Abstract
Background :
Angiogenesis is of crucial importance for tumor growth and development of metastases. Vascular endothelial growth factor (VEGF) has a potent angiogenic activity and mutations of the p53 gene has been thought to upregulate VEGF. The purpose of our study was to evaluate the prognostic significance of these tumor biomarkers for angiogenesis relative to the information derived from established clinicopathological parameters in gastric cancer.
Methods :
In this study, we conducted an immunohistochemicai investigation of VEGF and p53 expression in 145 tissue samples obtained from gastric cancer patients undergoing curative surgical treatment. To evaluate angiogenesis, microvessel density (MVD) was counted by staining endothelial cells immunohistochemically using anti-CD34 monoclonal antibody.
Results :
High MVD was significantly associated with depth of tumor invasion and distant metastasis (p=0.004, 0.021, respectively). Moreover, overall survival for patients with high MVD were significantly lower than that of low MVD (p=0.048). Positive expression of VEGF correlated significantly with lymph node and distant metastasis (p=0.040, 0.048, respectively). However, no significant correlation was found between p53 expression and various clinicopathological parameters. VEGF positive tumors showed a higher MVD than VEGF negative tumors (p=0.028). The expression of p53 did not correlate with VEGF expression. Also, the relationship between the status of p53 expression and MVD had not statistically significant differences. In the multivariate analysis, status of VEGF, p53 expression and MVD were not an independent prognostic factor.
Conclusion :
VEGF seems to be an important, clinically relevant inducer of angiogenesis and angiogenesis assessed by the MVD may be a useful marker for predicting metastasis in gastric cancer. However, further studies are warranted to clarify the impact of p53 on the angiogenesis and the prognostic significance of angiogenesis in gastric cancer.
Keywords: Angiogenesis; Genes, p53; Stomach Neoplasms; Immunohistochemistry
INTRODUCTION
Angiogenesis has been shown to be a critical aspect of tumor growth and metastasis1–3). The induction of angiogenesis by a tumor is controlled process, influenced by angiogenic and angiostatic factors which involves a complex interaction between tumor and endothelial cells3–5). Among the many reported angiogenic factors, vascular endothelial growth factor (VEGF) is the most powerful endothelial-cell-specific mitogen that plays a key role in the complicated process of angiogenesis. It has been shown to be significantly upregulated in various human malignant tumors and to be associated with tumor angiogenesis and disease outcome6–9).
Tumor growth and metastasis are characterized by uncontrolled cellular proliferation. This is usually the result of multiple genetic and epigenetic insults to the cell, particularly involving proto-oncogenes and tumor suppressor genes. The genetic and epigenetic alterations that are responsible for tumor growth and metastasis may underlie the ability of tumors to switch to an angiogenic phenotype3–5).
p53 which encodes the tumor suppressor gene is mutated or deleted in about 50% of spontaneously arising tumors10). Several studies have indicated that angiogenesis may be regulated, in part, by the function of the p53 tumor suppressor gene. Functional p53 suppresses angiogenesis by downregulating angiogenic factor expression, whereas dysfunctional p53 stimulates angiogenesis by both upregulating VEGF and downregulating thrombospondin-1, an angiogenesis inhibitor11–14).
The degree of intratumoral microvessel density (MVD) is thought to reflect the angiogenic activity generated by the neoplastic cells and the supporting stroma. Moreover, tumor angiogenesis, as quantitated by measurement of intratumoral MVD, has shown to be a significant negative prognostic factor in various human tumors, including breast carcinoma, lung carcinoma, prostate carcinoma, endometrial carcinoma, colon carcinoma and gastric carcinoma15–20).
The purpose of our study was to evaluate the prognostic significance of these tumor biomarkers for angiogenesis relative to the information derived from established clinicopathological parameters in gastric cancer.
MATERIALS AND METHODS
Patients and tumor specimens
The study included 145 patients who underwent curative surgery for gastric cancer at Chonnam National University Hospital between January 1992 and December 1993. Formalin-fixed and paraffin-embedded tissue blocks were selected by viewing original pathologic slides and choosing blocks that show the junction between carcinoma and benign tissue. This allowed for direct comparison of carcinoma and benign tissue side by side after immunohistochemistry. Patient characteristics, including sex, age, histologic grade, stage and survival data, were obtained by medical records and pathologist and physician contact when necessary. No patient had received anticancer therapy prior to the operation. The histologic grade was classified according to the criteria of Lauren and the World Health Organization21, 22). The tumors were staged at the time of surgery by the standard criteria for TNM staging using the American Joint Committee on Cancer23). This study group comprised 99 males and 46 females. The mean age was 59.2±10.3 (mean±standard deviation) with a range from 28 to 79 years. The mean size of the tumor was 5.1±2.8 cm (mean±standard deviation) with a range from 0.5 to 15.0 cm.
