Abstract
Background:
Primary lymphoma of bone is a rare disease. There is yet no systematical evaluation of primary lymphoma of bone in Korea. Here we report our experience of sixteen cases with primary lymphoma of bone focusing on the survival.
Methods:
Sixteen cases, collected for 13 years, were evaluated on the clinical presentation, histologic subtype, stage and treatment outcomes of the primary bone lymphoma.
Results:
The most common presenting complaint was bone pain. Malignant lymphoma of bone involved a wide variety of sites, the most prevalent site of which in this study was the spine. Most of the cases were in the diffuse large B-cell category. The clinical stage of lymphoma was IEA in two cases, IIEA in three cases, IVEA in five cases and IVEB in three cases. All treated cases received systemic chemotherapy and ten cases among them were treated with combined modality therapy. Median overall survival was not reached after median follow-up period of 28 months and five-year overall survival rate was 54%.
Conclusion:
More promising therapeutic strategies are needed for survival improvement on more accumulated cases.
Keywords: Bone and Bones, Lymphoma, Survival, Prognosis
INTRODUCTION
Primary lymphoma of bone (PLB) was previously called reticulum cell sarcoma. It accounts for only 5% of the primary bone tumor and constitutes approximately 3–15% of all extranodal non-Hodgkin’s lymphoma (NHL)1,2). Although the diagnosis of primary lymphoma of bone was first suggested by Oberling in 1928, the disease was established as an entity in 1939 by Parker and Jackson3), who reported 17 cases. In general, lymphoma presenting in bone is a sign of disseminated (stage IV) disease, but it may be a true solitary lesion, defined as involvement of single extralymphatic organ or site (stage IE).
There is yet no systematical evaluation of PLB in Korea. Here we report our experience of 16 cases with PLB focusing on the survival.
MATERIALS and METHODS
Sixteen cases with PLB at Yonsei Medical Center between January 1988 and July 2001 were retrospectively evaluated.
Four cases presented with the solitary lymphoma of bone which was defined as lymphoma presenting in an osseous site with no evidence of disease elsewhere for at least 6 months after diagnosis. Nine cases presented with multifocal bone involvement, that is, lymphoma in two or more osseous sites only, without evidence of soft tissue or nodal involvement. And three cases presented with simultaneous bone and nodal or soft tissue involvement.
The histopathological classification was done according to the WHO classification.
Patients were retrospectively staged according to the Ann Arbor staging system. The work-up for staging included complete physical examination, complete blood count, chemistry panel, computerized tomographic scan of neck, chest and abdomen, whole body bone scan, gallium scan, PET scan and bone marrow aspiration and biopsy. A skeletal magnetic resonance image was obtained in five cases. CT scan was also performed in the abdomino-pelvic area in 13 cases, the chest in 13, the neck in 13 and the brain in 10. Whole body bone scan was done in 13 cases and gallium scan was done in 10. Bone marrow study was done in 15 cases.
Response to treatment was recorded as complete remission (CR), partial remission (PR) or no response (NR). CR was defined as a complete disappearance of all clinical evidence of lymphoma by physical examination and imaging studies; PR as a reduction of more than 50% in the sum of the products of perpendicular diameters of all measurable masses with no new lesion; NR as stable or progressive disease except CR or PR.
The overall survival time was calculated from the date of diagnosis until the date of the last follow-up or death. The disease-free survival time was calculated from the date of documentation of CR until the date of the last follow-up in a disease-free state. Survival curves were calculated according to the Kaplan-Meier method and comparison of survival was performed using the log-rank test.
RESULTS
Age and sex
Of the 16 cases studied, ten were male and six were female with a ratio of 1:0.6 (Table 1). The median age was 44 years (range, 1–71 years).
Table 1.
