Abstract
Background :
An appreciable number of patients with toluene diisocyanate (TDI)-induced asthma have high serum levels of specific IgE (sIgE) antibody to TDI-human serum albumin conjugate (HSA). A recent investigation suggested a role of specific IgG (sIgG) in the development of TDI asthma.
Methods :
We observed the changes in the levels of specific IgE and IgG antibodies to TDIHSA conjugate in TDI-induced asthmatic patients during seven years avoidance.
Results :
Six subjects with high sIgE and five with high sIgG were enrolled. All of them had taken anti-asthmatic medications with complete avoidance. Serum levels of sIgE and sIgG to TDI-HSA conjugate were detected by ELISA. The level of sIgE continued to decline up to 7 years and the mean half-life was 3.9 years. The mean half-life of sIgG was 4.5 yrs.
Conclusion :
These findings suggest that both sIgE and sIgG to TDI-HSA conjugate may persist for several years after the last exposure to TDI.
Keywords: TDI-induced asthma, Specific IgE, Specific IgG, Half-life
INTRODUCTION
An appreciable number of patients with TDI-asthma do not recover completely even after several years from exposure to TDI1). Our previous study demonstrated that sIgG to TDI-HSA conjugate, not sIgE, was more closely associated with TDI bronchoprovocation test (BPT) results and a possible role of sIgG in the development of TDI asthma was suggested2). A twelve-year follow-up study3) of tetrachlorophthalic anhydride (TCPA)-induced asthma showed that sIgE level fell over several years with persistent airway hyperresponsiveness and asthmatic symptoms. One case study4) of isocyanate-induced asthma for 2 years revealed that the half-life of sIgE antibody to TDI-HSA conjugate was 5.8 months. However, there has been little data dealing with changes in the levels of sIgE or sIgG antibodies for periods greater than 5 years. In this study, we observed changes in the levels of serum sIgE and sIgG in TDI-induced asthmatic subjects after complete avoidance and using anti-asthmatic medications for over 7 years.
SUBJECTS AND METHOD
Six patients with high sIgE and 5 with high sIgG at initial diagnosis were studied every year for up to 7 years. The clinical and laboratory findings are shown in Table 1. All the subjects had persistent asthmatic symptoms requiring anti-asthmatic medications and follow-up methacholine challenge tests revealed persistent airway hyperresponsiveness. Sera were collected before the treatment and every year for 1 to 7 years (one for 1 year, one for 4 years, one for 5 years, one for 6 years, two for 7 years) and kept frozen until ELISA was performed. Their bronchial sensitization was confirmed by TDI-BPT. The methacholine bronchial challenge and the TDI-BPT were performed according to the previously described methods1, 4). Their clinical features are summarized in Table 1. All the subjects gave their informed consents, which were regulated by the Institutional Review Board of Ajou Medical Center, Suwon, Korea.
Table 1.
Clinical characteristics of patients with toluene diisocyanate (TDI)-induced occupational asthma
| Patient | Sex/Age | Latent period (yrs) | Follow-up period (yrs) | Atopy | Specific IgE | Specific IgG | Methacholine PC20 (mg/mL) |
|---|---|---|---|---|---|---|---|
| CK | M/36 | 15 | 6 | − | − | + | 5.0 |
| KS | M/35 | 8 | 8 | + | + | + | 0.16 |
| KT | M/49 | 13 | 9 | + | + | + | 0.44 |
| AJ | M/44 | 7 | 7 | + | + | − | 15.0 |
| JB | M/36 | 7 | 8 | + | + | + | 0.65 |
| SJ | M/51 | 8 | 9 | + | + | − | 2.02 |
| SS | M/45 | 3 | 1 | + | + | − | 1.20 |
| RJ | M/47 | 15 | 4 | + | − | + | 2.5 |
Specific IgE and IgG antibodies to TDI-HSA conjugate by ELISA
Preparation of TDI-HSA conjugate and ELISA were performed according to the method described previously2). In brief, ELISA plate was coated with 1 g of TDI-HSA conjugate or HSA dissolved in 0.1 M sodium bicarbonate buffer, pH 9.5, then washed with PBS-Tween 20 and blocked with blocking buffer (PBS containing 5% bovine serum albumin, 0.1% Tween 20). Fifty I of diluted serum (1:500 for sIgG, 1:10 for sIgE) from patients or controls was incubated in both TDI-HSA and HSA-coated wells, respectively. Peroxidase-conjugated anti-IgG (1:500 v/v, Vector Laboratories, Burlingame, CA) or biotinylated anti-human IgE (1:500 v/v, Sigma Co., St. Louis, MO) was incubated. As substrate, O-phenyl deamine for sIgG and streptavidin-peroxidase and TMB (3,3′, 5,5′ tetramethylbenzidine <Sigma Co., St Louis, MO>) for sIgE were added. Reactions were stopped with H2SO4 and read using ELISA reader. Final absorbance value was decided after the subtraction of HSA-coated value from TDI-HSA coated value. Positive cut-off value was determined as mean plus 2×S.D. of the absorbance values from 20 unexposed healthy controls. All the sera were run on one day.