Immunohistochemistry
All procedures for immunohistochemical staining were done by the Micro-Probe staining system (Fisher Scientific, Pittsburgh, PA) based on capillary action24). Paraffin sections, of 4 μm in thickness with mounted probe on slides, were immunostained with anti-mouse monoclonal antibodies by the avidin-biotin peroxidase complex method24). Sections were deparaffinized and rehydrated. They were immersed in 0.6% hydrogen peroxide for 5 minutes to block the endogenous peroxidase activity. A polyclonal antibody against VEGF (A-20; diluted 1:50; Santa Cruz Biotechnology, Santa Cruz, Calf, USA), a monoclonal antibody against CD34 (QB-END/10; diluted 1:25; Novocstra Lab., Newcastle, UK) and a monoclonal mouse antihuman p53 antibody (DO-7, diluted 1:100; Dakopatts, Glostrup, Denmark) were used as primary antibodies. The primary antibodies, in the aforementioned concentrations, were diluted in phosphate- buffered saline supplemented with 5% normal horse serum and 1% bovine serum albumin and then incubated with tissues for 15 minutes at 45°C. Anti-mouse immunoglobulin G (Sigma, St. Louis, MO) labeled with biotin was added as a secondary antibody for the detection of primary antibodies and the samples were incubated for 7 minutes at 45°C. After multiple rinses with universal buffer, streptavidin-alkaline phosphatase detection system (Biomeda, Foster, CA) was applied for 7 minutes. As the final step, the slides were developed for 7 minutes with the enzyme substrate 3 amino-9-ethyl carbazole (AEC, Sigma, St. Louis, MO). The slides were counterstained with hematoxylin solution for 1 minute (Research Genetics, Huntsville, AL). After dehydration, the tissue was sealed with a universal mount (Research Genetics, Huntsville, AL). For negative controls, the primary antibody was omitted and replaced with phosphate-buffered saline.
Evaluation of VEGF and p53 expression
Staining intensity was classified from zero (no staining) to 3 (strong staining) and the percentage of staining area was classified as 0 for no positive staining of tumor cells, 1 for positive staining in <10% of the tumor cells, 2 for positive staining in 10% to 50% of the tumor cells, or 3 for positive staining in >50% of the tumor cells. A staining index was calculated as the product of staining intensity and staining area18). Assessment of the staining was evaluated by two independent observers without knowledge of the clinical outcomes, such as tumor stage, grade and survival. Consensus scores were assigned for each case by reviewing the slides with discrepancies in scoring. All sections on which the two observers disagreed were re-evaluated and, after discussion, there was total agreement on the classification. The tumors were categorized as positive expression (staining index>4) or negative expression (staining index≤4).
Microvessel staining and density
Microvessels were highlighted with a monoclonal antibody against CD34 (QB-END/10; diluted 1:25; Novocstra Lab., Newcastle, UK) using the Micro-Probe staining system (Fisher Scientific, Pittsburgh, PA) based on capillary action. Microvessel quantification was performed according to an international consensus25). Any single brown-stained cell or cluster of endothelial cells that was clearly separate from adjacent microvessels was regarded as a microvessel (Figure 1). Neither vessel lumens nor the presence of red blood cells were used to define a micovessel. Large vessels with thick muscular walls were excluded from the counts. The stained sections were screened at ×40 magnification to identify the areas of the highest vascular density within the tumor. Vessels were counted in the 5 areas of highest vascular density at ×200 magnification. MVD was expressed as the mean number of vessels in these areas.
Figure 1.
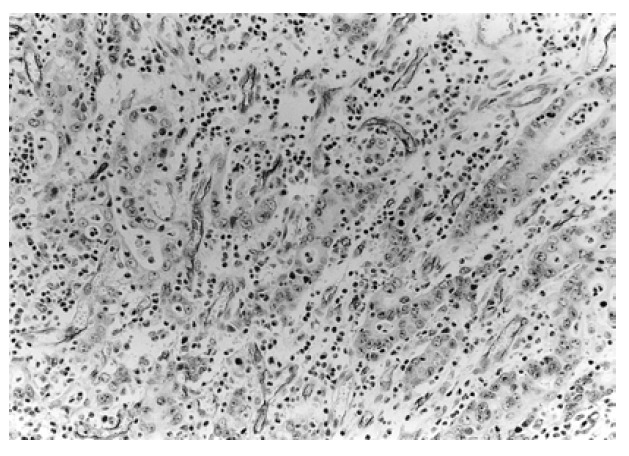
Immunohistochemical staining of endothelial cells with an antibody against CD-34. Individual microvessels can easily be identified (×200).
Statistical analysis
The χ2-test and Fisher’s exact test, where appropriate, were used to compare expression of the VEGF and p53 with various clinicopathological parameters. The relationship between VEGF or p53 expression and MVD was evaluated by the Mann-Whitney U test. Actuarial survival rates of patients were evaluated according to the Kaplan-Meier method and the differences were tested with a log-rank test. The Cox regression model was used to determine the prognostic significance of each parameter by a multivariate analysis. The statistical software program used was Statistical Package for the Social Sciences (SPSS/PC+ 10.0, Chicago, IL). A p value of less than 0.05 was accepted as statistically significant.
RESULTS
Expression of VEGF and p53 in gastric cancer tissues
Normal gastric mucosa was not immunoreactive with an anti-VEGF antibody. VEGF was mainly localized to the cytoplasm or the membrane of the tumor cells (Figure 2). Tumor cells that stained strongly for VEGF were observed more often in the invasive front than in the tumor center. In cancerous tissues, positive expression of VEGF was 31.0% (45/145) (Table 1). Abnormal accumulation of the p53 protein was evident in the nuclei of tumor cells (Figure 3), and heterogeneously distributed. Based on our criteria, the positive expression of p53 in cancerous tissues was 35.9% (52/145) (Table 1).