Clinical, histological and therapeutic parameters of the patients
| Number of cases | Percentage (%) | |
|---|---|---|
| Sex | ||
| Male | 10 | 62 |
| Female | 6 | 37 |
| Age | ||
| >60 years | 25 | |
| ≤ 60 years | 12 | 75 |
| Stage | ||
| I | 2 | 12 |
| II | 3 | 19 |
| III | 0 | 0 |
| IV | 8 | 50 |
| Uncertain | 3 | 19 |
| Histology (WHO classification) | ||
| Diffuse follicular center | 1 | 6 |
| T cell rich B cell | 1 | 6 |
| Diffuse large cell | 10 | 62 |
| Precursor B lymphoblastic leukemia/lymphoma | 1 | 6 |
| Hodgkin’s disease (mixed cellularity) | 1 | 6 |
| Peripheral T cell, not otherwise specified | 1 | 6 |
| Unspecified | 1 | 6 |
| Cell type | ||
| T cell | 1 | 6 |
| B cell | 14 | 88 |
| Unspecified | 1 | 6 |
| International Prognostic Index score | ||
| Low (0–1) | 4 | 25 |
| Low intermediate (2) | 5 | 31 |
| High intermediate (3) | 0 | 0 |
| High (4–5) | 4 | 25 |
| Unknown | 3 | 18 |
| Therapy | ||
| Chemotherapy only | 3 | 18 |
| Radiotherapy and chemotherapy | 8 | 50 |
| Radiotherapy only | 0 | 0 |
| Surgery, radiotherapy and chemotherapy | 2 | 12 |
| No treatment | 3 | 18 |
| Response to therapy | ||
| Complete remission | 7 | 53 |
| Partial remission | 3 | 23 |
| No response | 3 | 23 |
Clinical manifestation
The most common presenting complaints were bone pain (Table 2). Three cases presented with B symptoms. Neurologic symptom (voiding difficulty) was present in two cases. Pathologic fracture was present in one case.
Table 2.
Presenting signs and symptoms
| Symptom and sign | Number of cases |
|---|---|
| Pain of bone | 10 |
| Mass | 3 |
| Fever | 2 |
| Voiding difficulty | 2 |
| Fracture | 1 |
| Swelling | 1 |
Site of involvement
PLB involved a wide variety of sites (Figure 1). Femur and thoracic spine, which appeared in 6 cases, were the most commonly involved sites at diagnosis. The PLB most often presented in the irregular bone (T spine, femur, L spine, ileum and C spine in order).
Figure 1.
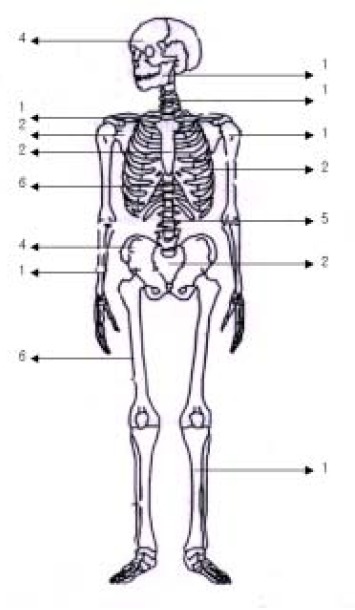
Site of involvement. The sites of involvement are included in the figure; femur 6 cases; thoracic spine 6 cases; lumbar spine 5 cases; skull 4 cases; ileum 4 cases; rib 2 cases; sacrum 2 cases; scapula 2 cases; sternum 2 cases; clavicle 1 case; humerus 1 case; mandible 1 case; cervical spine 1 case; tibia 1 case; ulna 1 case
Histological classification
Using the WHO classification, most of the cases were in the diffuse large B-cell category (Table 1). One case was classified as Hodgkin’s disease. T-cell immunophenotype was noted in one case.
Clinical staging
The clinical stage of lymphoma was IEA in two cases, IIEA in three cases, IVEA in five cases and IVEB in three cases (Table 1). Stage II diseases had lymph node involvement near the site of the bone localization.
Response to treatment, survival and prognostic factors
Among treated thirteen cases, three cases were treated with only chemotherapy, eight cases with radiotherapy and chemotherapy and two cases with surgery, radiotherapy and chemotherapy. Radiotherapy was delivered by either linear accelerator or cobalt-60. Radiation dose ranged from 30 to 60 Gy with a median dose of 45 Gy.