RESULTS
Changes of specific IgE and IgG antibody to TDI-HSA conjugate, Figure 1, demonstrate the changes in the levels of sIgE to TDI-HSA conjugate after complete avoidance. They continued to fall for up to 7 years. The mean half-life, calculated from the time of stopping exposure, was 3.9 years, ranging from 2.3 to 4.8 years. Figure 2 demonstrates the changes in the levels of sIgG to TDI-HSA conjugate. The mean half-life was 4.5 yrs, ranging from 1.7 to 6.7 years.
Figure 1.
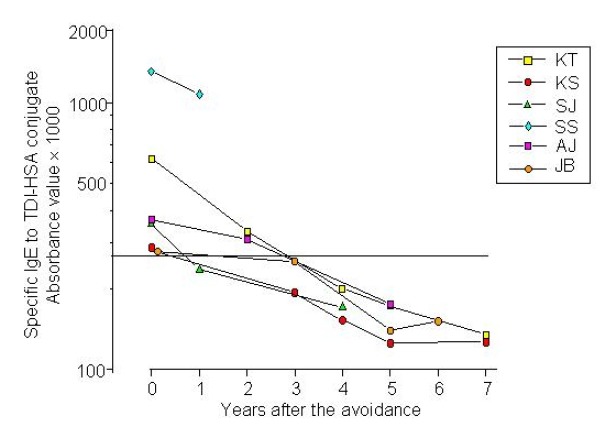
Changes in the levels of serum specific IgE antibody to TDI-HSA conjugate in sera of six TDI-induced asthmatic patients.
Figure 2.
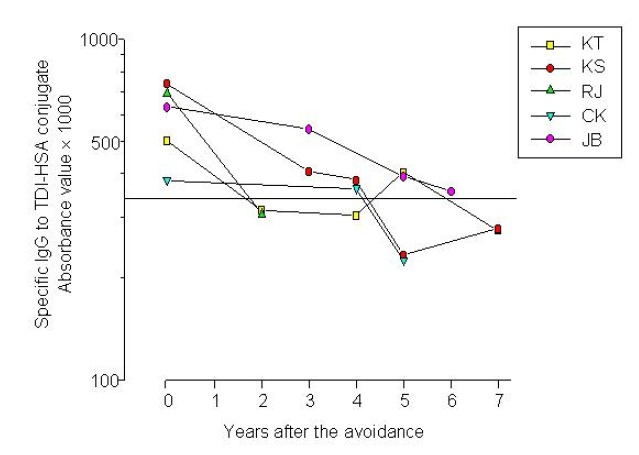
Changes in the levels of serum specific IgG antibodies to TDI-HSA conjugate measured by ELISA after the last exposure to TDI.