Figure 2.
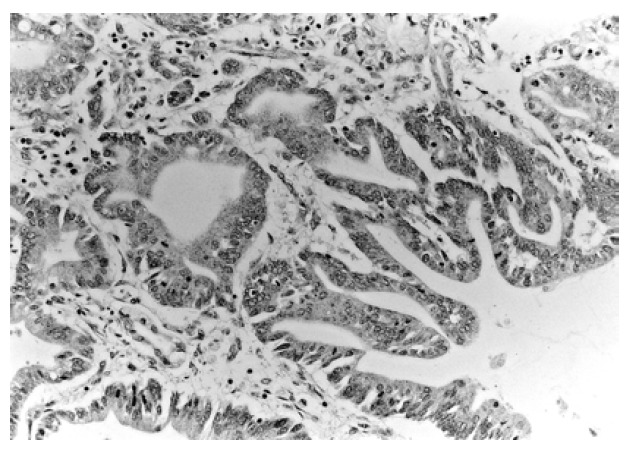
Typical immunohistochemical staining of VEGF in gastric cancer tissue. VEGF immunoreactivity is strongly expressed in the cytoplasm of the tumor cells (×200).
Table 1.
Correlation between VEGF and p53 expression in gastric cancer
| VEGF expression | p53 expression | p-value | |
|---|---|---|---|
| Positive (n=52) | Negative (n=93) | ||
| Positive (n=45) | 16 | 29 | |
| Negative (n=100) | 36 | 64 | 0.959 |
VEGF, vascular endothelial growth factor
Figure 3.
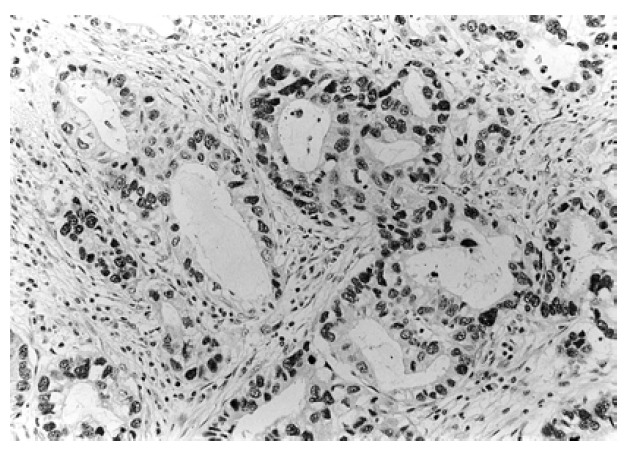
Typical immunohistochemical staining of p53 in gastric cancer tissue. Intense nuclear localization of p53 protein is detected in tumor cells (×200).
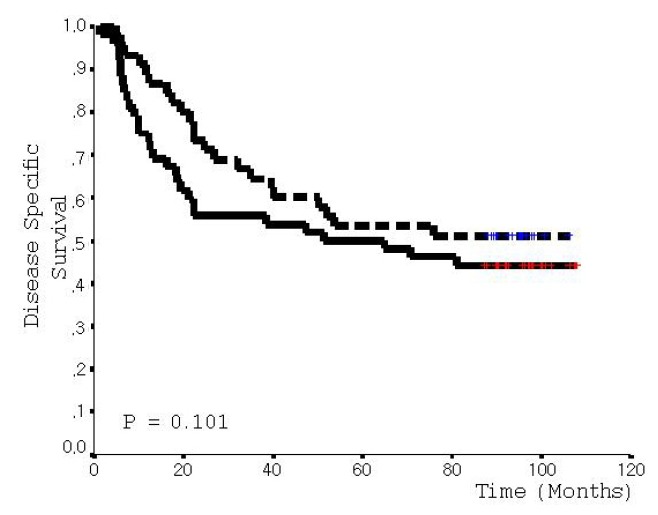
Correlation between VEGF and p53 expression and clinicopathological features
The expression of p53 did not correlate with VEGF expression (p=0.959, Table 1). The correlation between VEGF or p53 expression and clinicopathological parameters is summarized in Table 2, 3. Positive expression of VEGF correlated significantly with lymph node and distant metastasis (p=0.040, 0.048, respectively, Table 2). There was a trend towards an association between the positive expression of VEGF and poor survival (p=0.087, Figure 4). However, no significant correlation was found between p53 expression and various clinicopathological parameters, including survival (Table 3, Figure 5).
Table 2.