Seven cases (54%) of all treated cases achieved CR, three cases (23%) PR and three cases (23%) NR (Table 1). The median follow-up period was 28 months (range, 2–108 months). The median disease-free survival of seven cases which achieved CR was not reached (range, 15–97 months) and five-year disease-free survival rate was 85%. The median overall survival of all treated cases was not reached (range, 2–108 months) and five-year overall survival rate was 54% (Figure 2).
Figure 2.
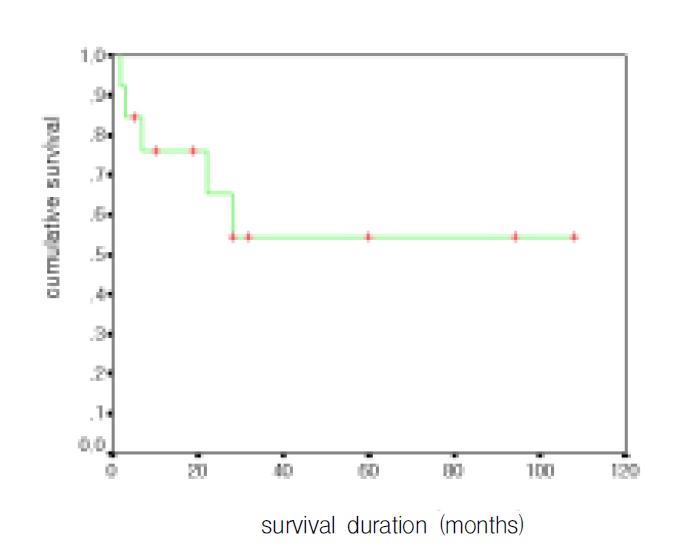
Overall survival (months) of treated patients (N=13)
There was no significant difference of overall survival according to stage, performance, LDH and IPI (International Prognostic Index) scores (Figure 3).
Figure 3.
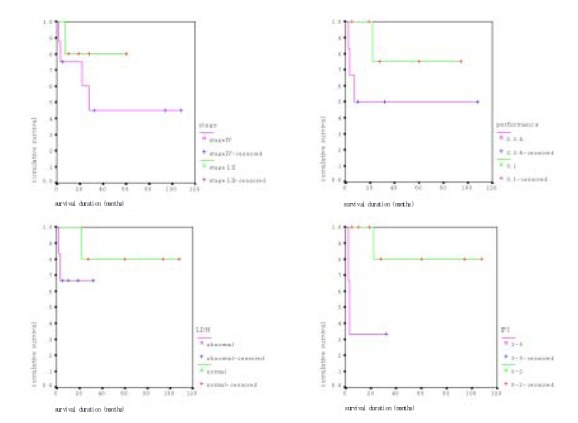
Comparison of overall survival according to stage (stage I, II vs. stage IV, p=0.392), performance (ECOG 0, 1 vs. 2–4, p=0.1974), LDH (normal vs. abnormal, p=0.3235) and IPI score (0–2 vs. 3–5, p=0.0537)
DISCUSSION
PLB (previously called reticulum cell sarcoma) is a rare lymphoid malignancy and accounts for approximately 3–15% of all extranodal non-Hodgkin’s lymphoma2,4). The true incidence of PLB is difficult to assess, as the site of origin is unclear in patients with disseminated lymphoma and bony involvement. In Korea, PLB accounts for about 1.3–1.6% of all malignant lymphoma, 1.4–1.8% of non-Hodgkin’s lymphoma and 3.7% of extranodal non-Hodgkin’s lymphoma5,6), while there was no report of primary lymphoma of bone in Hodgkin’s disease. Song et al.7) reported the first case of primary bone lymphoma associated with acquired immunodeficiency syndrome in Korea. During this study, primary lymphoma of bone accounted for 1% (16/1,600 cases) of malignant lymphoma, 1% (15/1,448 cases) of non-Hodgkin’s lymphoma and 0.65% (1/152 cases) of Hodgkin’s disease in Severance Hospital.