DISCUSSION
Recent investigations have detected sIgE to TDI-HSA conjugate in sera of TDI-asthma, while none in unexposed subjects or healthy controls2, 4). These findings suggest that TDI exposure may induce IgE-mediated bronchoconstriction in some asthmatic patients exposed to TDI. Regarding sIgG response to isocyanate-asthma, there has been one report suggesting a pathogenic role of sIgG to hexamethylene diisocyanate (HDI)- and methylene diisocyanate (MDI)-HSA conjugates5), while another report has suggested sIgG to MDI as an indicator of exposure6). Our previous study2) demonstrated that prevalence of sIgG to TDI-HSA conjugate was significantly higher in TDI-asthma than in those with negative responses on TDI-BPT, as well as those of allergic asthma and unexposed healthy controls, suggesting that sIgG may be closely linked with TDI-BPT results. Further studies are needed to clarify the role of sIgG in the pathogenesis of TDI asthma.
A two-year follow-up study7) of TDI-asthma showed that 51% had persistent asthmatic symptoms and airway hyperresponsiveness to methacholine. In the present study, all the subjects had persistent asthma symptoms and needed anti-asthmatic medications to control their symptoms. The time interval for sIgE antibodies to decline below the cut-off value was more than 2 years. The half-life was 3.9 years, which was longer than in the study by Tee at al4). Also, our study showed that the half-life of sIgG was 4.5 years. To our knowledge, this is the first report to observe changes in the levels of sIgG after complete avoidance from exposure. Further studies are needed to evaluate the clinical significance of long-lasting sIgE and sIgG. In conclusion, both sIgE and sIgG to TDI-HSA conjugate may persist for several years after the last exposure to TDI.
Footnotes
This work was supported by the Korean Research Foundation (KRF 2001-041-FOO 155)
REFERENCES
- 1.Park HS, Cho SH, Hong CS, Kim YY. Isocyanate-induced occupational asthma in far-east Asia: pathogenesis to prognosis. Clin Exp Allergy. 2002;32:198–204. doi: 10.1046/j.1365-2222.2002.01290.x. [DOI] [PubMed] [Google Scholar]
- 2.Park HS, Kim HY, Nahm DH, Son JW, Kim YY. Specific IgG, not specific IgE, antibodies to TDI-HSA conjugate are associated with TDI-bronchoprovocation test results. J Allergy Clin Immunol. 1999;104:847–851. doi: 10.1016/s0091-6749(99)70297-6. [DOI] [PubMed] [Google Scholar]
- 3.Barker RD, Harris JM, Welch JA, Venables KM, Newman Taylor AJ. Occupational asthma caused by tetrachlorophthalic anhydride: A 12-year follow-up. J Allergy Clin Immunol. 1998;101:717–719. doi: 10.1016/s0091-6749(98)70401-4. [DOI] [PubMed] [Google Scholar]
- 4.Tee RD, Cullinan P, Welch J, Burge PS, Newman-Taylor AJ. Specific IgE to isocyanates: A useful diagnostic role in occupational asthma. J Allergy Clin Immunol. 1998;101:709–715. doi: 10.1016/S0091-6749(98)70181-2. [DOI] [PubMed] [Google Scholar]
- 5.Cartier A, Grammer L, Malo JL, Lagier F, Ghezzo H, Harris K. Specific serum antibodies against isocyanate: association with occupational asthma. J Allergy Clin Immunol. 1989;84:507–514. doi: 10.1016/0091-6749(89)90364-3. [DOI] [PubMed] [Google Scholar]
- 6.Lushniak BD, Rich CM, Bernstein DI, Gallagner JS. Indirect assessment of exposure to diphenyl-methane diisocyanate (MDI) by evaluation of specific immune response to MDI-human serum albumin in farm worker at risk for occupational asthma. Am J Ind Med. 1998;33:471–477. doi: 10.1002/(sici)1097-0274(199805)33:5<471::aid-ajim6>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 7.Park HS, Nahm DH. Prognostic factors for toluene diisocyanate-induced occupational asthma after removal from exposure. Clin Exp Allergy. 1997;27:1145–1150. [PubMed] [Google Scholar]