Correlation between VEGF expression and clinicopathological parameters of gastric cancer
| Clinicopathological parameters | Total (n=145) | VEGF expression | p-value | |
|---|---|---|---|---|
| Positive (n=45) | Negative (n=100) | |||
| Age (years) | ||||
| < 60 | 67 | 19 | 48 | 0.519 |
| ≥ 60 | 78 | 26 | 52 | |
| Sex | ||||
| Male | 99 | 32 | 67 | 0.623 |
| Female | 46 | 13 | 33 | |
| Tumor size (cm) | ||||
| < 5.0 | 66 | 18 | 48 | 0.403 |
| ≥ 5.0 | 79 | 27 | 52 | |
| Lauren Classification | ||||
| Intestinal | 70 | 17 | 53 | 0.223 |
| Diffuse | 42 | 15 | 27 | |
| Mixed | 33 | 13 | 20 | |
| Differentiation grade* | ||||
| WD | 24 | 3 | 21 | 0.096 |
| MD | 45 | 15 | 30 | |
| PD | 76 | 27 | 49 | |
| TNM stage | ||||
| I | 52 | 10 | 42 | 0.064 |
| II | 21 | 8 | 13 | |
| III | 47 | 15 | 32 | |
| IV | 25 | 12 | 13 | |
| Depth of tumor invasion (T) | ||||
| T1 | 24 | 7 | 17 | 0.163 |
| T2 | 32 | 5 | 27 | |
| T3 | 75 | 28 | 47 | |
| T4 | 14 | 5 | 9 | |
| Lymph node metastasis (N) | ||||
| N0 | 70 | 16 | 54 | 0.040 |
| N1–3 | 75 | 29 | 46 | |
| Distant metastasis (M) | ||||
| M0 | 125 | 35 | 90 | 0.048 |
| M1 | 20 | 10 | 10 | |
VEGF, vascular endothelial growth factor;
WD, well differentiated; MD, moderately differentiated; PD, poorly differentiated adenocarcinoma
Table 3.
Correlation between p53 expression and clinicopathological parameters of gastric cancer
| Clinicopathological parameters | Total (n=145) | p53 expression | p-value | |
|---|---|---|---|---|
| Positive (n=52) | Negative (n=93) | |||
| Age (years) | ||||
| < 60 | 67 | 25 | 42 | 0.736 |
| ≥ 60 | 78 | 27 | 51 | |
| Sex | ||||
| Male | 99 | 37 | 62 | 0.578 |
| Female | 46 | 15 | 31 | |
| Tumor size (cm) | ||||
| < 5.0 | 66 | 25 | 41 | 0.594 |
| ≥ 5.0 | 79 | 27 | 52 | |
| Lauren Classification* | ||||
| Intestinal | 70 | 27 | 43 | 0.280 |
| Diffuse | 42 | 11 | 31 | |
| Mixed | 33 | 14 | 19 | |
| Differentiation grade* | ||||
| WD | 24 | 9 | 15 | 0.721 |
| MD | 45 | 18 | 27 | |
| PD | 76 | 25 | 51 | |
| TNM stage | ||||
| I | 52 | 17 | 35 | 0.280 |
| II | 21 | 6 | 15 | |
| III | 47 | 22 | 25 | |
| IV | 25 | 7 | 18 | |
| Depth of tumor invasion (T) | ||||
| T1 | 24 | 3 | 21 | 0.147 |
| T2 | 32 | 18 | 14 | |
| T3 | 75 | 25 | 50 | |
| T4 | 14 | 6 | 8 | |
| Lymph node metastasis (N) | ||||
| N0 | 70 | 23 | 47 | 0.456 |
| N1–3 | 75 | 29 | 46 | |
| Distant metastasis (M) | ||||
| M0 | 125 | 46 | 79 | 0.556 |
| M1 | 20 | 6 | 14 | |
WD, well differentiated; MD, moderately differentiated; PD, poorly differentiated adenocarcinoma
Figure 4.
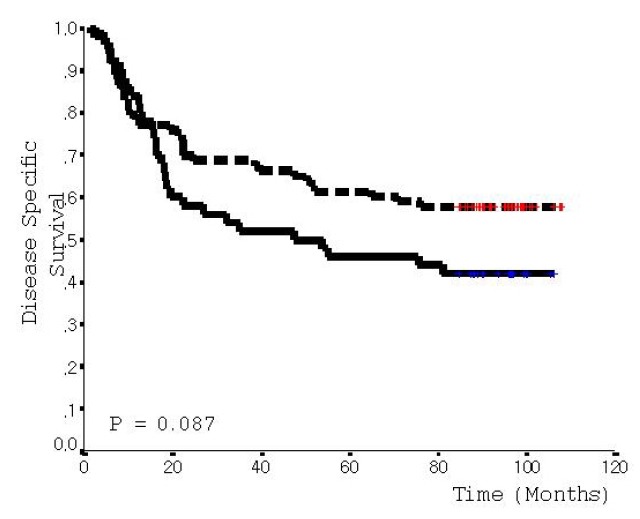
Kaplan-Meier survival curve correlating disease specific survival with positive (solid line) or negative (dotted line) expression of VEGF.
Figure 5.
Kaplan-Meier survival curve correlating disease specific survival with positive (solid line) or negative (dotted line) expression of p53.
Correlation between MVD and clinicopathological features
The MVD for 145 tumors ranged from 23.0 to 182.0 with a mean MVD of 74.0±31.1. When a mean MVD value of 74.0 was chosen as the cut-off point for discrimination of the 145 patients into two subgroups, 74 patients were categorized as high MVD and 71 as low MVD. High MVD was significantly associated with the depth of tumor invasion (p=0.004) and also did correlate with distant metastasis (p=0.021) (Table 4). Moreover, the overall survival for patients with high MVD was significantly lower than that of low MVD (p=0.048) (Figure 6).