In general, lymphoma presenting in bone is a sign of disseminated (stage IV) disease. But, occasionally, it may be a true solitary lesion, defined as involvement of single extralymphatic organ or site (stage IE)8–10). Reimer et al.8) reported that only one of twelve presenting with bone lymphomas had a true solitary lesion. Sweet et al.9) reported that 50% of so called solitary lesions were associated with disease elsewhere. He emphasized that all cases with a presumed solitary lymphoma of bone should undergo a thorough evaluation for other involvement. Many studies on primary lymphoma of bone excluded patients with stage IV disease in an effort to eliminate malignancies in which bone involvement is secondary11,12). In our study, three cases (19%) presented with simultaneous bone and nodal or soft tissue involvement and nine cases (56%) presented with multifocal bone involvement.
The peak incidence appears to be in the fifth decade, with a slight preponderance of males over females13). In our study, age and sex distribution were similar to other studies (median age at presentation was 44 years and there was a male predominance with a male to female ratio of 1:06). In most of our cases, the initial symptoms were localized bone pain or swelling, as reported by others14). Pathologic fractures are possible complication of bone lymphoma. Kenan et al.15) reported 6 cases (30%) with pathologic fracture among 20 cases of primary skeletal lymphoma. In our study there was one case (6.3%) with pathologic fracture.
Malignant lymphoma of bone involved a wide variety of sites as reported by others15). The most prevalent site in this studies was the irregular bone. In one study, tumor localization within the pelvis or vertebra was associated with a worse prognosis16), but in our study tumor localization was not a significant prognostic factor.
Although the histomorphologic features of malignant lymphomas of lymph nodes have been extensively studied in relation to prognosis, there are relatively few similar studies of lymphomas of bone16,17). Most of the lesions were in the diffuse large B-cell category, as other studies16). Some study revealed that histologic subgroup has no prognostic significance15), but in one study, immunoblastic lymphoma had a worse prognosis than other large B cell lymphoma subtypes10). In our study, there was no significant difference in overall survival between histologic grades (data was not shown).
The stage of the disease is the single most important prognostic indicator in malignant lymphoma of bone10,18,19). In this study, the 5-year overall survival rate of stage I or II disease was 80% and the 5-year overall survival rate of stage IV disease was 45%. But there was no significant difference between the two groups (p=0.3920).
Treatment of bone lymphoma is based on the extent of disease. Stage IE lesions have traditionally been treated with radiotherapy, with which the cure rate is reported up to 90%. Some studies suggested that the outcomes are superior for patients with primary bone lymphoma who are treated with combined modality therapy versus single modality therapy20), while other studies did not detect any difference between treatments21). In this study, all treated patients received systemic chemotherapy. And ten cases were treated with combined modality therapy. Of ten cases who were treated with combined modality therapy, six achieved complete remission, but of three cases who were treated with chemotherapy alone one achieved complete remission. But there was no significant difference in overall survival between treatment modalities (p=0.66).
The overall survival of PLB was reported variably by many authors. Bacci et al.22) reported on 30 cases treated for localized PLB over a 10-year period, with overall disease-free survival rate of 88% at a mean follow-up period of 87 months. Mendenhall et al.18) reported their experience with 11 cases who received combined modality therapy, nine cases who received local radiotherapy alone and one case who received chemotherapy alone. In the study, five-year overall survival rate was 56% and no treatment modality demonstrated any advantage. Susnerwala et al.23) reported on 39 cases treated for PLB over a 10-year period. In their report, overall and disease-free survival rates at 60 months were 66% and 56%, respectively. Barr et al.24) reported on 17 cases with PLB, overall survival of which was 79%. Heyning et al.10) reported on 60 cases with PLB which included the disseminated (stage IV) disease. In their report, the five-year overall survival rate was 61%.
