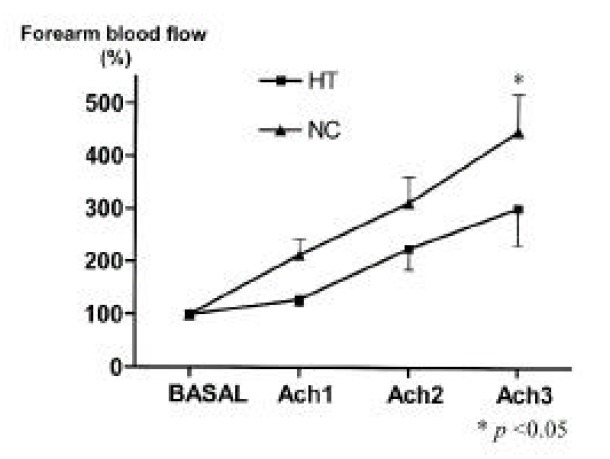
FBF responses to three doses of acetylcholine in normal control and hypertensive patients. Values are mean±SEM. Ach1, Ach2 and Ach3 represent 7.5, 15 and 30 μg/min, respectively.
FBF response to intra-arterial vitamin C infusion
Forearm blood flow response to acetylcholine was significantly enhanced with intra-arterial infusion of vitamin C in hypertensive group before antihypertensive treatment (maximum forearm blood flow in Vit C (−): 302±58%, Vit C (+): 446±43%, p<0.05, Figure 3A). Such an enhanced response was not observed in normal control group (maximum forearm blood flow in Vit C (−): 448±63%, Vit C (+): 383±51%, p=0.11, Figure 3B). Co-infusion of L-NMMA, an inhibitor of nitric oxide synthase, blunted forearm blood flow response to acetylcholine (maximum forearm blood flow in Vit C (+): 446±43%, Vit C +L-NMMA (+): 229±23%, p<0.05, Figure 3C).
Figure 3.
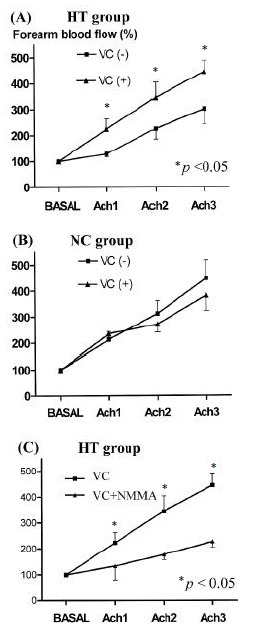
Effect of vitamin C and NMMA on the FBF response to acetylcholine.
FBF after antihypertensive treatment in HT group
After antihypertensive treatment with amlodipine for 2 months in hypertensive group, endothelium-dependent vasorelaxation (vasodilatory response to acetylcholine) was significantly improved in amlodipine treated group compared to before treatment (maximum forearm blood flow in before treatment: 302±58%, after treatment: 539±81%, p<0.05, Figure 4A). Intra-arterial infusion of vitamin C in amlodipine treated hypertensive group did not change the forearm blood flow response to acetylcholine (maximum forearm blood flow in Vit C (−): 539±81%, Vit C (+): 448±78%, p=0.21, Figure 4B).
Figure 4.
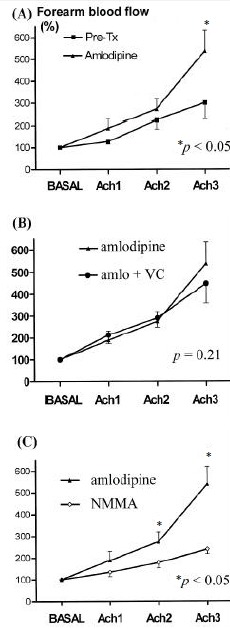
Effect of amlodipine treatment on the vasodilatory response to acetylcholine (A). Intra-arterial infusion of vitamin C in amlodipine treated hypertensive group did not change the forearm blood flow response to acetylcholine (B). Co-infusion of L-NMMA, an inhibitor of nitric oxide synthase, blunted forearm blood flow response to acetylcholine (C).
Co-infusion of L-NMMA, an inhibitor of nitric oxide synthase, blunted forearm blood flow response to acetylcholine in amlodipine treated hypertensive group (maximum forearm blood flow in L-NMMA (−): 539±81%, L-NMMA (+): 240±22%, p<0.05, Figure 4C).