Table 4.
Correlation between microvessel density group and clinicopathological parameters of gastric cancer
| Clinicopathological parameters | Total (n=145) | Microvessel density (MVD) Group | p-value | |
|---|---|---|---|---|
| High MVD (n=74) | Low MVD (n=71) | |||
| Age (years) | ||||
| < 60 | 67 | 33 | 34 | 0.627 |
| ≥ 60 | 78 | 41 | 37 | |
| Sex | ||||
| Male | 99 | 49 | 50 | 0.599 |
| Female | 46 | 25 | 21 | |
| Tumor size (cm) | ||||
| < 5.0 | 66 | 30 | 36 | 0.501 |
| ≥ 5.0 | 79 | 44 | 35 | |
| Lauren Classification | ||||
| Intestinal | 70 | 32 | 38 | 0.382 |
| Diffuse | 42 | 25 | 17 | |
| Mixed | 33 | 17 | 16 | |
| Differentiation grade* | ||||
| WD | 24 | 7 | 17 | 0.613 |
| MD | 45 | 27 | 18 | |
| PD | 76 | 40 | 36 | |
| TNM stage | ||||
| I | 52 | 21 | 31 | 0.068 |
| II | 21 | 11 | 10 | |
| III | 47 | 23 | 24 | |
| IV | 25 | 19 | 6 | |
| Depth of tumor invasion (T) | ||||
| T1 | 24 | 5 | 19 | 0.004 |
| T2 | 32 | 16 | 16 | |
| T3 | 75 | 40 | 35 | |
| T4 | 14 | 13 | 1 | |
| Lymph node metastasis (N) | ||||
| N0 | 70 | 35 | 35 | 0.756 |
| N1–3 | 75 | 39 | 36 | |
| Distant metastasis (M) | ||||
| M0 | 125 | 58 | 67 | 0.021 |
| M1 | 20 | 16 | 4 | |
WD, well differentiated; MD, moderately differentiated; PD, poorly differentiated adenocarcinoma
Figure 6.
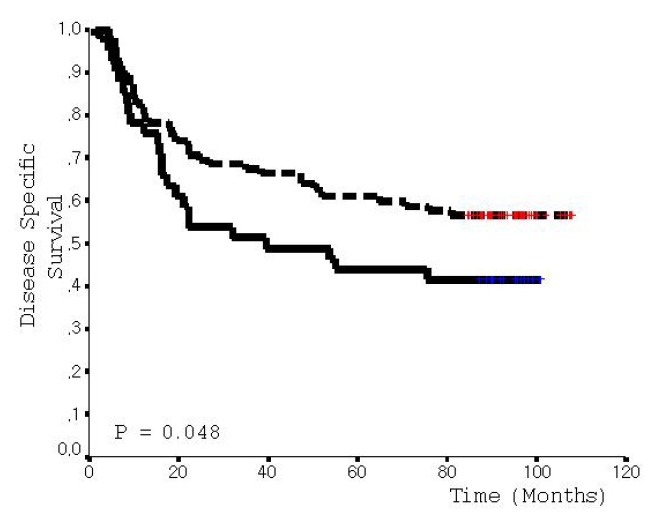
Kaplan-Meier survival curve correlating disease specific survival with high MVD (solid line) or low MVD (dotted line).
Correlation between VEGF or p53 expression and MVD
The mean MVD value of VEGF positive tumors was 78.5±31.3 and was a significantly higher MVD than that of VEGF negative tumors (p=0.028). However, the relationship between the status of p53 expression and MVD was not statistically significant (p=0.525). The mean MVD value of VEGF and p53 positive tumors was 75.6±30.3 and was higher than that of VEGF and p53 negative tumors, but the mean MVD value of both groups did not show statistically significant difference (p=0.147) (Table 5).
Table 5.
The relationship between microvessel density and the expression of VEGF and p53 in gastric cancer
| VEGF/p53 status | Total (n=145) | Microvessel density (MVD) No. | p-value | |
|---|---|---|---|---|
| Mean±SD | Range | |||
| VEGF | ||||
| Positive | 45 | 78.5±1.3 | 30.3–182.0 | 0.028 |
| Negative | 100 | 71.2±26.3 | 23.0–164.5 | |
| p53 | ||||
| Positive | 52 | 72.7±29.8 | 23.0–182.0 | 0.525 |
| Negative | 93 | 76.9±34.1 | 27.5–173.6 | |
| VEGF/p53 | ||||
| Positive/Positive* | 16 | 75.6±30.3 | 45.1–182.0 | 0.147* |
| Positive/Negative | 29 | 74.5±28.5 | 30.3–173.6 | |
| Negative/Positive | 36 | 73.7±35.5 | 23.0–164.5 | |
| Negative/Negative* | 64 | 72.3±32.0 | 27.5–157.3 | |
VEGF, vascular endothelial growth factor; No, number; SD, standard deviation
Prognostic value of VEGF status, p53 status, MVD and conventional clinicopathological parameters
When the status of VEGF and p53, MVD and conventional clinicopathological parameters were analyzed by the Cox regression model, the stage and status of metastasis were found to be significant, independent, prognostic factors, while the status of VEGF, p53 expression and MVD were not significant (data not shown).