The median overall survival in our study was not reached after median follow-up period of 28 months. And our study revealed 54% of five-year overall survival rate. The overall survival of our study was similar or inferior to other studies10,18,22–24). Considering that our study included multifocal skeletal lymphomas, the overall survival was considered to be similar to other studies10,18,22–24). More promising therapeutic strategies are needed for survival improvement on more accumulated cases.
Table 3.
Summary of clinical characteristics of 16 cases
| No | Age/Sex | Site of involvement | Symptom | Symptom duration (months) | Histology (WHO classification) | Stage | Operation | Chemotherapy | Radiation dose (cGy) | Response to induction | Overall survival (months) | Disease-free survival (months) | Current status (cause of death) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M/49 | Mandible, femur | submandible mass | 3 | diffuse follicular center | IVEA | CHOP | 4500 | CR | 94 | 87 | alive | |
| 2 | M/24 | T8, L5, S1 spine, femur, ilium, skull | back pain | 1 | diffuse mixed small and large B cell (Working formulation) | IVEA | MACOP-B IMVP16 DHAP Steroid pulse |
4080 | CR | 28 | 20 | death (marrow failure, pneumonia, brain hemorrhage) | |
| 3 | M/49 | Rib, C spine, T spine, L spine, skull | fever | 2 | T cell rich B cell (large B cell, variant) | IVEB | M-BACOP, IMVP-16, HOAP-Bleo | none | CR | 108 | 97 | alive | |
| 4 | M/20 | Clavicle, skull, femur, L1 | back pain | 4 | precursor B lymphoblastic leukemia/lymphoma | IVEB | MACOP-B | none | NR | 3 | death (panperitonitis) | ||
| 5 | M/27 | T spine, L spine | back pain | 10 days | diffuse large B cell | IVEA | laminectomy | CHOP HOAP-Bleo IMVP-16 |
3550 | CR | 32 | 15 | alive |
| 6 | M/40 | Ilium | pelvic pain | 8 | diffuse large B cell | uncertain | none | none | 12 | death | |||
| 7 | M/47 | Humerus, femur, skull, TLS spine, ilium | back pain, voiding difficulty | 2 | diffuse large B cell | IVEA | CVP | 3000 | NR | 2 | death (pneumonia) | ||
| 8 | M/64 | Sacrum, sternum | coccyx pain, voiding difficulty | 1 | diffuse large B cell | uncertain | none | none | 15 | death (pneumonia) | |||
| 9 | M/29 | Sternum, T spine | sternal pain, back pain | 3 | diffuse large B cell | IVEA | M-BACOD | 6000 | PR | 22 | death (PCP pneumonia, AIDS) | ||
| 10 | M/21 | Rib, T spine, sacrum, ilium | Fever | 1.5 | Hodgkins disease (mixed cellularity) | IVEB | ABVD | 2520 | PR | 5 | alive | ||
| 11 | F/59 | Tibia | tibia pain | 1 | diffuse large B cell | IIEA | ampulation | VCR+ADR+ Endoxan+ Dactinomycin |
6000 | NR | 7 | death (brain hemorrhage) | |
| 12 | F/63 | Femur | fracture | 1 day | diffuse large B cell | uncertain | none | none | 3 | death (liver cirrhosis, HCC, pneumonia) | |||
| 13 | F/63 | Scapula | shoulder mass | 4 | diffuse large B cell | IIEA | CEOP | 4500 | CR | 19 | 12 | alive | |
| 14 | F/71 | Ulna | elbow pain | 12 | diffuse large B cell | IIEA | M-BACOP | 5040 | CR | 28 | 20 | alive | |
| 15 | F/44 | Femur | knee pain, swelling | 5 | diffuse large B cell | IEA | M-BACOP | 6000 | CR | 60 | 53 | alive | |
| 16 | F/1 | Scapula | scapular mass | 20 days | peripheral T cell, unspecified | IEA | BECOP | none | PR | 10 | alive |