DISCUSSION
The present study demonstrates that the endothelium-dependent vasodilation is impaired in essential hypertensive patients as compared with normotensive control subjects. In addition, short-term, intra-arterial administration of the antioxidant vitamin C restores endothelium-dependent vasodilation in patients with essential hypertension. A nitric oxide (NO) synthase inhibitor, L-NMMA, blunted the improvement of endothelium-dependent vasodilation. These findings suggest that oxygen-derived free radicals may decrease the bioavailability of endothelium-derived nitric oxide and impair endothelium-dependent vasodilation in patients with essential hypertension. These results were consistent with previous observations that, in essential hypertensive patients, impaired endothelium-dependent vasodilation of forearm circulation could be improved by the antioxidant vitamin C3, 18).
Solzbach et al demonstrated that impaired endothelium-dependent vasodilatory function of human coronary arteries in hypertensive patients could be improved by the administration of the antioxidant vitamin C19).
Assessment of the clinical relevance of the present results should take into account the fact that superoxide anion production has been found to cause endothelial dysfunction in the presence of several cardiovascular risk factors. In patients with coronary artery disease, both single dose (2 g PO) and long-term (500 mg/d) administration of vitamin C reverse endothelial vasomotor dysfunction in the brachial circulation20, 21).
With regard to mechanism, it has been proposed that ascorbic acid improves NO action by scavenging superoxide anion and preventing inactivation of NO. This explanation is attractive because atherosclerosis and hypercholesterolemia are linked to excess generation of superoxide, and superoxide reacts with NO and eliminates its biological activity22).
In addition to scavenging superoxide anion or inhibiting LDL oxidation, vitamin C could alernatively improve NO action by sparing intracellular glutathione which, together with vitamin C, is the primary regulator of intracellular redox state.
In essential hypertension, impaired endothelium-dependent vasodilation seems to be a primary phenomenon and the endothelial vasomotor dysfunction is not normalized by the mere reduction of blood pressure12, 23, 24).
Several investigators have addressed the possibility that antihypertensive treatment could restore or at least improve endothelial function.
Calcium antagonists have been shown to be effective in reversing endothelial dysfunction of angiographically normal and stenotic epicardial coronary vessels in essential hypertension25). In agreement with these results, calcium antagonists also show a beneficial effect on endothelial function in the forearm microcirculation26). But several other studies have demonstrated that the treatment with long-term calcium antagonist did not improve forearm vasodilator response to reactive hyperemia9, 10). Hirooka et al also reported that single dose administration of nifedipine did not alter forearm vasodilation with acetylcholine in hypertensive patients27).
In our findings, prolonged (8 weeks of oral treatment) amlodipine administration could improve endothelium -dependent vasodilation in essential hypertensive patients. Intra-arterial infusion of vitamin C to the treated patients did not increase forearm vasodilation in response to acetylcholine. L-NMMA blunted the effect of amlodipine on endothelium-dependent vasodilation. These data indicate that amlodipine is effective in improving endothelial dysfunction in essential hypertension and amlodipine appears to act specifically on the NO pathway by a mechanism that is probably related to antioxidant activity. Experimental data indicate that calcium antagonists exert an antioxidant effect and therefore, could protect endothelial cells against free radical injury and diminish oxidative breakdown of NO28).
An insufficient blood pressure reduction with an antihypertensive drug with antioxidant activity would not improve the endothelial function. So, a sufficient blood pressure reduction with an antihypertensive drug with antioxidant activity would be required. All the hypertensive patients in this study have normalized their systolic and diastolic blood pressure.
CONCLUSION AND IMPLICATIONS
Even though the relative importance of the various possible mechanisms leading to depressed endothelial function in essential hypertension remains to be elucidated, our study shows that vitamin C or amlodipine result in demonstrable improvement by a mechanism that is probably related to antioxidant activity.