DISCUSSION
Angiogenesis is crucial for normal growth and development and in protective responses, such as wound healing and inflammation. However, aberrant angiogenesis can occur in a variety of pathological settings including growth and dissemination of tumors1–3).
Recognition of the importance of angiogenesis for the growth and dissemination of tumors has raised fundamental questions regarding the molecular mechanisms of the angiogenic switch during tumor progression. The angiogenic switch is regulated by changes in the relative balance between inducers and inhibitors of endothelial cell proliferation and migration5). The switch can be activated by increasing the levels of inducers, such as VEGF and/or by reducing the concentration of inhibitors, such as thrombospondin15). Among the many reported angiogenic inducers, VEGF is thought to be the most powerful angiogenic inducer. In various human cancers, VEGF expression was correlated with tumor angiogenesis and prognosis6–9). Also, in our study, VEGF positive tumors showed a higher MVD than VEGF negative tumors. Positive expression of VEGF correlated significantly with lymph node and distant metastasis. There was a trend towards an association between the positive expression of VEGF and poor survival. These results suggest that VEGF may be an important, clinical relevant inducer of angiogenesis and a predictor of metastatic potential in gastric cancer.
The genetic alterations involved in the tumorigenesis are also responsible for the phenotypic characteristics of cancer cells. The p53 tumor suppressor gene is one of the most frequently mutated genes in human cancers10). Previous reports indicate that loss of p53 function, via somatic mutations or expression of viral oncoproteins, contributes to activation of the angiogenic switch during tumorigenesis11–14). The p53-mediated inhibition of VEGF expression, with the ability of p53 to upregulate thrombospondin-1, indicates that p53 provides dual functions that regulate angiogenesis. Thus, loss of p53 function during tumorigenesis deregulates both arms of the balance, providing a potent stimulus for angiogenesis and tumor progression11–14). Recent studies have shown that p53 expression correlates with tumor angiogenesis through VEGF upregulation in human gastric cancers26–29). However, in our study, the expression of p53 did not correlate with VEGF expression. Also, p53 expression was not related with high MVD. Our results suggest that tumor angiogenesis, through the regulation of VEGF in gastric cancer, may be not dependent on p53 status. However, these contradictory findings might be due to differences in the antibody used, staining methods or the criteria used. Also, immunohistochemistry has been shown to have a discordancy rate of 30–35% when compared with techniques that determine p53 gene status, including single strand conformation polymorphism polymerase chain reaction analysis and direct DNA sequencing30, 31). Thus, it should be noted that the expression of p53 as detected by immunohistochemistry does not provide adequate information about the dysfunction of the protein and gene mutation. Further studies are needed to evaluate the effect of p53 status on angiogenesis in an in vivo tumorigenesis context.
Tumor angiogenesis, as quantitated by measurement of intratumoral MVD, has recently shown to be a parameter of potential prognostic significance for various human tumors15–20). In our study, high MVD was significantly associated with the depth of tumor invasion, distant metastasis and poor survival. These results suggest that tumor angiogenesis may be a useful marker for predicting metastasis in gastric cancer, but MVD or VEGF expression were not found to be significant, independent, prognostic factors in a multivariate analysis by the Cox regression model. Furthermore, several reports have shown that MVD is not a reliable predictor of metastasis-free survival or overall survival in colon and pancreatic cancers32–34).
A discrepancy still exists in the impact of tumor angiogenesis as a prognostic predictor of cancer patients, according to our and other reports. There are several possible explanations for this discrepancy. First, in various human cancers, the quantitation of tumor angiogenesis by MVD, as reported in different studies, is difficult to compare due to different score systems and different antibodies used. Also, accurately measuring MVD requires superb immunohistochemistry, representative tumor tissue, relatively standard field size and considerable experience at tumor pathology35). Second, this may be due in part to inadequate sample size, inappropriate multiple significance testing and arbitrary definition of patients’ group36). Third, biological processes, such as tumor growth and metastasis, are regulated by a complex interplay of multiple factors, including angiogenic factor, growth factor, motility factor and cell adhesion molecules. Thus, the capacity of tumor cells to induce angiogenesis does not always correlate with malignant potential and it is unclear whether the growth, metastasis and clinical outcome of a tumor is angiogenesis-dependent37).
In conclusion, VEGF seems to be an important, clinically relevant inducer of angiogenesis, and tumor angiogenesis assessed by the MVD may be a useful marker for predicting metastasis in gastric cancer. However, further studies are warranted to clarify the impact of p53 on the angiogenesis and prognostic significance of angiogenesis in gastric cancer.