CR, complete remission; PR, partial remission; NR, no response; PCP, Pneumocystis carinii pneumonia; AIDS, acquired immunodeficiency syndrome; HCC, hepatocellular carcinoma;
CHOP, cyclophosphamide, adriamycin, vincristine, and prednisolone; MACOP-B, methotrexate, adriamycin, cyclophosphamide, vincristine, prednisolone, and bleomycin, HOAP-Bleo; adriamycin, vincristine, cytosine arabinoside, prednisolone, and bleomycin, IMVP-16; ifosfamide, methothrexate, and etoposide, CVP; cyclophosphamide, vincristine, and prednisolone, CEOP; cyclophosphamide, epirubicin, vincristine, and prednisolone; M-BACOP(D), methotrexate, bleomycin, adriamycin, cyclophosphamide, vincristine, and prednisolone (dexamethasone); DHAP, dexamethasone, cytarabine, and cisplatin; BECOP, bleomycin, epirubicin, cyclophosphamide, vincristine, prednisolone; ABVD, doxorubicin, bleomycin, vinblastine, and dacarbazine
REFERENCES
- 1.Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972;29:252–260. doi: 10.1002/1097-0142(197201)29:1<252::aid-cncr2820290138>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 2.Rudders RA, Ross ME, DeLellis RA. Primary extranodal lymphoma. Response to treatment and factors influencing prognosis. Cancer. 1978;42:406–416. doi: 10.1002/1097-0142(197808)42:2<406::aid-cncr2820420205>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 3.Parker F, Jackson H. Primary reticulum cell sarcoma of bone. Surg Gynecol Obstet. 1939;68:45–53. [Google Scholar]
- 4.Rosenberg SA, Diamond HD, Jaslowitz B, Cravwer LF. Lymphosarcoma. A review of 1269 cases. Medicine. 1961;40:31–81. doi: 10.1097/00005792-196102000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Hahn JS, Lee S, Chong SY, Min YH, Ko YW. Eight-year experience of malignant lymphoma. Yonsei Med J. 1997;38(5):270–284. doi: 10.3349/ymj.1997.38.5.270. [DOI] [PubMed] [Google Scholar]
- 6.Hahn JS, Ko YW, Min YH, et al. Statistical analysis of malignant lymphoma in Korea. Kor J Hematol. 1995;30:197–214. [Google Scholar]
- 7.Song YG, Hahn JS, Choi YH, Yeom JS, Yang WI, Seo CO, Kim JM. A case of primary bone lymphoma associated with acquired immunodeficiency syndrome. Yonsei Med J. 1998;39(4):383–389. doi: 10.3349/ymj.1998.39.4.383. [DOI] [PubMed] [Google Scholar]
- 8.Reimer RR, Chabner BA, Young RC, Reddick R, Johnson RE. Lymphoma presenting in bone. Results of histopathology, staging and therapy. Ann Intern Med. 1977;87:50–55. doi: 10.7326/0003-4819-87-1-50. [DOI] [PubMed] [Google Scholar]
- 9.Sweet DL, Mass DP, Simon MA, Shapiro CM. Histiocytic lymphoma (reticulum cell sarcoma) of bone. Current strategy for orthopaedic surgeons. J Bone Joint Surg. 1981;63:79–84. [PubMed] [Google Scholar]
- 10.Heyning FH, Hogendoorn PCW, Kramer MHH, Hermans J, Kluin-Nelemans JC, Noorkijk EM, Kluin PhM. Primary non-Hodgkin’s lymphoma of bone: a clinicopathological investigation of 60 cases. Leukemia. 1999;13:2094–2098. doi: 10.1038/sj.leu.2401582. [DOI] [PubMed] [Google Scholar]
- 11.Rathmell AJ, Gospodarowicz MK, Sutcliffe SB, Clark RM. Localized lymphoma of bone. Prognostic factors and treatment recommendations. The Princess Margaret Hospital lymphoma group. Br J Cancer. 1992;66:603–606. doi: 10.1038/bjc.1992.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fairbanks RK, Bonner JA, Inwards CY, Strickler JG, Habermann TM, Unni KK, Su J. Treatment of stage IE primary lymphoma of bone. Int J Radiat Oncol Biol Phys. 1994;28:363–372. doi: 10.1016/0360-3016(94)90059-0. [DOI] [PubMed] [Google Scholar]