REFERENCES
- 1.Linder L, Kiowski W, Buhler FR, Luscher TF. Indirect evidence for release of endothelium-derived relaxing factor in human forearm circulation in vivo: blunted response in essential hypertension. Circulation. 1990;81:1762–1767. doi: 10.1161/01.cir.81.6.1762. [DOI] [PubMed] [Google Scholar]
- 2.Panza JA, Quyyumi AA, Brush JE, Jr, Epstein SE. Abnormal endothelium-dependent vascular relaxation in patients with essential hypertension. N Engl J Med. 1990;323:22–27. doi: 10.1056/NEJM199007053230105. [DOI] [PubMed] [Google Scholar]
- 3.Taddei S, Virdis A, Ghiadoni L, Magagna A, Salvetti A. Vitamin C improves endothelium-dependent vasodilation by restoring nitric oxide activity in essential hypertension. Circulation. 1998;97:2222–2229. doi: 10.1161/01.cir.97.22.2222. [DOI] [PubMed] [Google Scholar]
- 4.Egashira K, Suzuki S, Hirooka Y, Kai H, Sugimachi M, Imaizumi T, Takeshita A. Impaired endothelium-dependent vasodilation in large epicardial and resistance coronary arteries in patients with essential hypertension: different responses to acetylcholine and substance P. Hypertension. 1995;25:201–206. doi: 10.1161/01.hyp.25.2.201. [DOI] [PubMed] [Google Scholar]
- 5.Higashi Y, Oshima T, Sasaki N, Ishioka N, Nakano Y, Ozono R, Yoshimura M, Ishibashi K, Matsuwa H, Kajiyama G. Relationship between insulin resistance and endothelium-dependent vascular relaxation in patients with essential hypertension. Hypertension. 1997;29:280–285. doi: 10.1161/01.hyp.29.1.280. [DOI] [PubMed] [Google Scholar]
- 6.Higashi Y, Oshima T, Ozono R, Matsunra H, Kajiyama G. Aging and severity of hypertension attenuate endothelium-dependent renal vascular relaxation in humans. Hypertension. 1997;30:252–258. doi: 10.1161/01.hyp.30.2.252. [DOI] [PubMed] [Google Scholar]
- 7.Bode-Boger SM, Boger RH, Alfke H, Heinzel D, Tsikas D, Creutzig A, Alexander K, Frolich JC. L-Arginine induces nitric oxide dependent vasodilation in patients with critical limb ischemia. Circulation. 1996;93:85–90. doi: 10.1161/01.cir.93.1.85. [DOI] [PubMed] [Google Scholar]
- 8.Taddei S, Virdis A, Ghiadoni L, Salvetti A. Endothelial dysfunction in hypertension: fact or fancy? J Cardiovasc Pharmacol. 1998;32(Suppl 3):S41–S47. [PubMed] [Google Scholar]
- 9.Iwatubo H, Nagano M, Sakai T, Kumamoto K, Morita R, Higaki J, Ogihara T, Hata T. Converting enzyme inhibitor improves forearm reactive hyperemia in essential hypertension. Hypertension. 1997;29:286–290. doi: 10.1161/01.hyp.29.1.286. [DOI] [PubMed] [Google Scholar]
- 10.Higashi Y, Sasaki S, Nakagawa K, Veda T, Yoshimizu A, Kurisu S, Matsunra H, Kajiyama G, Oshima T. A comparison of angiotensin-converting enzyme inhibitors, calcium antagonists, beta-blockers and diuretic agents on reactive hyperemia in patients with essential hypertension: a multicenter study. J Am Coll Cardiol. 2000;35:284–291. doi: 10.1016/s0735-1097(99)00561-6. [DOI] [PubMed] [Google Scholar]
- 11.Schiffrin EL, Deng LY. Comparison of effects of angiotensin I converting enzyme inhibition and b- blockade for 2 years on function of small arteries from hypertensive patients. Hypertension. 1995;25:699–703. doi: 10.1161/01.hyp.25.4.699. [DOI] [PubMed] [Google Scholar]
- 12.Panza JA, Quyyumi AA, Callahan TS, Epstein SE. Effects of antihypertensive treatment on endothelium -dependent vascular relaxation in patients with essential hypertension. J Am Coll Cardiol. 1993;21:1145–1151. doi: 10.1016/0735-1097(93)90238-v. [DOI] [PubMed] [Google Scholar]
- 13.Creager MA, Roddy MA. Effect of captopril and enalapril on endothelial function in hypertensive patients. Hypertension. 1994;24:499–505. doi: 10.1161/01.hyp.24.4.499. [DOI] [PubMed] [Google Scholar]