Footnotes
This study was supported by a grant from the Korean Circulation Society (2000-5)
REFERENCES
- 1.Folkman J, Shing Y. Angiogenesis. J Biol Chem. 1992;267:10931–10934. [PubMed] [Google Scholar]
- 2.Folkman J. What is the evidence that tumors are angiogenesis dependent? J Natl Cancer Inst. 1990;82:4–6. doi: 10.1093/jnci/82.1.4. [DOI] [PubMed] [Google Scholar]
- 3.Folkman J. Clinical application of research on angiogenesis. N Engl J Med. 1995;333:1757–1763. doi: 10.1056/NEJM199512283332608. [DOI] [PubMed] [Google Scholar]
- 4.Risau W. Mechanisms of angiogenesis. Nature. 1997;386:671–674. doi: 10.1038/386671a0. [DOI] [PubMed] [Google Scholar]
- 5.Hanahan D, Folkman J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell. 1996;86:353–364. doi: 10.1016/s0092-8674(00)80108-7. [DOI] [PubMed] [Google Scholar]
- 6.Ferrara N, Heinsohn H, Walder CE, Bunting S, Thomas GR. The regulation of blood vessel growth by vascular endothelial growth factor. Ann NY Acad Sci. 1995;752:246–256. doi: 10.1111/j.1749-6632.1995.tb17435.x. [DOI] [PubMed] [Google Scholar]
- 7.Ferrara N. The role of vascular endothelial growth factor in pathological angiogenesis. Breast Cancer Res Treat. 1995;36:127–137. doi: 10.1007/BF00666035. [DOI] [PubMed] [Google Scholar]
- 8.Kolch W, Martiny-Baron G, Kieser A, Marme D. Regulation of the expression of the VEGF/VPS and its receptors: role in tumor angiogenesis. Breast Cancer Res Treat. 1995;36:139–155. doi: 10.1007/BF00666036. [DOI] [PubMed] [Google Scholar]
- 9.Leung DW, Cachianes G, Kuang WJ, Goeddel DV, Ferrara N. Vascular endothelial growth factor is a secreted angiogenic mitogen. Science. 1989;246:1306–1309. doi: 10.1126/science.2479986. [DOI] [PubMed] [Google Scholar]
- 10.Hollstein M, Rice K, Greenblatt MS, Soussi T, Fuchs R, Sorlie T, Hovig E, Smith-Sorensen B, Montesano R, Harris CC. Database of p53 gene somatic mutations in human tumors and cell lines. Nucleic Acids Res. 1994;22:3551–3555. [PMC free article] [PubMed] [Google Scholar]
- 11.Kieser A, Weich HA, Brandner G, Marme D, Lolch W. Mutant p53 potentiates protein kinase C production of vascular endothelial growth factor expression. Oncogene. 1994;9:963–969. [PubMed] [Google Scholar]
- 12.Dameron KM, Volpert OV, Tainsky MA, Bouck N. Control of angiogenesis in fibroblasts by p53 regulation of thrombospondin-1. Science. 1994;265:1582–1584. doi: 10.1126/science.7521539. [DOI] [PubMed] [Google Scholar]
- 13.Van Meir EG, Polverini P, Chazin VR, Su Huang HJ, de Tribolet N, Cavenee WK. Release of an inhibitor of angiogenesis upon induction of wild-type p53 expression in glioblastoma cells. Nat Genet. 1994;8:171–176. doi: 10.1038/ng1094-171. [DOI] [PubMed] [Google Scholar]
- 14.Bouck N. p53 and angiogenesis. Biochem Biophys Acta. 1996;1287:63–66. doi: 10.1016/0304-419x(96)00005-4. [DOI] [PubMed] [Google Scholar]
- 15.Weider N, Semple JP, Welch WR, Folkman J. Tumor angiogenesis and metastasis: correlation in invasive breast carcinoma. N Engl J Med. 1991;324:1–8. doi: 10.1056/NEJM199101033240101. [DOI] [PubMed] [Google Scholar]
- 16.Macchiarini P, Fontanini G, Hardin MJ, Squartini F, Angeletti CA. Relation of neovascularization to metastasis of non-small cell lung cancer. Lancet. 1992;340:145–147. doi: 10.1016/0140-6736(92)93217-b. [DOI] [PubMed] [Google Scholar]
- 17.Weider N, Carroll PR, Flax J, Blumenfeld W, Folkman J. Tumor angiogenesis correlates with metastasis in invasive prostate carcinoma. Am J Pathol. 1993;143:401–409. [PMC free article] [PubMed] [Google Scholar]
- 18.Salvesen HB, Iversen OE, Akslen LA. Prognostic significance of angiogenesis and Ki-67, p53, and p21 expression: a population-based endometrial carcinoma study. J Clin Oncol. 1999;17:1382–1390. doi: 10.1200/JCO.1999.17.5.1382. [DOI] [PubMed] [Google Scholar]
- 19.Takahashi Y, Kitadai Y, Bucana CD, Cleary K, Ellis LM. Expression of vascular endothelial growth factor and its receptor, KDR, correlates with vascularity, metastasis and proliferation of human colon cancer. Cancer Res. 1995;55:3964–3968. [PubMed] [Google Scholar]
- 20.Tanigawa N, Amaya H, Matsumura M, Shimomatsuya T, Horiuchi T, Muraoka R, Iki M. Extent of tumor vascularization correlates with prognosis and hematogenous metastasis in gastric carcinomas. Cancer Res. 1996;56:2671–2676. [PubMed] [Google Scholar]