- 13.Joseph B, Ronald LB, Mary G. Primary Non-Hodgkin’s Lymphoma of Bone. Semin Oncol. 1999;26:270–275. [PubMed] [Google Scholar]
- 14.Vassallo J, Roessner A, Vollmer E, Grundmann E. Malignant lymphomas with primary bone manifestation. Path Res Pract. 1987;182:381–389. doi: 10.1016/S0344-0338(87)80074-2. [DOI] [PubMed] [Google Scholar]
- 15.Kenan B, Yusuf Y, Yener S, Murat A, Hamit O, Mustafa S, Selim E. Primary lymphoma of bones. Int Orthop. 2001;25:123–126. doi: 10.1007/s002640100224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ostrowski ML, Unni KK, Banks PM, Shives TC, Evans RG, OConnell MJ, Taylor WF. Malignant lymphoma of bone. Cancer. 1986;58:2646–2655. doi: 10.1002/1097-0142(19861215)58:12<2646::aid-cncr2820581217>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 17.Dosoretz DE, Raymond AK, Murphy GF, Doppke KP, Schiller AL, Wang CC, Suit HD. Primary lymphoma of bone. The relationship of morphologic diversity to clinical behavior. Cancer. 1982;50:1009–1014. doi: 10.1002/1097-0142(19820901)50:5<1009::aid-cncr2820500532>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 18.Mendenhall NP, Jones JJ, Kramer BS, Hudson TM, Carter RL, Enneking WF, Marcus RB, Million RR. The management of primary lymphoma of bone. Radiother Oncol. 1987;9:137–145. doi: 10.1016/s0167-8140(87)80201-3. [DOI] [PubMed] [Google Scholar]
- 19.Sothi S, Spooner D. Primary bone lymphoma. Treatment and outcome. J Bone Joint Surg. 1998;80:202. doi: 10.1016/j.clon.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Panos F, Ira S, Mark LS, Gunnlaugur PN, Eugene FR, Henry M, Herman DS, David CH. Long-term results of combined modality therapy in primary bone lymphomas. Int J Radiation Oncology Biol Phys. 1999;45:1213–1218. doi: 10.1016/s0360-3016(99)00305-3. [DOI] [PubMed] [Google Scholar]
- 21.Dubey P, Ha CS, Besa PC, Fuller L, Cabanillas F, Murray J, Hess MA, Cox JD. Localized primary malignant lymphoma of bone. Int J Radiat Oncol Biol Phys. 1997;37:1087–1093. doi: 10.1016/s0360-3016(97)00106-5. [DOI] [PubMed] [Google Scholar]
- 22.Bacci G, Jaffe N, Emiliani E, Van Horn J, Manfrini M, Picci P, Bertoni F, Gherlinzoni F, Campanacci M. Therapy for primary non-Hodgkin’s lymphoma of bone and a comparison of results with Ewings sarcoma. Ten years’ experience at the Istituto Ortopedico Rizzoli. Cancer. 1986;57:1468–1472. doi: 10.1002/1097-0142(19860415)57:8<1468::aid-cncr2820570806>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 23.Susnerwala SS, Dinshaw KA, Pande SC, Shrivastava SK, Gonsalves MA, Advani SH, Gopal R. Primary lymphoma of bone. Experience of 39 cases at the Tata Memorial Hospital, India. J Surg Oncol. 1990;44:229–233. doi: 10.1002/jso.2930440408. [DOI] [PubMed] [Google Scholar]
- 24.Baar J, Burkes RL, Bell R, Blackstein ME, Fernandes B, Langer F. Primary non-Hodgkin’s lymphoma of bone. A clinicopathologic study. Cancer. 1994;73:1194–1199. doi: 10.1002/1097-0142(19940215)73:4<1194::aid-cncr2820730412>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]