- 14.Fridovich I. The biology of oxygen radicals. Science. 1978;201:875–880. doi: 10.1126/science.210504. [DOI] [PubMed] [Google Scholar]
- 15.Mugge A, Elwell JH, Peterson TE, Harrison DG. Release of intact endothelium-dependent relaxing factor depends on endothelial superoxide dismutase activity. Am J Physiol. 1991;260:C219–C225. doi: 10.1152/ajpcell.1991.260.2.C219. [DOI] [PubMed] [Google Scholar]
- 16.McIntyre M, Bohr DF, Dominiczak AF. Endothelial function in hypertension: the role of superoxide anion. Hypertension. 1999;34:539–545. doi: 10.1161/01.hyp.34.4.539. [DOI] [PubMed] [Google Scholar]
- 17.Frei B, England L, Ames BN. Ascorbate is an outstanding antioxidant in human blood plasma. Proc Natl Acad Sci USA. 1989;86:6377–6381. doi: 10.1073/pnas.86.16.6377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Natali A, Sironi AM, Toschi E, Camasfra S, Sanna G, Perissinotto A, Taddei S, Ferrannini E. Effect of vitamin C on forearm blood flow and glucose metabolism in essential hypertension. Arterioscler Thromb Vase Biol. 2000;20:2401–2406. doi: 10.1161/01.atv.20.11.2401. [DOI] [PubMed] [Google Scholar]
- 19.Solzbach U, Hornig B, Jeserich M, Just H. Vitamin C improves endothelial dysfunction of epicardial coronary arteries in hypertensive patients. Circulation. 1997;96:1513–1519. doi: 10.1161/01.cir.96.5.1513. [DOI] [PubMed] [Google Scholar]
- 20.Levine GN, Frei B, Koulouris SN, Gerhard MD, Keaney JF, Vita JA. Ascorbic acid reverses endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation. 1996;93:1107–1113. doi: 10.1161/01.cir.93.6.1107. [DOI] [PubMed] [Google Scholar]
- 21.Gokce N, Keaney JF, Frei B, Holbrook M, Olesiak M, Zachariah BJ, Leeuwenburgh C, Meinecke JW, Vita JA. Long-term ascorbic acid administration reverses endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation. 1999;99:3234–3240. doi: 10.1161/01.cir.99.25.3234. [DOI] [PubMed] [Google Scholar]
- 22.Ohara Y, Peterson TE, Harrison DG. Hypercholesterolemia increases endothelial superoxide anion production. J Clin Invest. 1993;91:2546–2551. doi: 10.1172/JCI116491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lind L, Millgard J, Sarabi M, Kahan T, Malmqvist K, Hagg A. Endothelium-dependent vasodilation in treated and untreated hypertensive subjects. Blood Press. 1999;8:158–164. doi: 10.1080/080370599439689. [DOI] [PubMed] [Google Scholar]
- 24.Taddei S, Virdis A, Ghiadoni L, Sudano I, Salvetti A. Antihypertensive drugs and reversing of endothelial dysfunction in hypertension. Curr Hypertens Rep. 2000;2:64–70. doi: 10.1007/s11906-000-0061-8. [DOI] [PubMed] [Google Scholar]
- 25.Frielingsdorf J, Seiler C, Kauffman P, Vassalli G, Suter T, Hess OM. Normalization of abnormal coronary vasomotion by calcium antagonists in patients with hypertension. Circulation. 1996;93:1380–1387. doi: 10.1161/01.cir.93.7.1380. [DOI] [PubMed] [Google Scholar]
- 26.Taddei S, Virdis A, Ghiadoni L, Uleri S, Magagna A, Salvetti A. Lacidipine restores endothelium-dependent vasodilation in essential hypertensive patients. Hypertension. 1997;30:1606–1612. doi: 10.1161/01.hyp.30.6.1606. [DOI] [PubMed] [Google Scholar]
- 27.Hirooka Y, Imaizumi T, Masaki H, Ando S, Harada S, Momohara M, Takeshita A. Captopril improves impaired endothelium-dependent vasodilation in hypertensive patients. Hypertension. 1992;20:175–180. doi: 10.1161/01.hyp.20.2.175. [DOI] [PubMed] [Google Scholar]
- 28.Mak IT, Boehme P, Weglicki WB. Antioxidant effects of calcium channel blockers against free radical injury in endothelial cells. Correlation of protection with preservation of glutathione levels. Circ Res. 1992;70:1099–1103. doi: 10.1161/01.res.70.6.1099. [DOI] [PubMed] [Google Scholar]