- 21.Lauren P. The two histologic main types of gastric carcinoma. Acta Pathol Microbiol Scand. 1965;63:31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 22.Watanabe H, Jass JR, Sobin LH. WHO International Histologic Classification of Tumors. Berlin, Heidelberg, New York, Paris, Tokyo, Hong Kong: Springer-Verlag; 1990. Histologic typing of oesophageal and gastric tumors. [Google Scholar]
- 23.American Joint Committee on Cancer . Stomach cancer. Philadelphia: Lippincott-Raven; 1997. Manual for staging cancer; pp. 71–76. [Google Scholar]
- 24.Reed JA, Manahan LJ, Park CS, Brigati DJ. Complete one-hour immunohistochemistry based on capillary action. Biotechniques. 1992;13:434–443. [PubMed] [Google Scholar]
- 25.Vermeulen PB, Gasparini G, Fox SB, Toi M, Martin L, McCulloch P, Pezzella F, Viale G, Weidner N, Harris AL, Dirix LY. Quantification of angiogenesis in solid human tumours: an international consensus on the methodology and criteria of evaluation. Eur J Cancer. 1996;32:2474–2484. doi: 10.1016/s0959-8049(96)00379-6. [DOI] [PubMed] [Google Scholar]
- 26.Maehara Y, Kabashima A, Koga T, Tokunaga E, Takeuchi H, Kakeji Y, Sugimachi K. Vascular invasion and potential for tumor angiogenesis and metastasis in gastric carcinoma. Surgery. 2000;128:408–416. doi: 10.1067/msy.2000.107265. [DOI] [PubMed] [Google Scholar]
- 27.Saito H, Tujitani S, Ikeguchi M, Maeta M, Kaibara N. Neoangiogenesis and relationship to nuclear p53 accumulation and vascular endothelial growth factor expression in advanced gastric carcinoma. Oncology. 1999;57:164–172. doi: 10.1159/000012025. [DOI] [PubMed] [Google Scholar]
- 28.Maeda K, Kang SM, Onoda N, Ogawa M, Sawada T, Nakata B, Kato Y, Chung YS, Sowa M. Expression of p53 and vascular endothelial growth factor associated with tumor angiogenesis and prognosis in gastric cancer. Oncology. 1998;55:594–599. doi: 10.1159/000011918. [DOI] [PubMed] [Google Scholar]
- 29.Giatromanolaki A, Koukourakis MI, Stathopoulos GP, Kapsoritakis A, Paspatis G, Kakolyris S, Sivridis E, Georgoulias V, Harris AL, Gatter KC. Angiogenic interactions of vascular endothelial growth factor, of thymidine phosphoryiase and of p53 protein expression in locally advanced gastric cancer. Oncol Res. 2000;12:33–41. doi: 10.3727/000000001108747426. [DOI] [PubMed] [Google Scholar]
- 30.Dix B, Robbins P, Carrello S, Howe A, Iacopetta B. Comparison of p 53 gene mutation and protein overexpression in colorectal carcinomas. Br J Cancer. 1990;70:585–590. doi: 10.1038/bjc.1994.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kahlenberg MS, Stoler DL, Rodriguez-Bigas MA, Weber TK, Driscoll DL, Anderson GR, Petrelli NJ. p53 tumor suppressor gene mutations predict decreased survival of patients with sporadic colorectal carcinoma. Cancer. 2000;88:1814–1819. [PubMed] [Google Scholar]
- 32.Bossi P, Viale G, Lee AK, Alfano R, Coggi G, Bosari S. Angiogenesis in colorectal tumors: microvessel quantitation in adenomas and carcinomas with clinicopathological correlations. Cancer Res. 1995;55:5049–5053. [PubMed] [Google Scholar]
- 33.Mooteri S, Rubin D, Leurgans S, Jakate S, Drabe E, Saclarides T. Tumor angiogenesis in primary and metastatic colorectal cancers. Dis Colon Rectum. 1996;39:1073–1080. doi: 10.1007/BF02081403. [DOI] [PubMed] [Google Scholar]
- 34.Fujimoto K, Hosotani R, Wada M, Lee JU, Koshiba T, Miyamoto Y, Tsuji S, Nakajima S, Doi R, Imamura M. Expression of two angiogenic factors, vascular endothelial growth factor and platelet-derived endothelial cell growth factor in human pancreatic cancer, and its relationship to angiogenesis. Eur J Cancer. 1998;34:1439–1447. doi: 10.1016/s0959-8049(98)00069-0. [DOI] [PubMed] [Google Scholar]
- 35.Weidner N. Angiogenesis as a predictor of clinical outcome in cancer patients. Hum Pathol. 2000;31:403–405. doi: 10.1053/hp.2000.6724. [DOI] [PubMed] [Google Scholar]
- 36.Hall PA, Going JJ. Review. Predicting the future: a critical appraisal of cancer prognosis studies. Histopathology. 1999;35:489–494. doi: 10.1046/j.1365-2559.1999.00862.x. [DOI] [PubMed] [Google Scholar]
- 37.Ellis LM, Fidler IJ. Angiogenesis and metastasis. Eur J Cancer. 1996;32:2451–2460. doi: 10.1016/s0959-8049(96)00389-9. [DOI] [PubMed] [Google Scholar]


